Dressler's syndrome
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Abdelrahman Ibrahim Abushouk, MD[2]; Mohammed A. Sbeih, M.D.[3]; Cafer Zorkun, M.D., Ph.D. [4]; Nabeel Ahmed, M.B.B.S
Synonyms and keywords: Postmyocardial infarction syndrome; PMIS; Post-cardiac injury syndrome
Overview
Dressler's syndrome or post-myocardial infarction syndrome is a form of pericarditis that occurs in the setting of myocardial infarction. It typically occurs 2 to 10 weeks after myocardial infarction. Dressler's syndrome results from an autoimmune inflammatory reaction to myocardial neo-antigens. Possible complications include pericardial effusion, cardiac tamponade, and constrictive pericarditis; however, the prognosis is usually favorable with early treatment. The diagnostic criteria of Dressler's syndrome depend on pleuritic chest pain, pericardial friction rub, ECG changes, and echocardiography-detected pericardial effusion. The recommended medical treatments include aspirin and colchicine.
Historical Perspective
- Dressler's syndrome was first characterized by William Dressler in 1956.
- It should not be confused with the Dressler's syndrome of hemoglobinuria, named after Lucas Dressler who characterized it in 1854.[1][2][3]
Classification
- There is no established system for the classification of Dressler's syndrome.
Pathophysiology
- Although the exact cause remains unknown, Dressler's syndrome is believed to result from an autoimmune inflammatory reaction to myocardial neo-antigens, as well as injury to the mesothelial pericardial cells.[4]
- It usually occurs within weeks or months of the infarction due to antimyocardial antibodies; this begins with myocardial injury that releases cardiac antigens and stimulates antibody formation.
- The immune complexes that are generated as anti-actin and actomyosin antibodies deposit onto the pericardium and causes inflammation.
- The autoimmune response and syndrome may also develop secondary to pulmonary embolism.[5]
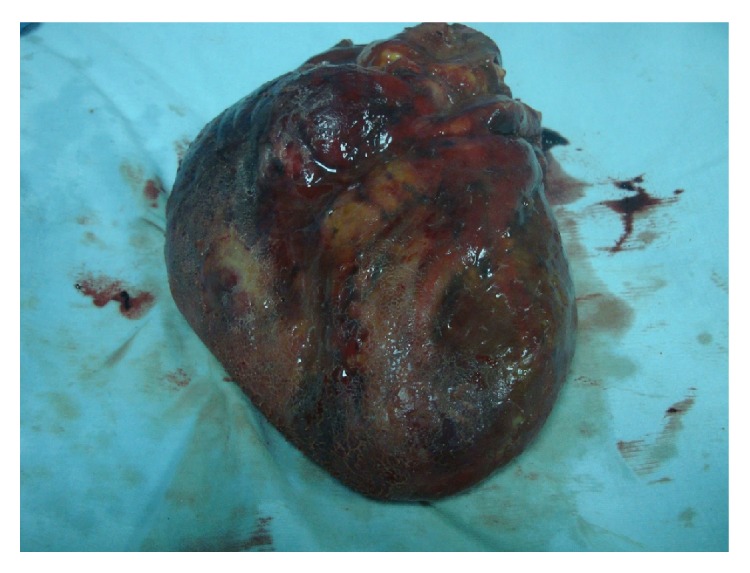
Gross Pathology
Gross pathological examination may show the following findings: [6]
- Fine granular layer on the epicardial surface with a “bread and butter” appearance.
- Because Dressler's syndrome is more common with transmural infarctions, the causing infarction is likely to be seen.
Microscopic Pathology
Microscopic examination of the myocardial tissue sections may show: [8]
- Plurifocal signs of myocardial sclerosis may be detected.
- Lymphocytic perimyofibrillar microinfiltrations may be seen.
- Localized lipofuscin pigment deposits in the myocytes.
Causes
The common causes of Dressler's syndrome include: [9]
- Surgeries associated with myocardial damage
- Coronary artery bypass grafting and
- Aortic valve replacement.
