Differentiating crohn's disease from other diseases: Difference between revisions
(Created page with "__NOTOC__ {{Crohn's disease}} {{CMG}} ==Differentiating Crohn's Disease from other Diseases== The most common disease that mimics the symptoms of Crohn's disease is ulcerat...") |
m (Bot: Removing from Primary care) |
||
| (8 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | [[Image:Home_logo1.png|right|250px|https://www.wikidoc.org/index.php/Crohn%27s_disease]] | ||
{{ | {{CMG}} ; {{AE}} {{ADG}} | ||
==Overview== | |||
The most common disease that mimics the symptoms of Crohn's disease is [[ulcerative colitis]], as both are [[Inflammatory bowel disease|inflammatory bowel diseases]] that can affect the [[colon (anatomy)|colon]] with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis. | |||
==Differentiating Crohn's Disease from other Diseases== | ==Differentiating Crohn's Disease from other Diseases== | ||
The most common disease that mimics the symptoms of Crohn's disease is [[ulcerative colitis]], as both are inflammatory bowel diseases that can affect the [[colon (anatomy)|colon]] with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis. | The most common disease that mimics the symptoms of Crohn's disease is [[ulcerative colitis]], as both are [[Inflammatory bowel disease|inflammatory bowel diseases]] that can affect the [[colon (anatomy)|colon]] with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis. | ||
{| class="prettytable" cellpadding=1 style="text-align:center" | {| class="prettytable" cellpadding=1 style="text-align:center" | ||
| Line 15: | Line 18: | ||
| '''Colon involvement''' || Usually || Always | | '''Colon involvement''' || Usually || Always | ||
|- | |- | ||
| '''Rectum involvement''' || Seldom || Usually<ref name="Kornbluth-Sachar2004">{{cite journal | last = Kornbluth | first = Asher | | '''Rectum involvement''' || Seldom || Usually<ref name="Kornbluth-Sachar2004">{{cite journal | last = Kornbluth | first = Asher | title = Ulcerative Colitis Practice Guidelines in Adults | journal = American Journal of Gastroenterology | doi = 10.1111/j.1572-0241.2004.40036.x | id = PMID 15233681 | url = http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf | format = PDF | accessdate = 2006-11-08}}</ref> | ||
|- | |- | ||
| '''Involvement around the [[anus]]''' || Common<ref name="HanauerCrohns">{{cite journal | last = Hanauer | first = Stephen B. | | '''Involvement around the [[anus]]''' || Common<ref name="HanauerCrohns">{{cite journal | last = Hanauer | first = Stephen B. | title = Management of Crohn's Disease in Adults | journal=American Journal of Gastroenterology | volume = 96 | issue = 3 | pages = 635-643 | doi = 10.1111/j.1572-0241.2001.03671.x | id = PMID 11280528 | url = http://www.acg.gi.org/physicians/guidelines/CrohnsDiseaseinAdults.pdf | format = PDF | accessdate = 2006-11-08}}</ref> | ||
|| Seldom | || Seldom | ||
|- | |- | ||
| '''Bile duct involvement''' || No increase in rate of [[primary sclerosing cholangitis]] || Higher rate<ref>{{cite journal | last = Broomé | first = Ulrika | | '''Bile duct involvement''' || No increase in rate of [[primary sclerosing cholangitis]] || Higher rate<ref>{{cite journal | last = Broomé | first = Ulrika | title = Primary sclerosing cholangitis, inflammatory bowel disease, and colon cancer | journal = Seminars in Liver Disease | volume = 26 | issue = 1 | pages = 31-41 | doi =10.1055/s-2006-933561 | id = PMID 16496231 }}</ref> | ||
|- | |- | ||
| '''Distribution of Disease''' || Patchy areas of inflammation (Skip lesions) || Continuous area of inflammation<ref name="Kornbluth-Sachar2004"/> | | '''Distribution of Disease''' || Patchy areas of inflammation (Skip lesions) || Continuous area of inflammation<ref name="Kornbluth-Sachar2004"/> | ||
| Line 46: | Line 49: | ||
| '''[[Tobacco smoking|Smoking]]''' || Higher risk for smokers || Lower risk for smokers<ref name="Kornbluth-Sachar2004"/> | | '''[[Tobacco smoking|Smoking]]''' || Higher risk for smokers || Lower risk for smokers<ref name="Kornbluth-Sachar2004"/> | ||
|} | |} | ||
Oral lesioins of Crohn's disease must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer | |||
<div style="width: 70%;"> | |||
<small><small> | |||
{| class="wikitable" | |||
!Disease | |||
!Presentation | |||
!Risk Factors | |||
!Diagnosis | |||
!Affected Organ Systems | |||
!Important features | |||
!Picture | |||
|- | |||
! colspan="3" |Diseases predominantly affecting the oral cavity | |||
! | |||
! | |||
! | |||
! | |||
|- | |||
|[[Oral candidiasis|Oral Candidiasis]] | |||
| | |||
* [[Dysphagia]] or [[odynophagia]] | |||
* White patches on the mouth and tongue | |||
| | |||
*[[Newborn]] babies | |||
*Denture users | |||
*Poorly controlled [[diabetes]] | |||
*As a side effect of medication, most commonly having taken [[antibiotic]]s. Inhaled [[corticosteroids]] for the treatment of lung conditions (e.g, [[asthma]] or [[COPD]]) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication. | |||
*People with poor [[nutrition]], specifically [[vitamin A]], [[Iron deficiency anemia|iron]] and [[Folate deficiency|folate deficiencies]]. | |||
*People with an [[immune deficiency]] (e.g. as a result of [[AIDS]]/[[HIV]] or [[chemotherapy]] treatment). | |||
*Women undergoing hormonal changes, like [[pregnancy]] or those on [[birth control pills]]. | |||
*[[Organ transplantation]] patients | |||
| | |||
* Clinical diagnosis | |||
* Confirmatory tests rarely needed | |||
|'''Localized candidiasis''' | |||
* [[Oral candidiasis|Oral]] and [[Esophageal candidiasis|esophageal candidasis]] | |||
* [[Candida vulvovaginitis]] | |||
* [[Chronic mucocutaneous candidiasis]] | |||
'''Invasive candidasis''' | |||
* [[Candidiasis|Candidaemia]] | |||
* [[Endocarditis|Candida endocarditis]] | |||
* [[Osteoarthritis|Candida osteoarticular disease]] | |||
| | |||
* [[Osteoarthritis|Oral candidiaisis is]] a benign self limiting disease unless accompanied by [[immunosuppression]]. | |||
|[[File:Human tongue infected with oral candidiasis--By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|thumb|Tongue infected with oral candidiasis - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|400x400px]] | |||
|- | |||
|[[Herpes simplex|Herpes simplex oral lesions]] | |||
| | |||
* [[Fever]] | |||
* [[Sore throat]] | |||
* Painful [[ulcer]]s | |||
| | |||
* Stress | |||
* Recent [[URTI]] | |||
* Female sex | |||
| | |||
* Physical examination | |||
* [[Viral culture]] | |||
* [[Tzanck smear]] | |||
| | |||
* Orofacial Infection | |||
* [[Herpes simplex anogenital infection|Anogenital Infection]] | |||
* [[Herpes simplex ocular infection|Ocular Infection]] | |||
* [[Herpes simplex encephalitis|Herpes Encephalitis]] | |||
* [[Herpes simplex neonatorum|Neonatal Herpes]] | |||
* [[Herpetic whitlow|Herpetic Whitlow]] | |||
* [[Herpes gladiatorum|Herpes Gladiatorum]] | |||
| | |||
* The symptoms of primary [[HSV]] infection generally resolve within two weeks | |||
|[[File:Herpesinfection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|thumb|Oral herpes simplex infection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|400x400px]] | |||
|- | |||
|[[Aphthous ulcer|Aphthous ulcers]] | |||
| | |||
* Painful, red spot or bump that develops into an open [[ulcer]] | |||
| | |||
* Being a female | |||
* Between the ages of 10-40 | |||
* Family history of [[Aphthous ulcer|aphthous ulcers]] | |||
| | |||
* Physical examination | |||
* Diagnosis of exclusion | |||
| | |||
* Oral cavity | |||
| | |||
* Self-limiting , [[Pain]] decreases in 7 to 10 days, with complete healing in 1 to 3 weeks | |||
|[[File:Afta foto - By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358.jpg|thumb|Apthous ulcer on the under surface of the tongue|By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358|400x400px]] | |||
|- | |||
|[[Squamous cell carcinoma]] | |||
| | |||
*Non healing [[ulcer]], [[nodule]], indurated plaque or mass | |||
*May involve [[skin]], [[lips]], inside the [[mouth]], [[throat]] or [[esophagus]] | |||
| | |||
* Chronic sun or [[Ultraviolet|UV exposure]] | |||
* Fair [[skin]] | |||
* [[Elderly]] age (>45 yrs) | |||
* [[Male sex]] | |||
* [[Smoking]] | |||
| | |||
*[[Physical exam]] | |||
*[[Biopsy]] | |||
| | |||
*[[Oral Cavity]] | |||
**Floor of [[mouth]] | |||
**Lateral [[tongue]] | |||
*[[Throat]] | |||
*[[Esophagus]] | |||
| | |||
*[[Malignant]] | |||
*Can spread to [[TMJ]] | |||
*Some times associated with [[leukoplakia]] | |||
|[[File:PLoS oral cancer.png|thumb|400x400px| |Squamous cell carcinoma - By Luca Pastore, Maria Luisa Fiorella, Raffaele Fiorella, Lorenzo Lo Muzio - http://www.plosmedicine.org/article/showImageLarge.action?uri=info%3Adoi%2F10.1371%2Fjournal.pmed.0050212.g001, CC BY 2.5, https://commons.wikimedia.org/w/index.php?curid=15252632]] | |||
|- | |||
|[[Leukoplakia]] | |||
| | |||
*White leathery spots on the [[mucous membranes]] of the [[tongue]] and inside of the [[mouth]] | |||
*Lateral borders of [[tongue]] | |||
| | |||
*Atypical [[Tobacco]] use | |||
*Chronic [[irritation]] | |||
*[[Immunodeficiency]] | |||
*[[Bloodroot]] ([[Sanguinarine|sanguinaria]]) | |||
| | |||
*[[Physical exam]] | |||
*Diagnosis of exclusion | |||
*[[Biopsy]] | |||
| | |||
*[[Vulva|Vulvar]] lesions occur independent of oral lesions | |||
| | |||
*Associated with [[HIV]] | |||
*Persistant white spots | |||
*[[Benign]] but can progress to [[carcinoma]] after almost 10 years | |||
*Oral proliferative [[Leukoplakia|verrucous leukoplakia]] is an aggressive sub type with multiple lesions and higher conversion to [[warts]] or [[carcinoma]]<ref>{{Cite journal | |||
| author = [[Ann M. Gillenwater]], [[Nadarajah Vigneswaran]], [[Hanadi Fatani]], [[Pierre Saintigny]] & [[Adel K. El-Naggar]] | |||
| title = Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity! | |||
| journal = [[Advances in anatomic pathology]] | |||
| volume = 20 | |||
| issue = 6 | |||
| pages = 416–423 | |||
| doi = 10.1097/PAP.0b013e3182a92df1 | |||
| pmid = 24113312 | |||
}}</ref> | |||
|[[File:Oral hairy leukoplakia (EBV, in HIV)a.jpg|thumb|400x300px|Leukoplakia - By Aitor III - Own work, Public Domain, https://commons.wikimedia.org/w/index.php?curid=9873087]] | |||
|- | |||
|[[Melanoma]] | |||
| | |||
*A lesion with [[ABCD]] | |||
**[[Asymmetry]] | |||
**Border irregularity | |||
**Color variation | |||
**[[Diamete]]r changes | |||
*[[Bleeding]] from the lesion | |||
| | |||
*[[Ultraviolet|UV radiations]] | |||
*[[Genetic predisposition]] | |||
*[[Old age]] | |||
*[[Male gender]] | |||
*Family or personal history of [[melanoma]] | |||
*Multiple benign or atypical [[Nevus|nevi]] | |||
