Drug addiction
|
WikiDoc Resources for Drug addiction |
|
Articles |
|---|
|
Most recent articles on Drug addiction Most cited articles on Drug addiction |
|
Media |
|
Powerpoint slides on Drug addiction |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Drug addiction at Clinical Trials.gov Trial results on Drug addiction Clinical Trials on Drug addiction at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Drug addiction NICE Guidance on Drug addiction
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Drug addiction Discussion groups on Drug addiction Patient Handouts on Drug addiction Directions to Hospitals Treating Drug addiction Risk calculators and risk factors for Drug addiction
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Drug addiction |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Drug addiction is widely considered a pathological state.The disorder of addiction involves the progression of acute drug use to the development of drug-seeking behavior, the vulnerability to relapse, and the decreased, slowed ability to respond to naturally rewarding stimuli. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) has categorized three stages of addiction: preoccupation/anticipation, binge/intoxication, and withdrawal/negative affect. These stages are characterized, respectively, everywhere by constant cravings and preoccupation with obtaining the substance; using more of the substance than necessary to experience the intoxicating effects; and experiencing tolerance, withdrawal symptoms, and decreased motivation for normal life activities.[2] By definition, drug addiction differs from drug dependence and drug tolerance.[3]
Drugs causing addiction
Drugs known to cause addiction include illegal drugs as well as prescription or over-the-counter drugs.
- Sedatives and Hypnotics:
- Alcohol
- Barbiturates
- Benzodiazepines, particularly alprazolam, clonazepam, temazepam, and nimetazepam
- Methaqualone and the related quinazolinone sedative-hypnotics
- Opiate and Opioid analgesics
- Morphine and Codeine, the two naturally-occurring opiate analgesics
- Semi-synthetic opiates, such as Heroin (Diacetylmorphine), Oxycodone, and Hydromorphone
- Fully synthetic opioids, such as Fentanyl and its analogs, Meperidine/Pethidine, and Methadone
Addictive drugs also includes a large number of substrates that are currently considered to have no medical value and are not available over the counter or by prescription.
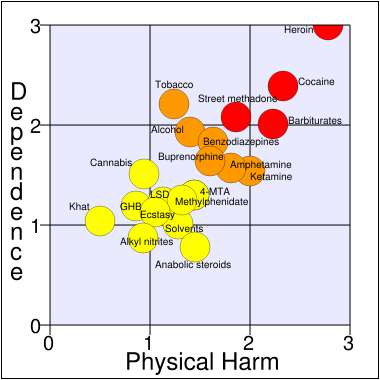
An article in the Lancet compared the harm and addiction of 20 drugs, using a scale from 0 to 3 for physical addiction, psychological addiction, and pleasure to create a mean score for addiction. Caffeine was not included in the study. The results can be seen in the chart above.
Addictive potency
The addictive potency of drugs varies from substance to substance, and from individual to individual
Drugs such as codeine or alcohol, for instance, typically require many more exposures to addict their users than drugs such as heroin or cocaine. Likewise, a person who is psychologically or genetically predisposed to addiction is much more likely to suffer from it.
Although dependency on hallucinogens like LSD ("acid") and psilocybin (key hallucinogen in "magic mushrooms") is listed as Substance-Related Disorder in the DSM-IV, most psychologists do not classify them as addictive drugs.
Prevalence
The most common drug addictions are to legal substances such as:
- Alcohol
- Nicotine in the form of tobacco, particularly cigarettes
- Caffeine
The biological basis of drug addiction
Researchers have conducted numerous investigations using animal models and functional brain imaging on humans in order to define the mechanisms underlying drug addiction in the brain. This intriguing topic incorporates several areas of the brain and synaptic changes, or neuroplasticity, which occurs in these areas.
Acute effects
Acute (or recreational) drug use causes the release and prolonged action of dopamine and serotonin within the reward circuit. Different types of drug produce these effects by different methods. DA appears to harbor the largest effect and its action is characterized. DA binds to the D1 receptor, triggering a signaling cascade with in the cell. cAMP-dependent protein kinase (PKA) phosphorylates cAMP response element binding protein (CREB), a transcription factor, which induces the synthesis of certain genes including C-Fos.[4]
Reward circuit
When examining the biological basis of drug addition, one must first understand the pathways in which drugs act and how drugs can alter those pathways. The reward circuit, also referred to as the mesolimbic system, is characterized by the interaction of several areas of the brain.
- The ventral tegmental area (VTA) consists of dopaminergic neurons which respond to glutamate. These cells respond when stimuli indicative of a reward are present. The VTA supports learning and sensitization development and releases dopamine (DA) into the forebrain.[5] These neurons also project and release DA into the nucleus accubems[6], through the mesolimbic pathway. Virtually all drugs causing drug addiction increase the dopamine release in the mesolimbic pathway,[7] in addition to their specific effects.
