Pericarditis pathophysiology: Difference between revisions
Homa Najafi (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (4 intermediate revisions by one other user not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Pericarditis is [[inflammation]] of the [[pericardium]], which is the double-walled sac that contains the [[heart]] and the roots of the [[great vessels]]. There can be an accompanying accumulation of fluid that can be either [[serous]] (free flowing fluid) or [[fibrinous]] (an [[exudate]], which is a thick fluid composed of proteins, [[fibrin]] strands, inflammatory cells, cell breakdown products, and sometimes [[bacteria]]). Vascular congestion of the [[pericardium]] is also present. The underlying [[myocardium]] may or may not be inflamed as well. If the [[myocardium]] is involved in the [[inflammatory process]], it is called myopericarditis, and [[CK]] and [[troponin]] levels may be elevated. | Pericarditis is [[inflammation]] of the [[pericardium]], which is the double-walled sac that contains the [[heart]] and the roots of the [[great vessels]]. There can be an accompanying accumulation of [[fluid]] that can be either [[serous]] (free flowing [[fluid]]) or [[fibrinous]] (an [[exudate]], which is a thick [[fluid]] composed of [[proteins]], [[fibrin]] strands, [[inflammatory cells]], [[cell]] breakdown products, and sometimes [[bacteria]]). [[Vascular congestion]] of the [[pericardium]] is also present. The underlying [[myocardium]] may or may not be [[inflamed]] as well. If the [[myocardium]] is involved in the [[inflammatory process]], it is called [[myopericarditis]], and [[CK]] and [[troponin]] levels may be elevated. [[Cardio|Cardiotropic]] [[viruses]] usually spread to the [[myocardium]] and [[pericardium]] [[Hematogen|hematogenously]] and cause [[acute]] [[inflammation]] with [[Infiltration (medical)|infiltration]] of [[Polymorphonuclear cells|polymorphonuclear]] ([[PMN]]) [[leukocytes]] and [[pericardial]] vascularization. Most [[patients]] with [[viral]] pericarditis recover completely with few developing recurrences. Some [[patients]] develop [[constrictive pericarditis]] which could be disabling. [[Bacterial]] pericarditis results from [[contiguous]] spread of [[infection]] within the [[chest]], either [[de novo]] or after [[surgery]] or [[trauma]], spread from [[infective endocarditis]], [[Hematogen|hematogenous]], or direct [[inoculation]] as a result of [[Penetrating trauma|penetrating injury]] or [[cardiothoracic surgery]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 53: | Line 53: | ||
* [[Constrictive pericarditis]] occurs when there is a [[scar]] encasing, the [[heart]] that [[Chronic (medicine)|chronically]] constricts the filling of the [[heart]]. | * [[Constrictive pericarditis]] occurs when there is a [[scar]] encasing, the [[heart]] that [[Chronic (medicine)|chronically]] constricts the filling of the [[heart]]. | ||
* [[Cardiac tamponade]] is a [[medical emergency]] in which [[fluid]] in the [[pericardial sac]] [[Acute (medicine)|acutely]] restricts the filling of the [[heart]]. This requires [[Surgery|surgical]] drainage or [[pericardiocentesis]]. | * [[Cardiac tamponade]] is a [[medical emergency]] in which [[fluid]] in the [[pericardial sac]] [[Acute (medicine)|acutely]] restricts the filling of the [[heart]]. This requires [[Surgery|surgical]] drainage or [[pericardiocentesis]]. | ||
<br /> | |||
==== Additional Images ==== | |||
| Line 67: | Line 71: | ||
===Pathogenesis=== | |||
*Cardiotropic [[viruses]] usually spread to the [[myocardium]] and [[pericardium]] [[Hematogen|hematogenously]] and cause [[acute]] [[inflammation]] with [[Infiltration (medical)|infiltration]] of [[Polymorphonuclear cells|polymorphonuclear]] ([[PMN]]) [[leukocytes]] and [[pericardial]] vascularization. This may cause [[pericardial effusion]] and [[fibrinous]] change of the [[pericardium]]. The [[pericardium]] may also develop a [[serous]] or [[hemorrhagic]] effusion. Most [[patients]] with [[viral]] pericarditis recover completely with few developing recurrences. Some [[patients]] develop [[constrictive pericarditis]] which could be disabling.<ref name="pmid5489188">{{cite journal| author=Matthews JD, Cameron SJ, George M| title=Constrictive pericarditis following Coxsackie virus infection. | journal=Thorax | year= 1970 | volume= 25 | issue= 5 | pages= 624-6 | pmid=5489188 | doi= | pmc=PMC472200 | url= }} </ref><ref name="pmid1920818">{{cite journal| author=Ilan Y, Oren R, Ben-Chetrit E| title=Acute pericarditis: etiology, treatment and prognosis. A study of 115 patients. | journal=Jpn Heart J | year= 1991 | volume= 32 | issue= 3 | pages= 315-21 | pmid=1920818 | doi= | pmc= | url= }} </ref><ref name="pmid2249218">{{cite journal| author=Shabetai R| title=Acute pericarditis. | journal=Cardiol Clin | year= 1990 | volume= 8 | issue= 4 | pages= 639-44 | pmid=2249218 | doi= | pmc= | url= }} </ref> | |||
=== | *[[Bacterial]] pericarditis results from:<ref name="pmid930941">{{cite journal| author=Klacsmann PG, Bulkley BH, Hutchins GM| title=The changed spectrum of purulent pericarditis: an 86 year autopsy experience in 200 patients. | journal=Am J Med | year= 1977 | volume= 63 | issue= 5 | pages= 666-73 | pmid=930941 | doi= | pmc= | url= }} </ref><ref name="pmid4200204">{{cite journal| author=Kauffman CA, Watanakunakorn C, Phair JP| title=Purulent pneumococcal pericarditis. A continuing problem in the antibiotic era. | journal=Am J Med | year= 1973 | volume= 54 | issue= 6 | pages= 743-50 | pmid=4200204 | doi= | pmc= | url= }} </ref><ref name="pmid1138554">{{cite journal| author=Rubin RH, Moellering RC| title=Clinical, microbiologic and therapeutic aspects of purulent pericarditis. | journal=Am J Med | year= 1975 | volume= 59 | issue= 1 | pages= 68-78 | pmid=1138554 | doi= | pmc= | url= }} </ref><ref name="pmid4076207">{{cite journal| author=Ribeiro P, Shapiro L, Nihoyannopoulos P, Gonzalez A, Oakley CM| title=Pericarditis in infective endocarditis. | journal=Eur Heart J | year= 1985 | volume= 6 | issue= 11 | pages= 975-8 | pmid=4076207 | doi= | pmc= | url= }} </ref><ref name="pmid4402567">{{cite journal| author=Roberts WC, Buchbinder NA| title=Right-sided valvular infective endocarditis. A clinicopathologic study of twelve necropsy patients. | journal=Am J Med | year= 1972 | volume= 53 | issue= 1 | pages= 7-19 | pmid=4402567 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4402567 }} </ref> | ||
#[[Contiguous]] spread of [[infection]] within the [[chest]], either [[de novo]] or after [[surgery]] or [[trauma]]. | |||
#Spread from [[infective endocarditis]] | |||
#[[Hematogen|Hematogenous]] spread of [[infection]] | |||
#Direct [[inoculation]] as a result of [[Penetrating trauma|penetrating injury]] or [[cardiothoracic surgery]] | |||
=== | |||
