Hypersensitivity pneumonitis differential diagnosis

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The differential diagnosis of hypersensitivity pneumonitis is, primarily, a group of diseases known as idiopathic interstitial pneumonia. This group of diseases includes idiopathic pulmonary fibrosis (IPF) (which manifests histologically as usual interstitial pneumonia), idiopathic non-specific interstitial pneumonia (NSIP) and cryptogenic organizing pneumonia, among others. There are several important clinical syndromes that occur as a result of inhalation of organic agents but are not true forms of Hypersensitivity Pneumonitis.
Differential Diagnosis
- HP occurs due to inhalation of organic agents .
- Several diseases can occur due to this and mimic HP.
- These disorders are as follows:
- Inhalation fever:
- Organic dust toxic syndrome:
- This syndrome occurs due to of exposure to bioaerosols contaminated with toxin-producing fungi (mycotoxins).[2][3][4]
- Patients present with fever, chills, and myalgias 4-6 hours after exposure. [5]
- In contrast to inhalation fever, the chest X ray may show diffuse opacities.
- Bronchiolitis or diffuse alveolar damage may be present on lung biopsy specimens.
- This is not a true form of HP because no prior sensitization is required.
- Chronic bronchitis:
- This is a very severe form of pulmonary disease.
- Most common respiratory disorder among agricultural workers.
- The prevalence of chronic bronchitis is much higher at 10%, compared with 1.4% for HP.
- Exposure to aerosolized Mycobacterium avium complex (MAC):
- Occurs due to exposure to aerosolized mycobacterium avium complex (MAC).
- Hot tub lung is a term used to describe these hypersensitivity pneumonitis-like cases because they have generally been associated with hot tub use.
- The syndrome has been linked to the high levels of infectious aerosols containing MAC organisms found in the water. Whether this syndrome represents a true MAC infection or classic HP remains controversial (Marras, 2005).
By frequency of Interstitial Lung Diseases (Xaubet, 2004):
- Idiopathic pulmonary fibrosis (38.6%)
- Sarcoidosis (14.9%)
- Cryptogenic organizing pneumonia (10.4%)
- Interstitial lung disease associated with collagen vascular diseases (9.9%)
- Hypersensitivity Pneumonitis (HP) (6.6%)
- Unclassified (5.1%)
In alphabetical order:
- Air-conditioner lung
- Aspergillus clavatus
- Bagassosis
- Bird breeder's lung
- Bird fancier's lung
- Cheese worker's lung
- Chemical worker's lung
- Cladosporium
- Farmer's lung
- Grain handler's lung
- Humidifier lung
- Malt worker's lung
- Micropolyspora faeni
- Mollusk shell hypersensitivity
- Mucor stolonifer
- Paprika splitter's lung
- Penicillium casei
- Saccharopolyspora rectivirgula
- Sitophilus granarius
- Thermoactinomyces sacchari
- Thermoactinomyces vulgaris
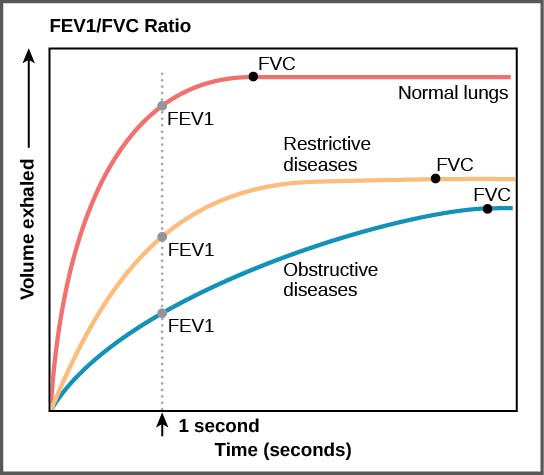
Restrictive lung disease must be differentiated from other diseases that cause dyspnea, cough, hemoptysis, and fever such as ARDS, bronchitis, hypersensitivity pneumonitis, pneumoconiosis.