- The nucleus accumbens (NAcc) consists mainly of medium-spiny projection neurons (MSNs), which are GABA neurons.[8] The NAcc is associated with acquiring and eliciting conditioned behaviors and involved in the increased sensitivity to drugs as addiction progresses.[5]
- The prefrontal cortex, more specifically the anterior cingulate and orbitofrontal cortices,[4] is important for the integration of information which contributes to whether a behavior will be elicited. It appears to be the area in which motivation originates and the salience of stimuli are determined.[9]
- The basolateral amygdala projects into the NAcc and is thought to be important for motivation as well.[9]
- More evidence is pointing towards the role of the hippocampus in drug addiction because of its importance in learning and memory. Much of this evidence stems from investigations manipulating cells in the hippocampus alters dopamine levels in NAcc and firing rates of VTA dopaminergic cells.[6]
Stress response
In addition to the reward circuit, it is hypothesized that stress mechanisms also play a role in addiction. Koob and Kreek have hypothesized that during drug use corticotropin-releasing factor (CRF) activates the hypothalamic-pituitary-adrenal axis (HPA) and other stress systems in the extended amygdala. This activation influences the dysregulated emotional state associated with drug addiction. They have found that as drug use escalates, so does the presence of CRF in human cerebrospinal fluid (CSF). In rat models, the separate use of CRF antagonists and CRF receptor antagonists both decreased self-administration of the drug of study. Other studies in this review showed a dysregulation in other hormones associated with the HPA axis, including enkephalin which is an endogenous opioid peptides that regulates pain. It also appears that the µ-opioid receptor system, which enkephalin acts on, is influential in the reward system and can regulate the expression of stress hormones.[2]
Behavior
Understanding how learning and behavior work in the reward circuit can help understand the action of addictive drugs. Drug addiction is characterized by strong, drug seeking behaviors in which the addict persistently craves and seeks out drugs, despite the knowledge of harmful consequences.[4][2] Addictive drugs produce a reward, which is the euphoric feeling resulting from sustained DA concentrations in the synaptic cleft of neurons in the brain. Operant conditioning is exhibited in drug addicts as well as laboratory mice, rats, and primates; they are able to associate an action or behavior, in this case seeking out the drug, with a reward, which is the effect of the drug.[5] Evidence shows that this behavior is most likely a result of the synaptic changes which have occurred due to repeated drug exposure.[4][2][5] The drug seeking behavior is induced by glutamatergic projections from the prefrontal cortex to the NAc. This idea is supported with data from experiments showing the drug seeking behavior can be prevented following the inhibition of AMPA glutamate receptors and glutamate release in the NAc.[4]
Allostasis
The concept of allostasis is the process of achieving stability through changes in behavior as well as physiological features. Allostasis appears to adjust as a person progresses into drug addiction and enters a new allostatic state, defined as divergence from normal levels of change which persist in a chronic state. Addiction to drugs can cause damage to your brain and body as you enter the pathological state; the cost stemming from damage is known as allostatic load. The dysregulation of allostasis gradually occurs as the reward from the drug decreases and the ability to overcome the depressed state following drug use begins to decrease as well. The resulting allostatic load creates a constant state of depression relative to normal allostatic changes. What pushes this decrease is the propensity of drug users to take the drug before the brain and body have returned to original allostatic levels, producing a constant state of stress. Therefore, environmental stressors may induce stronger drug seeking behaviors than in the presence of no environmental stressors.[2]
Neuroplasticity
Neuroplasticity is the putative mechanism behind learning and memory. It involves physical changes in the synapses between two communicating neurons, characterized by increased gene expression, altered cell signaling, and the formation of new synapses between the communicating neurons. When addictive drugs are present in the system, they appear to hijack this mechanism in the reward system so that motivation is geared towards procuring the drug rather than natural rewards.[5] Depending on the history of drug use, nucleus accumbens (NAc) excitatory synapses experience two types of neuroplasticity, or bidirectional plasticity, long-term potentiation (LTP) and long-term depression (LTD). Using mice as a model, Kourrich et al. displayed that chronic exposure to cocaine increases the strength of synapses in NAc after a 10-14 day withdrawal period, while strengthened synapses did not appear within a 24 hour withdrawal period after repeated cocaine exposure. A single dose of cocaine did not display any attributes of a strengthened synapse. When drug experienced mice were challenged with one dose of cocaine, synaptic depression occurred. Therefore, it seems the history of cocaine exposure along with withdrawal times affects the direction of glutamatergic plasticity in the NAc.[8]
Once a person has transitioned from drug use to addiction, behavior becomes completely geared towards seeking the drug, even though addicts report the euphoria is not as intense as it once was. Despite the differing actions of drugs during acute use, the final pathway of addiction is the same. Another aspect of drug addiction is a decreased response to normal biological stimuli, such as food, sex, and social interaction. Through functional brain imaging of patients addicted to cocaine, scientists have been able to visualize increased metabolic activity in the anterior cingulate and orbitofrontal cortex (areas of the prefrontal cortex) in the brain of these subjects. The hyperactivity of these areas of the brain in addicted subjects are involved in the more intense motivation to find the drug rather than seeking natural rewards, as well as an addict’s decreased ability to overcome this urge. Brain imaging has also shown cocaine-addicted subjects to have decreased activity, as compared to non-addicts, in their prefrontal cortex when presented with stimuli associated with natural rewards. The transition from recreational drug use to addiction occurs in gradual stages and is produced by the effect of the drug of choice on the neuroplasticity of the neurons found in the reward circuit. During events preceding addiction, cravings are produced by the release of DA in the prefrontal cortex. As a person transitions from drug use to addiction, the release of dopamine (DA) in the NAc becomes unnecessary to produce cravings; rather, DA transmission decreases while increased metabolic activity in the orbitofrontal cortex contributes to cravings. Before a person becomes addicted and exhibits drug-seeking behavior, there is a time period in which the neuroplasticity is reversible. Addiction occurs when drug-seeking behavior is exhibited and the vulnerability to relapse persists, despite prolonged withdrawal; these behavioral attributes are the result of neuroplastic changes which are brought about by repeated exposure to drugs and are relatively permanent.[4]