* | *[[Tuberculous]] pericarditis develops from [[lymphatic]] spread of peritracheal, peribronchial or [[mediastinal]] [[lymph nodes]] or by [[contiguous]] spread from a focus of [[infection]] in the [[lung]] or [[pleura]]. There are four pathologic stages observed:<ref name="pmid18610109">{{cite journal| author=Peel AA| title=TUBERCULOUS PERICARDITIS. | journal=Br Heart J | year= 1948 | volume= 10 | issue= 3 | pages= 195-207 | pmid=18610109 | doi= | pmc=PMC481044 | url= }} </ref><ref name="pmid4050698">{{cite journal| author=Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J| title=Primary acute pericardial disease: a prospective series of 231 consecutive patients. | journal=Am J Cardiol | year= 1985 | volume= 56 | issue= 10 | pages= 623-30 | pmid=4050698 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4050698 }} </ref><ref name="pmid16330703">{{cite journal| author=Mayosi BM, Burgess LJ, Doubell AF| title=Tuberculous pericarditis. | journal=Circulation | year= 2005 | volume= 112 | issue= 23 | pages= 3608-16 | pmid=16330703 | doi=10.1161/CIRCULATIONAHA.105.543066 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16330703 }} </ref> | ||
* | :*Stage 1: Presence of [[diffuse]] [[fibrin]] [[Deposition (chemistry)|deposition]], [[granuloma]]s and abundant [[mycobacterium]]. | ||
:*Stage 2: Development of [[serous]] or serosanguineous [[pericardial effusion]] with a predominantly lymphocytic exudate with [[monocyte]]s and foam cells. | :*Stage 2: Development of [[serous]] or [[Serosanguineous discharge|serosanguineous]] [[pericardial effusion]] with a predominantly [[lymphocytic]] [[exudate]] with [[monocyte]]s and [[foam cells]]. | ||
:*Stage 3: Absorption of effusion with organization of granulomatous caseation and thickening of pericardium secondary to deposition of [[fibrin]] and [[collagen]]. | :*Stage 3: [[Absorption]] of effusion with the organization of [[granulomatous]] caseation and thickening of [[pericardium]] [[secondary]] to [[Deposition (chemistry)|deposition]] of [[fibrin]] and [[collagen]]. | ||
:*Stage 4: Development of [[constrictive pericarditis]]. The pericardial space is obliterated by dense adhesions with marked thickening of parietal layer and replacement of [[granuloma]]s by fibrous tissue. | :*Stage 4: [[Development]] of [[constrictive pericarditis]]. The [[pericardial space]] is obliterated by [[dense]] [[adhesions]] with marked thickening of the parietal layer and replacement of [[granuloma]]s by [[fibrous]] [[tissue]]. | ||
:These types of [[granulomatous]] pericarditis also occur with [[fungal infection]]s, [[rheumatoid arthritis]] (RA), and [[sarcoidosis]]. | :These types of [[granulomatous]] pericarditis also occur with [[fungal infection]]s, [[rheumatoid arthritis]] ([[RA]]), and [[sarcoidosis]]. | ||
*Pericarditis in [[renal failure]] is thought to result from [[inflammation]] of the visceral and parietal layers of the pericardium by metabolic toxins such as [[urea]], [[creatinine]], [[uric acid]], methylguanidine, [[guanidinoacetate]], [[parathyroid hormone]], [[Beta-2 microglobulin|beta2-microglobulin]], and others. It may be associated with hemorrhagic or [[serous]] effusion. | *Pericarditis in [[renal failure]] is thought to result from [[inflammation]] of the [[visceral]] and [[parietal]] layers of the [[pericardium]] by [[metabolic]] [[toxins]] such as [[urea]], [[creatinine]], [[uric acid]], methylguanidine, [[guanidinoacetate]], [[parathyroid hormone]], [[Beta-2 microglobulin|beta2-microglobulin]], and others. It may be associated with [[hemorrhagic]] or [[serous]] effusion. | ||
==Gross Pathology Images== | ==Gross Pathology Images== | ||
| Line 217: | Line 216: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
Latest revision as of 23:39, 29 July 2020
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pericarditis pathophysiology |
|
Risk calculators and risk factors for Pericarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Varun Kumar, M.B.B.S., Cafer Zorkun, M.D., Ph.D. [2], Rim Halaby Homa Najafi, M.D.[3]
Overview
Pericarditis is inflammation of the pericardium, which is the double-walled sac that contains the heart and the roots of the great vessels. There can be an accompanying accumulation of fluid that can be either serous (free flowing fluid) or fibrinous (an exudate, which is a thick fluid composed of proteins, fibrin strands, inflammatory cells, cell breakdown products, and sometimes bacteria). Vascular congestion of the pericardium is also present. The underlying myocardium may or may not be inflamed as well. If the myocardium is involved in the inflammatory process, it is called myopericarditis, and CK and troponin levels may be elevated. Cardiotropic viruses usually spread to the myocardium and pericardium hematogenously and cause acute inflammation with infiltration of polymorphonuclear (PMN) leukocytes and pericardial vascularization. Most patients with viral pericarditis recover completely with few developing recurrences. Some patients develop constrictive pericarditis which could be disabling. Bacterial pericarditis results from contiguous spread of infection within the chest, either de novo or after surgery or trauma, spread from infective endocarditis, hematogenous, or direct inoculation as a result of penetrating injury or cardiothoracic surgery.
Pathophysiology
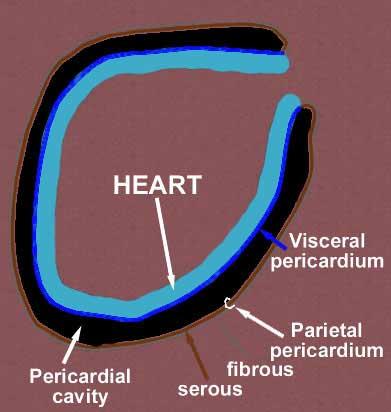
Anatomy and Physiology of Pericardium
Layers of the Pericardium
- The pericardium is made up of two layers:[1][2][3]
- Fibrous pericardium:
- Hard protective external layer
- Attached to sternum anteriorly by sterno-pericardial ligaments and fused with the central tendon of the diaphragm and great vessels to allow mobility of the pericardial sac against sudden cardiac overfilling
- Serous pericardium:
- Smooth internal layer made up of 2 components:
- Parietal: reflects onto fibrous pericardium
- Visceral: reflects onto heart and great vessels and forms the epicardium, the external layer of the heart wall
- Smooth internal layer made up of 2 components:
- Fibrous pericardium:
- Pericardial cavity: Potential space between parietal and visceral layers. It contains a serous fluid film that occupies the cavity and functions as lubricant against friction by all chest movements.
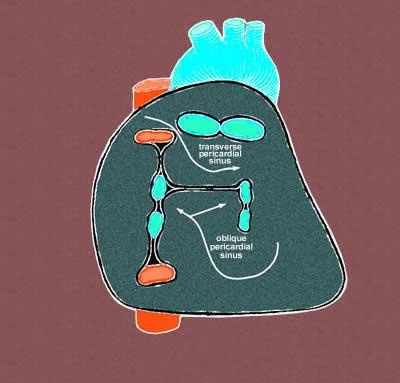
Pericardial Sinuses
- There are two small chambers or sinuses located where the visceral and parietal pericardium are continuous with one another within the pericardial cavity.[4][5][6]
- Transverse sinus:
- Located posterior to the pulmonary trunk and ascending aorta at the level between the superior vena cava and aortic arch
- Formed after dorsal myocardium ruptured embryonically
- Functional role is to allow the unhindered expansion of great arteries posteriorly during cardiac systole
- Utilized surgically to pass surgical clamps or place ligatures around great arteries.
- Oblique sinus:
- A blind recess (cul-de-sac) posterior to the left atrium between superior vena cava, right and left pulmonary veins inferior to the transverse sinus
- Formed embryonically by the incorporation of the pulmonary vein tributaries into the left atrium
- Functional role believed to be the expansion of the left atrium upon normal collapse of the thorax
Diseases of the Pericardium
- Pericarditis is an inflammatory condition of the pericardium.
- Pericardial effusion is fluid accumulation in the pericardial sac.
- Constrictive pericarditis occurs when there is a scar encasing, the heart that chronically constricts the filling of the heart.
- Cardiac tamponade is a medical emergency in which fluid in the pericardial sac acutely restricts the filling of the heart. This requires surgical drainage or pericardiocentesis.
Additional Images
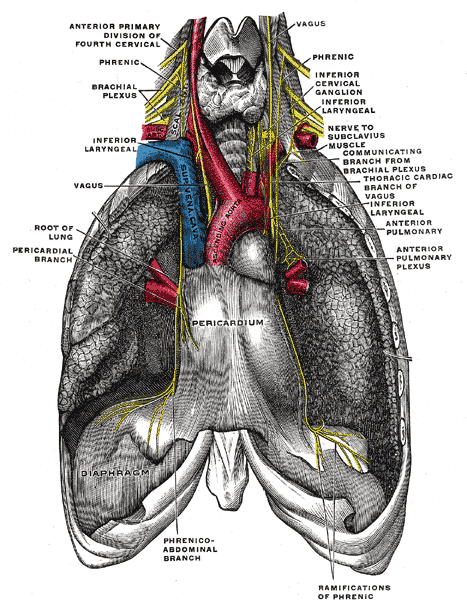
-
The phrenic nerve and its relations with the vagus nerve.