| | |||
*[[ABCD]] characteristics | |||
*[[Bleeding]] or [[ulceration]] may show [[malignancy]] | |||
*Serum [[LDH]] may be elevated in case of [[malignancy]] | |||
*[[Biopsy]] | |||
| | |||
*Can [[metastasize]] | |||
*All [[UV radiation]] or sun exposed areas can be effected independently | |||
*1-2 to hundreds of [[granules]] | |||
| | |||
*[[Neural crest cell]] derivative | |||
*Development begins with disruption of [[nevus]] growth control | |||
*Progression involves [[MAPK/ERK pathway]] | |||
*[[RAS|N-RAS]] or [[BRAF]] [[oncogene]] also involved | |||
|[[File:Palate malign melanoma 01.jpg|thumb|400x400px|Oral melanoma - By Emmanouil K Symvoulakis, Dionysios E Kyrmizakis, Emmanouil I Drivas, Anastassios V Koutsopoulos, Stylianos G Malandrakis, Charalambos E Skoulakis and John G Bizakis - Symvoulakis et al. Head & Face Medicine 2006 2:7 doi:10.1186/1746-160X-2-7 (Open Access), [1], CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=9839811]] | |||
|- | |||
|[[Fordyce spots]] | |||
| | |||
*Rice-like [[granules]] or [[spots]] | |||
*Small, [[painless]], [[raised]], [[pale]], red or white | |||
*1 to 3 mm in [[diameter]] | |||
| | |||
*Greasy skin types | |||
*Some [[Rheumatic|rheumatic disorders]] | |||
*[[Hereditary nonpolyposis colorectal cancer]] | |||
**Lower [[gingiva]] (gums) | |||
**[[Vestibular system|Vestibular mucosa]] | |||
| | |||
*[[Physical exam]] | |||
*Small [[keratin]]-filled [[pseudocysts]] | |||
*May be seen on [[incidental]] [[mucosal]] [[biopsy]] | |||
**[[Biopsy]] not done for them primarily | |||
| | |||
*[[Oral cavity]] | |||
**[[Vermillion border|Vermilion border]] of the lips | |||
**[[Oral mucosa]] of the upper lip | |||
*[[Buccal mucosa]] in the commissural region often bilaterally | |||
*[[Genitals]] | |||
| | |||
*[[Benign neoplasms]] with [[sebaceous]] features | |||
*Visible [[sebaceous glands]] | |||
*No surrounding [[mucosal]] change | |||
*Several adjacent [[glands]] may coalesce into a larger cauliflower-like cluster | |||
|[[File:Fospot.jpg|thumb|400x400px|Fordyce spots - Por Perene - Obra do próprio, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=19772899]] | |||
|- | |||
|[[Burning mouth syndrome]] | |||
| | |||
*Burning or [[tingling]] on the [[lips]], [[tongue]], or entire [[mouth]] | |||
| | |||
*[[Nutritional deficiencies]] | |||
*Chronic [[anxiety]] or [[depression]] | |||
*[[Diabetes type 2]] | |||
*[[Menopause]] | |||
*[[Oral thrush]] or [[dry mouth]], or damaged [[nerves]] transmitting taste | |||
*[[Female gender ]] | |||
*[[Menopause]] | |||
| | |||
*[[Presentation]] | |||
*[[Physical exam]] | |||
| | |||
*[[Oral cavity]] | |||
| | |||
*Pain typically is low in the morning and builds up over the day | |||
*Low dosages of [[benzodiazepines]], [[tricyclic antidepressants]] or [[anticonvulsants]] may be effective | |||
| | |||
|- | |||
|[[Torus palatinus]] | |||
| | |||
*Bony growth on midline of the [[hard palate]] | |||
*[[Nodular]] mass covered with normal [[mucosa]] | |||
| | |||
*[[Genetic predisposition]] | |||
**[[Autosomal dominant]] | |||
| | |||
*[[Physical exam]] | |||
*Types | |||
**[[Torus palatinus|Flat tori]] | |||
**[[Torus palatinus|Spindle tori]] | |||
**[[Torus palatinus|Nodular tori]] | |||
**[[Torus palatinus|Lobular tori]] | |||
| | |||
*[[Hard palate]] | |||
| | |||
*More common in [[Asian]] and Inuit populations | |||
*Twice more common in [[females]] | |||
*Repeated [[trauma]] can cause [[bleeding]] | |||
*[[Surgery]] may be required in symptomatic | |||
|[[File:06-06-06palataltoria.jpg|thumb|Torus palatinus|400x400px|Torus palatinus - By Photo taken by dozenist, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=846591]] | |||
|- | |||
| colspan="4" |'''Diseases involving oral cavity and other organ systems''' | |||
| | |||
| | |||
| | |||
|- | |||
|[[Behçet's disease|Behcet's disease]] | |||
| | |||
*Painful [[mouth sores]] | |||
*[[Acne]] like skin lesions | |||
*Headache, [[fever]], poor [[balance]], [[disorientation]] | |||
*[[Abdominal pain]], [[diarrhea]] or [[bleeding]] | |||
*[[Uveitis]] | |||
*Joint [[swelling]] and joint [[pain]] | |||
*Genital [[sores]] wit [[pain]] and [[scaring]] | |||
*[[Aneurysms]] | |||
| | |||
*Over active [[immune system]] | |||
| | |||
*[[Physical examination]] | |||
| | |||
*[[Mouth]] | |||
*[[Genitals]] | |||
*[[GIT]] | |||
*[[Eye]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
*[[Vascular system]] | |||
*[[Brain]] | |||
| | |||
*[[Outbreaks]] of exaggerated [[inflammation]] | |||
*Affects smaller [[blood vessels]] | |||
|[[File:Behcets disease.jpg|thumb|400x400px|Behcet's disease - By Ahmet Altiner MD, Rajni Mandal MD - http://dermatology.cdlib.org/1611/articles/18_2009-10-20/2.jpg, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=17863021]] | |||
|- | |||
|[[Crohn's disease]] | |||
| | |||
*Chronic, episodic [[diarrhea]] or [[constipation]] | |||
*[[Abdominal pain]] | |||
*[[Vomiting]] | |||
*[[Weight loss]] or [[weight gain]] | |||
| | |||
*[[Smoking]] | |||
*[[Whites]] and [[European]] [[Jews]] | |||
*[[Hormonal contraception]] | |||
*Diets high in microparticles, sweet, fatty or refined foods | |||
*Industrialized country | |||
| | |||
*Typical [[history]] and [[symptoms]] | |||
*[[Skip lesions]] on [[biopsy]] | |||
*[[Anti saccharomyces cerevisiae antibodies|Anti-Saccharomyces cerevisiae antibodies (ASCA)]] | |||
*[[Anti-neutrophil cytoplasmic antibodies]] ([[ANCA]]) | |||
| | |||
*[[Eyes]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
| | |||
*May lead to | |||
**[[Obstruction]]s | |||
**[[Abscess]]es | |||
**Free [[perforation]] | |||
**[[Hemorrhage]] | |||
| | |||
|- | |||
|[[Agranulocytosis]] | |||
| | |||
*[[Fever]] or [[chills]] | |||
*Frequent [[infections]] | |||
*Unusual [[redness]], [[pain]], or [[swelling]] around a wound | |||
*Mouth [[ulcers]] | |||
*[[Abdominal pain]] | |||
*[[Burning sensation when urinating]] | |||
*[[Sore throat]] | |||
| | |||
*[[Medications]]<ref name="pmid17142169">{{cite journal |vauthors=Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F |title=Idiosyncratic drug-induced agranulocytosis: Update of an old disorder |journal=Eur. J. Intern. Med. |volume=17 |issue=8 |pages=529–35 |year=2006 |pmid=17142169 |doi=10.1016/j.ejim.2006.07.012 |url=}}</ref> | |||
*[[List of chemotherapeutic agents#Cytotoxic Chemotherapy|Cytotoxic chemotherapy]] | |||
*[[Hematological malignancy|Hematologic malignancies]] | |||
*[[Autoimmune disorders]] | |||
| | |||
*[[Neutropenia]] <100 cells per micro litre | |||
*[[Eosinopenia]] | |||
*[[Basopenia]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[GIT]] | |||
*[[Urinary system]] | |||
*[[Conjunctiva]] | |||
| | |||
*[[Immunocompromised|Immunocompromization]] | |||
*Types | |||
**[[Drug-induced]] | |||
**[[Malignant]] | |||
**[[Autoimmune]] | |||
| | |||
|- | |||
|[[Syphilis]]<ref> title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"</ref> | |||
| | |||
*[[Chancre]] | |||
*Regional [[lymphadenopathy]] | |||
| | |||
*[[Multiple sexual partners]] | |||
*Illicit [[drug use]] | |||
*[[Unprotected sex]] | |||
*[[Homosexual men|Men who have sex with men]] | |||
*Residence in highly prevalent areas | |||
*[[Human Immunodeficiency Virus (HIV)|HIV]] infection | |||
*Presence of other [[STI]]s | |||
*Previous history of [[Sexually transmitted disease|STIs]] | |||
*[[Intravenous drug use]] | |||
| | |||
*[[Darkfield microscope|Darkfield microscopy]] | |||
*Non [[Treponema|treponemal]] tests like [[VDRL]] and [[RPR test]]) | |||
*[[Treponema|Treponemal]] tests[[FTA-ABS|FTA-ABS tests]], (TP-PA) assay, [[Enzyme linked immunosorbent assay (ELISA)|enzyme immunoassays]], and [[Chemiluminescence|chemiluminescence immunoassays]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Penis]] | |||
*[[Cervix]] | |||
*[[Labia]] | |||
*[[Anal canal]] | |||
*[[Rectum ]] | |||
*[[CNS]] | |||
*[[Cardiovascular|CVS]] | |||
| | |||
*[[Primary syphilis]] | |||
**[[Chancre]] | |||
*[[Secondary syphilis]] | |||
**[[Condyloma latum|Condylomata lata]] | |||
*[[Latent syphilis]] | |||
**[[Asymptomatic]] | |||
*[[Tertiary syphilis]] | |||
**[[Gumma|Gummas]] | |||
**[[Neurosyphilis]] | |||
|[[File:Hutchinson teeth congenital syphilis PHIL 2385.rsh.jpg|thumb|400x400px|oral syphilis - By CDC/Susan Lindsley - http://phil.cdc.gov/phil_images/20021114/34/PHIL_2385_lores.jpg, Public Domain, https://commons.wikimedia.org/w/index.php?curid=2134349]] | |||
|- | |||
|[[Coxsackie virus]] | |||
| | |||
*[[Fever]] | |||
*[[Sores]] in the [[mouth]] | |||
*[[Rash]] with [[blisters]] | |||
*[[Aches]] | |||
| | |||
*[[Pregnancy]] | |||
*[[immunodeficiency]] | |||
| | |||
*[[History]] and [[Physical exam]] | |||
*[[Swabbing|Throat swabs]] | |||
*Swabs from the lesion | |||
*[[Tzanck test]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*Symptomatic treatment | |||
|[[File:Hand foot mouth disease 07a.jpg|Hand-foot-and-mouth disease|400x400px]] | |||
|- | |||
|[[Chickenpox|Chicken pox]] | |||
| | |||
*[[Conjunctival]] symptoms | |||
*[[Catarrhal]] symptoms | |||
*Characteristic [[spots]] on the trunk appearing in two or three waves | |||
*[[Itching]] | |||
| | |||
*[[Pregnancy]] | |||
*[[Premature infants]] born to susceptible mothers | |||
*All [[infants]] born at less than 28 weeks [[gestation]] or who weigh =1000 grams | |||
*[[Immunocompromised]] | |||
| | |||
*[[History]] and [[physical exam]] | |||
*[[PCR]] to detect [[VZV]] in [[skin lesions]] ([[vesicles]], [[scabs]], [[Maculopapular|maculopapular lesions]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*[[Sodium bicarbonate]] in baths or [[antihistamines]] for [[itching]] | |||
*[[Paracetamol]] ([[acetaminophen]]) for [[fever]] | |||
*[[Prednisolone]] is [[contraindicated]] | |||
|[[File:Herpangina2016.jpg|thumb|400x400px|Chickenpox - By James Heilman, MD - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=52872565]] | |||
|- | |||
|[[Measles]] | |||
| | |||
*[[Fever]] | |||
*[[Rash]] | |||
*[[Cough]] | |||
*[[Coryza]] (runny nose) | |||
*[[Conjunctivitis]] (pink eye) | |||
*[[Malaise]] | |||
*[[Koplick spots]] in mouth | |||
| | |||
*Unvaccinated individuals<ref name="pmid11135778">{{cite journal| author=Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE| title=Individual and community risks of measles and pertussis associated with personal exemptions to immunization. | journal=JAMA | year= 2000 | volume= 284 | issue= 24 | pages= 3145-50 | pmid=11135778 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11135778 }} </ref><ref name="pmid9009400">{{cite journal| author=Ratnam S, West R, Gadag V, Williams B, Oates E| title=Immunity against measles in school-aged children: implications for measles revaccination strategies. | journal=Can J Public Health | year= 1996 | volume= 87 | issue= 6 | pages= 407-10 | pmid=9009400 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9009400 }} </ref> | |||
