Rivastigmine (transdermal)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Rivastigmine (transdermal) is a acetylcholinesterase inhibitor that is FDA approved for the treatment of mild to moderate dementia of the Alzheimer’s type and Parkinson’s Disease Dementia. Common adverse reactions include nausea, vomiting, anorexia, dyspepsia, and asthenia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Alzheimer’s Disease
- Rivastigmine (rivastigmine transdermal system) is indicated for the treatment of mild to moderate dementia of the Alzheimer’s type.
Parkinson’s Disease Dementia
- Rivastigmine (rivastigmine transdermal system) is indicated for the treatment of mild to moderate dementia associated with Parkinson’s disease.
- The dementia of Parkinson’s disease is purportedly characterized by impairments in executive function, memory retrieval, and attention in patients with an established diagnosis of Parkinson’s disease. The diagnosis of dementia of Parkinson’s disease can be made reliably in patients in whom a progressive dementia syndrome occurs (without the necessity to document the specific deficits described above) at least 2 years after a diagnosis of Parkinson’s disease has been made, and in whom other causes of dementia have been ruled out.
Dosing Information
Alzheimer’s Disease
Initial Dose
- Treatment is started with rivastigmine 4.6 mg/24 hours.
- After a minimum of four weeks of treatment and if well tolerated, this dose should be increased to rivastigmine 9.5 mg/24 hours, which is the recommended effective dose.
Maintenance Dose
- Dose increases should occur only after a minimum of 4 weeks at the previous dose, and only if the previous dose has been well tolerated. The maximum recommended dose is 9.5 mg/24 hours. Higher doses confer no appreciable additional benefit, and are associated with significant increase in the incidence of adverse events .
- If adverse effects (e.g., nausea, vomiting, diarrhea, loss of appetite) cause intolerance during treatment, the patient should be instructed to discontinue treatment for several days and then restart at the same or next lower dose level. If treatment is interrupted for longer than several days, treatment should be reinitiated with the lowest daily dose and titrated as described above .
Switching from Capsules or Oral Solution
- Patients treated with Exelon capsules or oral solution may be switched to rivastigmine as follows:
- A patient who is on a total daily dose of less than 6 mg of oral rivastigmine can be switched to rivastigmine 4.6 mg/24 hours.
- A patient who is on a total daily dose of 6-12 mg of oral rivastigmine may be directly switched to rivastigmine 9.5 mg/24 hours.
- It is recommended to apply the first patch on the day following the last oral dose.
Method of Administration
- Rivastigmine should be applied once a day to clean, dry, hairless, intact healthy skin in a place that will not be rubbed against by tight clothing. The upper or lower back is recommended as the site of application because the patch is less likely to be removed by the patient; however, when sites on the back are not accessible the patch can be applied to the upper arm or chest. The patch should not be applied to skin that is red, irritated, or cut. It is recommended that the site of patch application be changed daily to avoid potential irritation, although consecutive patches can be applied to the same anatomic site (e.g., another spot on the upper back).
- The patch should be pressed down firmly until the edges stick well. The patch can be used in situations that include bathing and hot weather.
- The patch should be replaced with a new one every 24 hours. Do not apply a new patch to that same spot for at least 14 days. Patients and caregivers should be instructed accordingly
Incompatibilities
- To prevent interference with the adhesive properties of the patch, the patch should not be applied to a skin area where cream, lotion or powder has recently been applied.
Special Populations
- Hepatic Impairment
- Dosage adjustment is not necessary in hepatically impaired patients, as the dose of drug is individually titrated to tolerability.
- Renal Impairment
- No dose adjustment is necessary for patients with renal impairment.
- Low Body Weight
- Patients with body weight below 50 kg may experience more adverse events and may be more likely to discontinue due to adverse events. Particular caution should be exercised in titrating these patients above the recommended maintenance dose of rivastigmine 9.5 mg/24 hours.
- Parkinson’s Disease Dementia
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Rivastigmine (transdermal) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Rivastigmine (transdermal) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Rivastigmine (transdermal) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Rivastigmine (transdermal) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Rivastigmine (transdermal) in pediatric patients.
Contraindications
- Hypersensitivity
- Rivastigmine (rivastigmine transdermal system) is contraindicated in patients with known hypersensitivity to rivastigmine, other carbamate derivatives, or other components of the formulation
Warnings
- Gastrointestinal Adverse Reactions
- At higher than recommended doses, rivastigmine (rivastigmine transdermal system) use is associated with significant gastrointestinal adverse reactions, including nausea, vomiting, diarrhea, anorexia/decreased appetite and weight loss. For this reason, patients administered rivastigmine should always be started at a dose of 4.6 mg/24 hours and titrated to the maintenance dose of 9.5 mg/24 hours. If treatment is interrupted for longer than several days, treatment should be reinitiated with the lowest daily dose to reduce the possibility of severe vomiting and its potentially serious sequelae (e.g., there has been one post-marketing report of severe vomiting with esophageal rupture following inappropriate reinitiation of treatment with a 4.5-mg dose of an oral formulation after 8 weeks of treatment interruption).
