Chickenpox differential diagnosis: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Chickenpox]] | |||
{{CMG}}; {{AE}} {{MJM}} {{JS}} {{ARK}} | {{CMG}}; {{AE}} {{MJM}} {{JS}} {{ARK}} | ||
| Line 7: | Line 7: | ||
==Differentiating Chickenpox from other Diseases== | ==Differentiating Chickenpox from other Diseases== | ||
Chickenpox must be differentiated from other diseases presenting with diffuse papulovesicular rash in a [[febrile]] patient. The various conditions that should be differentiated from [[chickenpox]] include:<ref name="pmid25250996">{{cite journal| author=Hartman-Adams H, Banvard C, Juckett G| title=Impetigo: diagnosis and treatment. | journal=Am Fam Physician | year= 2014 | volume= 90 | issue= 4 | pages= 229-35 | pmid=25250996 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25250996 }} </ref><ref name="pmid27265069">{{cite journal| author=Mehta N, Chen KK, Kroumpouzos G| title=Skin disease in pregnancy: The approach of the obstetric medicine physician. | journal=Clin Dermatol | year= 2016 | volume= 34 | issue= 3 | pages= 320-6 | pmid=27265069 | doi=10.1016/j.clindermatol.2016.02.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27265069 }} </ref><ref name="MooreSeward2006">{{cite journal|last1=Moore|first1=Zack S|last2=Seward|first2=Jane F|last3=Lane|first3=J Michael|title=Smallpox|journal=The Lancet|volume=367|issue=9508|year=2006|pages=425–435|issn=01406736|doi=10.1016/S0140-6736(06)68143-9}}</ref><ref name="pmid26612370">{{cite journal| author=Ibrahim F, Khan T, Pujalte GG| title=Bacterial Skin Infections. | journal=Prim Care | year= 2015 | volume= 42 | issue= 4 | pages= 485-99 | pmid=26612370 | doi=10.1016/j.pop.2015.08.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26612370 }} </ref><ref name="pmid26566601">{{cite journal| author=Ramoni S, Boneschi V, Cusini M| title=Syphilis as "the great imitator": a case of impetiginoid syphiloderm. | journal=Int J Dermatol | year= 2016 | volume= 55 | issue= 3 | pages= e162-3 | pmid=26566601 | doi=10.1111/ijd.13072 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26566601 }} </ref><ref name="pmid25855021">{{cite journal| author=Kimura U, Yokoyama K, Hiruma M, Kano R, Takamori K, Suga Y| title=Tinea faciei caused by Trichophyton mentagrophytes (molecular type Arthroderma benhamiae ) mimics impetigo : a case report and literature review of cases in Japan. | journal=Med Mycol J | year= 2015 | volume= 56 | issue= 1 | pages= E1-5 | pmid=25855021 | doi=10.3314/mmj.56.E1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25855021 }} </ref><ref name="pmid23176858">{{cite journal| author=CEDEF| title=[Item 87--Mucocutaneous bacterial infections]. | journal=Ann Dermatol Venereol | year= 2012 | volume= 139 | issue= 11 Suppl | pages= A32-9 | pmid=23176858 | doi=10.1016/j.annder.2012.01.002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23176858 }} </ref> | |||
=== Common conditions to be differentiated from chickenpox: === | === Common conditions to be differentiated from chickenpox: === | ||
| Line 67: | Line 67: | ||
=== Less common conditions to be differentiated from chickenpox: === | === Less common conditions to be differentiated from chickenpox: === | ||
{| class="wikitable" | {| class="wikitable" | ||
! style="width: 200px; background: #4479BA; text-align: center;" | {{fontcolor|#FFF|Less Common Diseases}} | ! style="width: 200px; background: #4479BA; text-align: center;" | {{fontcolor|#FFF|Less Common Diseases}} | ||
| Line 195: | Line 196: | ||
=== '''Oral lesions to be differentiated from chicken pox:''' === | === '''Oral lesions to be differentiated from chicken pox:''' === | ||
