Meperidine (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Meperidine (injection) is an analgesic that is FDA approved for the treatment of moderate to severe pain and for preoperative medication, support of anesthesia and obstetrical analgesia. Common adverse reactions include lightheadedness, dizziness, sedation, nausea, vomiting, headache, agitation and tremor.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- For the relief of moderate to severe pain
- For preoperative medication
- For support of anesthesia
- For obstetrical analgesia
Dosage
For Relief of Pain
- Dosage should be adjusted according to the severity of the pain and the response of the patient. While subcutaneous administration is suitable for occasional use, intramuscular administration is preferred when repeated doses are required. If intravenous administration is required, dosage should be decreased and the injection made very slowly, preferably utilizing a diluted solution. The dose of DEMEROL should be proportionately reduced (usually by 25 to 50 percent) when administered concomitantly with phenothiazines and many other tranquilizers since they potentiate the action of DEMEROL.
- The usual dosage is 50 mg to 150 mg intramuscularly or subcutaneously every 3 or 4 hours as necessary. Elderly patients should usually be given meperidine at the lower end of the dose range and observed closely.
For Preoperative Medication
- The usual dosage is 50 mg to 100 mg intramuscularly or subcutaneously, 30 to 90 minutes before the beginning of anesthesia. Elderly patients should usually be given meperidine at the lower end of the dose range and observed closely.
For Support of Anesthesia
- Repeated slow intravenous injections of fractional doses (e.g., 10 mg/mL) or continuous intravenous infusion of a more dilute solution (e.g., 1 mg/mL) should be used. The dose should be titrated to the needs of the patient and will depend on the premedication and type of anesthesia being employed, the characteristics of the particular patient, and the nature and duration of the operative procedure. Elderly patients should usually be given meperidine at the lower end of the dose range and observed closely.
For Obstetrical Analgesia
- The usual dosage is 50 mg to 100 mg intramuscularly or subcutaneously when pain becomes regular, and may be repeated at 1- to 3-hour intervals.
- Parenteral drug products should be inspected visually for particulate and discoloration prior to administration whenever solution and container permit.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Meperidine (injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Meperidine (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Meperidine (injection) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Meperidine (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Meperidine (injection) in pediatric patients.
Contraindications
Hypersensitivity to meperidine.
- Meperidine is contraindicated in patients who are receiving monoamine oxidase (MAO) inhibitors or those who have recently received such agents. Therapeutic doses of meperidine have occasionally precipitated unpredictable, severe, and occasionally fatal reactions in patients who have received such agents within 14 days. The mechanism of these reactions is unclear, but may be related to a preexisting hyperphenylalaninemia. Some have been characterized by coma, severe respiratory depression, cyanosis, and hypotension, and have resembled the syndrome of acute narcotic overdose. Serotonin syndrome with agitation, hyperthermia, diarrhea, tachycardia, sweating, tremors and impaired consciousness may also occur. In other reactions the predominant manifestations have been hyperexcitability, convulsions, tachycardia, hyperpyrexia, and hypertension. Although it is not known that other narcotics are free of the risk of such reactions, virtually all of the reported reactions have occurred with meperidine. If a narcotic is needed in such patients, a sensitivity test should be performed in which repeated, small, incremental doses of morphine are administered over the course of several hours while the patient’s condition and vital signs are under careful observation. (Intravenous hydrocortisone or prednisolone have been used to treat severe reactions, with the addition of intravenous chlorpromazine in those cases exhibiting hypertension and hyperpyrexia. The usefulness and safety of narcotic antagonists in the treatment of these reactions is unknown.)
- Solutions of DEMEROL and barbiturates are chemically incompatible.
- Demerol is contraindicated in patients with severe respiratory insufficiency.
Warnings
- Prolonged meperidine use may increase the risk of toxicity (e.g., seizures) from the accumulation of the meperidine metabolite, normeperidine.
Drug Dependence
- Meperidine can produce drug dependence of the morphine type and therefore has the potential for being abused. Psychic dependence, physical dependence, and tolerance may develop upon repeated administration of meperidine, and it should be prescribed and administered with the same degree of caution appropriate to the use of morphine. Like other narcotics, meperidine is subject to the provisions of the Federal narcotic laws.
Head Injury and Increased Intracranial Pressure
- The respiratory depressant effects of meperidine and its capacity to elevate cerebrospinal fluid pressure may be markedly exaggerated in the presence of head injury, other intracranial lesions, or a preexisting increase in intracranial pressure. Furthermore, narcotics produce adverse reactions which may obscure the clinical course of patients with head injuries. In such patients, meperidine must be used with extreme caution and only if its use is deemed essential.
