Oral candidiasis pathophysiology: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
m Bot: Removing from Primary care |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Oral candidiasis}} | {{Oral candidiasis}} | ||
{{CMG}} | {{CMG}};{{AE}}{{AY}} | ||
==Overview== | ==Overview== | ||
[[Candida]] is a normal [[commensal]] of the skin and mucous membranes. The balance between the [[virulence]] of the [[fungus]] and the [[Immune response|host immune defense]] is responsible avoiding [[opportunistic infection]] of candida. | [[Candida]] is a normal [[commensal]] of the skin and mucous membranes. The balance between the [[virulence]] of the [[fungus]] and the [[Immune response|host immune defense]] is responsible avoiding [[opportunistic infection]] of candida. | ||
Deficiency of [[cell-mediated immunity]] or poor general status are the main risk factors for having opportunistic candidiasis. | Deficiency of [[cell-mediated immunity]] or poor general status are the main risk factors for having opportunistic candidiasis. | ||
Candidiasis is usually localized to skin and mucous membranes. In rare cases, candidiasis can spread causing [[Candidiasis| | Candidiasis is usually localized to skin and mucous membranes. In rare cases, candidiasis can spread causing [[Candidiasis|candidemia]] and distant infection. These cases are usually associated with [[Immunodeficiency|deficient immunity]] | ||
[[C. albicans]] is the main species causing infection in humans more than any other candida species. | . [[C. albicans]] is the main species causing infection in humans more than any other [[Candida|candida species]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 19: | Line 16: | ||
*Secreting '''molecules that mediate adherence''' into host cells | *Secreting '''molecules that mediate adherence''' into host cells | ||
*Production of '''[[hydrolases]]''' which has a [[Lytic|lytic effect]] on tissues and facilitate the invasion by the [[fungus]]. | *Production of '''[[hydrolases]]''' which has a [[Lytic|lytic effect]] on tissues and facilitate the invasion by the [[fungus]]. | ||
*'''[[Polymorphism]]:''' [[Candida]] has the ability to grow either as [[Hyphae|pseudohyphae]] (elongated ellipsoid form) or in a [[Yeast|yeast form]] (rounded to oval budding form. While the role of polymorphism is not clearly understood in the [[virulence]] of [[Candida]], it’s noted that the species that are capable of producing the most severe form of the disease has this ability. | *'''[[Polymorphism]]:''' [[Candida]] has the ability to grow either as [[Hyphae|pseudohyphae]] (elongated ellipsoid form) or in a [[Yeast|yeast form]] (rounded to oval budding form. While the role of [[polymorphism]] is not clearly understood in the [[virulence]] of [[Candida]], it’s noted that the species that are capable of producing the most severe form of the disease has this ability. | ||
*'''[[Biofilm|Biofilm production]]:''' which means the ability to form a thick layer of the [[organism]] on the [[Mucosal|mucosal surfaces]] or even on [[catheters]] and [[dentures]]. | *'''[[Biofilm|Biofilm production]]:''' which means the ability to form a thick layer of the [[organism]] on the [[Mucosal|mucosal surfaces]] or even on [[catheters]] and [[dentures]]. | ||
Any condition that compromises [[ | Any condition that compromises [[cell-mediated immunity]], worsens the general status of the patient or provide a favorable medium for [[Candida]] to form [[biofilms]] put the patient at increased risk for having candidiasis.<ref name="pmid16984866">{{cite journal |vauthors=Pappas PG |title=Invasive candidiasis |journal=Infect. Dis. Clin. North Am. |volume=20 |issue=3 |pages=485–506 |year=2006 |pmid=16984866 |doi=10.1016/j.idc.2006.07.004 |url=}}</ref> | ||