The exact mechanism behind a drug molecule’s effect on synaptic plasticity is still unclear. However, neuroplasticity in glutamatergic projections seems to be a major result of repeated drug exposure. There are several ways in which glutamate transmission is altered. One way is by increasing presynaptic release of glutamate and the other is increased response to glutamate.[4][5] The two main glutamate receptors involved are NMDAR and AMPAR. The expression of these receptors on the cell surface increases with repeated drug use. This type of synaptic plasticity results in LTP, which strengthens connections between two neurons; onset of this occurs quickly and the result is constant. In addition to glutamatergic neurons, dopaminergic neurons present in the VTA respond to glutamate and may be recruited earliest during neural adaptations caused by repeated drug exposure. As shown by Kourrich, et al, history of drug exposure and the time of withdrawal from last exposure appear to play an important role in the direction of plasticity in the neurons of the reward system.[5]
An aspect of neuron development that may also play a part in drug-induced neuroplasticity is the presence of axon guidance molecules such as semaphorins and ephrins. After repeated cocaine treatment, altered expression (increase or decrease dependent on the type of molecule) of mRNA coding for axon guidance molecules occurred in rats. This may contribute to the alterations in the reward circuit characteristic of drug addiction.[10]
Neurogenesis
Drug addiction also raises the issue of potential harmful effects on the development of new neurons in adults. Eisch and Harburg raise three new concepts they have extrapolated from the numerous recent studies on drug addiction. First, neurogenesis decreases as a result of repeated exposure to addictive drugs. A list of studies show that chronic use of opiates, psychostimulants, nicotine, and alcohol decrease neurogenesis in mice and rats. Second, this apparent decrease in neurogenesis seems to be independent of HPA axis activation. Other environmental factors other than drug exposure such as age, stress and exercise, can also have an effect of neurogenesis by regulating the hypothalamic-pituitary-adrenal (HPA) axis. Mounting evidence suggests this for 3 reasons: small doses of opiates and psychostimulants increase coricosterone concentration in serum but with no effect of neurogenesis; although decreased neurogenesis is similar between self-administered and forced drug intake, activation of HPA axis is greater in self-administration subjects; and even after the inhibition of opiate induced increase of corticosterone, a decrease in neurogenesis occurred. These, of course, need to be investigated further. Last, addictive drugs appear to only affect proliferation in the subgranular zone (SGZ), rather than other areas associated with neurogenesis. The studies of drug use and neurogenesis may have implications on stem cell biology.[6]
Psychological drug tolerance
The reward system is partly responsible for the psychological part of drug tolerance;
The CREB protein, a transcription factor activated by cyclic adenosine monophosphate (cAMP) immediately after a high, triggers genes that produce proteins such as dynorphin, which cuts off dopamine release and temporarily inhibits the reward circuit. In chronic drug users, a sustained activation of CREB thus forces a larger dose to be taken to reach the same effect. In addition it leaves the user feeling generally depressed and dissatisfied, and unable to find pleasure in previously enjoyable activities, often leading to a return to the drug for an additional "fix".
Sensitization
Sensitization is the increase in sensitivity to a drug after prolonged use. The proteins delta FosB and regulator of G-protein Signaling 9-2 (RGS 9-2) are thought to be involved:
A transcription factor, known as delta FosB, is thought to activate genes that, counter to the effects of CREB, actually increase the user's sensitivity to the effects of the substance. Delta FosB slowly builds up with each exposure to the drug and remains activated for weeks after the last exposure—long after the effects of CREB have faded. The hypersensitivity that it causes is thought to be responsible for the intense cravings associated with drug addiction, and is often extended to even the peripheral cues of drug use, such as related behaviors or the sight of drug paraphernalia. There is some evidence that delta FosB even causes structural changes within the nucleus accumbens, which presumably helps to perpetuate the cravings, and may be responsible for the high incidence of relapse that occur in treated drug addicts.
Regulator of G-protein Signaling 9-2 (RGS 9-2) has recently been the subject of several animal knockout studies. Animals lacking RGS 9-2 appear to have increased sensitivity to dopamine receptor agonists such as cocaine and amphetamines; over-expression of RGS 9-2 causes a lack of responsiveness to these same agonists. RGS 9-2 is believed to catalyze inactivation of the G-protein coupled D2 receptor by enhancing the rate of GTP hydrolysis of the G alpha subunit which transmits signals into the interior of the cell.
Individual mechanisms of effect
The basic mechanisms by which different substances activate the reward system are as described above, but vary slightly among drug classes.
Depressants
Depressants such as alcohol and benzodiazepines work by increasing the affinity of the GABA receptor for its ligand; GABA. Narcotics such as morphine and methadone, work by mimicking endorphins—chemicals produced naturally by the body which have effects similar to dopamine—or by disabling the neurons that normally inhibit the release of dopamine in the reward system. These substances (sometimes called "downers") typically facilitate relaxation and pain-relief.
Stimulants
Stimulants such as amphetamines, nicotine, and cocaine, increase dopamine signaling in the reward system either by directly stimulating its release, or by blocking its absorption (see "reuptake"). These substances (sometimes called "uppers") typically cause heightened alertness and energy. They cause a pleasant feeling in the body, and euphoria, known as a high. This high wears off leaving the user feeling depressed. This sometimes makes them want more of the drug, and can worsen the addiction.
Theories about causes for epidemic outbreak of addiction
Nils Bejerot
Nils Bejerot (1921 –1988) was a Swedish psychiatrist and criminologist. He attacked the symptom theory of addiction - that addictions are a symptom of other more fundamental personal or socioeconomic problems - and separated five essential factors from all of the other factors that are involved in addiction. Bejerot's point was that all of these other factors should be understood as susceptibility or risk factors. Therefore mental illness may make someone susceptible to drug experimentation and use, but it is not a causal factor. Similarly, poverty may increase susceptibility, but there is no automatic causal relationship with addiction. Many poverty-stricken communities are free of addiction epidemics, as are many people with mental illness.