*Crowded and/or unsanitary conditions | |||
*Traveling to less developed and developing countries | |||
*Immunocompromized | |||
*Winter and [[spring]] seasons | |||
*Born after 1956 and never fully vaccinated | |||
*Health care workers | |||
| | |||
*[[History]] and [[examination]] | |||
*[[PCR]] for [[Measles]]-specific [[IgM|IgM antibody]] | |||
*[[PCR]] for [[Measles]] [[RNA]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[Respiratory tract]] | |||
*[[Eyes]] | |||
*[[Throat]] | |||
| | |||
*Caused by [[Morbillivirus]] | |||
*Primary site of infection is the [[respiratory epithelium]] of the [[nasopharynx]] | |||
*Transmitted in [[respiratory secretions]], via [[aerosol droplets]] containing [[Virus|virus particles]] | |||
|[[File:Koplik spots, measles 6111 lores.jpg|thumb|400x400px|Koplick spots (Measles) - By CDC - http://phil.cdc.gov/PHIL_Images/20040908/4f54ee8f0e5f49f58aaa30c1bc6413ba/6111_lores.jpg, Public Domain, https://commons.wikimedia.org/w/index.php?curid=824483]] | |||
|}</small></small> | |||
</div> | |||
The following table differentiates all the diseases presenting with abdominal pain, fever and lower gastrointestinal bleeding. | |||
{| align="center" | |||
|- | |||
| | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
| colspan="13" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Clinical manifestations''' | |||
! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diagnosis | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
| colspan="9" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Symptoms''' | |||
! colspan="4" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Signs | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI bleeding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
|- | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diverticulitis|Acute diverticulitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |LLQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated diverticulitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT scan | |||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[constipation]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Inflammatory bowel disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal or hyperactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | |||
* [[Anti saccharomyces cerevisiae antibodies]] (ASCA) in [[Crohn's disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[String sign]] on [[abdominal x-ray]] in [[Crohn's disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
Extra intestinal findings: | |||
* [[Uveitis]] | |||
* [[Arthritis]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Infective colitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in fulminant colitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Stool culture]] and studies | |||
* Shiga toxin in bloody diarrhea | |||
* [[PCR]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | |||
* Bowel wall thickening | |||
* Edema | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Colon carcinoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse/localized | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal or hyperactive if obstruction present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CBC | |||
* Carcinoembryonic antigen (CEA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Colonoscopy | |||
* Flexible sigmoidoscopy | |||
* Barium enema | |||
* CT colonography | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* PILLCAM 2: A colon capsule for CRC screening may be used in patients with an incomplete colonoscopy who lacks obstruction | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hemochromatosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in cirrhotic patients | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* >60% TS | |||
* >240 μg/L SF | |||
* Raised LFT <br>Hyperglycemia | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ultrasound shows evidence of cirrhosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Extra intestinal findings: | |||
* Hyperpigmentation | |||
* Diabetes mellitus | |||
* Arthralgia | |||
* Impotence in males | |||
* Cardiomyopathy | |||
* Atherosclerosis | |||
* Hypopituitarism | |||
* Hypothyroidism | |||
* Extrahepatic cancer | |||
* Prone to specific infections | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Mesenteric ischemia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Periumbilical | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive to absent | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] and [[lactic acidosis]] | |||
* [[Amylase]] levels | |||
* [[D-dimer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT angiography | |||
* SMA or SMV thrombosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Also known as abdominal angina that worsens with eating | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ischemic colitis|Acute ischemic colitis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive then absent | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal x-ray]] | |||
* Distension and pneumatosis | |||
CT scan | |||
* Double halo appearance, thumbprinting | |||
* Thickening of bowel | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* May lead to shock | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ruptured abdominal aortic aneurysm]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Fibrinogen]] | |||
* [[D-dimer]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Focused Assessment with Sonography in Trauma (FAST) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Unstable hemodynamics | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intra-abdominal or [[retroperitoneal hemorrhage]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* ↓ Hb | |||
* ↓ Hct | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT scan | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[trauma]] | |||
|- | |||
|} | |||
|} | |||
<span style="font-size:85%">'''Abbreviations:''' | |||
'''[[RUQ]]'''= Right upper quadrant of the abdomen, '''LUQ'''= Left upper quadrant, '''LLQ'''= Left lower quadrant, '''RLQ'''= Right lower quadrant, '''LFT'''= Liver function test, SIRS= [[Systemic inflammatory response syndrome]], '''[[ERCP]]'''= [[Endoscopic retrograde cholangiopancreatography]], '''IV'''= Intravenous, '''N'''= Normal, '''AMA'''= Anti mitochondrial antibodies, '''[[LDH]]'''= [[Lactate dehydrogenase]], '''GI'''= Gastrointestinal, '''CXR'''= Chest X ray, '''IgA'''= [[Immunoglobulin A]], '''IgG'''= [[Immunoglobulin G]], '''IgM'''= [[Immunoglobulin M]], '''CT'''= [[Computed tomography]], '''[[PMN]]'''= Polymorphonuclear cells, '''[[ESR]]'''= [[Erythrocyte sedimentation rate]], '''[[CRP]]'''= [[C-reactive protein]], TS= [[Transferrin saturation]], SF= Serum [[Ferritin]], SMA= [[Superior mesenteric artery]], SMV= [[Superior mesenteric vein]], ECG= [[Electrocardiogram]]</span> | |||
===Differentiating Crohn's disease from other causes of abdominal pain and diarrhea=== | |||
Crohn's disease must be differentiated from other causes of abdominal pain and diarrhea. | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="2" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diseases | |||
| colspan="9" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Clinical manifestations''' | |||
| | |||
| | |||
| | |||
! colspan="10" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Para-clinical findings | |||
| colspan="1" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Gold standard''' | |||
! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Additional findings | |||
|- | |||
| colspan="3" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Symptoms''' | |||
| | |||
| | |||
| | |||
! colspan="3" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Physical examination | |||
! | |||
! | |||
! | |||
|- | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Lab Findings | |||
! colspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Imaging | |||
! | |||
! | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Histopathology | |||
|- | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Abdominal pain]] | |||
! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Diarrhea]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Flushing]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Dyspnea]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Palpitations]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other symptoms | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Wheezing]] | |||
! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Telangiectasia]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Hypotension]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Tachycardia]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Systolic murmurs|Systolic murmur]] of [[tricuspid regurgitation]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other physical findings | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Urinary 5-hydroxyindoleacetic acid (5-HIAA) | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Serum [[Chromogranin]] A (CgA) | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other markers | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Computed tomography|Abdominal computed tomography]] (CT) | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |[[Mri|Abdominal MRI]] | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Somatostatin receptor scintigraphy [SRS], or Octreoscan | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Metaiodobenzylguanidine (MIBG) scintigraphy | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other diagnostic studies | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Transthoracic echocardiography | |||
|- | |||
| rowspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Carcinoid Syndrome<ref name="pmid30133565">{{cite journal |vauthors=Rubin de Celis Ferrari AC, Glasberg J, Riechelmann RP |title=Carcinoid syndrome: update on the pathophysiology and treatment |journal=Clinics (Sao Paulo) |volume=73 |issue=suppl 1 |pages=e490s |date=August 2018 |pmid=30133565 |pmc=6096975 |doi=10.6061/clinics/2018/e490s |url=}}</ref><ref name="pmid14693013">{{cite journal |vauthors=Hegyi J, Schwartz RA, Hegyi V |title=Pellagra: dermatitis, dementia, and diarrhea |journal=Int. J. Dermatol. |volume=43 |issue=1 |pages=1–5 |date=January 2004 |pmid=14693013 |doi= |url=}}</ref><ref name="pmid15100502">{{cite journal |vauthors=Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E |title=Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours |journal=Nucl Med Commun |volume=25 |issue=5 |pages=445–9 |date=May 2004 |pmid=15100502 |doi= |url=}}</ref><ref name="pmid151005022">{{cite journal |vauthors=Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E |title=Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours |journal=Nucl Med Commun |volume=25 |issue=5 |pages=445–9 |date=May 2004 |pmid=15100502 |doi= |url=}}</ref><ref name="BoraVithiavathi2012">{{cite journal|last1=Bora|first1=ManashKumar|last2=Vithiavathi|first2=S|title=Primary bronchial carcinoid: A rare differential diagnosis of pulmonary koch in young adult patient|journal=Lung India|volume=29|issue=1|year=2012|pages=59|issn=0970-2113|doi=10.4103/0970-2113.92366}}</ref><ref name="pmid25207053">{{cite journal |vauthors=Yazıcıoğlu A, Yekeler E, Bıcakcıoğlu P, Ozaydın E, Karaoğlanoğlu N |title=Synchronous bilateral multiple typical pulmonary carcinoid tumors: a unique case with 10 typical carcinoids |journal=Balkan Med J |volume=29 |issue=4 |pages=450–2 |date=December 2012 |pmid=25207053 |pmc=4115868 |doi=10.5152/balkanmedj.2012.081 |url=}}</ref><ref name="pmid14616879">{{cite journal |vauthors=Krausz Y, Keidar Z, Kogan I, Even-Sapir E, Bar-Shalom R, Engel A, Rubinstein R, Sachs J, Bocher M, Agranovicz S, Chisin R, Israel O |title=SPECT/CT hybrid imaging with 111In-pentetreotide in assessment of neuroendocrine tumours |journal=Clin. Endocrinol. (Oxf) |volume=59 |issue=5 |pages=565–73 |date=November 2003 |pmid=14616879 |doi= |url=}}</ref><ref name="van der LelyHerder2005">{{cite journal|last1=van der Lely|first1=Aart J.|last2=Herder|first2=Wouter W. de|title=Carcinoid syndrome: diagnosis and medical management|journal=Arquivos Brasileiros de Endocrinologia & Metabologia|volume=49|issue=5|year=2005|pages=850–860|issn=0004-2730|doi=10.1590/S0004-27302005000500028}}</ref><ref name="pmid28238592">{{cite journal |vauthors=Halperin DM, Shen C, Dasari A, Xu Y, Chu Y, Zhou S, Shih YT, Yao JC |title=Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study |journal=Lancet Oncol. |volume=18 |issue=4 |pages=525–534 |date=April 2017 |pmid=28238592 |pmc=6066284 |doi=10.1016/S1470-2045(17)30110-9 |url=}}</ref> | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Neuroendocrine tumor]] of [[midgut]] <ref name="pmid3227292">{{cite journal |vauthors=Sjöblom SM |title=Clinical presentation and prognosis of gastrointestinal carcinoid tumours |journal=Scand. J. Gastroenterol. |volume=23 |issue=7 |pages=779–87 |date=September 1988 |pmid=3227292 |doi= |url=}}</ref><ref name="pmid24059366">{{cite journal |vauthors=Ganeshan D, Bhosale P, Yang T, Kundra V |title=Imaging features of carcinoid tumors of the gastrointestinal tract |journal=AJR Am J Roentgenol |volume=201 |issue=4 |pages=773–86 |date=October 2013 |pmid=24059366 |doi=10.2214/AJR.12.9758 |url=}}</ref><ref name="symptoms">Signs and symptoms of carcinoid syndrome. National Cancer Institute. http://www.cancer.gov/types/gi-carcinoid-tumors/patient/gi-carcinoid-treatment-pdq</ref><ref name="pmid15887161">{{cite journal |vauthors=Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD |title=Current status of gastrointestinal carcinoids |journal=Gastroenterology |volume=128 |issue=6 |pages=1717–51 |date=May 2005 |pmid=15887161 |doi= |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
Mild | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
* Intermittent | |||
* Secretory [[diarrhea]] | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Pellagra]] | |||
[[Dermatitis]] | |||
[[Diarrhea]] | |||
[[Dementia]] | |||
[[Metastatic]] [[tumors]] in the [[Liver (2)|liver]]: [[Right upper quadrant]] pain, [[Hepatomegaly (new)|hepatomegaly]], and early [[satiety]] | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[NT-proBNP]] | |||
** [[Screening]] of [[Carcinoid disease|carcinoid heart disease]] | |||
** Blood [[Serotonin]] levels | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Neuroendocrine tumor]] of [[midgut]] are difficult to identify on [[CT]] because of their small size. | |||
* Findings: [[Mass|mass-]]<nowiki/>like process with soft tissue "spokes" radiating into the [[mesenteric]] [[fat]] toward the [[small bowel]] causing retraction. | |||
* [[Liver]] [[metastases]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[Sensitivity|Sensitive]] for detection of [[Liver (2)|liver]] [[metastases]] | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
* Localization of [[carcinoid tumor]] | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* 68-Ga DOTATATE [[PET scan]] | |||
* [[Positron emission tomography-computed tomography]] ([[PET-CT]]) using 18[[-fluoro-dihydroxyphenylalanine]] | |||
* Ki-67 labeling index | |||
* [[Endoscopy]] for [[metastatic]] [[Neuroendocrine tumour]] with an unknown primary site. | |||
| | |||
* Valve thickening with retraction and reduction in the mobility of the [[Tricuspid valves|tricuspid valve]] | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Enterochromaffin cells|Enterochromaffin]] [[cells]] stain with [[Potassium chromate|potassium chromate (chromaffin]]). | |||
*On [[electron microscopy]] ,the [[cells]] in [[tumors]] are found to contain [[membrane]]-bound [[Granules|secretory granules]] with dense-core [[granules]] in the [[cytoplasm]]. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Somatostatin receptor scintigraphy [SRS], or [[Octreoscan]] | |||
* [[Biopsy]] and [[histopathology]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Mesenteric]] [[fibrosis]] | |||
Pathognomonic radiological sign of [[midgut]] [[Neuroendocrine tumor|NET]]. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Neuroendocrine tumor]] of [[lung]]<ref name="pmid18473355">{{cite journal |vauthors=Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM |title=Bronchopulmonary neuroendocrine tumors |journal=Cancer |volume=113 |issue=1 |pages=5–21 |date=July 2008 |pmid=18473355 |doi=10.1002/cncr.23542 |url=}}</ref><ref name="JeungGasser2002">{{cite journal|last1=Jeung|first1=Mi-Young|last2=Gasser|first2=Bernard|last3=Gangi|first3=Afshin|last4=Charneau|first4=Dominique|last5=Ducroq|first5=Xavier|last6=Kessler|first6=Romain|last7=Quoix|first7=Elisabeth|last8=Roy|first8=Catherine|title=Bronchial Carcinoid Tumors of the Thorax: Spectrum of Radiologic Findings|journal=RadioGraphics|volume=22|issue=2|year=2002|pages=351–365|issn=0271-5333|doi=10.1148/radiographics.22.2.g02mr01351}}</ref><ref name="pmid1649924">{{cite journal |vauthors=Nessi R, Basso Ricci P, Basso Ricci S, Bosco M, Blanc M, Uslenghi C |title=Bronchial carcinoid tumors: radiologic observations in 49 cases |journal=J Thorac Imaging |volume=6 |issue=2 |pages=47–53 |date=April 1991 |pmid=1649924 |doi= |url=}}</ref><ref name="pmid5831899">{{cite journal |vauthors=Melmon KL, Sjoerdsma A, Mason DT |title=Distinctive clinical and therapeutic aspects of the syndrome associated with bronchial carcinoid tumors |journal=Am. J. Med. |volume=39 |issue=4 |pages=568–81 |date=October 1965 |pmid=5831899 |doi= |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Cough]] | |||
* [[Hemoptysis]] | |||
* [[Chest pain]] | |||
* [[Fever]] due to [[Pneumonia|post -obstructuve pneuomnia]] | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Immunohistochemical stains]]: | |||
* [[Synaptophysin]] | |||
* [[Neuron-specific enolase]] | |||
* [[NT-proBNP]] | |||
* Low [[serotonin]] content as compared to [[midgut]] [[Tumors|tumors.]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Atypical [[neuroendocrine tumors]] have a greater tendency to [[metastasize]] to [[Liver|liver,]][[hypervascular]], and becomies isodense relative to th[[Liver|e liver]] [[parenchyma]] after [[contrast]] administration. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" |[[Sensitivity (tests)|Sensitive]] for detection o[[Liver (2)|f liver]] [[metastases]] if present | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Chest X ray]]: round or oval [[Opacity|opacities]] from 2-5cm with sharp and notched margins | |||
* [[Chest]] [[CT]] : [[Hilar]] or Perihilar Masses, Endobronchial [[Nodules]],Related to [[Bronchial|bronchial Obstruction]]:peripheral [[atelectasis]] and postobstructive [[pneumonia]] | |||
* [[PFTs|Pulmonary funcation test]] | |||
* [[Bronchoscopy]] | |||
* [[68-Ga DOTATATE PET scan]] | |||
* Fluorodeoxyglucose [[PET scan|PET scans]] for atypical [[lung]] [[Neuroendocrine|NETs]] . | |||
| - | |||
| style="background: #F5F5F5; padding: 5px;" |Typical low-grade:bland cells containing regular round [[nuclei]] with finely dispersed [[chromatin]] and inconspicuous small [[nucleoli]].Mitotic figures are scarce and [[necrosis]] is absent. | |||
Intermediate-grade atypical: presence of [[Neuroendocrine]] morphology and either [[necrosis]] or 2 to 10 [[mitoses]] per 10 HPF | |||
| | |||
* [[Biopsy]] and [[histopathology]] | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Irritable Bowel Syndrome]]<ref name="pmid18371141">{{cite journal |vauthors=Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P |title=Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior |journal=Am. J. Gastroenterol. |volume=103 |issue=5 |pages=1229–39; quiz 1240 |date=May 2008 |pmid=18371141 |doi=10.1111/j.1572-0241.2007.01740.x |url=}}</ref><ref name="pmid28374308">{{cite journal |vauthors=Simren M, Palsson OS, Whitehead WE |title=Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice |journal=Curr Gastroenterol Rep |volume=19 |issue=4 |pages=15 |date=April 2017 |pmid=28374308 |pmc=5378729 |doi=10.1007/s11894-017-0554-0 |url=}}</ref><ref name="pmid12454865">{{cite journal |vauthors= |title=American Gastroenterological Association medical position statement: irritable bowel syndrome |journal=Gastroenterology |volume=123 |issue=6 |pages=2105–7 |date=December 2002 |pmid=12454865 |doi=10.1053/gast.2002.37095b |url=}}</ref><ref name="pmid27144627">{{cite journal |vauthors=Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R |title=Bowel Disorders |journal=Gastroenterology |volume= |issue= |pages= |date=February 2016 |pmid=27144627 |doi=10.1053/j.gastro.2016.02.031 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
Perioidic | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Intermittent | |||
* Chronic history of [[Diarrhea|diarhea]] alternating with [[constipation]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* | |||
* [[Fibromyalgia]] | |||
* [[Chronic fatigue syndrome]] | |||
* [[Gastroesophageal reflux disease]], | |||