[[Gene|Candidal gene]] VPS4 plays an important role in | [[Gene|Candidal gene]] [[VPS4A|VPS4]] plays an important role in mucosal candidiasis specifically. Moreover, fungi with mutations affecting this [[gene]] were found to be less virulent.<ref name="pmid25483774">{{cite journal |vauthors=Rane HS, Hardison S, Botelho C, Bernardo SM, Wormley F, Lee SA |title=Candida albicans VPS4 contributes differentially to epithelial and mucosal pathogenesis |journal=Virulence |volume=5 |issue=8 |pages=810–8 |year=2014 |pmid=25483774 |doi=10.4161/21505594.2014.956648 |url=}}</ref><ref name="pmid18814053">{{cite journal |vauthors=Lee SA, Jones J, Hardison S, Kot J, Khalique Z, Bernardo SM, Lazzell A, Monteagudo C, Lopez-Ribot J |title=Candida albicans VPS4 is required for secretion of aspartyl proteases and in vivo virulence |journal=Mycopathologia |volume=167 |issue=2 |pages=55–63 |year=2009 |pmid=18814053 |doi=10.1007/s11046-008-9155-7 |url=}}</ref> | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
====Pseudomembranous candidiasis:==== | ====Pseudomembranous candidiasis:==== | ||
On speculum examination typical curdy white discharge is present. Usually present in newborns or in patients with [[Immunodeficiency|deficient immunity]], administering [[corticosteroids]], etc. | On [[Speculum|speculum examination]] typical curdy white discharge is present. Usually present in newborns or in patients with [[Immunodeficiency|deficient immunity]], administering [[corticosteroids]], etc. | ||
====Atrophic candidiasis:==== | ====Atrophic candidiasis:==== | ||
Appears as [[erythema]] | Appears as [[erythema]] or [[edema]] without the characteristic [[Plaques|white plaques]]. Usually, seen in patients with [[Dentures|dental dentures]].<ref name="pmid7936588">{{cite journal |vauthors=Lynch DP |title=Oral candidiasis. History, classification, and clinical presentation |journal=Oral Surg. Oral Med. Oral Pathol. |volume=78 |issue=2 |pages=189–93 |year=1994 |pmid=7936588 |doi= |url=}}</ref> | ||
====Chronic hyperplastic candidiasis (Candidal leukoplakia):==== | ====Chronic hyperplastic candidiasis (Candidal leukoplakia):==== | ||
Persistent tough, adherent, white lesions that are indistinguishable from other [[leukoplakia]] except through [[biopsy]]. | Persistent tough, adherent, white lesions that are indistinguishable from other [[leukoplakia]] except through [[biopsy]]. | ||
Seen more in smokers, patients with [[iron deficiency anemia]] or [[Cell mediated immunity|deficient cell mediated immunity]].<ref name="urlCHRONIC HYPERPLASTTC CANDIDIASIS—CANDIDAL LEUKOPLAKIA - CAWSON - 1968 - British Journal of Dermatology - Wiley Online Library">{{cite web |url=http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2133.1968.tb11899.x/full |title=CHRONIC HYPERPLASTTC CANDIDIASIS—CANDIDAL LEUKOPLAKIA - CAWSON - 1968 - British Journal of Dermatology - Wiley Online Library |format= |work= |accessdate=}}</ref><ref name="pmid7936588">{{cite journal |vauthors=Lynch DP |title=Oral candidiasis. History, classification, and clinical presentation |journal=Oral Surg. Oral Med. Oral Pathol. |volume=78 |issue=2 |pages=189–93 |year=1994 |pmid=7936588 |doi= |url=}}</ref> | Seen more in smokers, patients with [[iron deficiency anemia]] or [[Cell mediated immunity|deficient cell-mediated immunity]].