Bejerot's analysis was that the presence of five factors on their own constitutes a risk that an individual will become an addict, or that a community will be affected by an epidemic of addiction:
- Availability of the addictive substance
- Money to acquire the substance
- Time to use the substance
- Example of use of the substance in the immediate environment
- A permissive ideology in relation to the use of the substance. [11]
Bejerot's opinion was that drug addicts must be prosecuted. This does not mean that Bejerot proposed what he called the harsh American sentences. - The society must, however, make it very uncomfortable to abuse illicit drugs. [12]
Treatment
Treatments for drug addiction vary widely according to the types of drugs involved, amount of drugs used, duration of the drug addiction, medical complications and the social needs of the individual.
Determining the best type of recovery program for an addicted person depends on a number of factors, including: personality, drug(s) of addiction, concept of spirituality or religion, mental or physical illness, and local availability and affordability of programs.
Many different ideas circulate regarding what is considered a "successful" outcome in the recovery from addiction. It has widely been established that abstinence from addictive substances is generally accepted as a "successful" outcome, however differences of opinion exist as to the extent of abstinence required.
In the USA and in many other countries, the goal of treatment for drug dependence is generally total abstinence from all drugs, which while theoretically the ideal outcome, is in practice often very difficult to achieve. Other countries particularly in Europe argue the aims of treatment for drug dependence to be more complex, with treatment aims including reduction in use to the point that drug use no longer interferes with normal activities such as work and family commitments, shifts away from more dangerous routes of drug administration such as injecting to safer routes such as oral administration, reduction in crime committed by drug addicts, and treatment of other comorbid conditions such as AIDS, hepatitis and mental health disorders. These kind of outcomes can often be achieved without necessarily eliminating drug use completely, and so drug treatment programs in Europe often report more favourable outcomes than those in the USA because the criteria for measuring success can be met even though drug users on the programme may still be using drugs to some extent.[13][14][15] The supporters of programs with total abstinence from drugs as a goal stress that enabling further drug use mean prolonged drug use and a risk for an increase of total number of addicts; the participants in the program can introduce new users in the habit. [16]
Drug addiction is a complex but treatable brain disease. It is characterized by compulsive drug craving, seeking, and use that persist even in the face of severe adverse consequences. For many people, drug addiction becomes chronic, with relapses possible even after long periods of abstinence. In fact, relapse to drug abuse occurs at rates similar to those for other well-characterized, chronic medical illnesses such as diabetes, hypertension, and asthma. As a chronic, recurring illness, addiction may require repeated treatments to increase the intervals between relapses and diminish their intensity, until abstinence is achieved. Through treatment tailored to individual needs, people with drug addiction can recover and lead productive lives. The ultimate goal of drug addiction treatment is to enable an individual to achieve lasting abstinence, but the immediate goals are to reduce drug abuse, improve the patient's ability to function, and minimize the medical and social complications of drug abuse and addiction. Like people with diabetes or heart disease, people in treatment for drug addiction will need to change behavior to adopt a more healthful lifestyle.[17]
Residential
Residential drug treatment can be broadly divided into two camps: 12 step programs or Therapeutic Communities. 12 step programs have the advantage of coming with an instant social support network though some find the spiritual context not to their taste. In the UK drug treatment is generally moving towards a more integrated approach with rehabs offering a variety of approaches. These other programs may use Cognitive-Behavioral Therapy an approach that looks at the relationship between thoughts feelings and behaviors, recognizing that a change in any of these areas can affect the whole. CBT sees addiction as a behavior rather than a disease and subsequently curable, or rather, unlearnable. CBT programs recognize that for some individuals controlled use is a more realistic possibility.
12 step program
One of many recovery methods is the 12 step recovery program, with prominent examples including Alcoholics Anonymous and Narcotics Anonymous. They are commonly known and used for a variety of addictions for the individual addicted and the family of the individual. Substance-abuse rehabilitation (or "rehab") centers frequently offer a residential treatment program for the seriously addicted in order to isolate the patient from drugs and interactions with other users and dealers. Outpatient clinics usually offer a combination of individual counseling and group counseling. Frequently a physician or psychiatrist will assist with prescriptions to assist with the side effects of the addiction (the most common side effect that the medications can help is anxiety).