- At higher than recommended doses, caregivers should be advised of the high incidence of nausea and vomiting associated with the use of rivastigmine along with the possibility of anorexia and weight loss. Caregivers should be encouraged to monitor for these adverse events and inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than several days, the next dose should not be administered until they have discussed this with the physician.
- Nausea and Vomiting
- In the controlled clinical trial, 7% of patients treated with rivastigmine 9.5 mg/24 hours developed nausea, as compared to 23% of patients who received the Exelon capsule at doses up to 6 mg BID and 5% of those who received placebo. In the same clinical trial, 6% of patients treated with rivastigmine 9.5 mg/24 hours developed vomiting, as compared with 17% of patients who received the Exelon capsule at doses up to 6 mg BID and 3% of those who received placebo. The proportion of patients who discontinued treatment on account of vomiting was 0% of the patients who received rivastigmine 9.5 mg/24 hours as well as 2% of patients who received the Exelon capsule at doses up to 6 mg BID and 0% of those who received placebo. Vomiting was severe in 0% of patients who received rivastigmine 9.5 mg/24 hours and 1% of patients who received the Exelon capsule at doses up to 6 mg BID and 0% of those who received placebo.
- In the same clinical trial, 21% of patients treated with the higher dose of rivastigmine 17.4 mg/24 hours developed nausea, 19% developed vomiting, and the proportion of these patients who discontinued treatment on account of vomiting was 2%. Vomiting was severe in 1% of patients treated with rivastigmine 17.4 mg/24 hours.
- Weight Loss
- In the controlled clinical trial, the proportion of patients who had weight loss equal to or greater than 7% of their baseline weight was 8% of those treated with rivastigmine 9.5 mg/24 hours, 11% of patients who received the Exelon capsule at doses up to 6 mg BID and 6% of those who received placebo.
- Diarrhea
- In the controlled clinical trial, 6% of patients treated with rivastigmine 9.5 mg/24 hours developed diarrhea, as compared with 5% of patients who received the Exelon capsule at doses up to 6 mg BID, 10% of those treated with 17.4 mg/24 hours and 3% of those who received placebo.
- Anorexia/Decreased Appetite
- In the controlled clinical trial, 3% of patients treated with rivastigmine 9.5 mg/24 hours were recorded as developing decreased appetite or anorexia, as compared with 9% of patients who received the Exelon capsule at doses up to 6 mg BID, 9% of those treated with rivastigmine 17.4 mg/24 hours and 2% of those who received placebo.
- Peptic Ulcers/Gastrointestinal Bleeding
- Because of their pharmacological action, cholinesterase inhibitors may be expected to increase gastric acid secretion due to increased cholinergic activity. Therefore, patients should be monitored closely for symptoms of active or occult gastrointestinal bleeding, especially those at increased risk for developing ulcers, e.g., those with a history of ulcer disease or those receiving concurrent nonsteroidal anti-inflammatory drugs (NSAIDs). Clinical studies of Exelon have shown no significant increase, relative to placebo, in the incidence of either peptic ulcer disease or gastrointestinal bleeding.
- Anesthesia
- Exelon, as a cholinesterase inhibitor, is likely to exaggerate succinylcholine-type muscle relaxation during anesthesia.
- Cardiovascular Conditions
- Drugs that increase cholinergic activity may have vagotonic effects on heart rate (e.g., bradycardia). The potential for this action may be particularly important to patients with sick sinus syndrome or other supraventricular cardiac conduction conditions. In clinical trials, Exelon was not associated with any increased incidence of cardiovascular adverse events, heart rate or blood pressure changes, or ECG abnormalities.
- Genitourinary Conditions
- Although this was not observed in clinical trials of Exelon, drugs that increase cholinergic activity may cause urinary obstruction.
- Neurological Conditions
- Seizures
- Drugs that increase cholinergic activity are believed to have some potential for causing seizures. However, seizure activity also may be a manifestation of Alzheimer's disease.
- Extrapyramidal Symptoms
- Like other cholinomimetics, rivastigmine may exacerbate or induce extrapyramidal symptoms. Worsening of parkinsonian symptoms, particularly tremor, has been observed in patients with dementia associated with Parkinson’s disease who were treated with Exelon capsules.