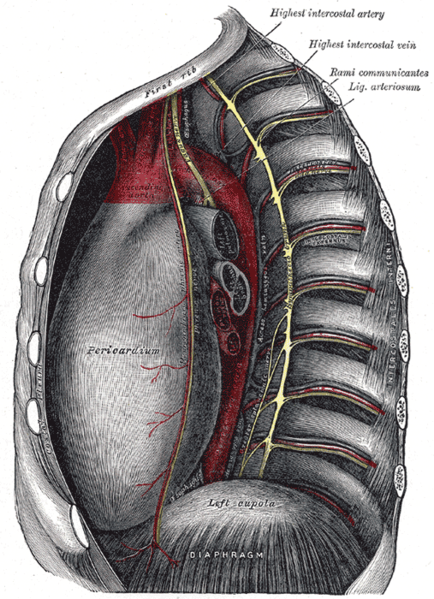
-
Thoracic portion of the sympathetic trunk.
-
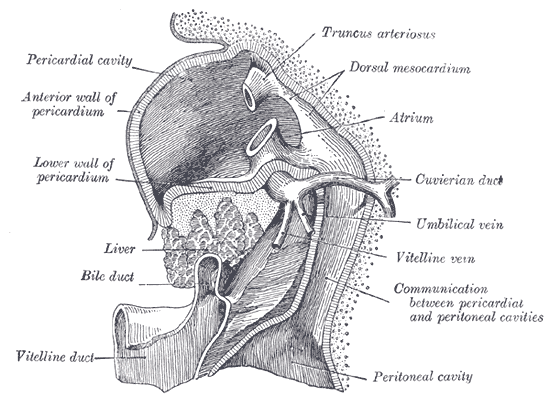
Liver with the septum transversum. Human embryo 3 mm long.
-
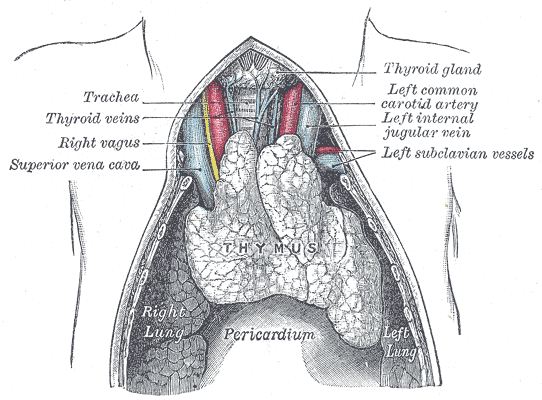
The thymus of a full-time fetus, exposed in situ.
Pathogenesis
- Cardiotropic viruses usually spread to the myocardium and pericardium hematogenously and cause acute inflammation with infiltration of polymorphonuclear (PMN) leukocytes and pericardial vascularization. This may cause pericardial effusion and fibrinous change of the pericardium. The pericardium may also develop a serous or hemorrhagic effusion. Most patients with viral pericarditis recover completely with few developing recurrences. Some patients develop constrictive pericarditis which could be disabling.[7][8][9]
- Contiguous spread of infection within the chest, either de novo or after surgery or trauma.