Anti-addictive drugs
Other forms of treatment include replacement drugs such as methadone or buprenorphine, used as a substitute for illicit opiate drugs.[18][19] Although these drugs are themselves addictive, opioid dependency is often so strong that a way to stabilize levels of opioid needed and a way to gradually reduce the levels of opioid needed are required. In some countries, other opioid derivatives such as levomethadyl acetate,[20] dihydrocodeine,[21] dihydroetorphine[22] and even heroin[23][24] are used as substitute drugs for illegal street opiates, with different drugs being used depending on the needs of the individual patient.[25]
Substitute drugs for other forms of drug dependence have historically been less successful than opioid substitute treatment, but some limited success has been seen with drugs such as dexamphetamine to treat stimulant addiction,[26][27] and clomethiazole to treat alcohol addiction.[28]
Other pharmacological treatments for alcohol addiction include drugs like disulfiram, acamprosate and topiramate,[29][30] but rather than substituting for alcohol, these drugs are intended to reduce the desire to drink, either by directly reducing cravings as with acamprosate and topiramate, or by producing unpleasant effects when alcohol is consumed, as with disulfiram. These drugs can be effective if treatment is maintained, but compliance can be an issue as alcoholic patients often forget to take their medication, or discontinue use because of excessive side effects.[31][32] Additional drugs acting on glutamate neurotransmission such as modafinil, lamotrigine, gabapentin and memantine have also been proposed for use in treating addiction to alcohol and other drugs.[33]
Opioid antagonists such as naltrexone and nalmefene have also been used successfully in the treatment of alcohol addiction,[34][35] which is often particularly challenging to treat. These drugs have also been used to a lesser extent for long-term maintenance treatment of former opiate addicts, but cannot be started until the patient has been abstinent for an extended period, otherwise they can trigger acute opioid withdrawal symptoms.[36]
Treatment of stimulant addiction can often be difficult, with substitute drugs often being ineffective, although newer drugs such as nocaine, vanoxerine and modafinil may have more promise in this area, as well as the GABAB agonist baclofen.[37][38] Another strategy that has recently been successfully trialled used a combination of the benzodiazepine antagonist flumazenil with hydroxyzine and gabapentin for the treatment of methamphetamine addiction.[39]
Another area in which drug treatment has been widely used is in the treatment of nicotine addiction. Various drugs have been used for this purpose such as bupropion, mecamylamine and the more recently developed varenicline. The cannaboinoid antagonist rimonabant has also been trialled for treatment of nicotine addiction but has not been widely adopted for this purpose.[40][41][42]
Ibogaine is a psychoactive drug that specifically interrupts the addictive response, and is currently being studied for its effects upon cocaine, heroin, nicotine, and SSRI addicts. Alternative medicine clinics offering ibogaine treatment have appeared along the U.S. border.[43] Ibogaine treatment for drug addiction can be reasonably effective, but potentially dangerous side effects which have been linked to several deaths have limited its adoption by conventional medical practice.[44] A synthetic analogue of ibogaine, 18-methoxycoronaridine has also been developed which has similar efficacy but less side effects, however this drug is still being tested in animals and human trials have not yet been carried out.[45][46]
Alternative therapies
Alternative therapies, such as acupuncture, are used by some practitioners to alleviate the symptoms of drug addiction. In 1997, the American Medical Association (AMA) was adopted as policy following statement after a report on a number of alternative therapies including acupuncture:
There is little evidence to confirm the safety or efficacy of most alternative therapies. Much of the information currently known about these therapies makes it clear that many have not been shown to be efficacious. Well-designed, stringently controlled research should be done to evaluate the efficacy of alternative therapies.
Accupuncture has been shown to be no more effective than control treatments in the treatment of opiate dependence.[47] Acupuncture, acupressure, laser therapy and electrostimulation have no demonstrated efficacy for smoking cessation.[48]
Medical definitions
The terms abuse and addiction have been defined and re-defined over the years. The 1957 World Health Organization (WHO) Expert Committee on Addiction-Producing Drugs defined addiction and habituation as components of drug abuse:
Drug addiction is a state of periodic or chronic intoxication produced by the repeated consumption of a drug (natural or synthetic). Its characteristics include: (i) an overpowering desire or need (compulsion) to continue taking the drug and to obtain it by any means; (ii) a tendency to increase the dose; (iii) a psychic (psychological) and generally a physical dependence on the effects of the drug; and (iv) detrimental effects on the individual and on society.
Drug habituation (habit) is a condition resulting from the repeated consumption of a drug. Its characteristics include (i) a desire (but not a compulsion) to continue taking the drug for the sense of improved well-being which it engenders; (ii) little or no tendency to increase the dose; (iii) some degree of psychic dependence on the effect of the drug, but absence of physical dependence and hence of an abstinence syndrome [withdrawal], and (iv) detrimental effects, if any, primarily on the individual.
In 1964, a new WHO committee found these definitions to be inadequate, and suggested using the blanket term "drug dependence":
The definition of addiction gained some acceptance, but confusion in the use of the terms addiction and habituation and misuse of the former continued. Further, the list of drugs abused increased in number and diversity. These difficulties have become increasingly apparent and various attempts have been made to find a term that could be <applied to drug abuse generally. The component in common appears to be dependence, whether psychic or physical or both. Hence, use of the term 'drug dependence', with a modifying phase linking it to a particular drug type in order to differentiate one class of drugs from another, had been given most careful consideration. The Expert Committee recommends substitution of the term 'drug dependence' for the terms 'drug addiction' and 'drug habituation'.
The committee did not clearly define dependence, but did go on to clarify that there was a distinction between physical and psychological ("psychic") dependence. It said that drug abuse was "a state of psychic dependence or physical dependence, or both, on a drug, arising in a person following administration of that drug on a periodic or continued basis." Psychic dependence was defined as a state in which "there is a feeling of satisfaction and psychic drive that requires periodic or continuous administration of the drug to produce pleasure or to avoid discomfort" and all drugs were said to be capable of producing this state:
There is scarcely any agent which can be taken into the body to which some individuals will not get a reaction satisfactory or pleasurable to them, persuading them to continue its use even to the point of abuse — that is, to excessive or persistent use beyond medical need.
The 1957 and 1964 definitions of addiction, dependence and abuse persist to the present day in medical literature. It should be noted that at this time (2006) the Diagnostic Statistical Manual (DSM IVR) now spells out specific criteria for defining abuse and dependence. (DSM IVR) uses the term substance dependence instead of addiction; a maladaptive pattern of substance abuse, leading to clinically significant impairment or distress, as manifested by three (or more) specified criteria, occurring at any time in the same 12-month period. This definition is also applicable on drugs with smaller or nonexistent physical signs of withdrawal, for ex. cannabis.
In 2001, the American Academy of Pain Medicine, the American Pain Society, and the American Society of Addiction Medicine jointly issued "Definitions Related to the Use of Opioids for the Treatment of Pain," which defined the following terms [3]:
Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving.
Physical dependence is a state of adaptation that is manifested by a drug class specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist.