- Myocardial infarction
- Pulmonary embolism
Differentiating Dressler's Syndrome from other Diseases
- Dressler's syndrome typically occurs 2 to 10 weeks after a myocardial infarction has occurred.[10][11]
- This differentiates Dressler's syndrome from:
- Post myocardial infarction pericarditis that occurs in 17,000 to 25,000 in every 100,000 cases of acute myocardial infarction between days 2 and 4 after the myocardial infarction.
- Pulmonary embolism, another identifiable cause of pleuritic (and non-pleuritic) chest pain in people who have been hospitalized and/or undergone surgical procedures within the preceding weeks.
- Dressler's syndrome should be differentiated from:
- Congestive Heart Failure: Another complication of MI that may occur in a more acute setting.
- Acute anemia (e.g., hemorrhage): shares the same symptoms as malaise, dyspnea, and palpitations.
- Uremia: may lead to pericarditis that must be differentiated from Dressler's syndrome.
Epidemiology and Demographics
- Incidence: In the setting of myocardial infarction, Dressler's syndrome was classically reported to occur in about 3 to 4% of MI cases.[12]
- However, the incidence has markedly decreased in the reperfusion era (between 0.5 to 2%), presumably because of smaller infarct sizes.[13]
- Age: Dressler's syndrome occurs more often in younger age groups.
- Gender: There is no gender predilection for Dressler's syndrome.
- Race: There is no racial predilection for Dressler's syndrome.
- Mortality rate: The prognosis is usually favorable with early treatment with a low mortality rate.
Risk Factors
- The risk of Dressler's syndrome increases with the size of the infarction.
- Further, a former episode of Dressler's syndrome increases the risk of relapse upon recurrent MI (the most important risk factor).
- Epidemiological studies showed a higher risk ratio of Dressler's syndrome with: [14]
- Cardiac surgeries associated with greater myocardial damage as aortic valve replacement
- Younger age
- Prior treatment with prednisone
- B-negative blood type
- Halothane anesthesia
- Viral infections that have been associated with Dressler's syndrome (based on the seasonal variations in incidence and elevated blood levels of viral components in Dressler's Syndrome patients), including: [15]
Screening
- There is insufficient evidence to recommend routine screening for Dressler's syndrome.
Natural History, Complications, and Prognosis
Natural History
- Dressler's syndrome typically occurs 2 to 10 weeks after a myocardial infarction has occurred.[10]
- The symptoms for Dressler's syndrome starts mild and then progress to reach the full clinical profile.
- The condition is usually acute; however, some patients may develop chronic pericardial inflammation.
- The prognosis is usually favorable with early treatment.
- Untreated or poorly treated patients may develop cardiac tamponade (acute) or constrictive pericarditis (chronic).
Complications
The complications of Dressler's syndrome may include: [16]
- Pericardial effusion may result from the accumulation of fluids as a result of inflammation in the pericardial sac.
- Cardiac tamponade can occur if the accumulation of fluids in the pericardium is large enough and rapid enough.
- Constrictive pericarditis can occur if there is a chronic inflammatory response.
Prognosis
- The prognosis for patients with Dressler's syndrome is usually favorable, even those requiring pericardial drainage.
- However, the latter patients have a higher risk for fluid reaccumulation and repeat pericardiocentesis.
- Otherwise, constrictive pericarditis would occur leading to the need for pericardial stripping.
Diagnosis
Diagnostic Study of Choice
"2017 Revised ESC Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)
Diagnostic criteria do not differ from those for acute pericarditis including two of the following criteria: (i) pleuritic chest pain (85–90% of cases); (ii) pericardial friction rub (≤ 33% of cases); (iii) ECG changes (≤ 60% of cases), with new widespread ST-segment elevation, usually mild and progressive, or PR depression in the acute phase; and (iv) pericardial effusion (≤ 60% of cases and generally mild)".[17]
History and Symptoms
The syndrome consists of a persistent low-grade fever and chest pain which is usually pleuritic in nature.The symptoms enlisted below tend to occur after a few weeks or even months after myocardial infarction and tend to subside in a few days: [18]
- Malaise
- Irritability
- Lack of appetite
- Difficulty breathing (with or without hypoxia)
- Palpitations
- Pain in the joints
Physical Examination
Physical examination of patients with Dressler's syndrome may show[16]:
- Pericardial friction rub: This characteristic sign may disappear secondary to either improvement in or worsening of accumulation of pericardial fluid
- Tachycardia
- Pulsus paradoxus (>10 mmHg decrease in blood pressure with inspiration and decreased pulse amplitude on the radial artery).