<small><div style="width: 70%;"> | Oral lesions caused by chickenpox must be differentiated from other diseases presenting with pain and [[Blisters|blistering]] within the mouth ([[gingivostomatitis]] and [[glossitis]]). The differentials include:<small><div style="width: 70%;"> | ||
{| class="wikitable" | {| class="wikitable" | ||
!Disease | !Disease | ||
| Line 215: | Line 216: | ||
*[[Sores]] in the [[mouth]] | *[[Sores]] in the [[mouth]] | ||
*[[Rash]] with [[blisters]] | *[[Rash]] with [[blisters]] | ||
*[[ | *[[Myalgia]] | ||
| | | | ||
*[[Pregnancy]] | *[[Pregnancy]] | ||
| Line 225: | Line 226: | ||
*[[Tzanck test]] | *[[Tzanck test]] | ||
| | | | ||
*[[ | *[[Mucuos membrane]] | ||
*[[Skin]] | *[[Skin]] | ||
| | | | ||
| Line 233: | Line 234: | ||
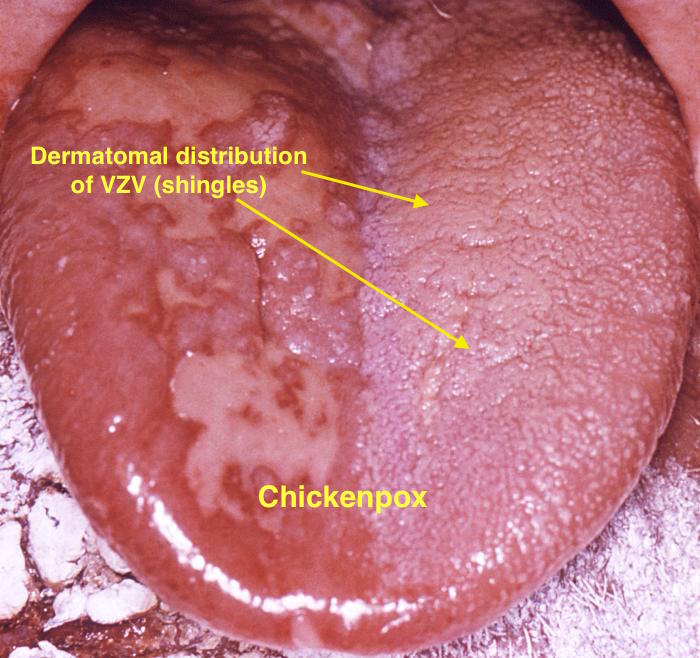
|[[Chickenpox|Chicken pox]] | |[[Chickenpox|Chicken pox]] | ||
| | | | ||
*[[Conjunctival symptoms]] | *Conjunctival symptoms: | ||
*[[ | :*[[Conjunctival injection]] | ||
:*Cloudy cornea | |||
*Catarrhal symptoms: | |||
:*[[Rhinorrhea]] | |||
:*[[Coughing]] | |||
:*[[Sneezing]] | |||
*Characteristic [[spots]] on the trunk appearing in two or three waves | *Characteristic [[spots]] on the trunk appearing in two or three waves | ||
*[[Itching]] | *[[Itching]] | ||
| Line 310: | Line 316: | ||
*Oral Cavity | *Oral Cavity | ||
| | | | ||
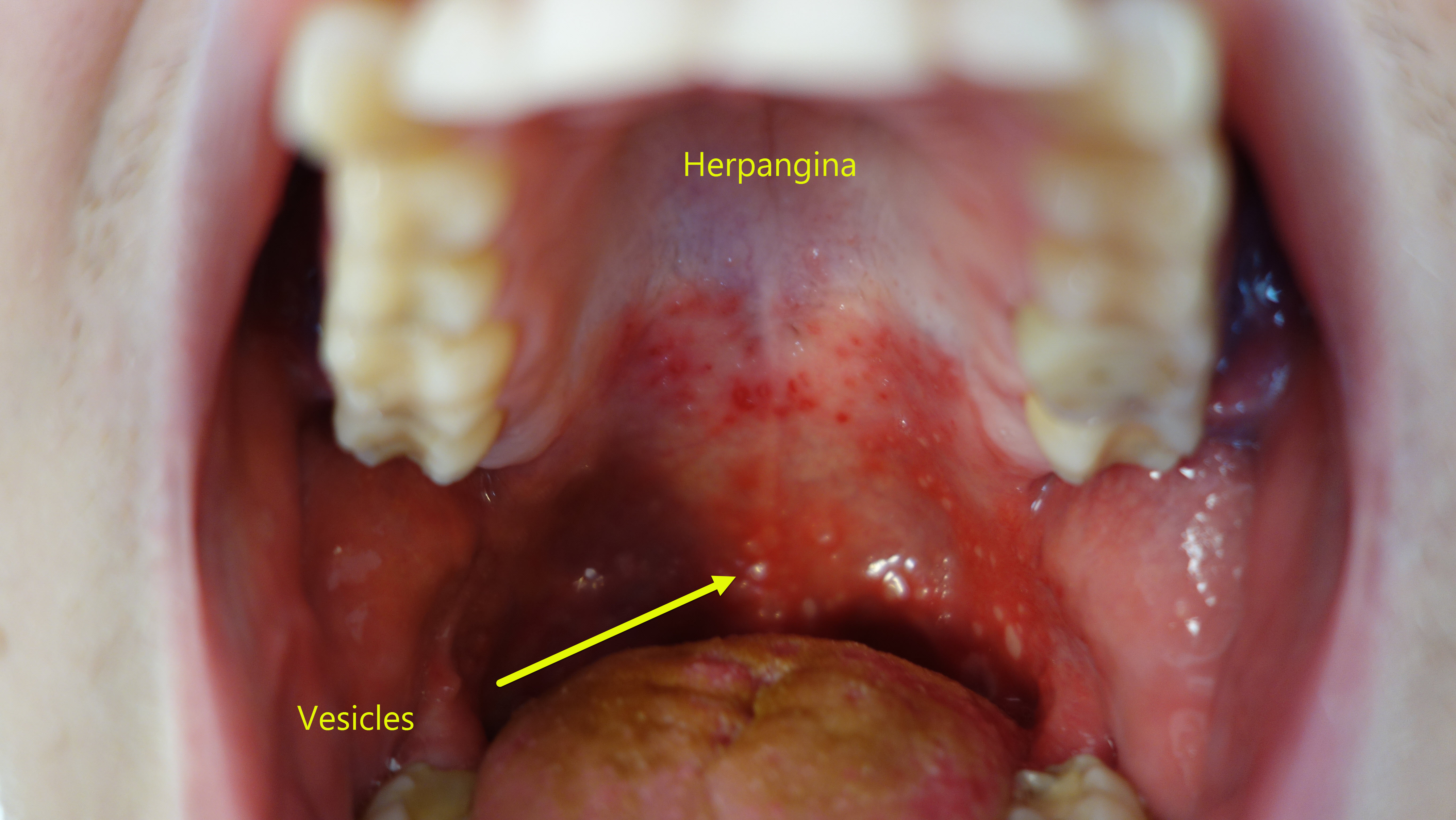
*Characteristic | *Characteristic exanthem- Punctate [[macule]] which evolve over a period of 24 hours to 2-4mm erythematous papules which vesiculate, and then centrally ulcerate. | ||
*The lesions are usually small in number, and evolve rapidly. The lesions are seen more commonly on the [[soft palate]] and [[uvula]]. The lesions can also be seen on the [[tonsils]], posterior pharyngeal wall and the [[buccal mucosa]]. | *The lesions are usually small in number, and evolve rapidly. The lesions are seen more commonly on the [[soft palate]] and [[uvula]]. The lesions can also be seen on the [[tonsils]], posterior pharyngeal wall and the [[buccal mucosa]]. | ||
| | | | ||
[[File:Herpangina3.jpg|center|400x400px|alt=Erythema, vesicles and ulcerating lesions in herpangina|Erythema, vesicles and ulcerating lesions in herpangina]] | [[File:Herpangina3.jpg|center|400x400px|alt=Erythema, vesicles and ulcerating lesions in herpangina|Erythema, vesicles and ulcerating lesions in herpangina]] | ||
|- | |- | ||
|Primary herpetic | |Primary herpetic [[gingivostomatitis]]<ref name="KolokotronisDoumas2006">{{cite journal|last1=Kolokotronis|first1=A.|last2=Doumas|first2=S.|title=Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis|journal=Clinical Microbiology and Infection|volume=12|issue=3|year=2006|pages=202–211|issn=1198743X|doi=10.1111/j.1469-0691.2005.01336.x}}</ref> | ||
| | | | ||
*Pin-head [[vesicles]] rupture to form painful irregular ulcerations covered by yellow-grey membrane | *Pin-head [[vesicles]] rupture to form painful irregular ulcerations covered by yellow-grey membrane | ||
| Line 359: | Line 365: | ||
|} | |} | ||
</div> | </div> | ||
{| class="wikitable" | |||
!Disease | |||
!Presentation | |||
!Risk Factors | |||
!Diagnosis | |||
!Affected Organ Systems | |||
!Important features | |||
!Picture | |||
|- | |||
! colspan="3" |Diseases predominantly affecting the oral cavity | |||
! | |||
! | |||
! | |||
! | |||
|- | |||
|[[Oral candidiasis|Oral Candidiasis]] | |||
| | |||
* [[Dysphagia]] or [[odynophagia]] | |||
* White patches on the mouth and tongue | |||
| | |||
*[[Newborn]] babies | |||
*Denture users | |||
*Poorly controlled [[diabetes]] | |||
*As a side effect of medication, most commonly having taken [[antibiotic]]s. Inhaled [[corticosteroids]] for the treatment of lung conditions (e.g, [[asthma]] or [[COPD]]) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication. | |||