- Pulmonary Conditions
- Like other drugs that increase cholinergic activity, Exelon should be used with care in patients with a history of asthma or obstructive pulmonary disease.
- Effects on Ability to Drive and Use Machines
- Dementia may cause gradual impairment of driving performance or compromise the ability to use machinery. The administration of rivastigmine may also result in adverse events that are detrimental to these functions. Thus, the ability to continue driving or operating machinery should be routinely evaluated by the treating physician.
- Special Populations
- Low Body Weight
- Patients with body weight below 50 kg may experience more adverse events and may be more likely to discontinue due to adverse events. Particular caution should be exercised in titrating these patients above the recommended maintenance dose of the rivastigmine 9.5 mg/24 hours.
- Low Body Weight
Adverse Reactions
Clinical Trials Experience
Significant gastrointestinal adverse reactions including nausea, vomiting, anorexia, and weight loss have been reported with the rivastigmine at higher than recommended doses .
- Incidence in Controlled Clinical Trial in Alzheimer’s Disease
- Associated with Discontinuation of Treatment
- In the single controlled clinical trial of rivastigmine , which randomized a total of 1195 patients, the proportions of patients in the rivastigmine 9.5 mg/24 hours, rivastigmine 17.4 mg/24 hours, Exelon capsules 6 mg BID, and placebo groups who discontinued treatment due to adverse events were 9.6%, 8.6%, 8.1%, and 5.0%, respectively.
- The most common adverse events in the rivastigmine-treated groups that led to treatment discontinuation in this study were nausea and vomiting. The proportions of patients who discontinued treatment due to nausea were 0.7%, 1.7%, 1.7%, and 1.3% in the rivastigmine 9.5 mg/24 hours, rivastigmine 17.4 mg/24 hours, Exelon capsules 6 mg BID, and placebo groups, respectively. The proportions of patients who discontinued treatment due to vomiting were 0%, 1.7%, 2.0%, and 0.3% in the rivastigmine 9.5 mg/24 hours, rivastigmine 17.4 mg/24 hours, Exelon capsules 6 mg BID, and placebo groups, respectively.
- Most Commonly Observed Adverse Events
- The most commonly observed adverse events seen in patients administered rivastigmine in the controlled clinical trial, defined as those occurring at a frequency of at least 5% in the 9.5 mg/24 hours group and at a frequency at least as high as in the placebo group are largely predicted by the cholinergic effects of Exelon. These are nausea, vomiting, and diarrhea. All these events were more common at the higher rivastigmine dose of 17.4 mg/24 hours than at a dose of 9.5 mg/24 hours.
- Adverse Events Observed at an incidence of ≥2%
- The following table lists treatment-emergent adverse events that were seen at an incidence of ≥2% in either rivastigmine-treated group in the controlled clinical trial and for which the rate of occurrence was greater for patients treated with that dose of rivastigmine than for those treated with placebo. The prescriber should be aware that these frequencies cannot be used to predict the frequency of adverse events in the course of usual medical practice when patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with frequencies obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescriber with one basis by which to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
- Incidence of Application Site Reactions
- The vast majority of patients participating in the controlled clinical trial had either no observed skin irritation or mild to moderate skin reactions. The incidence of severe reactions was very low regardless of administered dosage.
- Other Adverse Events Observed During Clinical Trials
- Rivastigmine has been administered to 1071 patients with Alzheimer’s disease during clinical trials worldwide. Of these, 869 patients have been treated for at least 3 months, 706 patients have been treated for at least 6 months, and 212 patients have been treated for 1 year.
- Treatment-emergent signs and symptoms that occurred during 1 controlled and 4 open-label trials in North America, Europe, Latin America, Asia and Japan were recorded as adverse events by the clinical investigators using terminology of their own choosing.
- To provide an overall estimate of the proportion of individuals having similar types of events, the events were grouped into a smaller number of standardized categories using the MedDRA dictionary, and event frequencies were calculated across all studies. These categories are used in the listing below. The frequencies represent the proportion of 1071 patients from these trials who experienced that event while receiving rivastigmine. All patch doses are pooled.
- All adverse events occurring in at least 1 patient (approximately 0.1%) are included, except for those already listed elsewhere in labeling, too general to be informative, or relatively minor events.
- Events are classified by system organ class and listed using the following definitions: Frequent – those occurring in at least 1/100 patients; Infrequent – those occurring in 1/100 to 1/1,000 patients. These adverse events are not necessarily related to rivastigmine treatment and in most cases were observed at a similar frequency in placebo-treated patients in the controlled studies.