Tolerance is the body's physical adaptation to a drug: greater amounts of the drug are required over time to achieve the initial effect as the body "gets used to" and adapts to the intake.
Pseudo addiction is a term which has been used to describe patient behaviors that may occur when pain is undertreated. Patients with unrelieved pain may become focused on obtaining medications, may “clock watch,” and may otherwise seem inappropriately “drug seeking.” Even such behaviors as illicit drug use and deception can occur in the patient's efforts to obtain relief. Pseudoaddiction can be distinguished from true addiction in that the behaviors resolve when pain is effectively treated.
The Diagnostic and Statistical Manual of Mental Disorders, DSM-IV-TR doesn’t use the word addiction at all. Instead it has a section about Substance dependence
- "When an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed. Compulsive and repetitive use may result in tolerance to the effect of the drug and withdrawal symptoms when use is reduced or stopped. This, along with Substance Abuse are considered Substance Use Disorders...." [49]
Addiction (definition proposed by professor Nils Bejerot).
- "An emotional fixation (sentiment) acquired through learning, which intermittently or continually expresses itself in purposeful, stereotyped behavior with the character and force of a natural drive, aiming at a specific pleasure or the avoidance of a specific discomfort."[50]
Addiction and drug control legislation
Depending on the jurisdiction, addictive drugs may be legal only as part of a government sponsored study, illegal to use for any purpose, illegal to sell, or even illegal to merely possess.
Most countries have legislation which brings various drugs and drug-like substances under the control of licensing systems. Typically this legislation covers any or all of the opiates, amphetamines, cannabinoids, cocaine, barbiturates, hallucinogenics and a variety of more modern synthetic drugs, and unlicensed production, supply or possession is a criminal offence.
Usually, however, drug classification under such legislation is not related simply to addictiveness. The substances covered often have very different addictive properties. Some are highly prone to cause physical dependency, whilst others rarely cause any form of compulsive need whatsoever. Also, under legislation specifically about drugs, alcohol is not usually included.
Although the legislation may be justifiable on moral or public health grounds, it can make addiction or dependency a much more serious issue for the individual: reliable supplies of a drug become difficult to secure, and the individual becomes vulnerable to both criminal abuse and legal punishment.
It is unclear whether laws against drugs do anything to stem usage and dependency. In jurisdictions where addictive drugs are illegal, they are generally supplied by drug dealers, who are often involved with organized crime. Even though the cost of producing most illegal addictive substances is very low, their illegality combined with the addict's need permits the seller to command a premium price, often hundreds of times the production cost. As a result, the addict sometimes turns to crime to support their habit.
History of addiction
The phenomenon of drug addiction has occurred to some degree throughout recorded history (see "opium"), though modern agricultural practices, improvements in access to drugs, advancements in biochemistry, and dramatic increases in the recommendation of drug usage by clinical practitioners have exacerbated the problem significantly in the 20th century. Improved means of active biological agent manufacture and the introduction of synthetic compounds, such as methamphetamine are also factors contributing to drug addiction.
In 1971, United States President Richard Nixon declared a war on illegal drugs in an attempt to control the growing problem of drug addiction and drug-related crime.
See also
- Addiction
- Addiction recovery groups
- Alcoholism
- Arguments for and against drug prohibition
- Demand reduction
- Drug abuse
- Drug policy
- Drugs and prostitution
- Drug Mix
- Drug tolerance
- Drug Intervention Program
- DSM-IV Codes
- Harm reduction
- Nils Bejerot
- Physical dependence
- Psychoactive drug
- Tachyphylaxis
- Treatment Improvement Protocols
- Rat Park
- Rational addiction
- Robinson v. California (1964), decision by the U.S. Supreme Court that states cannot criminalize narcotics addiction itself
- Substance dependence
Literature
- Sainsbury, Drug and the Drug Habit (New York, 1909)
- C. A. McBride, Modern Treatment of Alcoholism and Drug Narcotism (New York, 1910)
- G. E. Pettey, Narcotic Drug Diseases and Allied Ailments (Philadelphia, 1913)
- Fitz Hugh Ludlow wrote The Hasheesh Eater (1857) and The Opium Habit (1868), designed as a warning.
- Thomas de Quincey, Confessions of an English Opium Eater (London, 1822)
- William S. Burroughs, Junkie (New York, 1953)
References
- ↑ Nutt D, King LA, Saulsbury W, Blakemore C (2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet. 369 (9566): 1047–53. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831.
- ↑ 2.0 2.1 2.2 2.3 2.4 Koob G, Kreek MJ (2007). "Stress, dysregulation of drug reward pathways, and the transition to drug dependence". Am J Psychiatry. 164 (8): 1149–59. doi:10.1176/appi.ajp.2007.05030503. PMID 17671276.
- ↑ 3.0 3.1 2001 "Definitions Related to the Use of Opioids for the Treatment of Pain,", the American Academy of Pain Medicine, the American Pain Society, and the American Society of Addiction Medicine
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Kalivas PW, Volkow ND (2005). "The neural basis of addiction: a pathology of motivation and choice". Am J Psychiatry. 162 (8): 1403–13. doi:10.1176/appi.ajp.162.8.1403. PMID 16055761.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Jones S, Bonci A (2005). "Synaptic plasticity and drug addiction". Curr Opin Pharmacol. 5 (1): 20–5. doi:10.1016/j.coph.2004.08.011. PMID 15661621.
- ↑ 6.0 6.1 6.2 Eisch AJ, Harburg GC (2006). "Opiates, psychostimulants, and adult hippocampal neurogenesis: Insights for addiction and stem cell biology". Hippocampus. 16 (3): 271–86. doi:10.1002/hipo.20161. PMID 16411230.