*People with poor [[nutrition]], specifically [[vitamin A]], [[Iron deficiency anemia|iron]] and [[Folate deficiency|folate deficiencies]]. | |||
*People with an [[immune deficiency]] (e.g. as a result of [[AIDS]]/[[HIV]] or [[chemotherapy]] treatment). | |||
*Women undergoing hormonal changes, like [[pregnancy]] or those on [[birth control pills]]. | |||
*[[Organ transplantation]] patients | |||
| | |||
* Clinical diagnosis | |||
* Confirmatory tests rarely needed | |||
|'''Localized candidiasis''' | |||
* [[Oral candidiasis|Oral]] and [[Esophageal candidiasis|esophageal candidasis]] | |||
* [[Candida vulvovaginitis]] | |||
* [[Chronic mucocutaneous candidiasis]] | |||
'''Invasive candidasis''' | |||
* [[Candidiasis|Candidaemia]] | |||
* [[Endocarditis|Candida endocarditis]] | |||
* [[Osteoarthritis|Candida osteoarticular disease]] | |||
| | |||
* [[Osteoarthritis|Oral candidiaisis is]] a benign self limiting disease unless accompanied by [[immunosuppression]]. | |||
|[[File:Human tongue infected with oral candidiasis--By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|thumb|Tongue infected with oral candidiasis - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|400x400px]] | |||
|- | |||
|[[Herpes simplex|Herpes simplex oral lesions]] | |||
| | |||
* [[Fever]] | |||
* [[Sore throat]] | |||
* Painful [[ulcer]]s | |||
| | |||
* Stress | |||
* Recent [[URTI]] | |||
* Female sex | |||
| | |||
* Physical examination | |||
* [[Viral culture]] | |||
* [[Tzanck smear]] | |||
| | |||
* Orofacial Infection | |||
* [[Herpes simplex anogenital infection|Anogenital Infection]] | |||
* [[Herpes simplex ocular infection|Ocular Infection]] | |||
* [[Herpes simplex encephalitis|Herpes Encephalitis]] | |||
* [[Herpes simplex neonatorum|Neonatal Herpes]] | |||
* [[Herpetic whitlow|Herpetic Whitlow]] | |||
* [[Herpes gladiatorum|Herpes Gladiatorum]] | |||
| | |||
* The symptoms of primary [[HSV]] infection generally resolve within two weeks | |||
|[[File:Herpesinfection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|thumb|Oral herpes simplex infection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|400x400px]] | |||
|- | |||
|[[Aphthous ulcer|Aphthous ulcers]] | |||
| | |||
* Painful, red spot or bump that develops into an open [[ulcer]] | |||
| | |||
* Being a female | |||
* Between the ages of 10-40 | |||
* Family history of [[Aphthous ulcer|aphthous ulcers]] | |||
| | |||
* Physical examination | |||
* Diagnosis of exclusion | |||
| | |||
* Oral cavity | |||
| | |||
* Self-limiting , [[Pain]] decreases in 7 to 10 days, with complete healing in 1 to 3 weeks | |||
|[[File:Afta foto - By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358.jpg|thumb|Apthous ulcer on the lower surface of the tongue - By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358|400x400px]] | |||
|- | |||
|[[Squamous cell carcinoma]] | |||
| | |||
*Non healing [[ulcer]], [[nodule]], indurated plaque or mass | |||
*May involve [[skin]], [[lips]], inside the [[mouth]], [[throat]] or [[esophagus]] | |||
| | |||
* Chronic sun or [[Ultraviolet|UV exposure]] | |||
* Fair [[skin]] | |||
* [[Elderly]] age (>45 yrs) | |||
* [[Male sex]] | |||
* [[Smoking]] | |||
| | |||
*[[Physical exam]] | |||
*[[Biopsy]] | |||
| | |||
*[[Oral Cavity]] | |||
**Floor of [[mouth]] | |||
**Lateral [[tongue]] | |||
*[[Throat]] | |||
*[[Esophagus]] | |||
| | |||
*[[Malignant]] | |||
*Can spread to [[TMJ]] | |||
*Some times associated with [[leukoplakia]] | |||
|[[File:PLoS oral cancer.png|thumb|400x400px| |Squamous cell carcinoma - By Luca Pastore, Maria Luisa Fiorella, Raffaele Fiorella, Lorenzo Lo Muzio - http://www.plosmedicine.org/article/showImageLarge.action?uri=info%3Adoi%2F10.1371%2Fjournal.pmed.0050212.g001, CC BY 2.5, https://commons.wikimedia.org/w/index.php?curid=15252632]] | |||