- Blood and Lymphatic System Disorders: Frequent : Anemia.
- Cardiac Disorders: Infrequent : Angina pectoris, cardiac failure, bradycardia, atrial fibrillation, supraventricular extrasystoles, myocardial infarction, tachycardia, arrhythmia, atrioventricular block.
- Ear and Labyrinth Disorders: Infrequent : Tinnitus.
- Eye Disorders: Infrequent : Cataract, glaucoma, vision blurred.
- Gastrointestinal System: Frequent : Constipation, gastritis. Infrequent : Gastroesophageal reflux disease, hematochezia, peptic ulcer, hematemesis, pancreatitis, salivary hypersecretion.
- General Disorders and Administration Site Conditions: Infrequent : Application site dermatitis, application site irritation, peripheral edema, chest pain, application site eczema, hyperpyrexia.
- Hepatobiliary Disorders: Infrequent : Cholecystitis.
- Infections and Infestations: Frequent : Nasopharyngitis, pneumonia. Infrequent : Diverticulitis.
- Injury, Poisoning and Procedural Complications: Frequent : Fall. Infrequent : Hip fracture, subdural hematoma.
- Investigations: Infrequent : Blood creatine phosphokinase increased, lipase increased, blood amylase increased, electrocardiogram QT prolonged.
- Metabolic and Nutritional Disorders: Frequent : Dehydration Infrequent : Hyperlipidemia, hypokalemia, hyponatremia.
- Musculoskeletal and Connective Tissue Disorders: Infrequent: Arthralgia, muscle spasms, myalgia.
- Nervous System Disorders: Frequent : Tremor. Infrequent : Migraine, parkinsonism, epilepsy.
- Psychiatric Disorders: Infrequent : Delusion.
- Renal and Urinary Disorders: Frequent : Urinary incontinence. Infrequent : Pollakiuria, hematuria, nocturia, renal failure.
- Reproductive System and Breast Disorders: Infrequent : Benign prostatic hyperplasia.
- Respiratory, Thoracic, and Mediastinal Disorders: Infrequent : Dyspnea, bronchospasm, chronic obstructive pulmonary disease.
- Skin and Subcutaneous Tissue Disorders: Frequent : Pruritus. Infrequent : Erythema, eczema, dermatitis, rash erythematous, skin ulcer.
- Vascular Disorders: Infrequent : Hypotension.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Rivastigmine (transdermal) in the drug label.
Drug Interactions
No specific interaction studies have been conducted with rivastigmine (rivastigmine transdermal system).
- Effect of Exelon on the Metabolism of Other Drugs
- Rivastigmine is primarily metabolized through hydrolysis by esterases. Minimal metabolism occurs via the major cytochrome P450 isoenzymes. Based on in-vitro studies, no pharmacokinetic drug interactions with drugs metabolized by the following isoenzyme systems are expected: CYP1A2, CYP2D6, CYP3A4/5, CYP2E1, CYP2C9, CYP2C8, or CYP2C19.
- No pharmacokinetic interaction was observed between rivastigmine taken orally and digoxin, warfarin, diazepam or fluoxetine in studies in healthy volunteers. The increase in prothrombin time induced by warfarin is not affected by administration of rivastigmine.
- Effect of Other Drugs on the Metabolism of Exelon
- Drugs that induce or inhibit CYP450 metabolism are not expected to alter the metabolism of rivastigmine.
- Population PK analysis with a database of 625 patients showed that the pharmacokinetics of rivastigmine taken orally were not influenced by commonly prescribed medications such as antacids (n=77), antihypertensives (n=72), ß-blockers (n=42), calcium channel blockers (n=75), antidiabetics (n=21), nonsteroidal anti-inflammatory drugs (n=79), estrogens (n=70), salicylate analgesics (n=177), antianginals (n=35) and antihistamines (n=15).
- Use with Anticholinergics,Cholinomimetics and Other Cholinesterase Inhibitors
- In view of its pharmacodynamic effects, rivastigmine should not be given concomitantly with other cholinomimetic drugs and might interfere with the activity of anticholinergic medications. A synergistic effect may be expected when cholinesterase inhibitors are given concurrently with succinylcholine, similar neuromuscular blocking agents or cholinergic agonists such as bethanechol.
Use in Specific Populations
Pregnancy
- There are no adequate or well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, rivastigmine should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus. No dermal reproduction studies in animals have been conducted. Oral reproduction studies conducted in pregnant rats at doses up to 2.3 mg base/kg/day and in pregnant rabbits at doses up to 2.3 mg base/kg/day revealed no evidence of teratogenicity. Studies in rats showed slightly decreased fetal/pup weights, usually at doses causing some maternal toxicity.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Rivastigmine (transdermal) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Rivastigmine (transdermal) during labor and delivery.