- Spread from infective endocarditis
- Hematogenous spread of infection
- Direct inoculation as a result of penetrating injury or cardiothoracic surgery
- Tuberculous pericarditis develops from lymphatic spread of peritracheal, peribronchial or mediastinal lymph nodes or by contiguous spread from a focus of infection in the lung or pleura. There are four pathologic stages observed:[15][16][17]
- Stage 1: Presence of diffuse fibrin deposition, granulomas and abundant mycobacterium.
- Stage 2: Development of serous or serosanguineous pericardial effusion with a predominantly lymphocytic exudate with monocytes and foam cells.
- Stage 3: Absorption of effusion with the organization of granulomatous caseation and thickening of pericardium secondary to deposition of fibrin and collagen.
- Stage 4: Development of constrictive pericarditis. The pericardial space is obliterated by dense adhesions with marked thickening of the parietal layer and replacement of granulomas by fibrous tissue.
- These types of granulomatous pericarditis also occur with fungal infections, rheumatoid arthritis (RA), and sarcoidosis.
- Pericarditis in renal failure is thought to result from inflammation of the visceral and parietal layers of the pericardium by metabolic toxins such as urea, creatinine, uric acid, methylguanidine, guanidinoacetate, parathyroid hormone, beta2-microglobulin, and others. It may be associated with hemorrhagic or serous effusion.
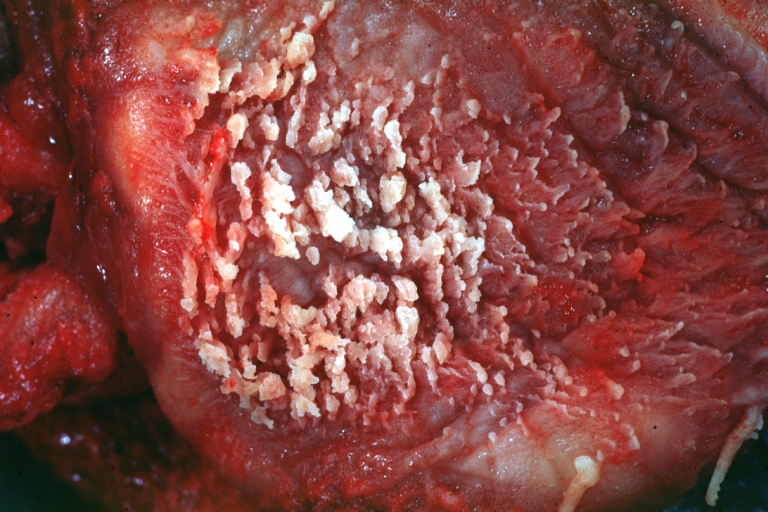
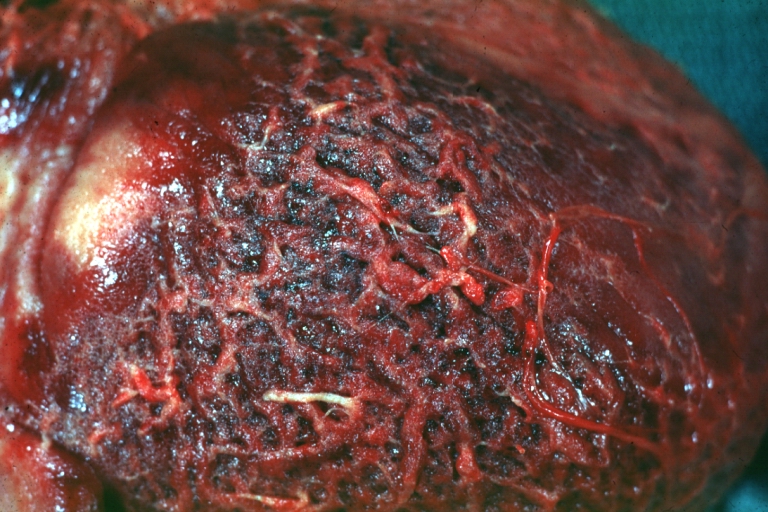
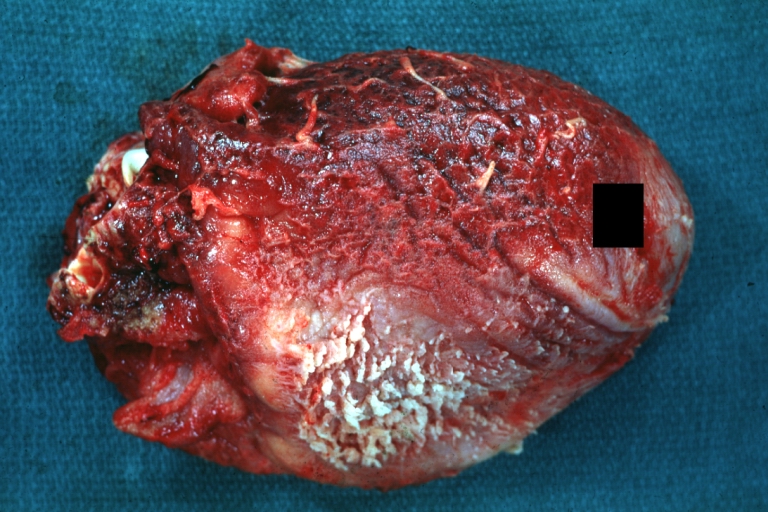
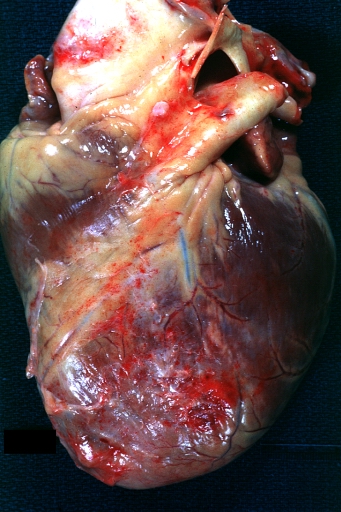
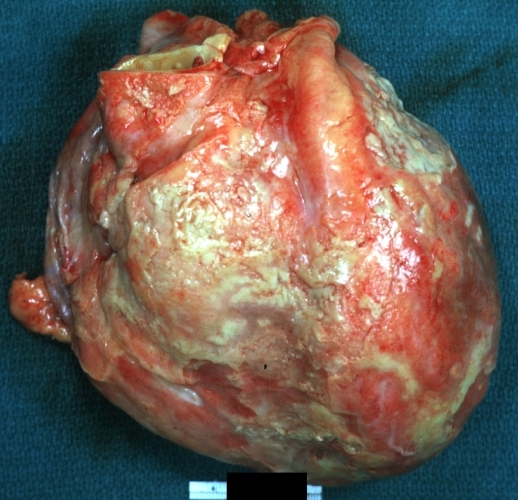
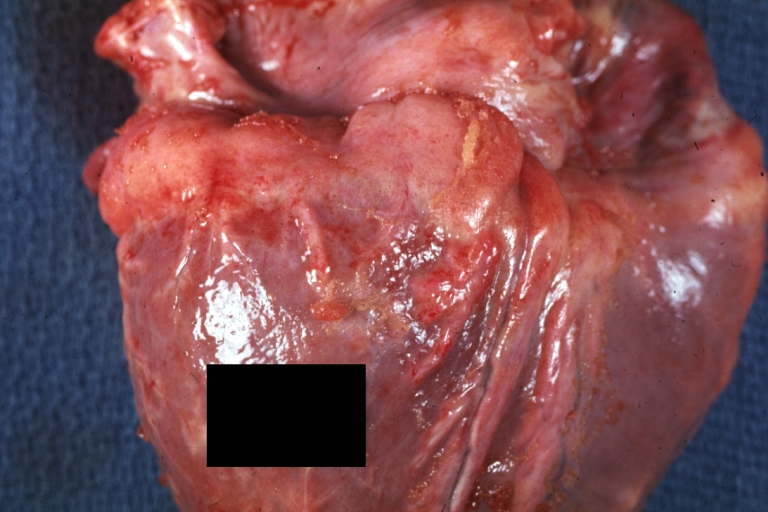
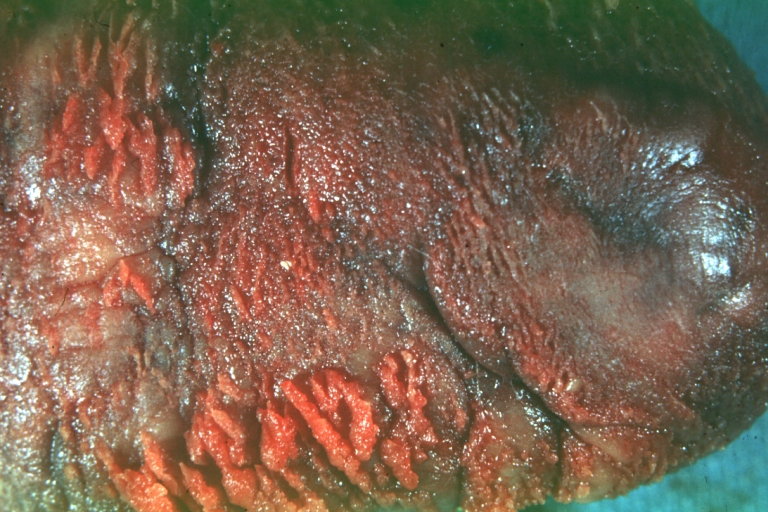