<ref name="urlCHRONIC HYPERPLASTTC CANDIDIASIS—CANDIDAL LEUKOPLAKIA - CAWSON - 1968 - British Journal of Dermatology - Wiley Online Library">{{cite web |url=http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2133.1968.tb11899.x/full |title=CHRONIC HYPERPLASTTC CANDIDIASIS—CANDIDAL LEUKOPLAKIA - CAWSON - 1968 - British Journal of Dermatology - Wiley Online Library |format= |work= |accessdate=}}</ref><ref name="pmid7936588">{{cite journal |vauthors=Lynch DP |title=Oral candidiasis. History, classification, and clinical presentation |journal=Oral Surg. Oral Med. Oral Pathol. |volume=78 |issue=2 |pages=189–93 |year=1994 |pmid=7936588 |doi= |url=}}</ref> | ||
====Chronic mucocutaneous candidiasis (CMCC):==== | ====Chronic mucocutaneous candidiasis (CMCC):==== | ||
*[[Chronic mucocutaneous candidiasis|CMCC]] is a syndrome characterized by chronic or recurrent superficial candida infection in the skin and mucous membranes in association with [[Endocrinopathy|endocrinal]] and [[autoimmune diseases]].<ref name="pmid21350122">{{cite journal |vauthors=Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim HK, Migaud M, Israel L, Chrabieh M, Audry M, Gumbleton M, Toulon A, Bodemer C, El-Baghdadi J, Whitters M, Paradis T, Brooks J, Collins M, Wolfman NM, Al-Muhsen S, Galicchio M, Abel L, Picard C, Casanova JL |title=Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity |journal=Science |volume=332 |issue=6025 |pages=65–8 |year=2011 |pmid=21350122 |pmc=3070042 |doi=10.1126/science.1200439 |url=}}</ref> | *[[Chronic mucocutaneous candidiasis|CMCC]] is a syndrome characterized by chronic or recurrent superficial candida infection in the skin and mucous membranes in association with [[Endocrinopathy|endocrinal]] and [[autoimmune diseases]].<ref name="pmid21350122">{{cite journal |vauthors=Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim HK, Migaud M, Israel L, Chrabieh M, Audry M, Gumbleton M, Toulon A, Bodemer C, El-Baghdadi J, Whitters M, Paradis T, Brooks J, Collins M, Wolfman NM, Al-Muhsen S, Galicchio M, Abel L, Picard C, Casanova JL |title=Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity |journal=Science |volume=332 |issue=6025 |pages=65–8 |year=2011 |pmid=21350122 |pmc=3070042 |doi=10.1126/science.1200439 |url=}}</ref> | ||
*Characterized by inability of [[T cells]] to react to [[Antigens|candidal antigens]]. | *Characterized by the inability of [[T cells]] to react to [[Antigens|candidal antigens]]. | ||
*Presents with recurrent or chronic candidal infections. Infection is usually superficial though invasive candidiasis is encountered especially in [[Immunosuppression|immunocompromised patients]].<ref name="pmid18615114">{{cite journal |vauthors=Eyerich K, Foerster S, Rombold S, Seidl HP, Behrendt H, Hofmann H, Ring J, Traidl-Hoffmann C |title=Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22 |journal=J. Invest. Dermatol. |volume=128 |issue=11 |pages=2640–5 |year=2008 |pmid=18615114 |doi=10.1038/jid.2008.139 |url=}}</ref> | *Presents with recurrent or chronic candidal infections. Infection is usually superficial though invasive candidiasis is encountered especially in [[Immunosuppression|immunocompromised patients]].<ref name="pmid18615114">{{cite journal |vauthors=Eyerich K, Foerster S, Rombold S, Seidl HP, Behrendt H, Hofmann H, Ring J, Traidl-Hoffmann C |title=Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22 |journal=J. Invest. Dermatol. |volume=128 |issue=11 |pages=2640–5 |year=2008 |pmid=18615114 |doi=10.1038/jid.2008.139 |url=}}</ref> | ||