|- | |||
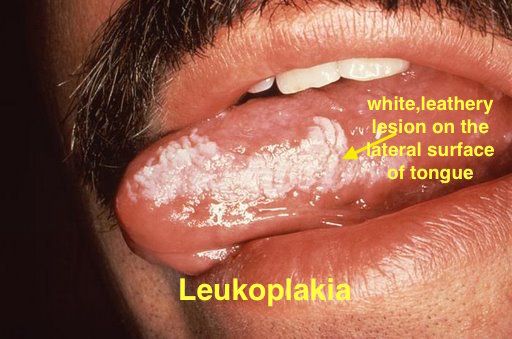
|[[Leukoplakia]] | |||
| | |||
*White leathery spots on the [[mucous membranes]] of the [[tongue]] and inside of the [[mouth]] | |||
*Lateral borders of [[tongue]] | |||
| | |||
*Atypical [[Tobacco]] use | |||
*Chronic [[irritation]] | |||
*[[Immunodeficiency]] | |||
*[[Bloodroot]] ([[Sanguinarine|sanguinaria]]) | |||
| | |||
*[[Physical exam]] | |||
*Diagnosis of exclusion | |||
*[[Biopsy]] | |||
| | |||
*[[Vulva|Vulvar]] lesions occur independent of oral lesions | |||
| | |||
*Associated with [[HIV]] | |||
*Persistant white spots | |||
*[[Benign]] but can progress to [[carcinoma]] after almost 10 years | |||
*Oral proliferative [[Leukoplakia|verrucous leukoplakia]] is an aggressive sub type with multiple lesions and higher conversion to [[warts]] or [[carcinoma]]<ref>{{Cite journal | |||
| author = [[Ann M. Gillenwater]], [[Nadarajah Vigneswaran]], [[Hanadi Fatani]], [[Pierre Saintigny]] & [[Adel K. El-Naggar]] | |||
| title = Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity! | |||
| journal = [[Advances in anatomic pathology]] | |||
| volume = 20 | |||
| issue = 6 | |||
| pages = 416–423 | |||
| year = 2013 | |||
| month = November | |||
| doi = 10.1097/PAP.0b013e3182a92df1 | |||
| pmid = 24113312 | |||
}}</ref> | |||
|[[File:Oral hairy leukoplakia (EBV, in HIV)a.jpg|thumb|400x300px|Leukoplakia - By Aitor III - Own work, Public Domain, https://commons.wikimedia.org/w/index.php?curid=9873087]] | |||
|- | |||
|[[Melanoma]] | |||
| | |||
*A lesion with [[ABCD]] | |||
**[[Asymmetry]] | |||
**Border irregularity | |||
**Color variation | |||
**[[Diamete]]r changes | |||
*[[Bleeding]] from the lesion | |||
| | |||
*[[Ultraviolet|UV radiations]] | |||
*[[Genetic predisposition]] | |||
*[[Old age]] | |||
*[[Male gender]] | |||
*Family or personal history of [[melanoma]] | |||
*Multiple benign or atypical [[Nevus|nevi]] | |||
| | |||
*[[ABCD]] characteristics | |||
*[[Bleeding]] or [[ulceration]] may show [[malignancy]] | |||
*Serum [[LDH]] may be elevated in case of [[malignancy]] | |||
*[[Biopsy]] | |||
| | |||
*Can [[metastasize]] | |||
*All [[UV radiation]] or sun exposed areas can be effected independently | |||
*1-2 to hundreds of [[granules]] | |||
| | |||
*[[Neural crest cell]] derivative | |||
*Development begins with disruption of [[nevus]] growth control | |||
*Progression involves [[MAPK/ERK pathway]] | |||
*[[RAS|N-RAS]] or [[BRAF]] [[oncogene]] also involved | |||
|[[File:Palate malign melanoma 01.jpg|thumb|400x400px|Oral melanoma - By Emmanouil K Symvoulakis, Dionysios E Kyrmizakis, Emmanouil I Drivas, Anastassios V Koutsopoulos, Stylianos G Malandrakis, Charalambos E Skoulakis and John G Bizakis - Symvoulakis et al. Head & Face Medicine 2006 2:7 doi:10.1186/1746-160X-2-7 (Open Access), [1], CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=9839811]] | |||
|- | |||
|[[Fordyce spots]] | |||
| | |||
*Rice-like [[granules]] or [[spots]] | |||
*Small, [[painless]], [[raised]], [[pale]], red or white | |||
*1 to 3 mm in [[diameter]] | |||
| | |||
*Greasy skin types | |||
*Some [[Rheumatic|rheumatic disorders]] | |||
*[[Hereditary nonpolyposis colorectal cancer]] | |||
**Lower [[gingiva]] (gums) | |||
**[[Vestibular system|Vestibular mucosa]] | |||
| | |||
*[[Physical exam]] | |||
*Small [[keratin]]-filled [[pseudocysts]] | |||
*May be seen on [[incidental]] [[mucosal]] [[biopsy]] | |||
**[[Biopsy]] not done for them primarily | |||
| | |||
*[[Oral cavity]] | |||