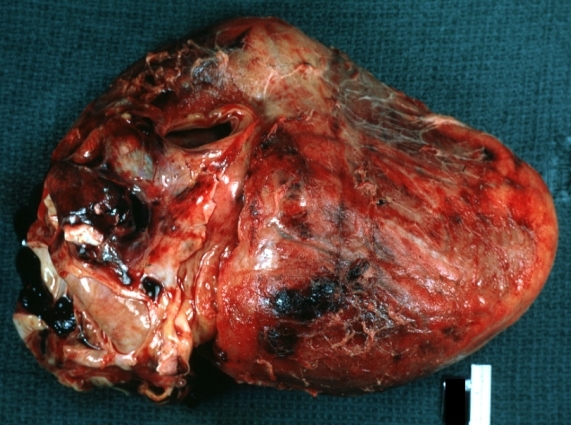
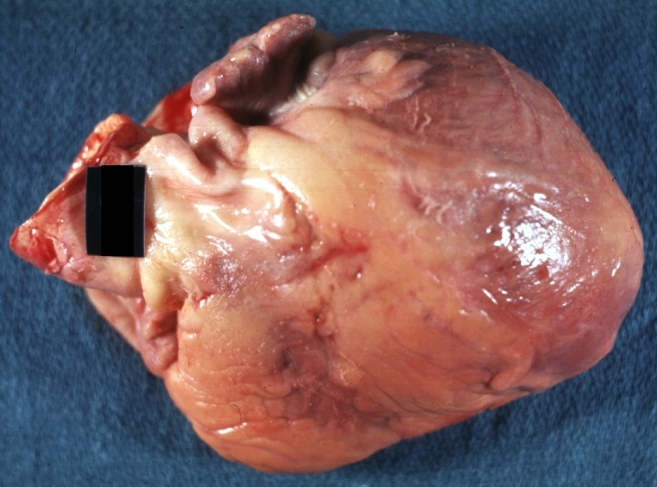
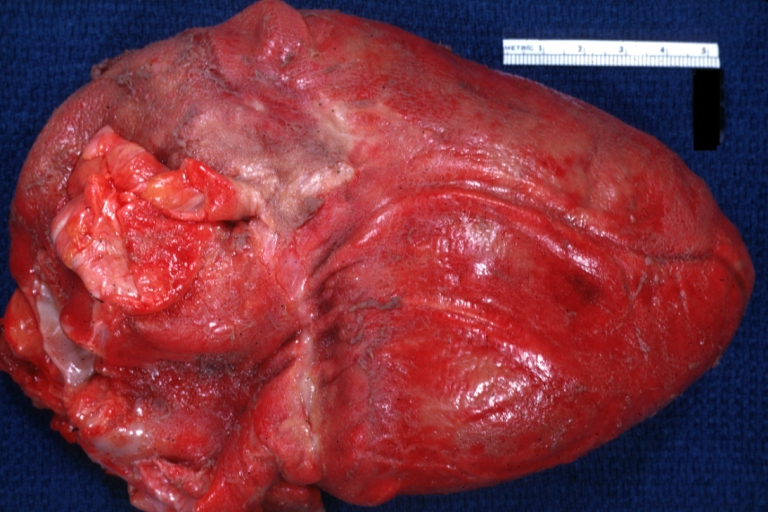
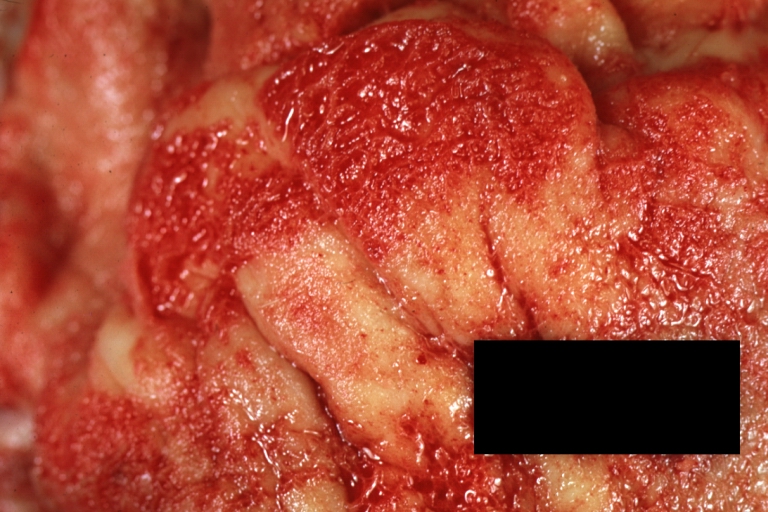
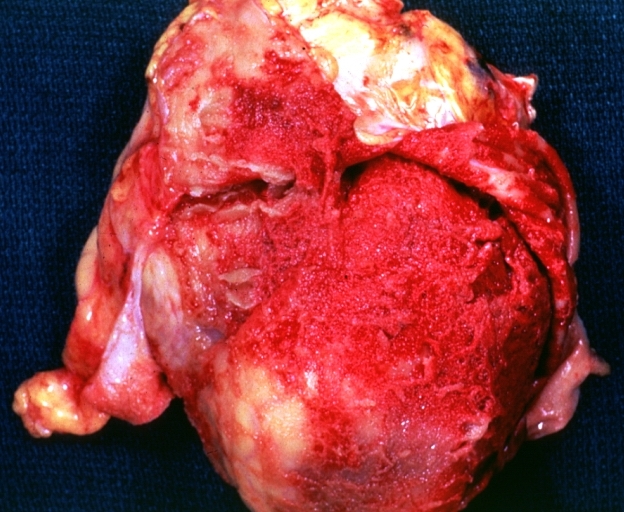
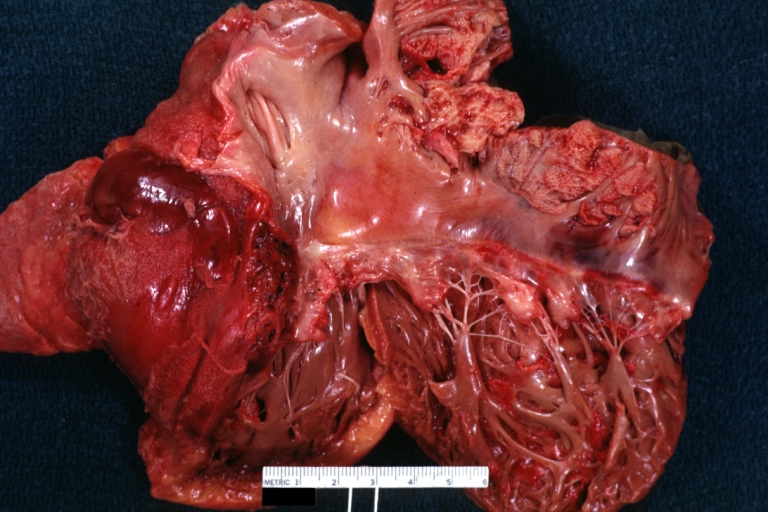
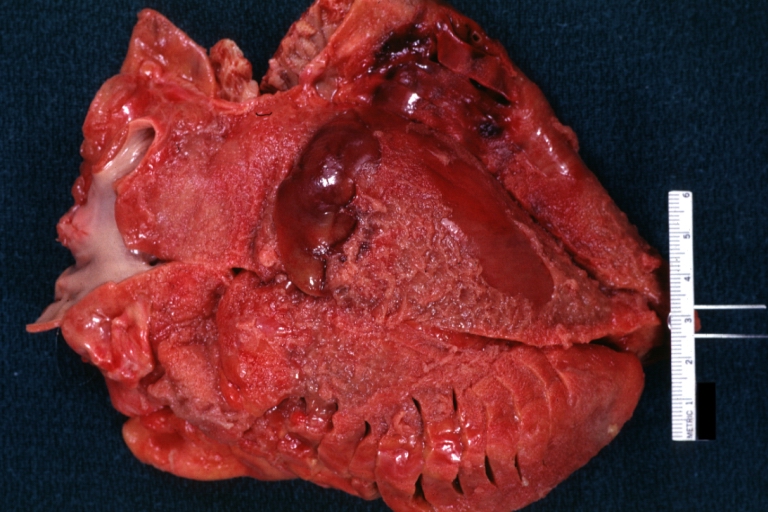
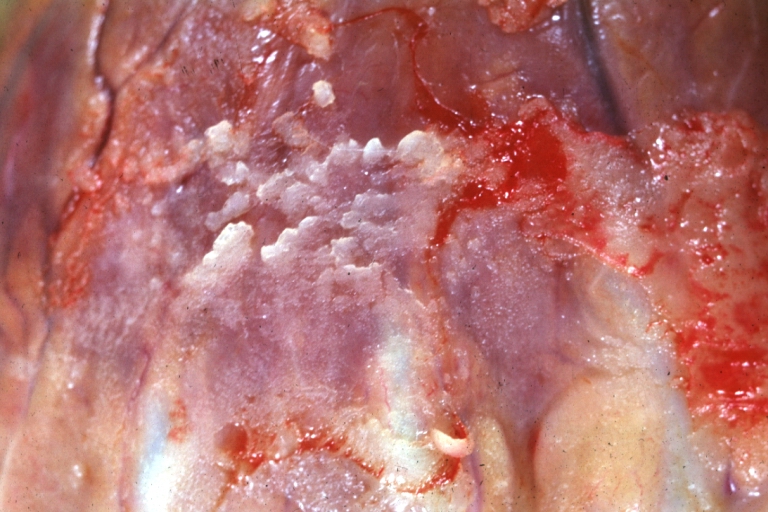
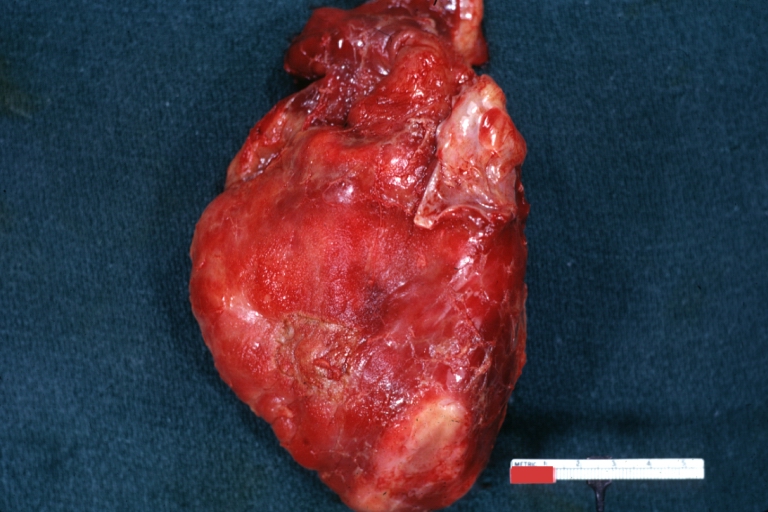
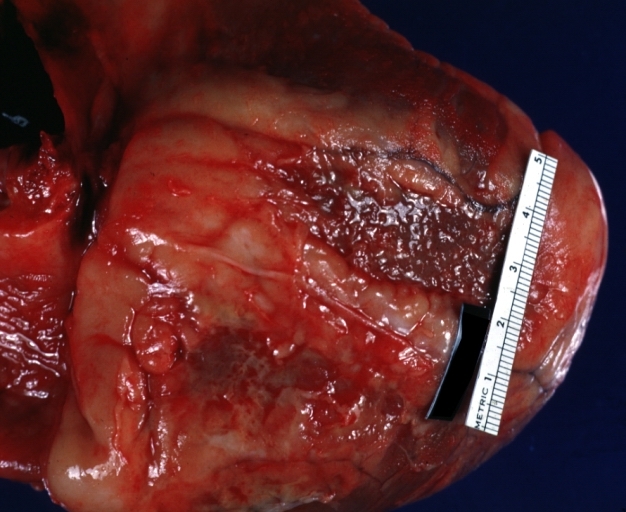
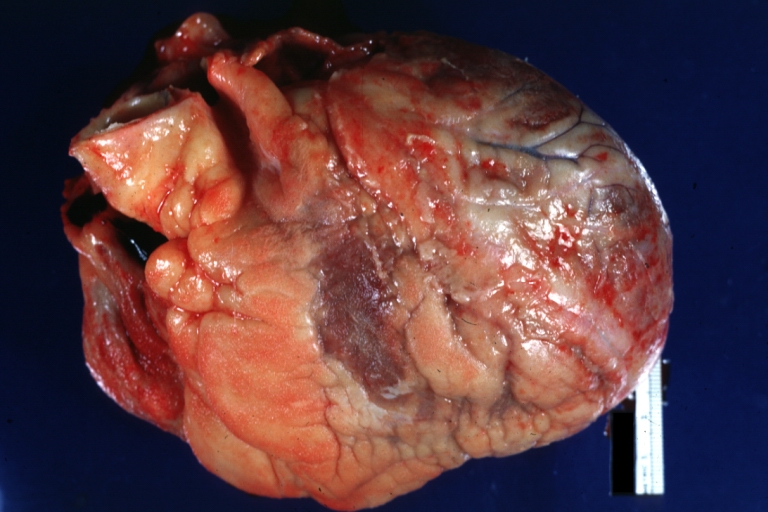
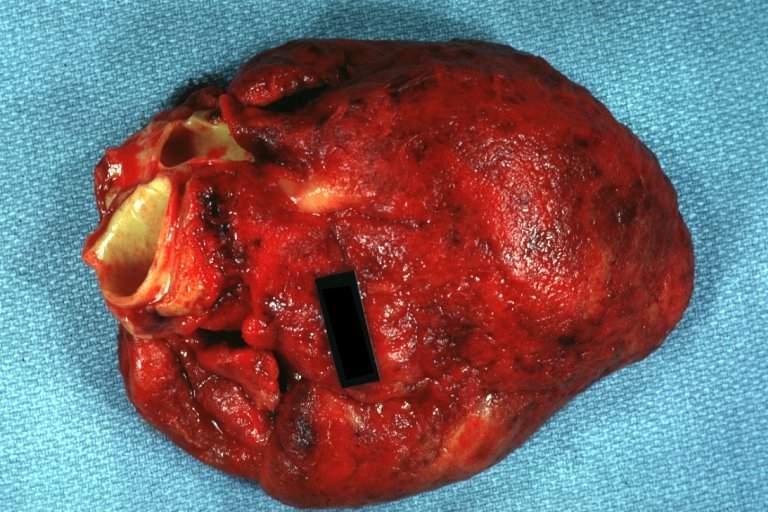
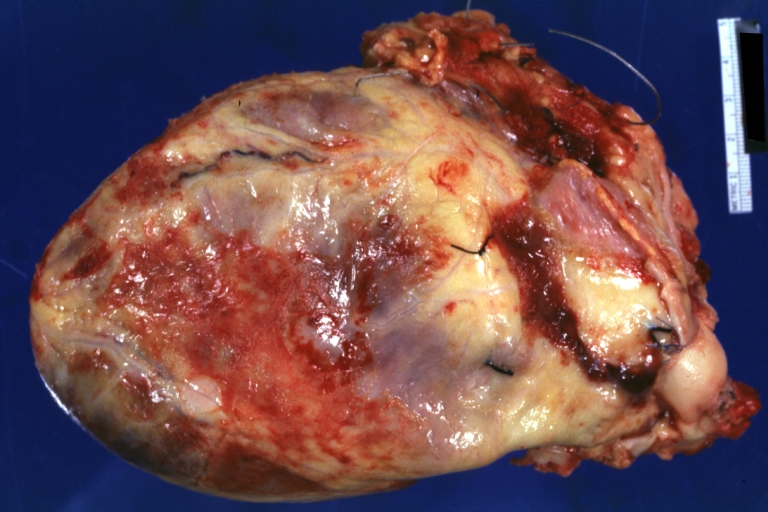
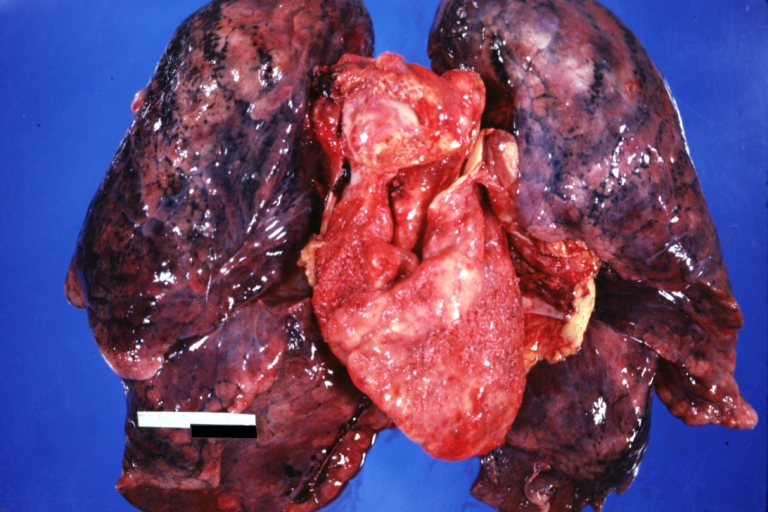
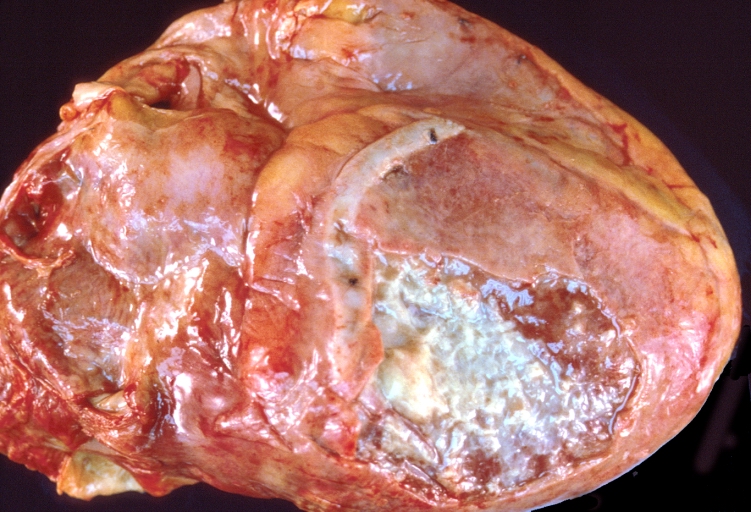
Gross Pathology Images
-
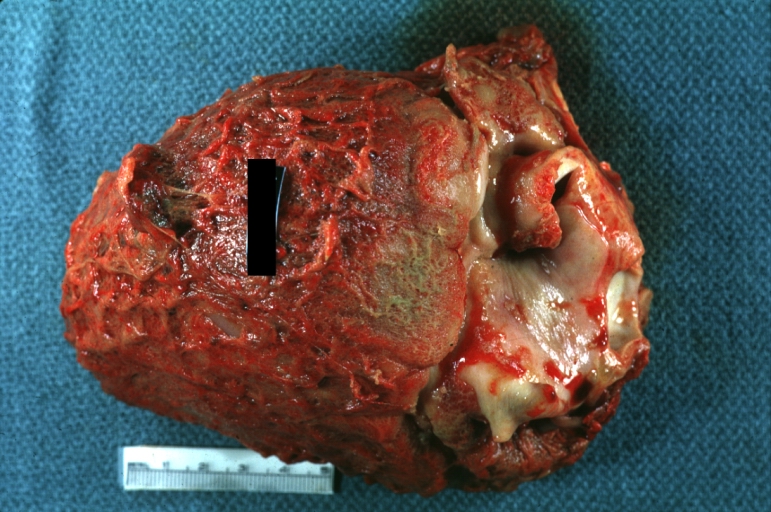
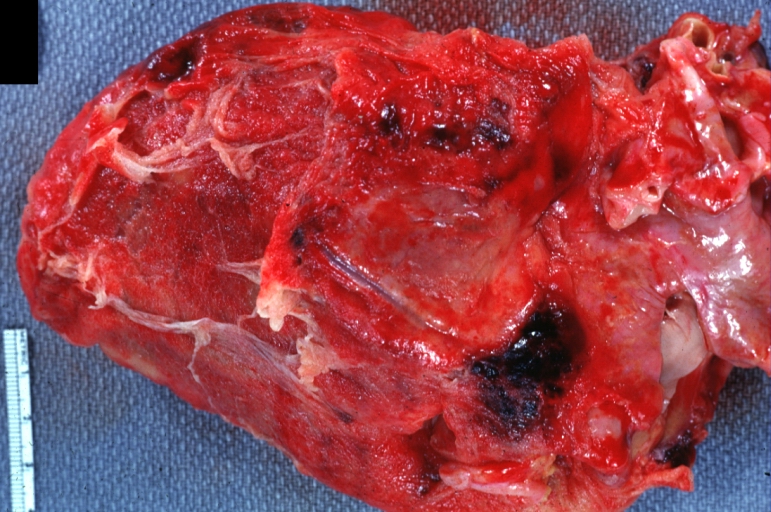
Fibrinous pericarditis: Gross, natural color, an excellent example of bread and butter appearance. Uremia, chronic glomerulonephritis and sepsis.