Nursing Mothers
- Milk transfer studies in animals have not been conducted with dermal rivastigmine. In rats given rivastigmine orally, concentrations of rivastigmine plus metabolites were approximately two times higher in milk than in plasma. It is not known whether rivastigmine is excreted in human breast milk. rivastigmine (rivastigmine transdermal system) has no indication for use in nursing mothers.
Pediatric Use
- There are no adequate and well-controlled trials documenting the safety and efficacy of Exelon in any illness occurring in children.
Geriatic Use
- Age had no impact on the exposure to rivastigmine in Alzheimer’s disease patients treated with rivastigmine.
Gender
- No specific pharmacokinetic study was conducted to investigate the effect of gender and race on the disposition of Exelon, but a population pharmacokinetic analysis indicates that gender (n=277 males and 348 females) and race (n=575 White, 34 Black, 4 Asian, and 12 Other) did not affect the clearance of Exelon administered orally. Similar results were seen with analyses of pharmacokinetic data obtained after the administration of rivastigmine.
Race
There is no FDA guidance on the use of Rivastigmine (transdermal) with respect to specific racial populations.
Renal Impairment
- No study was conducted with rivastigmine in subjects with renal impairment. Following a single 3-mg dose, mean oral clearance of rivastigmine is 64% lower in moderately impaired renal patients (n=8, GFR=10-50 mL/min) than in healthy subjects (n=10, GFR greater than or equal to 60 mL/min); Cl/F=1.7 L/min (cv=45%) and 4.8 L/min (cv=80%), respectively. In severely impaired renal patients (n=8, GFR less than 10 mL/min), mean oral clearance of rivastigmine is 43% higher than in healthy subjects (n=10, GFR greater than or equal to 60 mL/min); Cl/F=6.9 L/min and 4.8 L/min, respectively. For unexplained reasons, the severely impaired renal patients had a higher clearance of rivastigmine than moderately impaired patients. However, dosage adjustment may not be necessary in renally impaired patients as the dose of the drug is individually titrated to tolerability.
Hepatic Impairment
- No pharmacokinetic study was conducted with rivastigmine in subjects with hepatic impairment. Following a single 3-mg dose, mean oral clearance of rivastigmine was 60% lower in hepatically impaired patients (n=10, biopsy proven) than in healthy subjects (n=10). After multiple 6-mg BID oral dosing, the mean clearance of rivastigmine was 65% lower in mild (n=7, Child-Pugh score 5-6) and moderate (n=3, Child-Pugh score 7-9) hepatically impaired patients (biopsy proven, liver cirrhosis) than in healthy subjects (n=10). Dosage adjustment is not necessary in hepatically impaired patients as the dose of drug is individually titrated to tolerability.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Rivastigmine (transdermal) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Rivastigmine (transdermal) in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
There is limited information regarding Monitoring of Rivastigmine (transdermal) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Rivastigmine (transdermal) in the drug label.
Overdosage
- Because strategies for the management of overdose are continually evolving, it is advisable to contact a Poison Control Center to determine the latest recommendations for the management of an overdose of any drug. As in any case of overdose, general supportive measures should be utilized.
- As rivastigmine has a plasma half-life of about 3.4 hours after patch administration and a duration of acetylcholinesterase inhibition of about 9 hours, it is recommended that in cases of asymptomatic overdose the patch should be immediately removed and no further patch should be applied for the next 24 hours.
- As in any case of overdose, general supportive measures should be utilized. Overdosage with cholinesterase inhibitors can result in cholinergic crisis characterized by severe nausea, vomiting, salivation, sweating, bradycardia, hypotension, respiratory depression, collapse and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved. Atypical responses in blood pressure and heart rate have been reported with other drugs that increase cholinergic activity when coadministered with quaternary anticholinergics such as glycopyrrolate. Due to the short plasma elimination half-life of rivastigmine after patch administration, dialysis (hemodialysis, peritoneal dialysis, or hemofiltration) would not be clinically indicated in the event of an overdose.
- In overdose accompanied by severe nausea and vomiting, the use of antiemetics should be considered. In a documented case of an oral 46-mg overdose with Exelon, the patient experienced vomiting, incontinence, hypertension, psychomotor retardation, and loss of consciousness. The patient fully recovered within 24 hours and conservative management was all that was required for treatment.
- There are currently no data on overdose with rivastigmine (rivastigmine transdermal system).