**[[Vermillion border|Vermilion border]] of the lips | |||
**[[Oral mucosa]] of the upper lip | |||
*[[Buccal mucosa]] in the commissural region often bilaterally | |||
*[[Genitals]] | |||
| | |||
*[[Benign neoplasms]] with [[sebaceous]] features | |||
*Visible [[sebaceous glands]] | |||
*No surrounding [[mucosal]] change | |||
*Several adjacent [[glands]] may coalesce into a larger cauliflower-like cluster | |||
|[[File:Fospot.jpg|thumb|400x400px|Fordyce spots - Por Perene - Obra do próprio, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=19772899]] | |||
|- | |||
|[[Burning mouth syndrome]] | |||
| | |||
*Burning or [[tingling]] on the [[lips]], [[tongue]], or entire [[mouth]] | |||
| | |||
*[[Nutritional deficiencies]] | |||
*Chronic [[anxiety]] or [[depression]] | |||
*[[Diabetes type 2]] | |||
*[[Menopause]] | |||
*[[Oral thrush]] or [[dry mouth]], or damaged [[nerves]] transmitting taste | |||
*[[Female gender ]] | |||
*[[Menopause]] | |||
| | |||
*[[Presentation]] | |||
*[[Physical exam]] | |||
| | |||
*[[Oral cavity]] | |||
| | |||
*Pain typically is low in the morning and builds up over the day | |||
*Low dosages of [[benzodiazepines]], [[tricyclic antidepressants]] or [[anticonvulsants]] may be effective | |||
| | |||
|- | |||
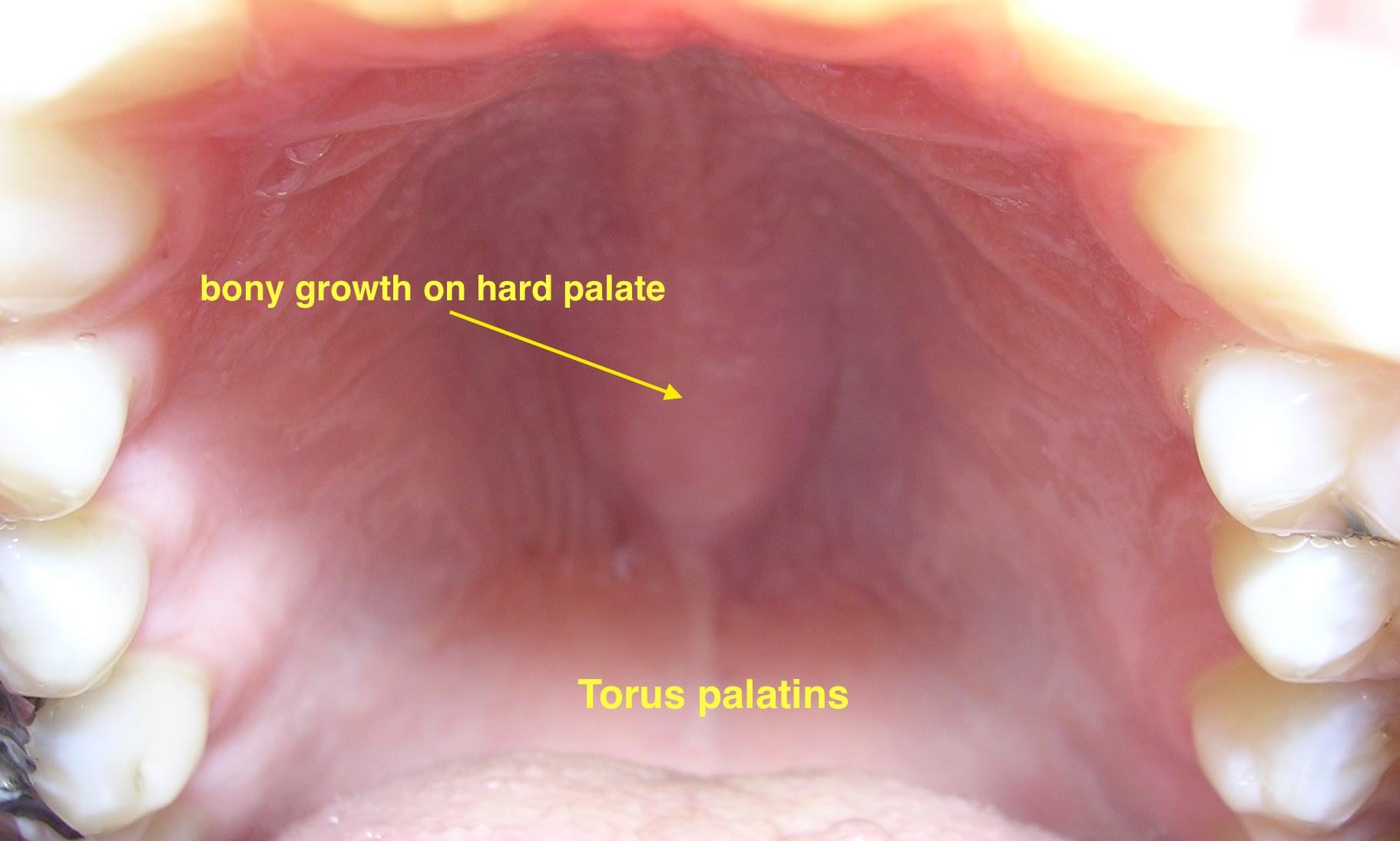
|[[Torus palatinus]] | |||
| | |||
*Bony growth on midline of the [[hard palate]] | |||
*[[Nodular]] mass covered with normal [[mucosa]] | |||
| | |||
*[[Genetic predisposition]] | |||
**[[Autosomal dominant]] | |||
| | |||
*[[Physical exam]] | |||
*Types | |||
**[[Torus palatinus|Flat tori]] | |||
**[[Torus palatinus|Spindle tori]] | |||
**[[Torus palatinus|Nodular tori]] | |||
**[[Torus palatinus|Lobular tori]] | |||
| | |||
*[[Hard palate]] | |||
| | |||
*More common in [[Asian]] and Inuit populations | |||
*Twice more common in [[females]] | |||
*Repeated [[trauma]] can cause [[bleeding]] | |||
*[[Surgery]] may be required in symptomatic | |||
|[[File:06-06-06palataltoria.jpg|thumb|Torus palatinus|400x400px|Torus palatinus - By Photo taken by dozenist, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=846591]] | |||
|- | |||
| colspan="4" |'''Diseases involving oral cavity and other organ systems''' | |||
| | |||
| | |||
| | |||
|- | |||
|[[Behçet's disease|Behcet's disease]] | |||
| | |||
*Painful [[mouth sores]] | |||
*[[Acne]] like skin lesions | |||
*Headache, [[fever]], poor [[balance]], [[disorientation]] | |||
*[[Abdominal pain]], [[diarrhea]] or [[bleeding]] | |||
*[[Uveitis]] | |||
*Joint [[swelling]] and joint [[pain]] | |||
*Genital [[sores]] wit [[pain]] and [[scaring]] | |||
*[[Aneurysms]] | |||
| | |||
*Over active [[immune system]] | |||
| | |||
*[[Physical examination]] | |||
| | |||
*[[Mouth]] | |||
*[[Genitals]] | |||
*[[GIT]] | |||
*[[Eye]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
*[[Vascular system]] | |||
*[[Brain]] | |||
| | |||
*[[Outbreaks]] of exaggerated [[inflammation]] | |||
*Affects smaller [[blood vessels]] | |||
|[[File:Behcets disease.jpg|thumb|400x400px|Behcet's disease - By Ahmet Altiner MD, Rajni Mandal MD - http://dermatology.cdlib.org/1611/articles/18_2009-10-20/2.jpg, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=17863021]] | |||
|- | |||
|[[Crohn's disease]] | |||
| | |||
*Chronic, episodic [[diarrhea]] or [[constipation]] | |||
*[[Abdominal pain]] | |||
*[[Vomiting]] | |||
*[[Weight loss]] or [[weight gain]] | |||
| | |||
*[[Smoking]] | |||
*[[Whites]] and [[European]] [[Jews]] | |||
*[[Hormonal contraception]] | |||
*Diets high in microparticles, sweet, fatty or refined foods | |||
*Industrialized country | |||
| | |||
*Typical [[history]] and [[symptoms]] | |||
*[[Skip lesions]] on [[biopsy]] | |||
*[[Anti saccharomyces cerevisiae antibodies|Anti-Saccharomyces cerevisiae antibodies (ASCA)]] | |||