*[[Endocrinopathy|Endocrinopathies]] as [[hypoparathyroidism]] and [[adrenal insufficiency]] may accompany chronic candidiasis. | *[[Endocrinopathy|Endocrinopathies]] as [[hypoparathyroidism]] and [[adrenal insufficiency]] may accompany chronic candidiasis. | ||
| Line 59: | Line 55: | ||
|} | |} | ||
` | ` | ||
*Microscopic examination of the wet mount with 10% KOH or saline demonstrates [[hyphae]], pseudohyphae and [[Yeast|blastospores]]. | *Microscopic examination of the wet mount with 10% KOH or saline demonstrates [[hyphae]], pseudohyphae, and [[Yeast|blastospores]]. | ||
<br> | <br> | ||
<br> | <br> | ||
| Line 80: | Line 75: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Needs content]] | [[Category:Needs content]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Fungal diseases]] | [[Category:Fungal diseases]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Emergency mdicine]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Otolaryngology]] | ||
[[Category:Pediatrics]] | |||
[[Category:Immunology]] | |||
Latest revision as of 23:00, 29 July 2020
|
Oral candidiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral candidiasis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Oral candidiasis pathophysiology |
|
Risk calculators and risk factors for Oral candidiasis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Candida is a normal commensal of the skin and mucous membranes. The balance between the virulence of the fungus and the host immune defense is responsible avoiding opportunistic infection of candida. Deficiency of cell-mediated immunity or poor general status are the main risk factors for having opportunistic candidiasis. Candidiasis is usually localized to skin and mucous membranes. In rare cases, candidiasis can spread causing candidemia and distant infection. These cases are usually associated with deficient immunity . C. albicans is the main species causing infection in humans more than any other candida species.
Pathophysiology
Pathogenesis
Candida is a normal commensal of skin and mucous membranes. A competent immune system and an intact regenerating healthy skin prevent the virulence of Candida.
Candida Virulence factors
The main virulence factors that mediate the infection:[1]
- Secreting molecules that mediate adherence into host cells
- Production of hydrolases which has a lytic effect on tissues and facilitate the invasion by the fungus.
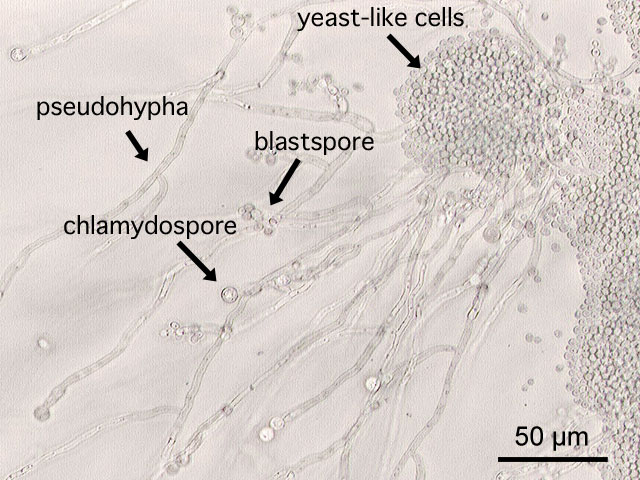
- Polymorphism: Candida has the ability to grow either as pseudohyphae (elongated ellipsoid form) or in a yeast form (rounded to oval budding form. While the role of polymorphism is not clearly understood in the virulence of Candida, it’s noted that the species that are capable of producing the most severe form of the disease has this ability.
- Biofilm production: which means the ability to form a thick layer of the organism on the mucosal surfaces or even on catheters and dentures.
Any condition that compromises cell-mediated immunity, worsens the general status of the patient or provide a favorable medium for Candida to form biofilms put the patient at increased risk for having candidiasis.[2]
Candidal gene VPS4 plays an important role in mucosal candidiasis specifically. Moreover, fungi with mutations affecting this gene were found to be less virulent.[3][4]
Gross Pathology
Pseudomembranous candidiasis:
On speculum examination typical curdy white discharge is present. Usually present in newborns or in patients with deficient immunity, administering corticosteroids, etc.
