Vasculitis
| Vasculitis | |
 | |
|---|---|
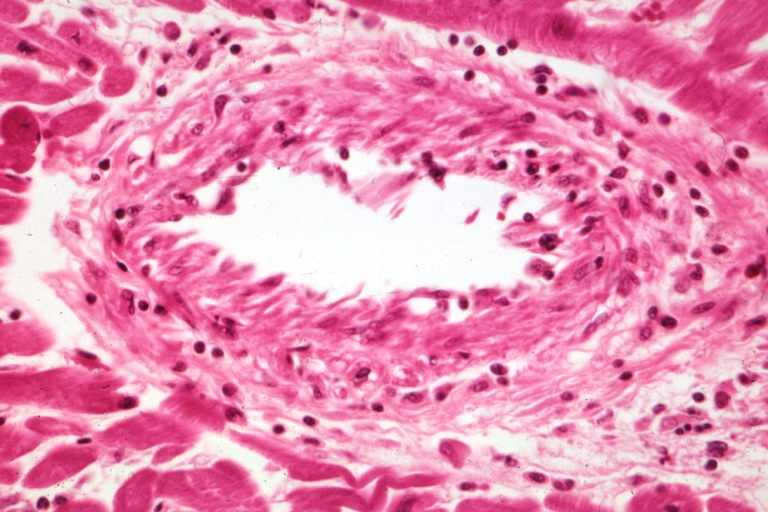
| Kidney: Transplant: Micro H&E high mag excellent example acute vasculitis due to rejection Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-9 | 447.6 |
| DiseasesDB | 13750 |
| MeSH | D014657 |
|
WikiDoc Resources for Vasculitis |
|
Articles |
|---|
|
Most recent articles on Vasculitis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Vasculitis at Clinical Trials.gov Clinical Trials on Vasculitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Vasculitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Vasculitis Discussion groups on Vasculitis Patient Handouts on Vasculitis Directions to Hospitals Treating Vasculitis Risk calculators and risk factors for Vasculitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Vasculitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Vasculitis (plural: vasculitides), a group of diseases featuring inflammation of the wall of blood vessels including veins (phlebitis), arteries (arteritis) and capillaries due to leukocyte migration and resultant damage. While most vasculitides are rare, they generally affect several organ systems and can cause severe disability.
Classification
Vasculitides can be classified by the size of the blood vessel that they predominantly affect.[1]
Large vessel vasculitis
Takayasu arteritis. Primarily affects the aorta and its main branches. At least 3 out of 6 criteria yields sensitivity and specificity of 90.5 and 97.8%:
- onset < 40 years
- claudication of extremities
- decreased pulsation of one or both brachial arteries
- at least 10 mmHg systolic difference in both arms
- bruit over one or both carotid arteries or abdominal aorta
- arteriographic narrowing of aorta, its primary branches, or large arteries in upper or lower extremities
Giant cell (temporal) arteritis. Chronic vasculitis of both large and medium vessels, primarily affecting cranial branches of the arteries arising from the aortic arch. At least 3 out of 5 criteria yields sensitivity and specificity of 95 and 91%:
- Age at onset ≥ 50 years
- New onset headache with localized tenderness
- Temporal artery tenderness or decreased pulsation
- Elevated ESR ≥ 50 mm/hour Westergren
- Temporal artery biopsy showing vasculitis with mononuclear cell infiltrate or granulomatous inflammation, usually with multinucleated giant cells
Medium vessel vasculitis
Polyarteritis nodosa. Systemic necrotizing vasculitis and aneurysm formation affecting both medium and small arteries. If only small vessels are affected, it is called microscopic polyangiitis, although it is more associated with Wegener's granulomatosis than to classic PAN. At least 3 out of 10 criteria yields sensitivity and specificity of 82 and 87%:
- unexplained weight loss > 4 kg
- livedo reticularis
- testicular pain
- myalgias, weakness
- mononeuropathy or polyneuropathy
- new onset diastolic blood pressure > 90 mmHg
- elevated serum BUN (> 40 mg/dL) or serum creatinine (> 1.5 mg/dL)
- hepatitis B infection
- arteriographic abnormalities
- arterial biopsy showing polymorphonuclear cells
Wegener's granulomatosis. Systemic vasculitis of medium and small arteries, including venules and arterioles. Produces granulomatous inflammation of the respiratory tracts and necrotizing, pauci-immune glomerulonephritis. Most common cause of saddle nose deformity in USA (nose flattened due to destruction of nasal septum by granulomatous inflammation). Almost all patients with WG has c-ANCA, but not vice versa. Current treatment of choice is cyclophosphamide. At least 2 out of 4 criteria yields sensitivity and specificity of 88 and 92%.