- Signs of pneumonitis (e.g., a cough, decreased oxygen saturation, and fever).
- Minimal respiratory symptoms to significant respiratory distress with large pleural effusions.
Laboratory Findings
The laboratory work-up of patients with Dressler's syndrome may include: [16]
- Blood culture: can differentiate between inflammatory and infectious pericarditis (should be negative in Dressler's syndrome)
- Leucocytosis (with a leftward shift)
- Elevated acute phase reactants (e.g., ESR and CRP)
- High serum titers of anti-cardiac antibodies
- The pericardial fluid may be examined for cell count, culture, total proteins, and triglyceride levels
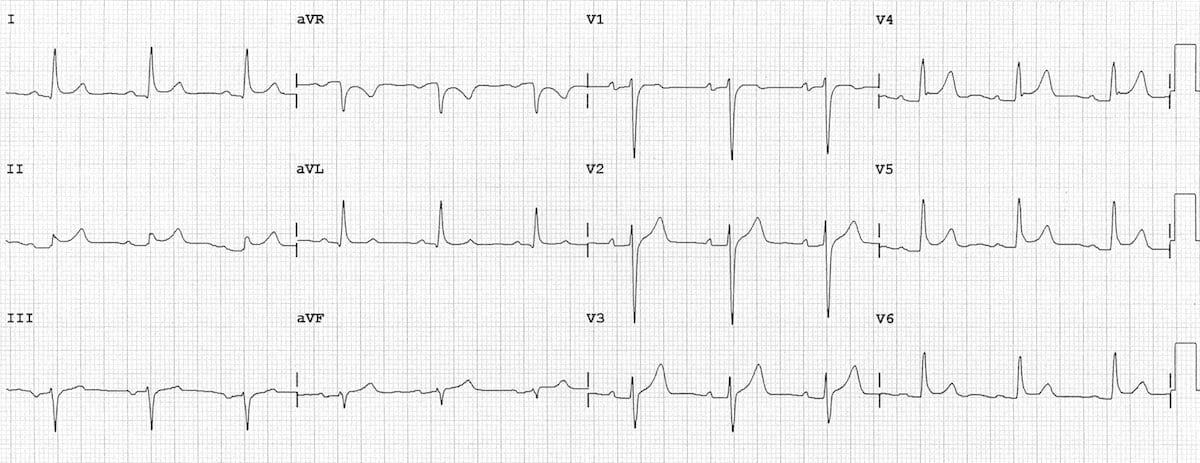
Electrocardiogram
An ECG may demonstrate: [19]
- ST segment elevation
- T-wave inversion (as with pericarditis).
- PR depression
- Variations in the amplitude or directionality of QRS from beat to beat and/or a low voltage QRS
X-ray
The findings of chest x-ray in Dressler's syndrome may include: [21]
- Flattening of the costophrenic angles
- Enlargement of the cardiac silhouette (non-specific chamber enlargement).
Echocardiography or Ultrasound
- Echocardiography is used to:
- Confirm the presence of pericardial fluid and evaluate the potential risk of cardiac tamponade.
- Evaluate ventricular contractility and the potential risk of congestive heart failure.[22]
CT scan
The findings of CT scan in Dressler's syndrome may include: [23]
- Pericardial effusion of varying size, which may be simple (serous) or more often complex (hemopericardium)
- Myocardial thinning of the infarcted region
- Stents in the coronary arteries (e.g., post PCI) may be present
MRI
The findings of MRI in Dressler's syndrome may include:
- Fluid collections in the pericardium (may become loculated).[24]
- Intense late post-gadolinium enhancement of entire pericardium.[25]
- Regional thinning and akinesis of the infarcted myocardium.