- ↑ Rang, H. P. (2003). Pharmacology. Edinburgh: Churchill Livingstone. pp. page 596. ISBN 0-443-07145-4.
- ↑ 8.0 8.1 Kourrich S, Rothwell PE, Klug JR, Thomas MJ (2007). "Cocaine experience controls bidirectional synaptic plasticity in the nucleus accumbens". J. Neurosci. 27 (30): 7921–8. doi:10.1523/JNEUROSCI.1859-07.2007. PMID 17652583.
- ↑ 9.0 9.1 Floresco SB, Ghods-Sharifi S (2007). "Amygdala-prefrontal cortical circuitry regulates effort-based decision making". Cereb. Cortex. 17 (2): 251–60. doi:10.1093/cercor/bhj143. PMID 16495432.
- ↑ Bahi A, Dreyer JL (2005). "Cocaine-induced expression changes of axon guidance molecules in the adult rat brain". Mol. Cell. Neurosci. 28 (2): 275–91. doi:10.1016/j.mcn.2004.09.011. PMID 15691709.
- ↑ Noel Pearson: Agendas of addiction, 2008
- ↑ Nils Bejerot: Swedish addiction epidemic in an international perspective, 1988
- ↑ Ball JC, van de Wijngaart GF (1994). "A Dutch addict's view of methadone maintenance--an American and a Dutch appraisal". Addiction. 89 (7): 799–802, discussion 803–14. PMID 8081178.
- ↑ Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A (2005). "Co-morbid post-traumatic stress disorder in a substance misusing clinical population". Drug Alcohol Depend. 77 (3): 251–8. doi:10.1016/j.drugalcdep.2004.08.017. PMID 15734225.
- ↑ Moggi F, Giovanoli A, Strik W, Moos BS, Moos RH (2007). "Substance use disorder treatment programs in Switzerland and the USA: Program characteristics and 1-year outcomes". Drug Alcohol Depend. 86 (1): 75–83. doi:10.1016/j.drugalcdep.2006.05.017. PMID 16782286.
- ↑ {http://www.rns.se/swedish-addiction.asp Nils Bejerot: The Swedish Addiction Epidemic in global perspective]
- ↑ http://www.nida.nih.gov/Infofacts/treatmeth.html
- ↑ Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE (2000). "A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence". N. Engl. J. Med. 343 (18): 1290–7. doi:10.1056/NEJM200011023431802. PMID 11058673.
- ↑ Connock M, Juarez-Garcia A, Jowett S; et al. (2007). "Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation". Health Technol Assess. 11 (9): 1–171, iii–iv. PMID 17313907.
- ↑ Marsch LA, Stephens MA, Mudric T, Strain EC, Bigelow GE, Johnson RE (2005). "Predictors of outcome in LAAM, buprenorphine, and methadone treatment for opioid dependence". Exp Clin Psychopharmacol. 13 (4): 293–302. doi:10.1037/1064-1297.13.4.293. PMID 16366759.
- ↑ Robertson JR, Raab GM, Bruce M, McKenzie JS, Storkey HR, Salter A (2006). "Addressing the efficacy of dihydrocodeine versus methadone as an alternative maintenance treatment for opiate dependence: A randomized controlled trial". Addiction. 101 (12): 1752–9. doi:10.1111/j.1360-0443.2006.01603.x. PMID 17156174.
- ↑ Qin Bo-Yi (1998). "Advances in dihydroetorphine: From analgesia to detoxification". Drug Development Research. 39 (2): 131–134. Link
- ↑ Metrebian N, Shanahan W, Wells B, Stimson GV (1998). "Feasibility of prescribing injectable heroin and methadone to opiate-dependent drug users: associated health gains and harm reductions". Med. J. Aust. 168 (12): 596–600. PMID 9673620.
- ↑ Metrebian N, Mott J, Carnwath Z, Carnwath T, Stimson GV, Sell L (2007). "Pathways into receiving a prescription for diamorphine (heroin) for the treatment of opiate dependence in the United kingdom". Eur Addict Res. 13 (3): 144–7. doi:10.1159/000101550. PMID 17570910.
- ↑ Kenna GA, Nielsen DM, Mello P, Schiesl A, Swift RM (2007). "Pharmacotherapy of dual substance abuse and dependence". CNS Drugs. 21 (3): 213–37. doi:10.2165/00023210-200721030-00003. PMID 17338593.
- ↑ Mattick RP, Darke S (1995). "Drug replacement treatments: is amphetamine substitution a horse of a different colour?". Drug Alcohol Rev. 14 (4): 389–94. doi:10.1080/09595239500185531. PMID 16203339.
- ↑ White R (2000). "Dexamphetamine substitution in the treatment of amphetamine abuse: an initial investigation". Addiction. 95 (2): 229–38. PMID 10723851.
- ↑ Majumdar SK (1991). "Chlormethiazole: current status in the treatment of the acute ethanol withdrawal syndrome". Drug Alcohol Depend. 27 (3): 201–7. doi:10.1016/0376-8716(91)90001-F. PMID 1884662.
- ↑ Soyka M, Roesner S (2006). "New pharmacological approaches for the treatment of alcoholism". Expert Opin Pharmacother. 7 (17): 2341–53. doi:10.1517/14656566.7.17.2341. PMID 17109610.
- ↑ Pettinati HM, Rabinowitz AR (2006). "Choosing the right medication for the treatment of alcoholism". Curr Psychiatry Rep. 8 (5): 383–8. doi:10.1007/s11920-006-0040-0. PMID 16968619.