* [[Functional dyspepsia]] | |||
* [[Non-cardiac chest pain]], | |||
* [[Major depression]] | |||
* ,[[Anxiety Disorder|Anxiety]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| | |||
* [[Bristol stool]] form scale should to record [[stool]] consistency | |||
* [[Abdominal|Abdomina]]<nowiki/>l [[Radiographic|radiograph]] to assess for [[Stool|stoo]]<nowiki/>l accumulation and determine the severity. | |||
* Age-appropriate [[colorectal cancer]] [[screening]] in all [[patients]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |[[Rome IV criteria]] | |||
* Recurrent [[abdominal pain]], at least 1day/week in the last 3 months, a/s with 2 or more of the following criteria: | |||
•Related to [[defecation]] | |||
•Associated with a change in [[stool]] frequency | |||
•Associated with a change in [[stool]] form (appearance) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Small intestine cancer|Malignant neoplasms of small intestine]]<ref name="pmid23789703">{{cite journal |vauthors=McLaughlin PD, Maher MM |title=Primary malignant diseases of the small intestine |journal=AJR Am J Roentgenol |volume=201 |issue=1 |pages=W9–14 |date=July 2013 |pmid=23789703 |doi=10.2214/AJR.12.8492 |url=}}</ref><ref name="pmid17372046">{{cite journal |vauthors=Hatzaras I, Palesty JA, Abir F, Sullivan P, Kozol RA, Dudrick SJ, Longo WE |title=Small-bowel tumors: epidemiologic and clinical characteristics of 1260 cases from the connecticut tumor registry |journal=Arch Surg |volume=142 |issue=3 |pages=229–35 |date=March 2007 |pmid=17372046 |doi=10.1001/archsurg.142.3.229 |url=}}</ref><ref name="pmid17026561">{{cite journal |vauthors=Lepage C, Bouvier AM, Manfredi S, Dancourt V, Faivre J |title=Incidence and management of primary malignant small bowel cancers: a well-defined French population study |journal=Am. J. Gastroenterol. |volume=101 |issue=12 |pages=2826–32 |date=December 2006 |pmid=17026561 |doi=10.1111/j.1572-0241.2006.00854.x |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Constipation]] | |||
* [[Fatigue]] | |||
* Early [[satiety]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |* [[Abdominal mass]] | |||
* [[Ascites]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" |[[Abdominal]] [[CT scan]] may be diagnostic of [[Small intestine cancer|small intestine cancer.]] Findings on [[CT scan]] suggestive of [[Small intestine cancer CT|small intestine cancer]] include intrinsic [[mass]] with a short segment of [[Bowel|bowel wall]] thickening | |||
| style="background: #F5F5F5; padding: 5px;" |[[MRI]] and [[MRI enteroscopy]] are other advance modalities to [[diagnose]] and [[Staging (pathology)|stage]] [[Small intestine cancer|small intestinal cancers]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |[[Endoscopy|Enteroscopy]], [[capsule endoscopy]] and double balloon [[enteroscopy]] | |||
| | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[Adenocarcinoma|Adenocarcinomas]] may be polypoid, infiltrating, or as annular constricting lesions is [[small intestine]]. | |||
*[[Polyps]] and [[adenomas]] of [[small intestine]] are considered precursor lesions of [[adenocarcinoma]]. | |||
*[[Lymphoma|Lymphomas]] of [[small intestine]] present with suspicious growths in [[submucosa]] with normal appearing [[muscosa]]. | |||
*[[Endoscopy|Endoscopic]] evaluation may show multifocal involvement and large [[biopsies]] are required for diagnoses | |||
|[[Biopsy]] and [[histopathology]] | |||
| | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Crohn disease]]<ref name="pmid18649092">{{cite journal |vauthors=Hara AK, Swartz PG |title=CT enterography of Crohn's disease |journal=Abdom Imaging |volume=34 |issue=3 |pages=289–95 |date=2009 |pmid=18649092 |doi=10.1007/s00261-008-9443-1 |url=}}</ref><ref name="BaumgartSandborn2012">{{cite journal|last1=Baumgart|first1=Daniel C|last2=Sandborn|first2=William J|title=Crohn's disease|journal=The Lancet|volume=380|issue=9853|year=2012|pages=1590–1605|issn=01406736|doi=10.1016/S0140-6736(12)60026-9}}</ref><ref name="FeuersteinCheifetz2017">{{cite journal|last1=Feuerstein|first1=Joseph D.|last2=Cheifetz|first2=Adam S.|title=Crohn Disease: Epidemiology, Diagnosis, and Management|journal=Mayo Clinic Proceedings|volume=92|issue=7|year=2017|pages=1088–1103|issn=00256196|doi=10.1016/j.mayocp.2017.04.010}}</ref><ref name="García-BoschOrdás2016">{{cite journal|last1=García-Bosch|first1=O.|last2=Ordás|first2=I.|last3=Aceituno|first3=M.|last4=Rodríguez|first4=S.|last5=Ramírez|first5=A. M.|last6=Gallego|first6=M.|last7=Ricart|first7=E.|last8=Rimola|first8=J.|last9=Panes|first9=J.|title=Comparison of Diagnostic Accuracy and Impact of Magnetic Resonance Imaging and Colonoscopy for the Management of Crohn’s Disease|journal=Journal of Crohn's and Colitis|volume=10|issue=6|year=2016|pages=663–669|issn=1873-9946|doi=10.1093/ecco-jcc/jjw015}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Right lower quadrant abdominal pain resident survival guide|Right lower quadrant]] [[pain]] | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Gross [[bloody diarrhea]] +/- | |||
* [[Weight loss]] | |||
* [[Fatigue (physical)|Fatigue]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* | |||
* [[Weight loss]] | |||
* [[Pallor]] | |||
* [[Oral lesions]] | |||
* [[Odynophagia]] | |||
* [[Dysphagia]] | |||
* Perianal skin tags | |||
* [[Sinus tracts]] | |||
* [[Gallstones]] | |||
* Extraintestinal manifestations | |||
* [[Arthritis]] | |||
* [[Uveitis]], [[Iritis]], and [[Episcleritis]] | |||
* [[Erythema nodosum]] and [[Pyoderma gangrenosum]] | |||
* [[Primary sclerosing cholangitis]] | |||
* Secondary [[amyloidosis]] | |||
* [[Thromboembolism]] | |||
* [[Renal stones]] | |||
* [[Osteoporosis]] | |||
* [[Vitamin B12 deficiency]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[CRP]] may be high | |||
* [[p-ANCA]] and [[Anti saccharomyces cerevisiae antibodies|ASCA]] | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* CT enterography [[:Small bowel]] [[inflammation]] by displaying mural hyperenhancement and thickening; engorged [[vasa recta]]; and [[perienteric]] [[inflammatory]] changes. | |||
| | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| | |||
* [[CBC]] | |||
* [[Blood chemistry tests|Blood chemistry]] including [[Electrolyte|electrolytes]] | |||
* [[Kidney function|Renal function tests]] | |||
* [[liver enzymes]] | |||
* [[Blood glucose]] | |||
* [[ESR]] | |||
* [[CRP]] | |||
* [[Serum iron]] | |||
* [[Vitamin D]] & [[vitamin B12 levels]] | |||
* [[Stool D/R]] and [[Culture media|culture]] for [[ova]] and [[parasites]], | |||
* [[Clostridium difficile|''C. difficile'' toxin]] | |||
|<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Focal ulcerations and acute and chronic inflammation | |||
* [[Granulomas]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Colonoscopic|Colonoscop]]<nowiki/>y:focal ulcerations adjacent to areas of normal appearing [[mucosa]] along with polypoid mucosa[[Skip lesion|l,skip lesion]]<nowiki/>s,[[pseudopolyps]], | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Benign cutaneous flushing]]<ref name="IziksonEnglish2006">{{cite journal|last1=Izikson|first1=Leonid|last2=English|first2=Joseph C.|last3=Zirwas|first3=Matthew J.|title=The flushing patient: Differential diagnosis, workup, and treatment|journal=Journal of the American Academy of Dermatology|volume=55|issue=2|year=2006|pages=193–208|issn=01909622|doi=10.1016/j.jaad.2005.07.057}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Mastocytosis|Systemic mastocytosis]]<ref name="HartmannEscribano2016">{{cite journal|last1=Hartmann|first1=Karin|last2=Escribano|first2=Luis|last3=Grattan|first3=Clive|last4=Brockow|first4=Knut|last5=Carter|first5=Melody C.|last6=Alvarez-Twose|first6=Ivan|last7=Matito|first7=Almudena|last8=Broesby-Olsen|first8=Sigurd|last9=Siebenhaar|first9=Frank|last10=Lange|first10=Magdalena|last11=Niedoszytko|first11=Marek|last12=Castells|first12=Mariana|last13=Oude Elberink|first13=Joanna N.G.|last14=Bonadonna|first14=Patrizia|last15=Zanotti|first15=Roberta|last16=Hornick|first16=Jason L.|last17=Torrelo|first17=Antonio|last18=Grabbe|first18=Jürgen|last19=Rabenhorst|first19=Anja|last20=Nedoszytko|first20=Boguslaw|last21=Butterfield|first21=Joseph H.|last22=Gotlib|first22=Jason|last23=Reiter|first23=Andreas|last24=Radia|first24=Deepti|last25=Hermine|first25=Olivier|last26=Sotlar|first26=Karl|last27=George|first27=Tracy I.|last28=Kristensen|first28=Thomas K.|last29=Kluin-Nelemans|first29=Hanneke C.|last30=Yavuz|first30=Selim|last31=Hägglund|first31=Hans|last32=Sperr|first32=Wolfgang R.|last33=Schwartz|first33=Lawrence B.|last34=Triggiani|first34=Massimo|last35=Maurer|first35=Marcus|last36=Nilsson|first36=Gunnar|last37=Horny|first37=Hans-Peter|last38=Arock|first38=Michel|last39=Orfao|first39=Alberto|last40=Metcalfe|first40=Dean D.|last41=Akin|first41=Cem|last42=Valent|first42=Peter|title=Cutaneous manifestations in patients with mastocytosis: Consensus report of the European Competence Network on Mastocytosis; the American Academy of Allergy, Asthma & Immunology; and the European Academy of Allergology and Clinical Immunology|journal=Journal of Allergy and Clinical Immunology|volume=137|issue=1|year=2016|pages=35–45|issn=00916749|doi=10.1016/j.jaci.2015.08.034}}</ref><ref name="LeeWhittaker2008">{{cite journal|last1=Lee|first1=Jason K|last2=Whittaker|first2=Scott J|last3=Enns|first3=Robert A|last4=Zetler|first4=Peter|title=Gastrointestinal manifestations of systemic mastocytosis|journal=World Journal of Gastroenterology|volume=14|issue=45|year=2008|pages=7005|issn=1007-9327|doi=10.3748/wjg.14.7005}}</ref><ref name="pmid2002264">{{cite journal |vauthors=Horan RF, Austen KF |title=Systemic mastocytosis: retrospective review of a decade's clinical experience at the Brigham and Women's Hospital |journal=J. Invest. Dermatol. |volume=96 |issue=3 |pages=5S–13S; discussion 13S–14S |date=March 1991 |pmid=2002264 |doi= |url=}}</ref><ref name="SokolGeorgin-Lavialle2010">{{cite journal|last1=Sokol|first1=Harry|last2=Georgin-Lavialle|first2=Sophie|last3=Grandpeix-Guyodo|first3=Catherine|last4=Canioni|first4=Danielle|last5=Barete|first5=Stéphane|last6=Dubreuil|first6=Patrice|last7=Lortholary|first7=Olivier|last8=Beaugerie|first8=Laurent|last9=Hermine|first9=Olivier|title=Gastrointestinal involvement and manifestations in systemic mastocytosis|journal=Inflammatory Bowel Diseases|volume=16|issue=7|year=2010|pages=1247–1253|issn=1078-0998|doi=10.1002/ibd.21218}}</ref><ref name="pmid17063092">{{cite journal |vauthors=Bedeir A, Jukic DM, Wang L, Mullady DK, Regueiro M, Krasinskas AM |title=Systemic mastocytosis mimicking inflammatory bowel disease: A case report and discussion of gastrointestinal pathology in systemic mastocytosis |journal=Am. J. Surg. Pathol. |volume=30 |issue=11 |pages=1478–82 |date=November 2006 |pmid=17063092 |doi=10.1097/01.pas.0000213310.51553.d7 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Maculopapular rash]] | |||