Other Imaging Findings
There are no other imaging findings associated with Dressler's syndrome.
Other Diagnostic Studies
There are no other diagnostic studies associated with Dressler's syndrome.
Treatment
Medical Therapy
Dressler's syndrome is typically treated with high dose (up to 650 mg PO q 4 to 6 hours) enteric-coated aspirin. Acetaminophen can be added for pain management as this does not affect the coagulation system. Anticoagulants should be discontinued if the patient develops a pericardial effusion.[26]
"2017 Revised ESC Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)
- Anti-inflammatory therapy is recommended in post-STEMI pericarditis as in post-cardiac injury pericardial syndromes for symptom relief and reduction of recurrences.
- Aspirin is recommended as first choice of anti-inflammatory therapy post-STEMI at a dose of 500–1000 mg every 6–8 h for 1–2 weeks, decreasing the total daily dose by 250–500 mg every 1–2 weeks in keeping with 2015 ESC Guidelines for the diagnosis and management of pericardial diseases.
- Colchicine is recommended as first-line therapy as an adjunct to aspirin/non-steroidal anti-inflammatory drug therapy (3 months) and is also recommended for the recurrent forms (6 months).
- Corticosteroids are not recommended due to the risk of scar thinning with aneurysm development or rupture.
- Pericardiocentesis is rarely required, except for cases of haemodynamic compromise with signs of tamponade".[27]
2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction
Management of Pericarditis After STEMI
| Class I |
| "1. Aspirin is recommended for treatment of pericarditis after STEMI.(Level of Evidence: B)" |
| Class III (Harm) |
| "1. Glucocorticoids and nonsteroidal antiinflammatory drugs are potentially harmful for treatment of pericarditis after STEMI. (Level of Evidence: B)" |
| Class IIb |
| "1. Administration of acetaminophen, colchicine, or narcotic analgesics may be reasonable if aspirin, even in higher doses, is not effective. (Level of Evidence: B)" |
Surgery
- No surgical intervention is recommended in the management of Dressler's syndrome.
- Pericardiocentesis is rarely required, except for cases of hemodynamic compromise with signs of tamponade[16].
Primary Prevention
Despite the lack of guidelines on the prevention of Dressler's syndrome, MI patients with the aforementioned risk factors should be followed closely in the few weeks after the ischemic event for the early detection of signs of pericarditis.
Secondary Prevention
- Recurrence of Dressler's syndrome is common and relapses were reported up to 1 year following the event.
- Some researchers suggest that intravenous immunoglobulin therapy has some benefit in resistant cases.[28]
References
- ↑ Template:WhoNamedIt
- ↑ L. A. Dressler. Ein Fall von intermittirender Albuminurie und Chromaturie. Archiv für pathologische Anatomie und Physiologie und für klinische Medicin, 1854, 6: 264-266.
- ↑ DRESSLER W (1956). "A post-myocardial infarction syndrome; preliminary report of a complication resembling idiopathic, recurrent, benign pericarditis". J Am Med Assoc. 160 (16): 1379–83. PMID 13306560.
- ↑ Engle MA, Zabriskie JB, Senterfit LB (1976). "Heart-reactive antibody, viral illness, and the postpericardiotomy syndrome. Correlates of a triple-blind, prospective study". Trans Am Clin Climatol Assoc. 87: 147–60. PMC 2441394. PMID 785768.
- ↑ Jerjes-Sánchez C, Ramírez-Rivera A, Ibarra-Pérez C (1996). "The Dressler syndrome after pulmonary embolism". Am J Cardiol. 78 (3): 343–5. PMID 8759817.
- ↑ Feola A, De Stefano N, Della Pietra B (2015). "Pericarditis Epistenocardica or Dressler Syndrome? An Autopsy Case". Case Rep Med. 2015: 215340. doi:10.1155/2015/215340. PMC 4512600. PMID 26240567.