*[[Anti-neutrophil cytoplasmic antibodies]] ([[ANCA]]) | |||
| | |||
*[[Eyes]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
| | |||
*May lead to | |||
**[[Obstruction]]s | |||
**[[Abscess]]es | |||
**Free [[perforation]] | |||
**[[Hemorrhage]] | |||
| | |||
|- | |||
|[[Agranulocytosis]] | |||
| | |||
*[[Fever]] or [[chills]] | |||
*Frequent [[infections]] | |||
*Unusual [[redness]], [[pain]], or [[swelling]] around a wound | |||
*Mouth [[ulcers]] | |||
*[[Abdominal pain]] | |||
*[[Burning sensation when urinating]] | |||
*[[Sore throat]] | |||
| | |||
*[[Medications]]<ref name="PMID17142169">{{cite journal |author=Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. |title=Idiosyncratic drug-induced agranulocytosis: Update of an old disorder. |journal=Eur J Intern Med. |volume=17|issue=8 |pages=529-35 |year=2006|pmid 17142169|doi=|url=https://www.ncbi.nlm.nih.gov/pubmed/17142169}}</ref> | |||
*[[List of chemotherapeutic agents#Cytotoxic Chemotherapy|Cytotoxic chemotherapy]] | |||
*[[Hematological malignancy|Hematologic malignancies]] | |||
*[[Autoimmune disorders]] | |||
| | |||
*[[Neutropenia]] <100 cells per micro litre | |||
*[[Eosinopenia]] | |||
*[[Basopenia]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[GIT]] | |||
*[[Urinary system]] | |||
*[[Conjunctiva]] | |||
| | |||
*[[Immunocompromised|Immunocompromization]] | |||
*Types | |||
**[[Drug-induced]] | |||
**[[Malignant]] | |||
**[[Autoimmune]] | |||
| | |||
|- | |||
|[[Syphilis]]<ref> title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"</ref> | |||
| | |||
*[[Chancre]] | |||
*Regional [[lymphadenopathy]] | |||
| | |||
*[[Multiple sexual partners]] | |||
*Illicit [[drug use]] | |||
*[[Unprotected sex]] | |||
*[[Homosexual men|Men who have sex with men]] | |||
*Residence in highly prevalent areas | |||
*[[Human Immunodeficiency Virus (HIV)|HIV]] infection | |||
*Presence of other [[STI]]s | |||
*Previous history of [[Sexually transmitted disease|STIs]] | |||
*[[Intravenous drug use]] | |||
| | |||
*[[Darkfield microscope|Darkfield microscopy]] | |||
*Non [[Treponema|treponemal]] tests like [[VDRL]] and [[RPR test]]) | |||
*[[Treponema|Treponemal]] tests[[FTA-ABS|FTA-ABS tests]], (TP-PA) assay, [[Enzyme linked immunosorbent assay (ELISA)|enzyme immunoassays]], and [[Chemiluminescence|chemiluminescence immunoassays]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Penis]] | |||
*[[Cervix]] | |||
*[[Labia]] | |||
*[[Anal canal]] | |||
*[[Rectum ]] | |||
*[[CNS]] | |||
*[[Cardiovascular|CVS]] | |||
| | |||
*[[Primary syphilis]] | |||
**[[Chancre]] | |||
*[[Secondary syphilis]] | |||
**[[Condyloma latum|Condylomata lata]] | |||
*[[Latent syphilis]] | |||
**[[Asymptomatic]] | |||
*[[Tertiary syphilis]] | |||
**[[Gumma|Gummas]] | |||
**[[Neurosyphilis]] | |||
|[[File:Hutchinson teeth congenital syphilis PHIL 2385.rsh.jpg|thumb|400x400px|oral syphilis - By CDC/Susan Lindsley - http://phil.cdc.gov/phil_images/20021114/34/PHIL_2385_lores.jpg, Public Domain, https://commons.wikimedia.org/w/index.php?curid=2134349]] | |||
|- | |||
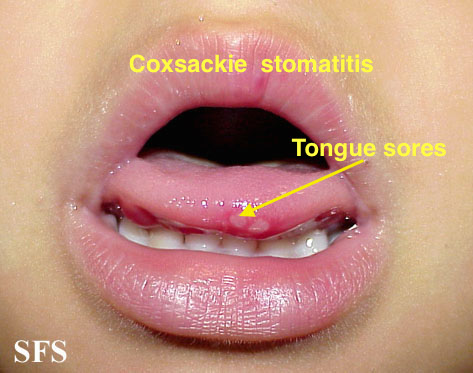
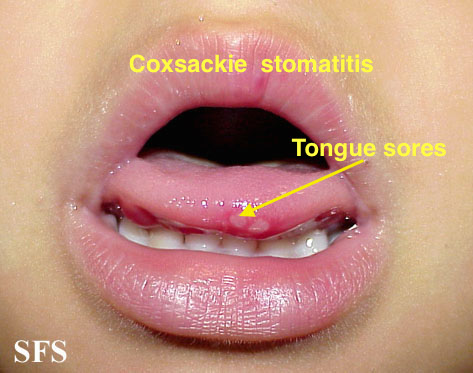
|[[Coxsackie virus]] | |||
| | |||
*[[Fever]] | |||
*[[Sores]] in the [[mouth]] | |||
*[[Rash]] with [[blisters]] | |||
*[[Aches]] | |||
| | |||
*[[Pregnancy]] | |||
*[[immunodeficiency]] | |||
| | |||
*[[History]] and [[Physical exam]] | |||
*[[Swabbing|Throat swabs]] | |||
*Swabs from the lesion | |||
*[[Tzanck test]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*Symptomatic treatment | |||
|[[File:Hand foot mouth disease 07a.jpg|thumb|400x400px|Coxsackie virus stomatitis - Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite web | title = Dermatology Atlas | url = http://www.atlasdermatologico.com.br/}}</ref>]] | |||