Pharmacology
| |
| |
Rivastigmine (transdermal)
| |
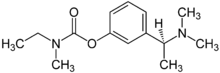
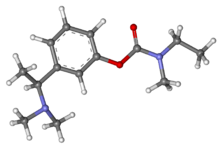
| Systematic (IUPAC) name | |
| (S)-3-[1-(dimethylamino)ethyl]phenyl N-ethyl-N-methylcarbamate | |
| Identifiers | |
| CAS number | |
| ATC code | N06 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 250.337 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 60 to 72% |
| Protein binding | 40% |
| Metabolism | Hepatic, via pseudocholinesterase |
| Half life | 1.5 hours |
| Excretion | Renal, 97% |
| Therapeutic considerations | |
| Pregnancy cat. |
B(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral, Transdermal |
Mechanism of Action
- Pathological changes in dementia of the Alzheimer’s type and dementia associated with Parkinson’s disease involve cholinergic neuronal pathways that project from the basal forebrain to the cerebral cortex and hippocampus. These pathways are thought to be intricately involved in memory, attention, learning, and other cognitive processes. While the precise mechanism of action for rivastigmine is unknown, it is postulated to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine through reversible inhibition of its hydrolysis by cholinesterase. If this proposed mechanism is correct, the effect of rivastigmine may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that rivastigmine alters the course of the underlying dementing process.
Structure
- rivastigmine (rivastigmine transdermal system) is a reversible cholinesterase inhibitor and is known chemically as (S)- 3-[1-(dimethylamino) ethyl]phenyl ethylmethylcarbamate. It has an empirical formula of C14H22N2O2 as the base and a molecular weight of 250.34 (as the base). Rivastigmine is a viscous, clear, and colorless to yellow to very slightly brown liquid that is sparingly soluble in water and very soluble in ethanol, acetonitrile, n-octanol and ethyl acetate.
- The distribution coefficient at 37°C in n-octanol/phosphate buffer solution pH 7 is 4.27.
- rivastigmine is for transdermal administration. The patch comprises a four-layer laminate containing the backing layer, drug matrix, adhesive matrix and overlapping release liner. *The release liner is removed and discarded prior to use. See Figure 1 for a detailed illustration.
- Excipients within the formulation include acrylic copolymer, poly(butylmethacrylate, methylmethacrylate), silicone adhesive applied to a flexible polymer backing film, silicone oil, and vitamin E.
Pharmacodynamics
- After a 6-mg oral dose of rivastigmine in humans, anticholinesterase activity is present in CSF for about 10 hours, with a maximum inhibition of about 60% 5 hours after dosing.
- In-vitro and in-vivo studies demonstrate that the inhibition of cholinesterase by rivastigmine is not affected by the concomitant administration of memantine, an N-methyl-D-aspartate receptor antagonist.
Pharmacokinetics
- Absorption
- After the first dose, there is a lag time of 0.5-1 hour in the absorption of rivastigmine from rivastigmine (rivastigmine transdermal system). Concentrations then rise slowly typically reaching a maximum after 8 hours, although maximum values (Cmax) are often reached at later times as well (10-16 hours). After the peak, plasma concentrations slowly decrease over the remainder of the 24-hour period of application. At steady state, trough levels are approximately 60-80% of peak levels. Fluctuation (between Cmax and Cmin) is lower for rivastigmine than for the oral formulation. rivastigmine 9.5 mg/24 hours exhibited exposure approximately the same as that provided by an oral

This image is provided by the National Library of Medicine. - Inter-subject variability in exposure was lower (43-49%) for the rivastigmine formulation as compared with the oral formulations (73-103%).
- A relationship between drug exposure at steady state (rivastigmine and metabolite NAP226-90) and bodyweight was observed in Alzheimer’s dementia patients. Compared to a patient with a body weight of 65 kg, the rivastigmine steady-state concentrations in a patient with a body weight of 35 kg are approximately doubled, while for a patient with a body weight of 100 kg the concentrations are approximately halved. The effect of body weight on drug exposure suggests special attention to patients with very low body weight during up-titration
- Over a 24-hour dermal application, approximately 50% of the drug load is released from the system.
- Exposure (AUC∞) to rivastigmine (and metabolite NAP266-90) was highest when the patch was applied to the upper back, chest, or upper arm. Two other sites (abdomen and thigh) could be used if none of the three other sites is available, but the practitioner should keep in mind that the rivastigmine plasma exposure associated with these sites was approximately 20-30% lower.
- There was no relevant accumulation of rivastigmine or the metabolite NAP226-90 in plasma in patients with Alzheimer’s disease upon multiple dosing.