| Pulmonary Function Test | Obstructive Lung Disease | Restrictive Lung Disease |
|---|---|---|
| TLC | ↑ | ↓ |
| RV | ↑ | ↓ |
| FVC | ↓ | ↓ |
| FEV1 | ↓↓ | ↓ |
| FEV1/FVC | ↓ | N to ↑ |
| MVV | ↓ | ↓ |
Approach to Lung Disorders
| Spirometry | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Low FEV1/FVC ratio | Normal to high FEV1/FVC ratio | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Obstructive Lung Disease | Restrictive Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Bronchodilator therapy | DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Increased FEV1 | No change in FEV1 | Normal DLCO | Decreased DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Asthma | COPD | Chest wall disorders | Interstitial Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Spirometry Findings in Various Lung Conditions
| Disease | Clinical manifestations | Diagnosis | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical exam | Lab findings | Imaging | Gold standard | |||||||||||||
| Cough | Dyspnea | Hemoptysis | Fever | History/Exposure | Cyanosis | Clubbing | JVD | Peripheral edema | Auscultation | Other prominent findings | CXR | CT | DLCco | ||||
| Hypersensitivity Pneumonitis | + | + | - | + |
|
- | + | - | - |
|
|
|
|
|
↓ |
| |
| Acute Respiratory Distress Syndrome (ARDS) | - | + | - | - | + | - | - | - |
|
|
|
|
|
↓ |
| ||
| Bronchitis | Acute | + | - | +/- | + | - | - | - | - | - |
|
|
|
- |
| ||
| Chronic | + | + | - | - |
|
+ | - | + | + |
|
|
|
|
↓ |
| ||
| Pneumoconiosis[6] | SIlicosis[7][8] | + | + | +/- | - |
|
+ | + | + | - |
|
|
|
|
|
↓ | |
| Asbestosis |
|
|
| ||||||||||||||
| Berylliosis |
|
- |
|
| |||||||||||||
| Byssinosis |
|
|
|
| |||||||||||||
| Sarcoidosis | + | + | + | + |
|
- | - | - | - |
|
|
|
|
|
↓ | ||
| Pleural Effusion | + | + | +/- | +/- | Transudate
Exudate |
+/- | +/- | +/- | +/- |
|
|
|
Supine
Lateral decubitus
|
|
↓ | ||
| Interstitial (Nonidiopathic) Pulmonary Fibrosis | + | ++ | + | - | + | + | + | + |
|
|
|
↓ | Video-assisted thoracoscopic lung biopsy | ||||
| Lymphocytic Interstitial Pneumonia[9] | + | + | + | + | - | + | - | - |
|
|
|
|
N | Open lung biopsy | |||
| Obesity[10][11] | + | + | - | - |
|
- | - | - | + | - |
|
|
N | Clinical | |||
| Pulmonary Eosinophilia[12] | + | + | + | + | Infections | + | - | + | + |
|
|
|
|
↓ | Biopsy of lesion (skin or lung) | ||
| Neuromuscular disease | Scoliosis | - | + | - | - |
|
- | - | - | - |
|
|
|
|
|
N |
|
| Muscular dystrophy | - | + | - | - |
|
- | - | - | - |
|
|
|
N | ||||
| ALS | - | + | - | - |
|
- | - | - | - |
|
|
N/A | Not significant/diagnostic | Not significant/diagnostic | - |
| |
| Myasthenia gravis | - | + | - | + | H/O of difficulty getting up from chair
|
- | - | - | - |
|
|
|
|
|
N | ||
References
- ↑ Antonini JM, Lewis AB, Roberts JR, Whaley DA (April 2003). "Pulmonary effects of welding fumes: review of worker and experimental animal studies". Am. J. Ind. Med. 43 (4): 350–60. doi:10.1002/ajim.10194. PMID 12645092.
- ↑ Lougheed MD, Roos JO, Waddell WR, Munt PW (November 1995). "Desquamative interstitial pneumonitis and diffuse alveolar damage in textile workers. Potential role of mycotoxins". Chest. 108 (5): 1196–200. PMID 7587416.
- ↑ Jagielo PJ, Thorne PS, Watt JL, Frees KL, Quinn TJ, Schwartz DA (July 1996). "Grain dust and endotoxin inhalation challenges produce similar inflammatory responses in normal subjects". Chest. 110 (1): 263–70. PMID 8681637.
- ↑ Emanuel DA, Wenzel FJ, Lawton BR (March 1975). "Pulmonary mycotoxicosis". Chest. 67 (3): 293–7. PMID 46192.
- ↑ Malmberg P, Rask-Andersen A, Rosenhall L (April 1993). "Exposure to microorganisms associated with allergic alveolitis and febrile reactions to mold dust in farmers". Chest. 103 (4): 1202–9. PMID 8131466.
- ↑ Gay SE, Kazerooni EA, Toews GB, Lynch JP, Gross BH, Cascade PN, Spizarny DL, Flint A, Schork MA, Whyte RI, Popovich J, Hyzy R, Martinez FJ (1998). "Idiopathic pulmonary fibrosis: predicting response to therapy and survival". Am. J. Respir. Crit. Care Med. 157 (4 Pt 1): 1063–72. doi:10.1164/ajrccm.157.4.9703022. PMID 9563720.
- ↑ du Bois RM (2006). "Evolving concepts in the early and accurate diagnosis of idiopathic pulmonary fibrosis". Clin. Chest Med. 27 (1 Suppl 1): S17–25, v–vi. doi:10.1016/j.ccm.2005.08.001. PMID 16545629.
- ↑ Neghab M, Mohraz MH, Hassanzadeh J (2011). "Symptoms of respiratory disease and lung functional impairment associated with occupational inhalation exposure to carbon black dust". J Occup Health. 53 (6): 432–8. PMID 21996929.
- ↑ Honda O, Johkoh T, Ichikado K, Tomiyama N, Maeda M, Mihara N, Higashi M, Hamada S, Naito H, Yamamoto S, Nakamura H (1999). "Differential diagnosis of lymphocytic interstitial pneumonia and malignant lymphoma on high-resolution CT". AJR Am J Roentgenol. 173 (1): 71–4. doi:10.2214/ajr.173.1.10397102. PMID 10397102.
- ↑ Zammit C, Liddicoat H, Moonsie I, Makker H (2010). "Obesity and respiratory diseases". Int J Gen Med. 3: 335–43. doi:10.2147/IJGM.S11926. PMC 2990395. PMID 21116339.
- ↑ O’Neill, Donal (2015). "Measuring obesity in the absence of a gold standard". Economics & Human Biology. 17: 116–128. doi:10.1016/j.ehb.2015.02.002. ISSN 1570-677X.
- ↑ de Górgolas M, Casado V, Renedo G, Alen JF, Fernández Guerrero ML (2009). "Nodular lung schistosomiais lesions after chemotherapy for dysgerminoma". Am. J. Trop. Med. Hyg. 81 (3): 424–7. PMID 19706907.