-
Fibrinous pericarditis: Gross, a good example (bread and butter appearance).
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, an excellent example, close-up view of fibrin.
-
Fibrinous pericarditis: Gross, an excellent example, close-up view.
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, external view of localized pericarditis over an acute infarction.
-
Fibrinous pericarditis: Gross, intact heart, good example.
-
Fibrinous pericarditis: Gross, good example, mild, with small amount of fibrin.
-
Fibrinous pericarditis: Gross, close-up, an excellent example of color and detail.
-
Fibrinous pericarditis: Gross, a good example.
-
Fibrinous pericarditis: Gross, a good example, very mild case.
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, a close-up view, an excellent illustration of fibrinous exudate.
-
Pericarditis in uremia.
-
Fibrinous pericarditis: Gross, fixed tissue (note to color changes), a close-up view of fibrin on epicardial surface of heart, a typical example.
-
Fibrinous pericarditis: Gross, natural color, large right atrial thrombus and fibrinous pericarditis. Normal tricuspid valve with some aging changes (good example).
-
Fibrinous pericarditis: Gross, natural color.
-
Fibrinous pericarditis: Gross, natural color, an excellent example.
-
Fibrinous pericarditis: Gross, natural color, very close-up photo showing fibrinous exudate simulating frost (an excellent example).
-
Rheumatoid fibrinous pericarditis: Gross, natural color, a typical lesion in 22 years old white female due to juvenile rheumatoid arthritis.
-
Fibrinous pericarditis: Gross, natural color, close-up view of minimal fibrinous exudate on epicardial surface due to terminal renal failure.
-
Fibrinous pericarditis: Gross, natural color, anterior view of heart with mild fibrinous exudate over epicardium due to terminal renal failure.
-
Tuberculous pericarditis: Gross, natural color, shaggy hemorrhagic exudate. This case is much more hemorrhagic than the typical tuberculous pericarditis.
-
Heart transplant: Gross, natural color, external view of heart. Two months after transplantation with fibrinous pericarditis.
-
Neoplastic pericarditis: Gross, natural color, shaggy pericarditis. Primer is adenocarcinoma of the lung.
-
Heart: Septic pericarditis.
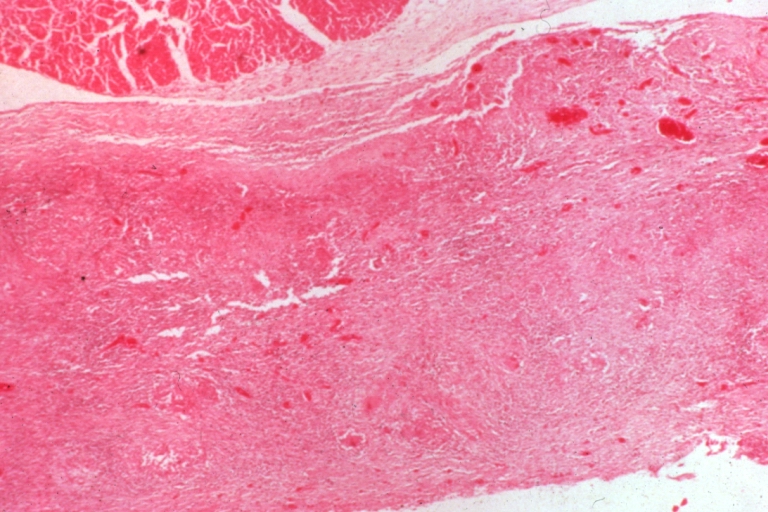
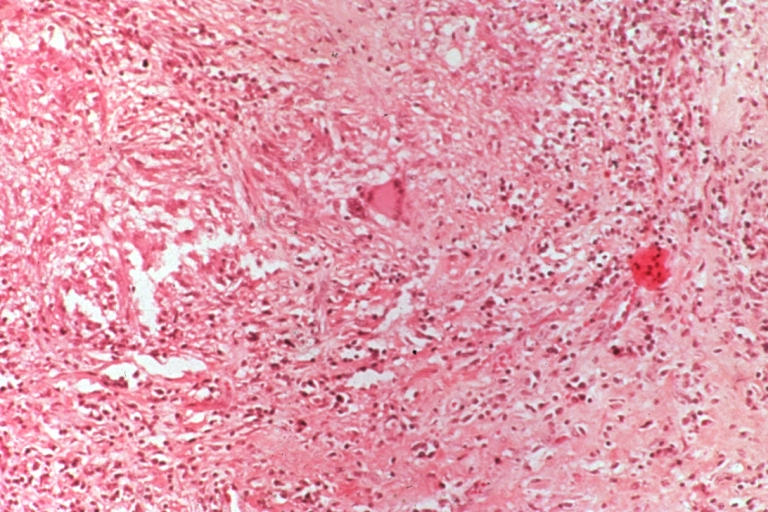
Microscopic Pathology Images
-
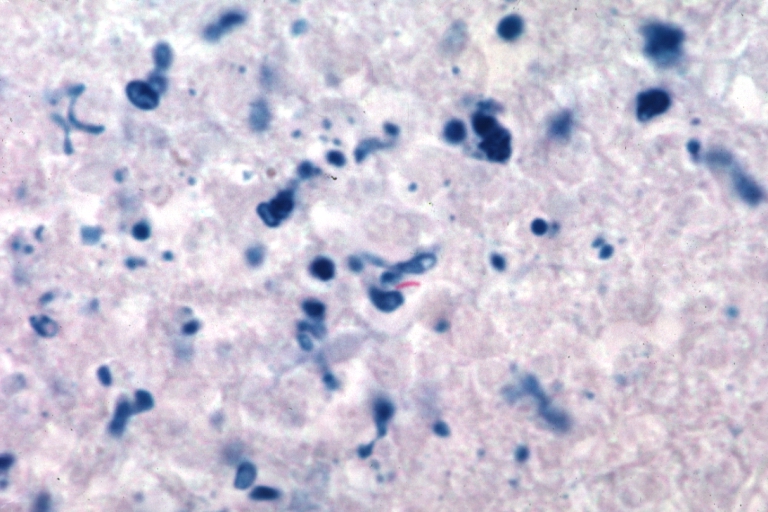
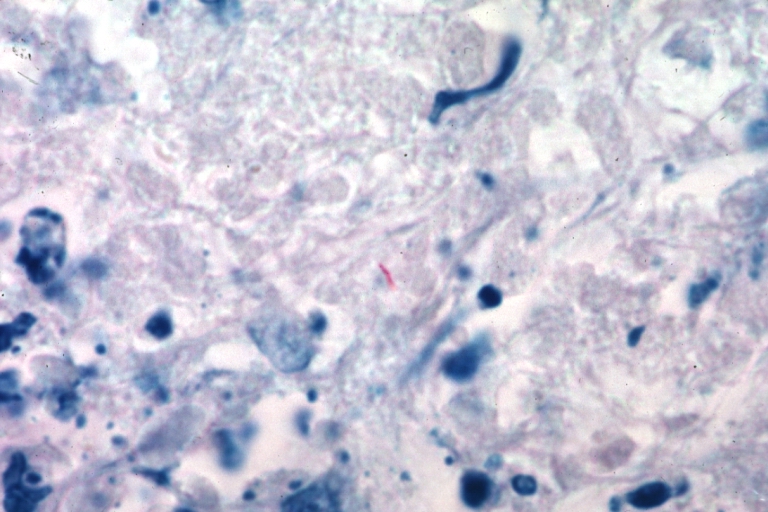
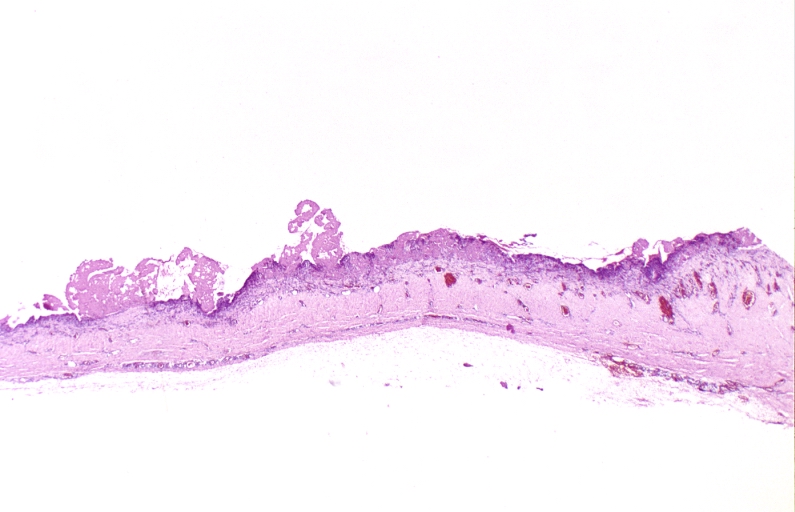
Tuberculous pericarditis.