|- | |||
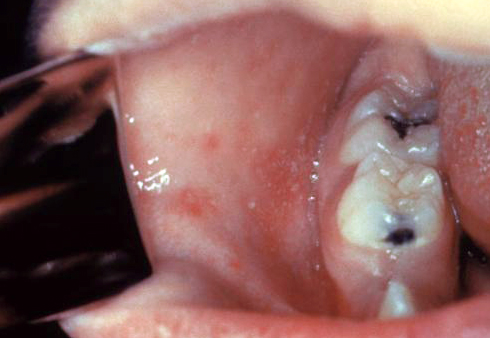
|[[Chickenpox|Chicken pox]] | |||
| | |||
*[[Conjunctival]] symptoms | |||
*[[Catarrhal]] symptoms | |||
*Characteristic [[spots]] on the trunk appearing in two or three waves | |||
*[[Itching]] | |||
| | |||
*[[Pregnancy]] | |||
*[[Premature infants]] born to susceptible mothers | |||
*All [[infants]] born at less than 28 weeks [[gestation]] or who weigh =1000 grams | |||
*[[Immunocompromised]] | |||
| | |||
*[[History]] and [[physical exam]] | |||
*[[PCR]] to detect [[VZV]] in [[skin lesions]] ([[vesicles]], [[scabs]], [[Maculopapular|maculopapular lesions]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*[[Sodium bicarbonate]] in baths or [[antihistamines]] for [[itching]] | |||
*[[Paracetamol]] ([[acetaminophen]]) for [[fever]] | |||
*[[Prednisolone]] is [[contraindicated]] | |||
|[[File:Herpangina2016.jpg|thumb|400x400px|Chickenpox - By James Heilman, MD - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=52872565]] | |||
|- | |||
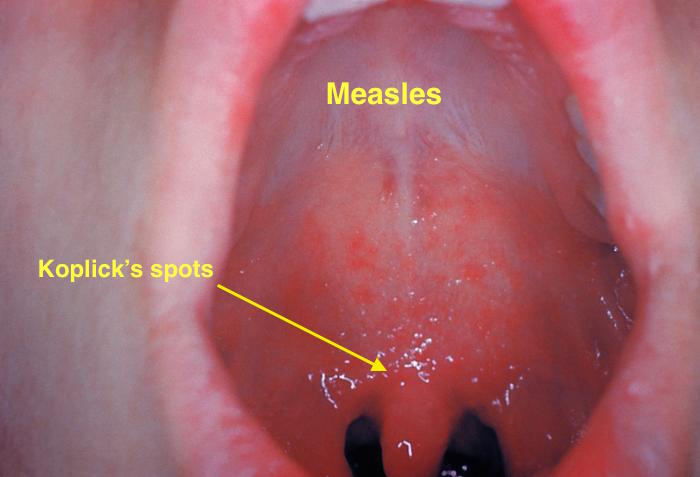
|[[Measles]] | |||
| | |||
*[[Fever]] | |||
*[[Rash]] | |||
*[[Cough]] | |||
*[[Coryza]] (runny nose) | |||
*[[Conjunctivitis]] (pink eye) | |||
*[[Malaise]] | |||
*[[Koplick spots]] in mouth | |||
| | |||
*Unvaccinated individuals<ref name="pmid11135778">{{cite journal| author=Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE| title=Individual and community risks of measles and pertussis associated with personal exemptions to immunization. | journal=JAMA | year= 2000 | volume= 284 | issue= 24 | pages= 3145-50 | pmid=11135778 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11135778 }} </ref><ref name="pmid9009400">{{cite journal| author=Ratnam S, West R, Gadag V, Williams B, Oates E| title=Immunity against measles in school-aged children: implications for measles revaccination strategies. | journal=Can J Public Health | year= 1996 | volume= 87 | issue= 6 | pages= 407-10 | pmid=9009400 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9009400 }} </ref> | |||
*Crowded and/or unsanitary conditions | |||
*Traveling to less developed and developing countries | |||
*Immunocompromized | |||
*Winter and [[spring]] seasons | |||
*Born after 1956 and never fully vaccinated | |||
*Health care workers | |||
| | |||
*[[History]] and [[examination]] | |||
*[[PCR]] for [[Measles]]-specific [[IgM|IgM antibody]] | |||
*[[PCR]] for [[Measles]] [[RNA]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[Respiratory tract]] | |||
*[[Eyes]] | |||
*[[Throat]] | |||
| | |||
*Caused by [[Morbillivirus]] | |||
*Primary site of infection is the [[respiratory epithelium]] of the [[nasopharynx]] | |||
*Transmitted in [[respiratory secretions]], via [[aerosol droplets]] containing [[Virus|virus particles]] | |||
|[[File:Koplik spots, measles 6111 lores.jpg|thumb|400x400px|Koplick spots (Measles) - By CDC - http://phil.cdc.gov/PHIL_Images/20040908/4f54ee8f0e5f49f58aaa30c1bc6413ba/6111_lores.jpg, Public Domain, https://commons.wikimedia.org/w/index.php?curid=824483]] | |||
|} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Dermatology]] | |||
[[Category:Pediatrics]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Infectious disease]] | |||
[[Category:Pulmonology]] | |||
Latest revision as of 20:53, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Michael Maddaleni, B.S. João André Alves Silva, M.D. [2] Aravind Reddy Kothagadi M.B.B.S[3]
Overview
Chickenpox must be differentiated from various rash-causing conditions like Coxsackievirus, Stevens-Johnson syndrome (SJS), measles, rubella, Rocky mountain spotted fever and syphilis.