- Distribution
- Rivastigmine is weakly bound to plasma proteins (approximately 40%) over the therapeutic range. It readily crosses the blood-brain barrier, reaching CSF peak concentrations in 1.4-2.6 hours. It has an apparent volume of distribution in the range of 1.8-2.7 L/kg.
- Metabolism
- Rivastigmine is extensively metabolized primarily via cholinesterase-mediated hydrolysis to the decarbamylated metabolite NAP226-90. In vitro, this metabolite shows minimal inhibition of acetylcholinesterase (less than 10%). Based on evidence from in-vitro and animal studies, the major cytochrome P450 isoenzymes are minimally involved in rivastigmine metabolism.
- The metabolite-to-parent AUC∞ ratio was about 0.7 after rivastigmine application versus 3.5 after oral administration, indicating that much less metabolism occurred after dermal treatment. Less NAP226-90 is formed following patch application, presumably because of the lack of presystemic (hepatic first pass) metabolism. Based on in-vitro studies, no unique metabolic routes were detected in human skin.
- Elimination
- Renal excretion of the metabolites is the major route of elimination. Unchanged rivastigmine is found in trace amounts in the urine. Following administration of 14C-rivastigmine, renal elimination was rapid and essentially complete (greater than 90%) within 24 hours. Less than 1% of the administered dose is excreted in the feces. The apparent eliminatio
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- In oral carcinogenicity studies conducted at doses up to 1.1 mg base/kg/day in rats and 1.6 mg base/kg/day in mice, rivastigmine was not carcinogenic.
- In a dermal carcinogenicity study conducted at doses up to 0.75 mg base/kg/day in mice, rivastigmine was not carcinogenic. The mean rivastigmine plasma exposure (AUC) at this dose was 0.3-0.4 times that observed in Alzheimer’s disease patients at the recommended clinical dose (one rivastigmine 9.5 mg/24 hours).
- Rivastigmine was clastogenic in two in-vitro assays in the presence, but not the absence, of metabolic activation. It caused structural chromosomal aberrations in V79 Chinese hamster lung cells and both structural and numerical (polyploidy) chromosomal aberrations in human peripheral blood lymphocytes. Rivastigmine was not genotoxic in three in-vitro assays: the Ames test, the unscheduled DNA synthesis (UDS) test in rat hepatocytes (a test for induction of DNA repair synthesis), and the HGPRT test in V79 Chinese hamster cells. Rivastigmine was not clastogenic in the in-vivo mouse micronucleus test.
- No fertility or reproduction studies have been conducted in animals treated with dermal rivastigmine. Rivastigmine had no effect on fertility or reproductive performance in rats at oral doses up to 1.1 mg base/kg/day.
Clinical Studies
- The effectiveness of the rivastigmine (rivastigmine transdermal system) in Alzheimer’s disease and dementia associated with Parkinson’s disease was based on the results of a single controlled trial in patients with Alzheimer’s disease (see below) as well as on three controlled trials of the immediate-release capsule in Alzheimer’s disease and one controlled trial in dementia associated with Parkinson’s disease (see package insert for the Exelon capsules and oral solution for details).
- International 24-Week Study of rivastigmine (rivastigmine transdermal system)
- This was a randomized double-blind clinical investigation in patients with Alzheimer’s disease [diagnosed by NINCDS-ADRDA and DSM-IV criteria, Mini-Mental Status Examination (MMSE) score ≥10 and ≤20]. The mean age of patients participating in this trial was 74 years with a range of 50-90 years. Approximately 67% of patients were women and 33% were men. The racial distribution was Caucasian 75%, Black 1%, Oriental 9% and Other Races 15%.
- Study Outcome Measures
- The effectiveness of the rivastigmine (rivastigmine transdermal system) was evaluated in this study using a dual outcome assessment strategy.
- The ability of the rivastigmine to improve cognitive performance was assessed with the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-Cog), a multi-item instrument that has been extensively validated in longitudinal cohorts of Alzheimer’s disease patients. The ADAS-Cog examines selected aspects of cognitive performance including elements of memory, orientation, attention, reasoning, language and praxis. The ADAS-Cog scoring range is from 0-70, with higher scores indicating greater cognitive impairment. Elderly normal adults may score as low as 0 or 1, but it is not unusual for non-demented adults to score slightly higher.
- The ability of the rivastigmine to produce an overall clinical effect was assessed using the Alzheimer’s Disease Cooperative Study - Clinical Global Impression of Change (ADCS-CGIC). The ADCS-CGIC is a more standardized form of CIBIC-Plus and is also scored as a seven-point categorical rating, ranging from a score of 1, indicating “markedly improved”, to a score of 4, indicating “no change” to a score of 7, indicating “marked worsening”.