* [[Pruritus]] | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Diffuse [[musculoskeletal pain]] | |||
* [[Neuropsychiatric symptoms]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Activating [[mutations]] of ''[[KIT]]'' | |||
* Serum [[Tryptase]] levels | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Asthma]] exacerbation<ref name="pmid22386508">{{cite journal |vauthors=Fuhlbrigge A, Peden D, Apter AJ, Boushey HA, Camargo CA, Gern J, Heymann PW, Martinez FD, Mauger D, Teague WG, Blaisdell C |title=Asthma outcomes: exacerbations |journal=J. Allergy Clin. Immunol. |volume=129 |issue=3 Suppl |pages=S34–48 |date=March 2012 |pmid=22386508 |pmc=3595577 |doi=10.1016/j.jaci.2011.12.983 |url=}}</ref><ref name="pmid16337448">{{cite journal |vauthors=Limb SL, Brown KC, Wood RA, Wise RA, Eggleston PA, Tonascia J, Adkinson NF |title=Irreversible lung function deficits in young adults with a history of childhood asthma |journal=J. Allergy Clin. Immunol. |volume=116 |issue=6 |pages=1213–9 |date=December 2005 |pmid=16337448 |doi=10.1016/j.jaci.2005.09.024 |url=}}</ref><ref name="pmid17468458">{{cite journal |vauthors=Aldington S, Beasley R |title=Asthma exacerbations. 5: assessment and management of severe asthma in adults in hospital |journal=Thorax |volume=62 |issue=5 |pages=447–58 |date=May 2007 |pmid=17468458 |pmc=2117186 |doi=10.1136/thx.2005.045203 |url=}}</ref><ref name="pmid19187331">{{cite journal |vauthors=Dougherty RH, Fahy JV |title=Acute exacerbations of asthma: epidemiology, biology and the exacerbation-prone phenotype |journal=Clin. Exp. Allergy |volume=39 |issue=2 |pages=193–202 |date=February 2009 |pmid=19187331 |pmc=2730743 |doi=10.1111/j.1365-2222.2008.03157.x |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Tachypnea | |||
* Prolonged expiratory phase of respiration (decreased I:E ratio) | |||
* Seated position with use of extended arms to support the upper chest (tripod position) | |||
* +/- Pulsus paradoxus | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | -- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
|[[Chest X ray]] | |||
| - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Loss of the normal pseudostratified structure of airway epithelium | |||
* Increase in the proportion of goblet cells | |||
* Fibrotic thickening of the sub-epithelial reticular basement membrane | |||
* Increased numbers of myofibroblasts | |||
* Increased vascularity | |||
* Increased airway smooth muscle mass | |||
* Increased extracellular matrix | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Anaphylaxis]]<ref name="pmid18596587">{{cite journal |vauthors=Peavy RD, Metcalfe DD |title=Understanding the mechanisms of anaphylaxis |journal=Curr Opin Allergy Clin Immunol |volume=8 |issue=4 |pages=310–5 |date=August 2008 |pmid=18596587 |pmc=2683407 |doi=10.1097/ACI.0b013e3283036a90 |url=}}</ref><ref name="pmid20944042">{{cite journal |vauthors=Tupper J, Visser S |title=Anaphylaxis: A review and update |journal=Can Fam Physician |volume=56 |issue=10 |pages=1009–11 |date=October 2010 |pmid=20944042 |pmc=2954079 |doi= |url=}}</ref><ref name="pmid12209078">{{cite journal |vauthors=Kemp SF, Lockey RF |title=Anaphylaxis: a review of causes and mechanisms |journal=J. Allergy Clin. Immunol. |volume=110 |issue=3 |pages=341–8 |date=September 2002 |pmid=12209078 |doi= |url=}}</ref><ref name="pmid21293765">{{cite journal |vauthors=Bjornsson HM, Graffeo CS |title=Improving diagnostic accuracy of anaphylaxis in the acute care setting |journal=West J Emerg Med |volume=11 |issue=5 |pages=456–61 |date=December 2010 |pmid=21293765 |pmc=3027438 |doi= |url=}}</ref><ref name="urlUsefulness and Limitations of Sequential Serum Tryptase for the Diagnosis of Anaphylaxis in 102 Patients - FullText - International Archives of Allergy and Immunology 2013, Vol. 160, No. 2 - Karger Publishers">{{cite web |url=https://www.karger.com/Article/Fulltext/339749 |title=Usefulness and Limitations of Sequential Serum Tryptase for the Diagnosis of Anaphylaxis in 102 Patients - FullText - International Archives of Allergy and Immunology 2013, Vol. 160, No. 2 - Karger Publishers |format= |work= |accessdate=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | -/+ | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Vomiting]] | |||
* [[Hives|Generalized hives]], | |||
* [[Pruritus]] | |||
* [[Itching]] | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Swollen [[lips]]-[[tongue]]-[[uvula]] | |||
* [[Periorbital edema]], | |||
* [[Conjunctival|Conjunctival swelling]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* plasma [[tryptase]] | |||
* Plasm[[Histamine|a histamine]] levels | |||
* Take proper clinical history and medication history specially [[beta blockers]],[[Angiotensin Converting Enzyme Inhibitor|ACE-inhibitors,]][[opioids]] | |||
* [[Skin testing]] with [[Allergens|allergen extracts]] | |||
* [[Enzyme linked immunosorbent assay (ELISA)|enzyme-linked immunosorbent assays (ELISAs)]] for quantification of allergen-specific [[IgE]] levels | |||
* | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|History of exposure to [[Insect allergy|insect]] stings,food alllergy,rubber latex,food [[Additives|additives,]],allergy to medications,physical factors such s excercise and cold | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Histaminergic [[Angioedema]]<ref name="pmid28687103">{{cite journal |vauthors=Busse PJ, Smith T |title=Histaminergic Angioedema |journal=Immunol Allergy Clin North Am |volume=37 |issue=3 |pages=467–481 |date=August 2017 |pmid=28687103 |doi=10.1016/j.iac.2017.03.001 |url=}}</ref><ref name="pmid28818177">{{cite journal |vauthors=Hahn J, Hoffmann TK, Bock B, Nordmann-Kleiner M, Trainotti S, Greve J |title=Angioedema |journal=Dtsch Arztebl Int |volume=114 |issue=29-30 |pages=489–496 |date=July 2017 |pmid=28818177 |pmc=5569554 |doi=10.3238/arztebl.2017.0489 |url=}}</ref><ref name="pmid28405953">{{cite journal |vauthors=Bernstein JA, Cremonesi P, Hoffmann TK, Hollingsworth J |title=Angioedema in the emergency department: a practical guide to differential diagnosis and management |journal=Int J Emerg Med |volume=10 |issue=1 |pages=15 |date=December 2017 |pmid=28405953 |pmc=5389952 |doi=10.1186/s12245-017-0141-z |url=}}</ref><ref name="pmid23131076">{{cite journal |vauthors=Bernstein JA, Moellman J |title=Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema |journal=Int J Emerg Med |volume=5 |issue=1 |pages=39 |date=November 2012 |pmid=23131076 |pmc=3518251 |doi=10.1186/1865-1380-5-39 |url=}}</ref><ref name="pmid23282406">{{cite journal |vauthors=Kaplan AP |title=Angioedema |journal=World Allergy Organ J |volume=1 |issue=6 |pages=103–13 |date=June 2008 |pmid=23282406 |pmc=3651192 |doi=10.1097/WOX.0b013e31817aecbe |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Generalized [[pruritus]] | |||
* [[Throat]] tightness | |||
* [[Hoarse voice]] | |||
* [[Difficulty swallowing]] | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Urticaria]] | |||
* Localized [[swelling]] of [[skin]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Bowel|Bowel wall]] edema | |||
* Circumferential thickening of the [[Small bowel|small bowel wall]] with [[ascites]] or incomplete [[obstruction]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[CBC|CBC with differential,]] | |||
* [[Electrolyte|Electrolytes]] | |||
* [[Liver function tests]] | |||
* [[C-reactive protein (CRP)|C-reactive protein]] | |||
* [[ESR|Erythrocyte sedimentation rate]] | |||
* Levels of the [[Complement System|complement protein C4]] | |||
* Serum tota[[Tryptase|l tryptase]] | |||
* Allergen-specific [[IgE immunoassay|IgE immunoassays]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Take proper clinical history of previous similar episodes | |||
* Medication history | |||
* Any allergy to insects stings , foods or any ingestion within previous 24 hours | |||
|- | |||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Medullary carcinoma of thyroid|Medullary Thyroid Carcinoma]]<ref name="pmid20627492">{{cite journal |vauthors=Pacini F, Castagna MG, Cipri C, Schlumberger M |title=Medullary thyroid carcinoma |journal=Clin Oncol (R Coll Radiol) |volume=22 |issue=6 |pages=475–85 |date=August 2010 |pmid=20627492 |doi=10.1016/j.clon.2010.05.002 |url=}}</ref><ref name="pmid24037980">{{cite journal |vauthors=Roy M, Chen H, Sippel RS |title=Current understanding and management of medullary thyroid cancer |journal=Oncologist |volume=18 |issue=10 |pages=1093–100 |date=2013 |pmid=24037980 |pmc=3805151 |doi=10.1634/theoncologist.2013-0053 |url=}}</ref><ref name="pmid24552221">{{cite journal |vauthors=Mian C, Perrino M, Colombo C, Cavedon E, Pennelli G, Ferrero S, De Leo S, Sarais C, Cacciatore C, Manfredi GI, Verga U, Iacobone M, De Pasquale L, Pelizzo MR, Vicentini L, Persani L, Fugazzola L |title=Refining calcium test for the diagnosis of medullary thyroid cancer: cutoffs, procedures, and safety |journal=J. Clin. Endocrinol. Metab. |volume=99 |issue=5 |pages=1656–64 |date=May 2014 |pmid=24552221 |doi=10.1210/jc.2013-4088 |url=}}</ref><ref name="pmid26494386">{{cite journal |vauthors=Bae YJ, Schaab M, Kratzsch J |title=Calcitonin as Biomarker for the Medullary Thyroid Carcinoma |journal=Recent Results Cancer Res. |volume=204 |issue= |pages=117–37 |date=2015 |pmid=26494386 |doi=10.1007/978-3-319-22542-5_5 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | +/- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Neck pain]] | |||
* [[Hoarseness]] | |||
* [[Cough]] | |||
* [[Difficulty swallowing]] | |||
* [[Difficulty breathing]] | |||
* [[Lethargy]] | |||
* [[Bone pain]] from [[metastasis]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Solitary thyroid nodule]] | |||
* [[Cervical lymph nodes|Cervical lymph node involvement]] | |||
* [[Weight loss]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Basal serum [[calcitonin]] concentrations | |||
* [[Carcinoembryonic antigen peptide-1|Carcinoembryonic antigen (CEA) concentration]] | |||
* [[Thyroid function tests]]: normal | |||
* [[Germline]] ''[[RET gene|RET]]'' testing | |||
* [[Calcium|Serum calcium]] | |||
* Plasma fractionated [[Metanephrine|metanephrines]] | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |- | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Ultrasonography]] of the [[neck]] | |||