Differentiating Chickenpox from other Diseases
Chickenpox must be differentiated from other diseases presenting with diffuse papulovesicular rash in a febrile patient. The various conditions that should be differentiated from chickenpox include:[1][2][3][4][5][6][7]
Common conditions to be differentiated from chickenpox:
| Common Conditions | Features |
|---|---|
| Coxsackievirus |
|
| Stevens-Johnson syndrome |
|
| Kawasaki disease |
|
| Measles |
|
| Syphilis | It commonly presents with gneralized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic It is classically described as:
|
| Rubella |
|
| Cytomegalovirus |
|
| Meningococcemia |
|
| Meningitis |
|
| Rocky Mountain spotted fever |
|
| Molluscum contagiosum |
|
| Mononucleosis |
|
Less common conditions to be differentiated from chickenpox:
| Less Common Diseases | Features |
|---|---|
| Atypical measles |
|
| Parvovirus B19 |
|
| Rickettsial pox | |
| Toxic erythema | |
| Monkeypox |
|
| Rat-bite fever | |
| Scarlet fever |
|
Differentiating chickenpox infection in immunocompromised host
Varicella Zoster virus infection is common among immunocompromised patients who are at high risk for other fungal, bacterial, and viral infections. It should be differentiated from the following diseases, which may present as confusion, fever and headache in immunocompromised patients:
| Disease | Differentiating signs and symptoms | Differentiating tests |
|---|---|---|
| CNS lymphoma[8] |
|
|
| Disseminated tuberculosis[9] |
|
|
| Aspergillosis[10] |
|
|
| Cryptococcosis |
|
|
| Chagas disease[11] |
|
|
| CMV infection[12] |
|
|
| HSV infection[13] |
|
|
| Varicella Zoster infection[14] |
|
|
| Brain abscess[15][16] |
|
|
| Progressive multifocal leukoencephalopathy[17] |
|
Oral lesions to be differentiated from chicken pox:
Oral lesions caused by chickenpox must be differentiated from other diseases presenting with pain and blistering within the mouth (gingivostomatitis and glossitis). The differentials include:
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Coxsackie virus |
|
|
| |||
| Chicken pox |
|
|
|
|
| |
| Measles |
|
|
|
|
| |
| Herpangina |
|
|
|
|
|
 |
| Primary herpetic gingivostomatitis[20] |
|
|
|
|
|
|
| Oral Candidiasis |
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[24] |
|
|
|
 | ||
| Coxsackie virus |
|
|
 | |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
References
- ↑ Hartman-Adams H, Banvard C, Juckett G (2014). "Impetigo: diagnosis and treatment". Am Fam Physician. 90 (4): 229–35. PMID 25250996.
- ↑ Mehta N, Chen KK, Kroumpouzos G (2016). "Skin disease in pregnancy: The approach of the obstetric medicine physician". Clin Dermatol. 34 (3): 320–6. doi:10.1016/j.clindermatol.2016.02.003. PMID 27265069.
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Ibrahim F, Khan T, Pujalte GG (2015). "Bacterial Skin Infections". Prim Care. 42 (4): 485–99. doi:10.1016/j.pop.2015.08.001. PMID 26612370.
- ↑ Ramoni S, Boneschi V, Cusini M (2016). "Syphilis as "the great imitator": a case of impetiginoid syphiloderm". Int J Dermatol. 55 (3): e162–3. doi:10.1111/ijd.13072. PMID 26566601.
- ↑ Kimura U, Yokoyama K, Hiruma M, Kano R, Takamori K, Suga Y (2015). "Tinea faciei caused by Trichophyton mentagrophytes (molecular type Arthroderma benhamiae ) mimics impetigo : a case report and literature review of cases in Japan". Med Mycol J. 56 (1): E1–5. doi:10.3314/mmj.56.E1. PMID 25855021.
- ↑ CEDEF (2012). "[Item 87--Mucocutaneous bacterial infections]". Ann Dermatol Venereol. 139 (11 Suppl): A32–9. doi:10.1016/j.annder.2012.01.002. PMID 23176858.
- ↑ Gerstner ER, Batchelor TT (2010). "Primary central nervous system lymphoma". Arch. Neurol. 67 (3): 291–7. doi:10.1001/archneurol.2010.3. PMID 20212226.
- ↑ von Reyn CF, Kimambo S, Mtei L, Arbeit RD, Maro I, Bakari M, Matee M, Lahey T, Adams LV, Black W, Mackenzie T, Lyimo J, Tvaroha S, Waddell R, Kreiswirth B, Horsburgh CR, Pallangyo K (2011). "Disseminated tuberculosis in human immunodeficiency virus infection: ineffective immunity, polyclonal disease and high mortality". Int. J. Tuberc. Lung Dis. 15 (8): 1087–92. doi:10.5588/ijtld.10.0517. PMID 21740673.
- ↑ Latgé JP (1999). "Aspergillus fumigatus and aspergillosis". Clin. Microbiol. Rev. 12 (2): 310–50. PMC 88920. PMID 10194462.
- ↑ Rassi A, Rassi A, Marin-Neto JA (2010). "Chagas disease". Lancet. 375 (9723): 1388–402. doi:10.1016/S0140-6736(10)60061-X. PMID 20399979.
- ↑ Emery VC (2001). "Investigation of CMV disease in immunocompromised patients". J. Clin. Pathol. 54 (2): 84–8. PMC 1731357. PMID 11215290.
- ↑ Bustamante CI, Wade JC (1991). "Herpes simplex virus infection in the immunocompromised cancer patient". J. Clin. Oncol. 9 (10): 1903–15. doi:10.1200/JCO.1991.9.10.1903. PMID 1919640.
- ↑ Hambleton S (2005). "Chickenpox". Curr. Opin. Infect. Dis. 18 (3): 235–40. PMID 15864101.
- ↑ Alvis Miranda H, Castellar-Leones SM, Elzain MA, Moscote-Salazar LR (2013). "Brain abscess: Current management". J Neurosci Rural Pract. 4 (Suppl 1): S67–81. doi:10.4103/0976-3147.116472. PMC 3808066. PMID 24174804.
- ↑ Patel K, Clifford DB (2014). "Bacterial brain abscess". Neurohospitalist. 4 (4): 196–204. doi:10.1177/1941874414540684. PMC 4212419. PMID 25360205.
- ↑ Tan CS, Koralnik IJ (2010). "Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis". Lancet Neurol. 9 (4): 425–37. doi:10.1016/S1474-4422(10)70040-5. PMC 2880524. PMID 20298966.
- ↑ 18.0 18.1 Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ 19.0 19.1 Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Kolokotronis, A.; Doumas, S. (2006). "Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis". Clinical Microbiology and Infection. 12 (3): 202–211. doi:10.1111/j.1469-0691.2005.01336.x. ISSN 1198-743X.
- ↑ Chauvin PJ, Ajar AH (2002). "Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management". J Can Dent Assoc. 68 (4): 247–51. PMID 12626280.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ "Dermatology Atlas".