- ↑ Bouza C, Angeles M, Magro A, Muñoz A, Amate JM (2004). "Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review". Addiction. 99 (7): 811–28. doi:10.1111/j.1360-0443.2004.00763.x. PMID 15200577.
- ↑ Williams SH (2005). "Medications for treating alcohol dependence". Am Fam Physician. 72 (9): 1775–80. PMID 16300039.
- ↑ Gass JT, Olive MF (2008). "Glutamatergic substrates of drug addiction and alcoholism". Biochem. Pharmacol. 75 (1): 218–65. doi:10.1016/j.bcp.2007.06.039. PMID 17706608.
- ↑ Srisurapanont M, Jarusuraisin N (2005). "Opioid antagonists for alcohol dependence". Cochrane Database Syst Rev (1): CD001867. doi:10.1002/14651858.CD001867.pub2. PMID 15674887.
- ↑ Karhuvaara S, Simojoki K, Virta A; et al. (2007). "Targeted nalmefene with simple medical management in the treatment of heavy drinkers: a randomized double-blind placebo-controlled multicenter study". Alcohol. Clin. Exp. Res. 31 (7): 1179–87. doi:10.1111/j.1530-0277.2007.00401.x. PMID 17451401.
- ↑ Comer SD, Sullivan MA, Hulse GK (2007). "Sustained-release naltrexone: novel treatment for opioid dependence". Expert Opin Investig Drugs. 16 (8): 1285–94. doi:10.1517/13543784.16.8.1285. PMID 17685876.
- ↑ Ling W, Rawson R, Shoptaw S, Ling W (2006). "Management of methamphetamine abuse and dependence". Curr Psychiatry Rep. 8 (5): 345–54. doi:10.1007/s11920-006-0035-x. PMID 16968614.
- ↑ Preti A (2007). "New developments in the pharmacotherapy of cocaine abuse". Addict Biol. 12 (2): 133–51. doi:10.1111/j.1369-1600.2007.00061.x. PMID 17508985.
- ↑ Urschel HC, Hanselka LL, Gromov I, White L, Baron M (2007). "Open-label study of a proprietary treatment program targeting type A gamma-aminobutyric acid receptor dysregulation in methamphetamine dependence". Mayo Clin. Proc. 82 (10): 1170–8. PMID 17908523.
- ↑ Garwood CL, Potts LA (2007). "Emerging pharmacotherapies for smoking cessation". Am J Health Syst Pharm. 64 (16): 1693–8. doi:10.2146/ajhp060427. PMID 17687057.
- ↑ Frishman WH (2007). "Smoking cessation pharmacotherapy--nicotine and non-nicotine preparations". Prev Cardiol. 10 (2 Suppl 1): 10–22. doi:10.1111/j.1520-037X.2007.05963.x. PMID 17396063.
- ↑ Siu EC, Tyndale RF (2007). "Non-nicotinic therapies for smoking cessation". Annu. Rev. Pharmacol. Toxicol. 47: 541–64. doi:10.1146/annurev.pharmtox.47.120505.105354. PMID 17209799.
- ↑ Alper KR, Lotsof HS, Kaplan CD (2008). "The ibogaine medical subculture". J Ethnopharmacol. 115 (1): 9–24. doi:10.1016/j.jep.2007.08.034. PMID 18029124.
- ↑ Mash DC, Kovera CA, Pablo J; et al. (2000). "Ibogaine: complex pharmacokinetics, concerns for safety, and preliminary efficacy measures". Ann. N. Y. Acad. Sci. 914: 394–401. PMID 11085338.
- ↑ Levi MS, Borne RF (2002). "A review of chemical agents in the pharmacotherapy of addiction". Curr. Med. Chem. 9 (20): 1807–18. PMID 12369879.
- ↑ Werneke U, Turner T, Priebe S (2006). "Complementary medicines in psychiatry: review of effectiveness and safety". Br J Psychiatry. 188: 109–21. doi:10.1192/bjp.188.2.109. PMID 16449696.
- ↑ Jordan JB (2006). "Acupuncture treatment for opiate addiction: a systematic review". J Subst Abuse Treat. 30 (4): 309–14. doi:10.1016/j.jsat.2006.02.005. PMID 16716845.
- ↑ White AR, Rampes H, Campbell JL (2006). "Acupuncture and related interventions for smoking cessation". Cochrane Database Syst Rev (1): CD000009. doi:10.1002/14651858.CD000009.pub2. PMID 16437420.
- ↑ DSM-IV & DSM-IV-TR:Substance Dependence
- ↑ Nils Bejerot in Theories of Drug abuse, Selected contemporary perspectives, page 246-255, NIDA, 1980
Sources
- The Cult of Pharmacology: How America Became the Most Troubled Drug Culture by Richard DeGrandpre, Duke University Press, 2006.
- Nestler, Eric and Malenka, Robert (March 2004). "The Addicted Brain". Scientific American, pg. 78-83.
- Leavitt, Fred (2003) The REAL Drug Abusers. Rowman & Littlefield.
bn:মাদকাসক্তি
bg:Пристрастяване
ca:Addicció
cs:Závislost
da:Narkoman
de:Missbrauch und Abhängigkeit
et:Sõltuvus (narkoloogia)
eo:Droga dependeco
fa:اعتیاد
gl:Adicción
ko:중독
hy:Թմրամոլություն
hr:Ovisnost
id:Kecanduan
is:Fíkn
it:Tossicodipendenza
he:התמכרות
lt:Narkomanija
hu:Függőség
nl:Verslaving
no:Narkomani
oc:Adiccion
scn:Divotu (idiali)
simple:Drug addiction
sr:Наркоманија
sh:Ovisnost
fi:Päihderiippuvuus
sv:Narkomani
uk:Наркоманія