Fo[[Metastasis|r metastasis]] | |||
* [[Chest]] [[computed tomography]] | |||
* [[Neck]] [[CT]] | |||
* Three-phase contrast-enhanced [[Liver (2)|liver]] [[CT-scans|CT]] | |||
* Axial [[MRI]] | |||
* Bone [[scintigraphy]]. | |||
| style="background: #F5F5F5; padding: 5px;" | - | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Immunohistochemical staining]] for [[calcitonin]] | |||
* [[Spindle cells|Spindle]]-shaped and frequently [[Pleomorphic|pleomorphic cells]] without follicle development | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Fine-needle aspiration|Fine-needle aspiration (FNA) biopsy]] | |||
* [[TNM staging system|TNM staging]] | |||
* American Thyroid Association (ATA) Guidelines for Management and evaluation of [[Medullary carcinoma of the thyroid|Medullary Thyroid Cancer]] | |||
| | |||
|} | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Autoimmune diseases]] | [[Category:Autoimmune diseases]] | ||
| Line 57: | Line 1,338: | ||
[[Category:Conditions diagnosed by stool test]] | [[Category:Conditions diagnosed by stool test]] | ||
[[Category:Abdominal pain]] | [[Category:Abdominal pain]] | ||
[[Category:Needs overview]] | [[Category:Needs overview]] | ||
Latest revision as of 21:22, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
Differentiating Crohn's Disease from other Diseases
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Terminal ileum involvement | Commonly | Seldom |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually[1] |
| Involvement around the anus | Common[2] | Seldom |
| Bile duct involvement | No increase in rate of primary sclerosing cholangitis | Higher rate[3] |
| Distribution of Disease | Patchy areas of inflammation (Skip lesions) | Continuous area of inflammation[1] |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers | Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues[2] | Shallow, mucosal |
| Fistulae | Common[2] | Seldom |
| Stenosis | Common | Seldom |
| Autoimmune disease | Widely regarded as an autoimmune disease | No consensus |
| Cytokine response | Associated with Th1 | Vaguely associated with Th2 |
| Granulomas on biopsy | Can have granulomas[2] | Granulomas uncommon[1] |
| Surgical cure | Often returns following removal of affected part | Usually cured by removal of colon |
| Smoking | Higher risk for smokers | Lower risk for smokers[1] |
Oral lesioins of Crohn's disease must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
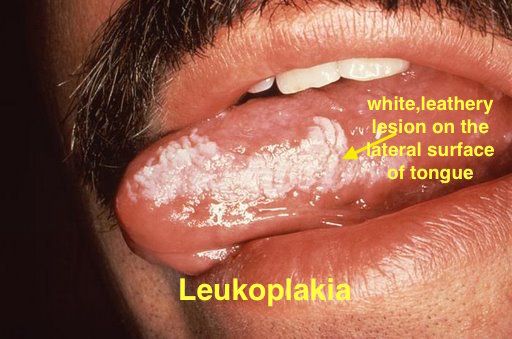 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
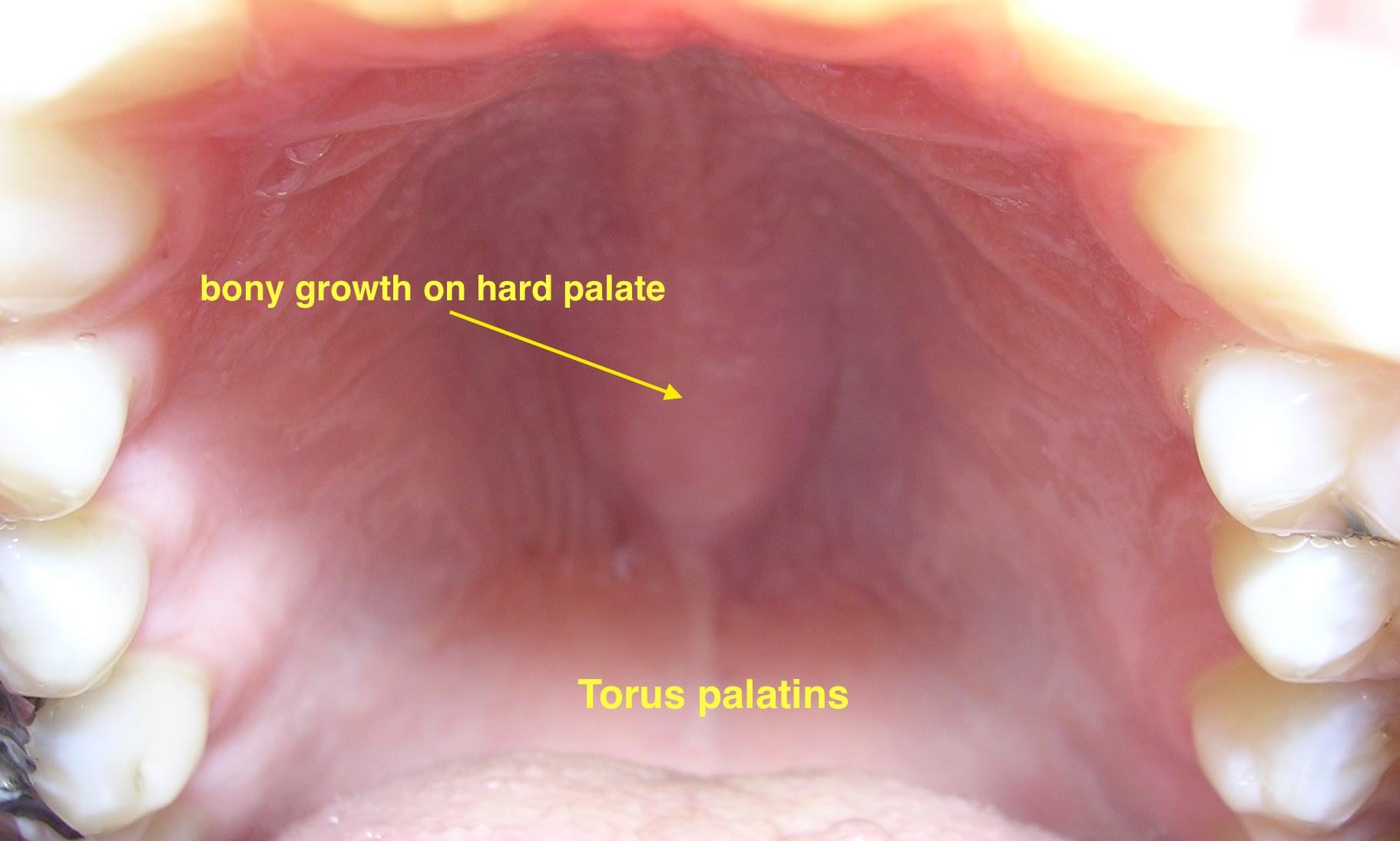 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[6] |
|
|
|
 | ||
| Coxsackie virus |
|
|
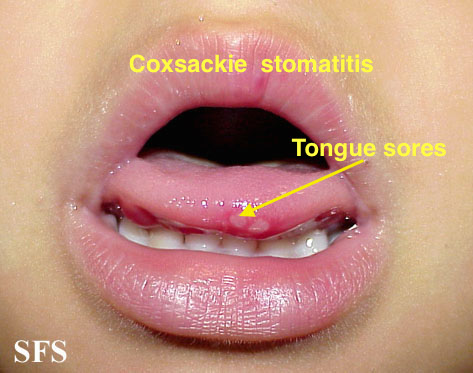
| |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
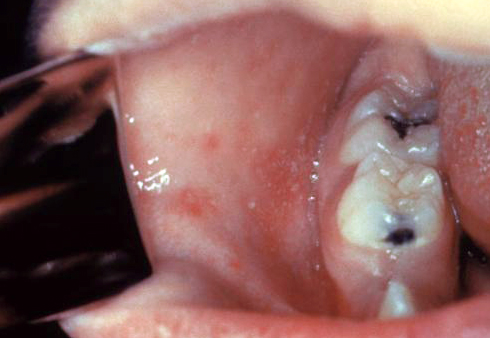 | ||
The following table differentiates all the diseases presenting with abdominal pain, fever and lower gastrointestinal bleeding.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Abbreviations: RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein, TS= Transferrin saturation, SF= Serum Ferritin, SMA= Superior mesenteric artery, SMV= Superior mesenteric vein, ECG= Electrocardiogram
Differentiating Crohn's disease from other causes of abdominal pain and diarrhea
Crohn's disease must be differentiated from other causes of abdominal pain and diarrhea.
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard | Additional findings | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | ||||||||||||||||||||||||
| Lab Findings | Imaging | Histopathology | |||||||||||||||||||||||
| Abdominal pain | Diarrhea | Flushing | Dyspnea | Palpitations | Other symptoms | Wheezing | Telangiectasia | Hypotension | Tachycardia | Systolic murmur of tricuspid regurgitation | Other physical findings | Urinary 5-hydroxyindoleacetic acid (5-HIAA) | Serum Chromogranin A (CgA) | Other markers | Abdominal computed tomography (CT) | Abdominal MRI | Somatostatin receptor scintigraphy [SRS], or Octreoscan | Metaiodobenzylguanidine (MIBG) scintigraphy | Other diagnostic studies | Transthoracic echocardiography | |||||
| Carcinoid Syndrome[9][10][11][12][13][14][15][16][17] | Neuroendocrine tumor of midgut [18][19][20][21] | +
Mild |
+
|
+ | + | + |
Metastatic tumors in the liver: Right upper quadrant pain, hepatomegaly, and early satiety |
+ | +/- | +/- | + | + | - | + | + |
|
|
|
+
|
+ |
|
|
|
|
|
| Neuroendocrine tumor of lung[22][23][24][25] | + | + | + | + | + |
|
+ | +/- | +/- | + | + | - | + | + |
|
Sensitive for detection of liver metastases if present | + | + |
|
- | Typical low-grade:bland cells containing regular round nuclei with finely dispersed chromatin and inconspicuous small nucleoli.Mitotic figures are scarce and necrosis is absent.
Intermediate-grade atypical: presence of Neuroendocrine morphology and either necrosis or 2 to 10 mitoses per 10 HPF |
| |||
| Irritable Bowel Syndrome[26][27][28][29] | +
Perioidic |
|
- | - | - | - | - | - | - | - | - | - | - | - | - | - |
|
- | - | Rome IV criteria
•Related to defecation •Associated with a change in stool frequency •Associated with a change in stool form (appearance) |
|||||
| Malignant neoplasms of small intestine[30][31][32] | +/- | +/- | - | - | +/- |
|
- | - | +/- | - | * Abdominal mass | - | + | Abdominal CT scan may be diagnostic of small intestine cancer. Findings on CT scan suggestive of small intestine cancer include intrinsic mass with a short segment of bowel wall thickening | MRI and MRI enteroscopy are other advance modalities to diagnose and stage small intestinal cancers | - | - | Enteroscopy, capsule endoscopy and double balloon enteroscopy |
|
Biopsy and histopathology | |||||
| Crohn disease[33][34][35][36] | +/- | - | - | - |
|
- | - | - | - | - |
|
- | - |
|
- | - |
|
- |
|
|
|||||
| Benign cutaneous flushing[37] | - | - | + | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||
| Systemic mastocytosis[38][39][40][41][42] | + | + | + | + | - | +/- | +/- | + | - | - | - | - | - | - | |||||||||||
| Asthma exacerbation[43][44][45][46] | - | - | - | + | + | + | - | - | + | - |
|
- | - | - | -- | - | - | - | Chest X ray | - |
|
||||
| Anaphylaxis[47][48][49][50][51] | + | -/+ | + | + | + | +/- | - | + | + | - | - | - | - | - | - | - | - |
|
- | - | History of exposure to insect stings,food alllergy,rubber latex,food additives,,allergy to medications,physical factors such s excercise and cold | ||||
| Histaminergic Angioedema[52][53][54][55][56] | +/- | +/- | + | + | + |
|
+ | - | + | + | - | - | - | - |
|
- | - | - |
|
- | - | - |
| ||
| Medullary Thyroid Carcinoma[57][58][59][60] | - | +/- | +/- | +/- | - | - | - | - | - | - | - | - |
|
- | - | - | - |
|
- |
|
|
||||
References
- ↑ 1.0 1.1 1.2 1.3 Kornbluth, Asher. "Ulcerative Colitis Practice Guidelines in Adults" (PDF). American Journal of Gastroenterology. doi:10.1111/j.1572-0241.2004.40036.x. PMID 15233681. Retrieved 2006-11-08.
- ↑ 2.0 2.1 2.2 2.3 Hanauer, Stephen B. "Management of Crohn's Disease in Adults" (PDF). American Journal of Gastroenterology. 96 (3): 635–643. doi:10.1111/j.1572-0241.2001.03671.x. PMID 11280528. Retrieved 2006-11-08.
- ↑ Broomé, Ulrika. "Primary sclerosing cholangitis, inflammatory bowel disease, and colon cancer". Seminars in Liver Disease. 26 (1): 31–41. doi:10.1055/s-2006-933561. PMID 16496231.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar. "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312.
- ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur. J. Intern. Med. 17 (8): 529–35. doi:10.1016/j.ejim.2006.07.012. PMID 17142169.
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Rubin de Celis Ferrari AC, Glasberg J, Riechelmann RP (August 2018). "Carcinoid syndrome: update on the pathophysiology and treatment". Clinics (Sao Paulo). 73 (suppl 1): e490s. doi:10.6061/clinics/2018/e490s. PMC 6096975. PMID 30133565.
- ↑ Hegyi J, Schwartz RA, Hegyi V (January 2004). "Pellagra: dermatitis, dementia, and diarrhea". Int. J. Dermatol. 43 (1): 1–5. PMID 14693013.
- ↑ Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E (May 2004). "Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours". Nucl Med Commun. 25 (5): 445–9. PMID 15100502.
- ↑ Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E (May 2004). "Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours". Nucl Med Commun. 25 (5): 445–9. PMID 15100502.
- ↑ Bora, ManashKumar; Vithiavathi, S (2012). "Primary bronchial carcinoid: A rare differential diagnosis of pulmonary koch in young adult patient". Lung India. 29 (1): 59. doi:10.4103/0970-2113.92366. ISSN 0970-2113.
- ↑ Yazıcıoğlu A, Yekeler E, Bıcakcıoğlu P, Ozaydın E, Karaoğlanoğlu N (December 2012). "Synchronous bilateral multiple typical pulmonary carcinoid tumors: a unique case with 10 typical carcinoids". Balkan Med J. 29 (4): 450–2. doi:10.5152/balkanmedj.2012.081. PMC 4115868. PMID 25207053.
- ↑ Krausz Y, Keidar Z, Kogan I, Even-Sapir E, Bar-Shalom R, Engel A, Rubinstein R, Sachs J, Bocher M, Agranovicz S, Chisin R, Israel O (November 2003). "SPECT/CT hybrid imaging with 111In-pentetreotide in assessment of neuroendocrine tumours". Clin. Endocrinol. (Oxf). 59 (5): 565–73. PMID 14616879.
- ↑ van der Lely, Aart J.; Herder, Wouter W. de (2005). "Carcinoid syndrome: diagnosis and medical management". Arquivos Brasileiros de Endocrinologia & Metabologia. 49 (5): 850–860. doi:10.1590/S0004-27302005000500028. ISSN 0004-2730.
- ↑ Halperin DM, Shen C, Dasari A, Xu Y, Chu Y, Zhou S, Shih YT, Yao JC (April 2017). "Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study". Lancet Oncol. 18 (4): 525–534. doi:10.1016/S1470-2045(17)30110-9. PMC 6066284. PMID 28238592.
- ↑ Sjöblom SM (September 1988). "Clinical presentation and prognosis of gastrointestinal carcinoid tumours". Scand. J. Gastroenterol. 23 (7): 779–87. PMID 3227292.
- ↑ Ganeshan D, Bhosale P, Yang T, Kundra V (October 2013). "Imaging features of carcinoid tumors of the gastrointestinal tract". AJR Am J Roentgenol. 201 (4): 773–86. doi:10.2214/AJR.12.9758. PMID 24059366.
- ↑ Signs and symptoms of carcinoid syndrome. National Cancer Institute. http://www.cancer.gov/types/gi-carcinoid-tumors/patient/gi-carcinoid-treatment-pdq
- ↑ Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD (May 2005). "Current status of gastrointestinal carcinoids". Gastroenterology. 128 (6): 1717–51. PMID 15887161.
- ↑ Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM (July 2008). "Bronchopulmonary neuroendocrine tumors". Cancer. 113 (1): 5–21. doi:10.1002/cncr.23542. PMID 18473355.