Atrophic candidiasis:
Appears as erythema or edema without the characteristic white plaques. Usually, seen in patients with dental dentures.[5]
Chronic hyperplastic candidiasis (Candidal leukoplakia):
Persistent tough, adherent, white lesions that are indistinguishable from other leukoplakia except through biopsy. Seen more in smokers, patients with iron deficiency anemia or deficient cell-mediated immunity.[6][5]
Chronic mucocutaneous candidiasis (CMCC):
- CMCC is a syndrome characterized by chronic or recurrent superficial candida infection in the skin and mucous membranes in association with endocrinal and autoimmune diseases.[7]
- Characterized by the inability of T cells to react to candidal antigens.
- Presents with recurrent or chronic candidal infections. Infection is usually superficial though invasive candidiasis is encountered especially in immunocompromised patients.[8]
- Endocrinopathies as hypoparathyroidism and adrenal insufficiency may accompany chronic candidiasis.
-
Oral manifestations of HIV infection and AIDS. Chronic oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Soft palate showing extensive oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Patient with swollen gingivae was diagnosed with oral moniliasis secondary to monocytic leukemia. From Public Health Image Library (PHIL). [9]
Microscopic pathology:
 |
`
- Microscopic examination of the wet mount with 10% KOH or saline demonstrates hyphae, pseudohyphae, and blastospores.
Videos
{{#ev:youtube|Qqb6vZtXxu8}}
References
- ↑ Mayer FL, Wilson D, Hube B (2013). "Candida albicans pathogenicity mechanisms". Virulence. 4 (2): 119–28. doi:10.4161/viru.22913. PMC 3654610. PMID 23302789.
- ↑ Pappas PG (2006). "Invasive candidiasis". Infect. Dis. Clin. North Am. 20 (3): 485–506. doi:10.1016/j.idc.2006.07.004. PMID 16984866.
- ↑ Rane HS, Hardison S, Botelho C, Bernardo SM, Wormley F, Lee SA (2014). "Candida albicans VPS4 contributes differentially to epithelial and mucosal pathogenesis". Virulence. 5 (8): 810–8. doi:10.4161/21505594.2014.956648. PMID 25483774.
- ↑ Lee SA, Jones J, Hardison S, Kot J, Khalique Z, Bernardo SM, Lazzell A, Monteagudo C, Lopez-Ribot J (2009). "Candida albicans VPS4 is required for secretion of aspartyl proteases and in vivo virulence". Mycopathologia. 167 (2): 55–63. doi:10.1007/s11046-008-9155-7. PMID 18814053.
- ↑ 5.0 5.1 Lynch DP (1994). "Oral candidiasis. History, classification, and clinical presentation". Oral Surg. Oral Med. Oral Pathol. 78 (2): 189–93. PMID 7936588.
- ↑ "CHRONIC HYPERPLASTTC CANDIDIASIS—CANDIDAL LEUKOPLAKIA - CAWSON - 1968 - British Journal of Dermatology - Wiley Online Library".
- ↑ Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim HK, Migaud M, Israel L, Chrabieh M, Audry M, Gumbleton M, Toulon A, Bodemer C, El-Baghdadi J, Whitters M, Paradis T, Brooks J, Collins M, Wolfman NM, Al-Muhsen S, Galicchio M, Abel L, Picard C, Casanova JL (2011). "Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity". Science. 332 (6025): 65–8. doi:10.1126/science.1200439. PMC 3070042. PMID 21350122.
- ↑ Eyerich K, Foerster S, Rombold S, Seidl HP, Behrendt H, Hofmann H, Ring J, Traidl-Hoffmann C (2008). "Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22". J. Invest. Dermatol. 128 (11): 2640–5. doi:10.1038/jid.2008.139. PMID 18615114.
- ↑ "Public Health Image Library (PHIL)".



![Patient with swollen gingivae was diagnosed with oral moniliasis secondary to monocytic leukemia. From Public Health Image Library (PHIL). [9]](/images/c/cb/Moniliasis03.jpeg)