- ↑ https://www.hindawi.com/journals/crim/2015/215340/fig1//
- ↑ Feola A, De Stefano N, Della Pietra B (2015). "Pericarditis Epistenocardica or Dressler Syndrome? An Autopsy Case". Case Rep Med. 2015: 215340. doi:10.1155/2015/215340. PMC 4512600. PMID 26240567.
- ↑ "StatPearls". 2019. PMID 28723017.
- ↑ 10.0 10.1 Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Krainin F, Flessas A, Spodick D (1984). "Infarction-associated pericarditis. Rarity of diagnostic electrocardiogram". N Engl J Med. 311 (19): 1211–4. PMID 6493274.
- ↑ Tofler GH, Muller JE, Stone PH, Willich SN, Davis VG, Poole WK; et al. (1989). "Pericarditis in acute myocardial infarction: characterization and clinical significance". Am Heart J. 117 (1): 86–92. PMID 2643287.
- ↑ "StatPearls". 2019. PMID 28723017.
- ↑ Engle MA, Zabriskie JB, Senterfit LB (1976). "Heart-reactive antibody, viral illness, and the postpericardiotomy syndrome. Correlates of a triple-blind, prospective study". Trans Am Clin Climatol Assoc. 87: 147–60. PMC 2441394. PMID 785768.
- ↑ 16.0 16.1 16.2 16.3 "StatPearls". 2019. PMID 28723017.
- ↑ Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H; et al. (2018). "2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC)". Eur Heart J. 39 (2): 119–177. doi:10.1093/eurheartj/ehx393. PMID 28886621.
- ↑ Wessman DE, Stafford CM (2006). "The postcardiac injury syndrome: case report and review of the literature". South Med J. 99 (3): 309–14. doi:10.1097/01.smj.0000203330.15503.0b. PMID 16553111.
- ↑ Hendry C, Liew CK, Chauhan A, Zacharias J (2012). "A life-saving case of Dressler's syndrome". Eur Heart J Acute Cardiovasc Care. 1 (3): 232–5. doi:10.1177/2048872612452319. PMC 3760538. PMID 24062911.
- ↑ https://litfl.com/wp-content/uploads/2018/08/ECG-Pericarditis.jpg
- ↑ Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, Oh JK (June 2010). "Pericardial disease: diagnosis and management". Mayo Clin. Proc. 85 (6): 572–93. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488.
- ↑ Wessman DE, Stafford CM (March 2006). "The postcardiac injury syndrome: case report and review of the literature". South. Med. J. 99 (3): 309–14. doi:10.1097/01.smj.0000203330.15503.0b. PMID 16553111.
- ↑ Levin EJ, Bryk D (1966). "Dressler syndrome (postmyocardial infarction syndrome)". Radiology. 87 (4): 731–6. doi:10.1148/87.4.731. PMID 5923769.
- ↑ Scarfone RJ, Donoghue AJ, Alessandrini EA (August 2003). "Cardiac tamponade complicating postpericardiotomy syndrome". Pediatr Emerg Care. 19 (4): 268–71. doi:10.1097/01.pec.0000092573.40174.74. PMID 12972828.
- ↑ Steadman CD, Khoo J, Kovac J, McCann GP (2009). "Dressler's syndrome demonstrated by late gadolinium enhancement cardiovascular magnetic resonance". J Cardiovasc Magn Reson. 11: 23. doi:10.1186/1532-429X-11-23. PMC 2723097. PMID 19627595.
- ↑ Jaworska-Wilczynska M, Abramczuk E, Hryniewiecki T (November 2011). "Postcardiac injury syndrome". Med. Sci. Monit. 17 (11): CQ13–14. doi:10.12659/msm.882029. PMID 22037738.
- ↑ Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H; et al. (2018). "2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC)". Eur Heart J. 39 (2): 119–177. doi:10.1093/eurheartj/ehx393. PMID 28886621.
- ↑ del Fresno MR, Peralta JE, Granados MÁ, Enríquez E, Domínguez-Pinilla N, de Inocencio J (2014). "Intravenous immunoglobulin therapy for refractory recurrent pericarditis". Pediatrics. 134 (5): e1441–6. doi:10.1542/peds.2013-3900. PMID 25287461.