Intravenous Use
- If necessary, meperidine may be given intravenously, but the injection should be given very slowly, preferably in the form of a diluted solution. Rapid intravenous injection of narcotic analgesics, including meperidine, increases the incidence of adverse reactions; severe respiratory depression, apnea, hypotension, peripheral circulatory collapse, and cardiac arrest have occurred. Meperidine should not be administered intravenously unless a narcotic antagonist and the facilities for assisted or controlled respiration are immediately available. When meperidine is given parenterally, especially intravenously, the patient should be lying down.
Asthma and Other Respiratory Conditions
- Meperidine should be used with extreme caution in patients having an acute asthmatic attack, patients with chronic obstructive pulmonary disease or cor pulmonale, patients having a substantially decreased respiratory reserve, and patients with preexisting respiratory depression, hypoxia, or hypercapnia. In such patients, even usual therapeutic doses of narcotics may decrease respiratory drive while simultaneously increasing airway resistance to the point of apnea.
Hypotensive Effect
- The administration of meperidine may result in severe hypotension in the postoperative patient or any individual whose ability to maintain blood pressure has been compromised by a depleted blood volume or the administration of drugs such as the phenothiazines or certain anesthetics.
Usage in Ambulatory Patients
- Meperidine may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. The patient should be cautioned accordingly.
- Meperidine, like other narcotics, may produce orthostatic hypotension in ambulatory patients.
Usage in Pregnancy
- Meperidine should not be used in pregnant women prior to the labor period, unless in the judgment of the physician the potential benefits outweigh the possible risks, because safe use in pregnancy prior to labor has not been established relative to possible adverse effects on fetal development.
Labor and Delivery
- When used as an obstetrical analgesic, meperidine crosses the placental barrier and can produce depression of respiration and psychophysiologic functions in the newborn. Resuscitation may be required. Therefore meperidine is not recommended during labor.
- Meperidine appears in the milk of nursing mothers receiving the drug. Due to the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the potential benefits of the drug to the nursing woman.
Precautions
- As with all intramuscular preparations, DEMEROL intramuscular injection should be injected well within the body of a large muscle.
General
- Opioid analgesics can have a narrow therapeutic index in certain patient populations, particularly when combined with CNS depressant drugs. The use of these products should be reserved for cases where the benefits of opioid analgesia outweigh the known risks of respiratory depression, altered mental state, and postural hypotension.
- Use of Demerol may be associated with increased potential risks and should be used with caution in the following conditions: sickle cell anemia, pheochromocytoma, acute alcoholism; adrenocortical insufficiency (e.g., Addison’s disease); CNS depression or coma; delirium tremens; debilitated patients; kyphoscoliosis associated with respiratory depression; myxedema or hypothyroidism; prostatic hypertrophy or urethral stricture; severe impairment of hepatic, pulmonary, or renal function; and toxic psychosis.
- The administration of meperidine may obscure the diagnosis or clinical course in patients with acute abdominal conditions. All opioids may induce or aggravate seizures in some clinical settings.
Interactions with Other CNS Depressants
- Meperidine should be used with caution and consideration should be given to starting with a reduced dosage in patients who are concurrently receiving other central nervous system depressants including sedatives or hypnotics, general anesthetics, phenothiazines, other tranquilizers, and alcohol. Drug-drug interactions may result in respiratory depression, hypotension, profound sedation, coma, or death if these drugs are taken in combination with the usual doses of Demerol.
Interactions with Mixed Agonist/Antagonist Opioid Analgesics
- Agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, butorphanol, and buprenorphine) should be administered with caution to a patient who has received or is receiving a course of therapy with a pure opioid agonist analgesic such as meperidine. In this situation, mixed agonist/antagonist analgesics may reduce the analgesic effect of meperidine and/or may precipitate withdrawal symptoms in these patients due to competitive blocking of receptors.
Supraventricular Tachycardias
- Meperidine should be used with caution in patients with atrial flutter and other supraventricular tachycardias because of a possible vagolytic action which may produce a significant increase in the ventricular response rate.
Convulsions
- Meperidine may aggravate preexisting convulsions in patients with convulsive disorders. If dosage is escalated substantially above recommended levels because of tolerance development, convulsions may occur in individuals without a history of convulsive disorders.
Acute Abdominal Conditions
- The administration of meperidine or other narcotics may obscure the diagnosis or clinical course in patients with acute abdominal conditions.