- Study Results
- In this study, 1195 patients were randomized to one of the following 4 treatments: rivastigmine 9.5 mg/24 hours, rivastigmine 17.4 mg/24 hours, Exelon capsules in a dose of 6 mg BID, or placebo. This 24-week study was divided into a 16-week titration phase followed by an 8-week maintenance phase. In the active treatment arms of this study, doses below the target dose were permitted during the maintenance phase in the event of poor tolerability.
- Effects on the ADAS-Cog
- Figure 3 illustrates the time course for the change from baseline in ADAS-Cog scores for all 4 treatment groups over the 24-week study. At 24 weeks, the mean differences in the ADAS-Cog change scores for the Exelon-treated patients, compared to the patients on placebo, were 1.8, 2.9, and 1.8 units for the rivastigmine 9.5 mg/24 hours, rivastigmine 17.4 mg/24 hours, and Exelon capsule 6 mg BID groups, respectively. The difference between each of these groups and placebo was statistically significant.
- Effects on the ADCS-CGIC
- Figure 4 is a histogram of the distribution of patients’ scores on the ADCS-CGIC for all 4 treatment groups.
- At 24 weeks, the mean difference in the ADCS-CGIC scores for the comparison of patients in each of the Exelon-treated groups with the patients on placebo was 0.2 units. The difference between each of these groups and placebo was statistically significant.

This image is provided by the National Library of Medicine.
.
How Supplied
- Patch 4.6 mg/24 hours
- Each patch of 5 cm2 contains 9 mg rivastigmine base with in-vivo release rate of 4.6 mg/24 hours.
- Carton of 30………………………NDC 21695-357-30*Store at 25°C (77°F); excursions permitted to 15-30°C
(59-86°F) [see USP Controlled Room Temperature].
- Keep rivastigmine (rivastigmine transdermal system) in the individual sealed pouch until use.
- Used systems should be folded, with the adhesive surfaces pressed together, and discarded safely.
- Each pouch contains one patch.
Storage
There is limited information regarding Rivastigmine (transdermal) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Rivastigmine (transdermal) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Rivastigmine (transdermal) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- General
- Patient information is printed in section 17.8. To assure safe and effective use of rivastigmine, this information and instructions provided in the patient information section should be discussed with patients.
- Importance of Correct Usage
- Patients or caregivers should be informed of the importance of applying the correct dose on the correct part of their body. They should be instructed to rotate the application site in order to minimize skin irritation. The same site should not be used within 14 days. rivastigmine should be replaced every 24 hours and the time of day should be consistent. It may be helpful for this to be part of a daily routine, such as the daily bath or shower.
- Patients or caregivers should be told to avoid exposure of the patch to external heat sources (excess sunlight, saunas, solariums) for long periods of time.
- Discarding Used Patches
- Patients or caregivers should be instructed to fold the patch in half after use. Return the used patch to its original pouch and discard it out of the reach and sight of children and pets. They should also be informed that drug still remains in the patch after 24-hour usage. They should be instructed to avoid eye contact and to wash their hands after handling the patch.
- Concomitant Use of Drugs with Cholinergic Action
- Patients or caregivers should be told that while wearing rivastigmine they should not be taking Exelon capsules or Exelon oral solution or other drugs with cholinergic effects.
- Gastrointestinal Adverse Events
- Patients or caregivers should be informed of the potential gastrointestinal adverse events such as nausea, vomiting and diarrhea. Patients and caregivers should be instructed to observe for these adverse reactions at all times, in particular when treatment is initiated or the dose is increased. Patients and caregivers should be instructed to inform their physician if these adverse events persist as a dose adjustment/
reduction may be required.
- Monitoring the Patient’s Weight
- Patients or caregivers should be informed that rivastigmine may affect the patient’s appetite and/or the patient’s weight. Any loss of appetite or weight reduction needs to be monitored.
- Missed Doses
- If the patient has missed a dose, he/she should be instructed to apply a new patch immediately. They may apply the next patch at the usual time the next day. Patients should not apply two patches to make up for one missed.
- If treatment has been missed for several days, the patient or caregiver should be informed to restart treatment with the starting patch dose of 4.6 mg/24 hours. Titration to the next patch dose should proceed after 4 weeks
Precautions with Alcohol
- Alcohol-Rivastigmine (transdermal) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Exelon
Look-Alike Drug Names
There is limited information regarding Rivastigmine (transdermal) Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Rivastigmine (transdermal) |Label Name=Rivastigmine (transdermal)07.png
}}
{{#subobject:
|Label Page=Rivastigmine (transdermal) |Label Name=Rivastigmine (transdermal)08.png
}}