-
Tuberculous pericarditis.
-
Tuberculous pericarditis: Micro oil acid fast stain. The organism easily seen.
-
Tuberculous pericarditis: Micro oil acid fast stain. The organism easily seen.
-
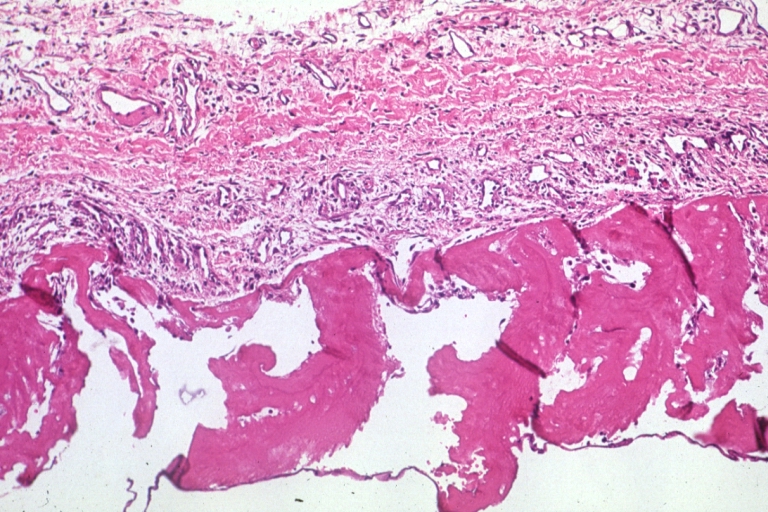
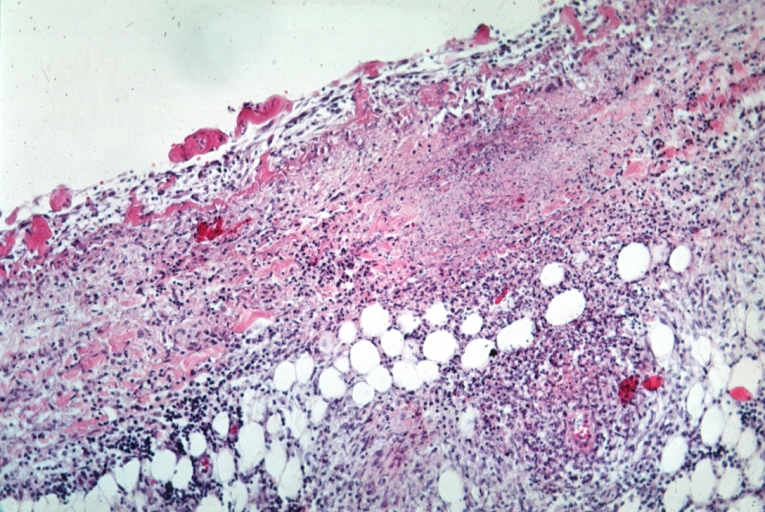
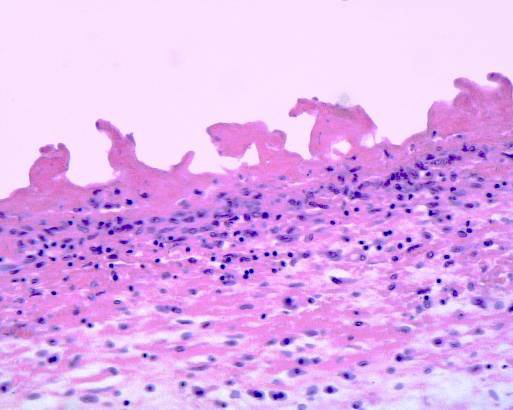
Uremic pericarditis: Micro med mag, H&E. A good example
-
Tuberculous pericarditis: Micro med mag, H&E, a typical lesion
-
Fibrinous pericarditis.
-
Pericarditis fibrinosa (Fibrinous pericarditis).
-
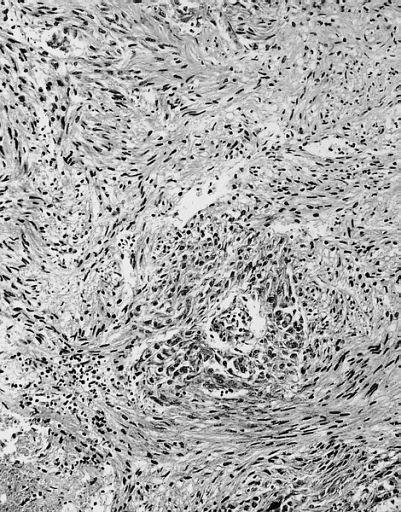
Malignant Mesothelioma, Biphasic Type: Pericardium: This tumor has epithelioid cells (lower half) surrounded by spindled cells. The patient was a 46-year-old woman with constrictive pericarditis; the pericardium was studded with coalescing tumor nodules.
Videos
| AKS7kSl4x5k}} | Acute Fibrinous Pericarditis
{{#ev:youtube|5fz_W1YxbC8}} |
|---|
References
- ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Matthews JD, Cameron SJ, George M (1970). "Constrictive pericarditis following Coxsackie virus infection". Thorax. 25 (5): 624–6. PMC 472200. PMID 5489188.
- ↑ Ilan Y, Oren R, Ben-Chetrit E (1991). "Acute pericarditis: etiology, treatment and prognosis. A study of 115 patients". Jpn Heart J. 32 (3): 315–21. PMID 1920818.
- ↑ Shabetai R (1990). "Acute pericarditis". Cardiol Clin. 8 (4): 639–44. PMID 2249218.
- ↑ Klacsmann PG, Bulkley BH, Hutchins GM (1977). "The changed spectrum of purulent pericarditis: an 86 year autopsy experience in 200 patients". Am J Med. 63 (5): 666–73. PMID 930941.
- ↑ Kauffman CA, Watanakunakorn C, Phair JP (1973). "Purulent pneumococcal pericarditis. A continuing problem in the antibiotic era". Am J Med. 54 (6): 743–50. PMID 4200204.
- ↑ Rubin RH, Moellering RC (1975). "Clinical, microbiologic and therapeutic aspects of purulent pericarditis". Am J Med. 59 (1): 68–78. PMID 1138554.
- ↑ Ribeiro P, Shapiro L, Nihoyannopoulos P, Gonzalez A, Oakley CM (1985). "Pericarditis in infective endocarditis". Eur Heart J. 6 (11): 975–8. PMID 4076207.
- ↑ Roberts WC, Buchbinder NA (1972). "Right-sided valvular infective endocarditis. A clinicopathologic study of twelve necropsy patients". Am J Med. 53 (1): 7–19. PMID 4402567.
- ↑ Peel AA (1948). "TUBERCULOUS PERICARDITIS". Br Heart J. 10 (3): 195–207. PMC 481044. PMID 18610109.
- ↑ Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J (1985). "Primary acute pericardial disease: a prospective series of 231 consecutive patients". Am J Cardiol. 56 (10): 623–30. PMID 4050698.
- ↑ Mayosi BM, Burgess LJ, Doubell AF (2005). "Tuberculous pericarditis". Circulation. 112 (23): 3608–16. doi:10.1161/CIRCULATIONAHA.105.543066. PMID 16330703.