- ↑ Jeung, Mi-Young; Gasser, Bernard; Gangi, Afshin; Charneau, Dominique; Ducroq, Xavier; Kessler, Romain; Quoix, Elisabeth; Roy, Catherine (2002). "Bronchial Carcinoid Tumors of the Thorax: Spectrum of Radiologic Findings". RadioGraphics. 22 (2): 351–365. doi:10.1148/radiographics.22.2.g02mr01351. ISSN 0271-5333.
- ↑ Nessi R, Basso Ricci P, Basso Ricci S, Bosco M, Blanc M, Uslenghi C (April 1991). "Bronchial carcinoid tumors: radiologic observations in 49 cases". J Thorac Imaging. 6 (2): 47–53. PMID 1649924.
- ↑ Melmon KL, Sjoerdsma A, Mason DT (October 1965). "Distinctive clinical and therapeutic aspects of the syndrome associated with bronchial carcinoid tumors". Am. J. Med. 39 (4): 568–81. PMID 5831899.
- ↑ Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P (May 2008). "Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior". Am. J. Gastroenterol. 103 (5): 1229–39, quiz 1240. doi:10.1111/j.1572-0241.2007.01740.x. PMID 18371141.
- ↑ Simren M, Palsson OS, Whitehead WE (April 2017). "Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice". Curr Gastroenterol Rep. 19 (4): 15. doi:10.1007/s11894-017-0554-0. PMC 5378729. PMID 28374308.
- ↑ "American Gastroenterological Association medical position statement: irritable bowel syndrome". Gastroenterology. 123 (6): 2105–7. December 2002. doi:10.1053/gast.2002.37095b. PMID 12454865.
- ↑ Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R (February 2016). "Bowel Disorders". Gastroenterology. doi:10.1053/j.gastro.2016.02.031. PMID 27144627.
- ↑ McLaughlin PD, Maher MM (July 2013). "Primary malignant diseases of the small intestine". AJR Am J Roentgenol. 201 (1): W9–14. doi:10.2214/AJR.12.8492. PMID 23789703.
- ↑ Hatzaras I, Palesty JA, Abir F, Sullivan P, Kozol RA, Dudrick SJ, Longo WE (March 2007). "Small-bowel tumors: epidemiologic and clinical characteristics of 1260 cases from the connecticut tumor registry". Arch Surg. 142 (3): 229–35. doi:10.1001/archsurg.142.3.229. PMID 17372046.
- ↑ Lepage C, Bouvier AM, Manfredi S, Dancourt V, Faivre J (December 2006). "Incidence and management of primary malignant small bowel cancers: a well-defined French population study". Am. J. Gastroenterol. 101 (12): 2826–32. doi:10.1111/j.1572-0241.2006.00854.x. PMID 17026561.
- ↑ Hara AK, Swartz PG (2009). "CT enterography of Crohn's disease". Abdom Imaging. 34 (3): 289–95. doi:10.1007/s00261-008-9443-1. PMID 18649092.
- ↑ Baumgart, Daniel C; Sandborn, William J (2012). "Crohn's disease". The Lancet. 380 (9853): 1590–1605. doi:10.1016/S0140-6736(12)60026-9. ISSN 0140-6736.
- ↑ Feuerstein, Joseph D.; Cheifetz, Adam S. (2017). "Crohn Disease: Epidemiology, Diagnosis, and Management". Mayo Clinic Proceedings. 92 (7): 1088–1103. doi:10.1016/j.mayocp.2017.04.010. ISSN 0025-6196.
- ↑ García-Bosch, O.; Ordás, I.; Aceituno, M.; Rodríguez, S.; Ramírez, A. M.; Gallego, M.; Ricart, E.; Rimola, J.; Panes, J. (2016). "Comparison of Diagnostic Accuracy and Impact of Magnetic Resonance Imaging and Colonoscopy for the Management of Crohn's Disease". Journal of Crohn's and Colitis. 10 (6): 663–669. doi:10.1093/ecco-jcc/jjw015. ISSN 1873-9946.
- ↑ Izikson, Leonid; English, Joseph C.; Zirwas, Matthew J. (2006). "The flushing patient: Differential diagnosis, workup, and treatment". Journal of the American Academy of Dermatology. 55 (2): 193–208. doi:10.1016/j.jaad.2005.07.057. ISSN 0190-9622.
- ↑ Hartmann, Karin; Escribano, Luis; Grattan, Clive; Brockow, Knut; Carter, Melody C.; Alvarez-Twose, Ivan; Matito, Almudena; Broesby-Olsen, Sigurd; Siebenhaar, Frank; Lange, Magdalena; Niedoszytko, Marek; Castells, Mariana; Oude Elberink, Joanna N.G.; Bonadonna, Patrizia; Zanotti, Roberta; Hornick, Jason L.; Torrelo, Antonio; Grabbe, Jürgen; Rabenhorst, Anja; Nedoszytko, Boguslaw; Butterfield, Joseph H.; Gotlib, Jason; Reiter, Andreas; Radia, Deepti; Hermine, Olivier; Sotlar, Karl; George, Tracy I.; Kristensen, Thomas K.; Kluin-Nelemans, Hanneke C.; Yavuz, Selim; Hägglund, Hans; Sperr, Wolfgang R.; Schwartz, Lawrence B.; Triggiani, Massimo; Maurer, Marcus; Nilsson, Gunnar; Horny, Hans-Peter; Arock, Michel; Orfao, Alberto; Metcalfe, Dean D.; Akin, Cem; Valent, Peter (2016). "Cutaneous manifestations in patients with mastocytosis: Consensus report of the European Competence Network on Mastocytosis; the American Academy of Allergy, Asthma & Immunology; and the European Academy of Allergology and Clinical Immunology". Journal of Allergy and Clinical Immunology. 137 (1): 35–45. doi:10.1016/j.jaci.2015.08.034. ISSN 0091-6749.
- ↑ Lee, Jason K; Whittaker, Scott J; Enns, Robert A; Zetler, Peter (2008). "Gastrointestinal manifestations of systemic mastocytosis". World Journal of Gastroenterology. 14 (45): 7005. doi:10.3748/wjg.14.7005. ISSN 1007-9327.
- ↑ Horan RF, Austen KF (March 1991). "Systemic mastocytosis: retrospective review of a decade's clinical experience at the Brigham and Women's Hospital". J. Invest. Dermatol. 96 (3): 5S–13S, discussion 13S–14S. PMID 2002264.
- ↑ Sokol, Harry; Georgin-Lavialle, Sophie; Grandpeix-Guyodo, Catherine; Canioni, Danielle; Barete, Stéphane; Dubreuil, Patrice; Lortholary, Olivier; Beaugerie, Laurent; Hermine, Olivier (2010). "Gastrointestinal involvement and manifestations in systemic mastocytosis". Inflammatory Bowel Diseases. 16 (7): 1247–1253. doi:10.1002/ibd.21218. ISSN 1078-0998.
- ↑ Bedeir A, Jukic DM, Wang L, Mullady DK, Regueiro M, Krasinskas AM (November 2006). "Systemic mastocytosis mimicking inflammatory bowel disease: A case report and discussion of gastrointestinal pathology in systemic mastocytosis". Am. J. Surg. Pathol. 30 (11): 1478–82. doi:10.1097/01.pas.0000213310.51553.d7. PMID 17063092.
- ↑ Fuhlbrigge A, Peden D, Apter AJ, Boushey HA, Camargo CA, Gern J, Heymann PW, Martinez FD, Mauger D, Teague WG, Blaisdell C (March 2012). "Asthma outcomes: exacerbations". J. Allergy Clin. Immunol. 129 (3 Suppl): S34–48. doi:10.1016/j.jaci.2011.12.983. PMC 3595577. PMID 22386508.
- ↑ Limb SL, Brown KC, Wood RA, Wise RA, Eggleston PA, Tonascia J, Adkinson NF (December 2005). "Irreversible lung function deficits in young adults with a history of childhood asthma". J. Allergy Clin. Immunol. 116 (6): 1213–9. doi:10.1016/j.jaci.2005.09.024. PMID 16337448.
- ↑ Aldington S, Beasley R (May 2007). "Asthma exacerbations. 5: assessment and management of severe asthma in adults in hospital". Thorax. 62 (5): 447–58. doi:10.1136/thx.2005.045203. PMC 2117186. PMID 17468458.
- ↑ Dougherty RH, Fahy JV (February 2009). "Acute exacerbations of asthma: epidemiology, biology and the exacerbation-prone phenotype". Clin. Exp. Allergy. 39 (2): 193–202. doi:10.1111/j.1365-2222.2008.03157.x. PMC 2730743. PMID 19187331.
- ↑ Peavy RD, Metcalfe DD (August 2008). "Understanding the mechanisms of anaphylaxis". Curr Opin Allergy Clin Immunol. 8 (4): 310–5. doi:10.1097/ACI.0b013e3283036a90. PMC 2683407. PMID 18596587.
- ↑ Tupper J, Visser S (October 2010). "Anaphylaxis: A review and update". Can Fam Physician. 56 (10): 1009–11. PMC 2954079. PMID 20944042.
- ↑ Kemp SF, Lockey RF (September 2002). "Anaphylaxis: a review of causes and mechanisms". J. Allergy Clin. Immunol. 110 (3): 341–8. PMID 12209078.
- ↑ Bjornsson HM, Graffeo CS (December 2010). "Improving diagnostic accuracy of anaphylaxis in the acute care setting". West J Emerg Med. 11 (5): 456–61. PMC 3027438. PMID 21293765.
- ↑ "Usefulness and Limitations of Sequential Serum Tryptase for the Diagnosis of Anaphylaxis in 102 Patients - FullText - International Archives of Allergy and Immunology 2013, Vol. 160, No. 2 - Karger Publishers".
- ↑ Busse PJ, Smith T (August 2017). "Histaminergic Angioedema". Immunol Allergy Clin North Am. 37 (3): 467–481. doi:10.1016/j.iac.2017.03.001. PMID 28687103.
- ↑ Hahn J, Hoffmann TK, Bock B, Nordmann-Kleiner M, Trainotti S, Greve J (July 2017). "Angioedema". Dtsch Arztebl Int. 114 (29–30): 489–496. doi:10.3238/arztebl.2017.0489. PMC 5569554. PMID 28818177.
- ↑ Bernstein JA, Cremonesi P, Hoffmann TK, Hollingsworth J (December 2017). "Angioedema in the emergency department: a practical guide to differential diagnosis and management". Int J Emerg Med. 10 (1): 15. doi:10.1186/s12245-017-0141-z. PMC 5389952. PMID 28405953.
- ↑ Bernstein JA, Moellman J (November 2012). "Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema". Int J Emerg Med. 5 (1): 39. doi:10.1186/1865-1380-5-39. PMC 3518251. PMID 23131076.
- ↑ Kaplan AP (June 2008). "Angioedema". World Allergy Organ J. 1 (6): 103–13. doi:10.1097/WOX.0b013e31817aecbe. PMC 3651192. PMID 23282406.
- ↑ Pacini F, Castagna MG, Cipri C, Schlumberger M (August 2010). "Medullary thyroid carcinoma". Clin Oncol (R Coll Radiol). 22 (6): 475–85. doi:10.1016/j.clon.2010.05.002. PMID 20627492.
- ↑ Roy M, Chen H, Sippel RS (2013). "Current understanding and management of medullary thyroid cancer". Oncologist. 18 (10): 1093–100. doi:10.1634/theoncologist.2013-0053. PMC 3805151. PMID 24037980.
- ↑ Mian C, Perrino M, Colombo C, Cavedon E, Pennelli G, Ferrero S, De Leo S, Sarais C, Cacciatore C, Manfredi GI, Verga U, Iacobone M, De Pasquale L, Pelizzo MR, Vicentini L, Persani L, Fugazzola L (May 2014). "Refining calcium test for the diagnosis of medullary thyroid cancer: cutoffs, procedures, and safety". J. Clin. Endocrinol. Metab. 99 (5): 1656–64. doi:10.1210/jc.2013-4088. PMID 24552221.
- ↑ Bae YJ, Schaab M, Kratzsch J (2015). "Calcitonin as Biomarker for the Medullary Thyroid Carcinoma". Recent Results Cancer Res. 204: 117–37. doi:10.1007/978-3-319-22542-5_5. PMID 26494386.