Tolerance and Physical Dependence
- Meperidine has the potential to produce tolerance and drug dependence. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Physical dependence and tolerance are not unusual during chronic opioid therapy.
- The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, mydriasis. Other symptoms also may develop, including: irritability, anxiety, backache' joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
- In general, opioids used regularly should not be abruptly discontinued.
Adverse Reactions
Clinical Trials Experience
- The major hazards of meperidine, as with other narcotic analgesics, are respiratory depression and, to a lesser degree, circulatory depression; respiratory arrest, shock, and cardiac arrest have occurred.
- The most frequently observed adverse reactions include lightheadedness, dizziness, sedation, nausea, vomiting, and sweating. These effects seem to be more prominent in ambulatory patients and in those who are not experiencing severe pain. In such individuals, lower doses are advisable. Some adverse reactions in ambulatory patients may be alleviated if the patient lies down.
- Other adverse reactions include:
- Nervous System. Mood changes (e.g. euphoria, dysphoria), weakness, headache, agitation, tremor, involuntary muscle movements (e.g. muscle twitches, myoclonus), severe convulsions, transient hallucinations and disorientation, confusion, delirium, visual disturbances. Inadvertent injection about a nerve trunk may result in sensory-motor paralysis which is usually, though not always, transitory.
- Gastrointestinal. Dry mouth, constipation, biliary tract spasm.
- Cardiovascular. Flushing of the face, tachycardia, bradycardia, palpitation, hypotension , syncope, phlebitis following intravenous injection.
- Genitourinary. Urinary retention.
- Allergic. Pruritus, urticaria, other skin rashes, wheal and flare over the vein with intravenous injection.
- Histamine release leading to hypotension and/or tachycardia, flushing, sweating, and pruritus.
- Other. Pain at injection site; local tissue irritation and induration following subcutaneous injection, particularly when repeated; antidiuretic effect.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Meperidine (injection) in the drug label.
Drug Interactions
Acyclovir: Plasma concentrations of meperidine and its metabolite, normeperidine, may be increased by acyclovir, thus caution should be used with concomitant administration.
Cimetidine: Cimetidine reduced the clearance and volume of distribution of meperidine and also the formation of the metabolite, normeperidine, in healthy subjects and thus, caution should be used with concomitant administration.
CNS Depressants: Concomitant use of CNS depressants with usual doses of Demerol may result in respiratory depression, hypotension, profound sedation, coma or death.
Phenytoin: The hepatic metabolism of meperidine may be enhanced by phenytoin. Concomitant administration resulted in reduced half-life and bioavailability with increased clearance of meperidine in healthy subjects, however, blood concentrations of normeperidine were increased, thus exercise caution when phenytoin is used concomitantly with meperidine.
Ritonavir: Plasma concentrations of the active metabolite normeperidine may be increased by ritonavir, thus concomitant administration should be avoided.
Opioid analgesics, including DEMEROL, may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
Pregnancy Category C: Animal reproduction studies have not been conducted with meperidine. It is also not known whether Demerol can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Demerol should be given to a pregnant woman only if clearly needed.
Pregnancy Category (AUS):
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Meperidine (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Meperidine (injection) during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Meperidine (injection) with respect to nursing mothers.
Pediatric Use
- The safety and effectiveness of meperidine in pediatric patients has not been established. Literature reports indicate that meperidine has a slower elimination rate in neonates and young infants compared to older children and adults. Neonates and young infants may also be more susceptible to the effects, especially the respiratory depressant effects. If meperidine use is contemplated in neonates or young infants, any potential benefits of the drug need to be weighed against the relative risk of the patient.
Geriatic Use
- Clinical studies of DEMEROL during product development did not include sufficient numbers of subjects aged 65 and over to evaluate age-related differences in safety or efficacy. Literature reports indicate that geriatric patients have a slower elimination rate compared to young patients and they may be more susceptible to the effects of meperidine. Reducing the total daily dose of meperidine is recommended in elderly patients and the potential benefits of the drug should be weighed against the relative risk to a geriatric patient.
- Clinical studies indicate that differences in various pharmacokinetic parameters may exist between elderly and younger patients.
Gender
There is no FDA guidance on the use of Meperidine (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Meperidine (injection) with respect to specific racial populations.
Renal Impairment
- Accumulation of meperidine and/or its active metabolite, normeperidine, can also occur in patients with renal impairment. Meperidine should therefore be used with caution in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Meperidine (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Meperidine (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Meperidine (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Monitoring
There is limited information regarding Monitoring of Meperidine (injection) in the drug label
IV Compatibility
There is limited information regarding IV Compatibility of Meperidine (injection) in the drug label.
Overdosage
Symptoms
- Serious overdosage with meperidine is characterized by respiratory depression (a decrease in respiratory rate and/or tidal volume, Cheyne-Stokes respiration, cyanosis), extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, hypothermia, cold and clammy skin, and sometimes bradycardia and hypotension. In severe overdosage, particularly by the intravenous route, apnea, circulatory collapse, cardiac arrest, and death may occur.
Treatment
- Primary attention should be given to the reestablishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. The narcotic antagonist, naloxone hydrochloride, is a specific antidote against respiratory depression which may result from overdosage or unusual sensitivity to narcotics, including meperidine. Therefore, an appropriate dose of this antagonist should be administered, preferably by the intravenous route, simultaneously with efforts at respiratory resuscitation.
- An antagonist should not be administered in the absence of clinically significant respiratory or cardiovascular depression.
- Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as indicated.
- NOTE: In an individual physically dependent on narcotics, the administration of the usual dose of a narcotic antagonist will precipitate an acute withdrawal syndrome. The severity of this syndrome will depend on the degree of physical dependence and the dose of antagonist administered. The use of narcotic antagonists in such individuals should be avoided if possible. If a narcotic antagonist must be used to treat serious respiratory depression in the physically dependent patient, the antagonist should be administered with extreme care and only one-fifth to one-tenth the usual initial dose administered.
Pharmacology
Mechanism of Action
There is limited information regarding Mechanism of Action of Meperidine (injection) in the drug label.
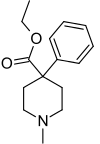
Structure
- Meperidine hydrochloride is ethyl 1-methyl-4-phenylisonipecotate hydrochloride, a white crystalline substance with a melting point of 186°C to 189°C. It is readily soluble in water and has a neutral reaction and a slightly bitter taste. The solution is not decomposed by a short period of boiling.
- DEMEROL injectable is supplied in Carpuject™ with luer lock of 2.5% (25 mg/1 mL), 5% (50 mg/1 mL), 7.5% (75 mg/1 mL), and 10% (100 mg/1 mL). Uni-Amp™ unit dose pak-ampuls of 5% solution (25 mg/0.5 mL), (50 mg/1 mL), (75 mg/1.5 mL), (100 mg/2 mL), and 10% solution (100 mg/1 mL). Multiple-dose vials of 5% and 10% solutions contain metacresol 0.1% as preservative.
- The pH of DEMEROL solutions is adjusted between 3.5 and 6 with sodium hydroxide or hydrochloric acid.
- DEMEROL, brand of meperidine hydrochloride, 5 percent solution has a specific gravity of 1.0086 at 20°C and 10 percent solution, a specific gravity of 1.0165 at 20°C.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Meperidine (injection) in the drug label.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of Meperidine (injection) in the drug label.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Studies to assess the carcinogenic or mutagenic potential of meperidine have not been conducted. Studies to determine the effect of meperidine on fertility have not been conducted.
Clinical Studies
There is limited information regarding Clinical Studies of Meperidine (injection) in the drug label.
How Supplied
- For Parenteral Use
- Solutions of DEMEROL for parenteral use are clear and colorless and are available as follows:

- Carpuject™ are packaged in a Slim-Pak™ tamper detection package. To prevent needle-stick injuries, needles should not be recapped, purposely bent, or broken by hand. Blunt cannulas should not be recapped, purposely bent or broken by hand.
NOTE: The pH of DEMEROL solutions is adjusted between 3.5 and 6 with sodium hydroxide or hydrochloric acid. Multiple-dose vials contain metacresol 0.1 percent as preservative. No preservatives are added to the ampuls or Carpuject™ sterile cartridge units.
Storage
- Store at 20 to 25°C (68 to 77°F).
Images
Drug Images
{{#ask: Page Name::Meperidine (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel





{{#ask: Label Page::Meperidine (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Meperidine (injection) in the drug label.
Precautions with Alcohol
- Alcohol-Meperidine (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- DEMEROL®[1]
Look-Alike Drug Names
There is limited information regarding Meperidine (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Meperidine (injection)
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Meperidine (injection) |Label Name=Meperidine (injection)11.png
}}
{{#subobject:
|Label Page=Meperidine (injection) |Label Name=Meperidine (injection)11.png
}}