- nasal or oral inflammation (oral ulcers or purulent/bloody nasal discharge, may be painful)
- abnormal CXR showing nodules, infiltrates, cavities
- microscopic hematuria or RBC casts
- vessel biopsy shows granulomatous inflammation
Kawasaki disease. Usually in children, it affects large, medium, and small vessels, prominently the coronary arteries. Associated with a mucocutaneous lymph node syndrome. Diagnosis requires fever lasting five days or more with at least 4 out of 5 criteria:
- bilateral conjunctival injection
- injected or fissured lips, injected pharynx, or strawberry tongue
- erythema of palms/soles, edema of hands/feet, periungual desquamation
- polymorphous rash
- cervical lymphadenopathy (at least one node > 1.5 cm)
Isolated CNS vasculitis. Affects medium and small arteries over a diffuse CNS area, without symptomatic extracranial vessel involvement. Patients have CNS symptoms as well as cerebral vasculitis by angiography and leptomeningeal biopsy.
Small vessel vasculitis
There are several vasculitides that affect small vessels.[2]
Churg-Strauss arteritis. Affects medium and small vessels with vascular and extravascular granulomatosis. Classically involves arteries of lungs and skin, but may be generalized. At least 4 criteria yields sensitivity and specificity of 85 and 99.7%.
- Asthma (history of wheezeing or presently wheezing)
- Eosinophilia > 10% on CBC
- Mononeuropathy or polyneuropathy
- Migratory or transient pulmonary opacities on CXR
- Paranasal sinus abnormalities
- Vessel biopsy showing eosinophils in extravascular areas
Microscopic polyarteritis/polyangiitis. Affects capillaries, venules, or arterioles. Thought to be part of a group that includes Wegeners since both are associated with ANCA and similar extrapulmonary manifestations. Patients do not usually have symptomatic or histologic respiratory involvement.
Hypersensitivity vasculitis. Usually due to a hypersensitivity reaction to a known drug. There is presence of skin vaculitis with palpable petechiae or purpura. Biopsy of these lesions reveal inflammation of the small vessels, termed leukocytoclastic vasculitis, which is most prominent in postcapillary venules. At least 3 out of 5 criteria yields sensitivity and specificity of 71 and 84%:
- Age > 16
- Use of possible triggering drug in relation to symptoms
- Palpable purpura
- Maculopapular rash
- Skin biopsy showing neutrophils around vessel
Henoch-Schonlein purpura. Systemic vasculitis due to tissue deposition of IgA-containing immune complexes. Biopsy of lesions shows inflammation of small vessels. It is considered a form of hypersensitivity vasculitis but is distinguished by prominent deposits of IgA. This is the most common vasculitis in children. Presence of 3 or more criteria yielded sensitivity of 87% while less than 2 criteria yielded hypersensitivity vasculitis in 74%:
- Palpable purpura (usually of buttocks & legs)
- Mesenteric ishemia
- GI bleed
- Hematuria
- Onset < 20 years
- No new medications
Essential cryoglobulinemic vasculitis. Most often due to hepatitic C infection, immune complexes of cryoglobulins --- proteins that consists of immunoglobulins and complement and precipitate in the cold while dissolving upon rewarming --- are deposited in walls of capillaries, venules, or arterioles. Therefore, complement will be low with histology showing vessel inflammation with immune deposits.
Vasculitis secondary to connective tissue disorders. Usually secondary to systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), relapsing polychondritis, Behcet's disease, and other connective tissue disorders.
Vasculitis secondary to viral infection. Usually due to hepatitis B and C, HIV, cytomegalovirus, Epstein-Barr virus, and Parvo B19 virus.
Symptoms and signs
Patients usually present with systemic symptoms with single or multiorgan dysfunction. Common (and nonspecific) complaints include fatigue, weakness, fever, arthralgias, abdominal pain, hypertension, renal insufficiency, and neurologic dysfunction. The following symptoms should raise a strong suspicion of a vasculitis:
- Mononeuritis multiplex. Also known as asymmetric polyneuropathy is highly suggestive of vasculitis, since diabetes is the only other cause of this.
- Palpable purpura. If patients have this in isolation, it is most likely due to cutaneous leukocytoclastic vasculitis. If the purpura is in combination with systemic organ involvement, it is most likely to be Henoch-Schonlein purpura or microscopic polyarteritis.
- Pulmonary-Renal. Patients with hemoptysis and renal involvement are likely to have Wegener's granulomatosis, microscopic polyangiitis, or anti-GBM disease (Goodpasture's syndrome).
Diagnosis
A detailed history is important to elicit any recent medications, any risk of hepatitis infection, or any recent diagnosis with a connective tissue disorder such as systemic lupus erythematosus (SLE). A thorough physical exam is needed as usual.
- Lab tests. Basic lab tests may include a CBC, chem-7 (look for creatinine), muscle enzyme, liver function tests, ESR, hepatitis seroloties, urinalysis, CXR, and EKG. Additional, more specific tests include:
- Antinuclear antibody (ANA) test can detect an underlying connective tissue disorder, especially SLE
- Complement levels that are low can suggest mixed cryoglobulinemia, hepatitis C infection, and SLE, but not most other vasculitides.
- Antineutrophil cytoplasmic antibody (ANCA) may highly suggest Wegener's granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome, or drug-induced vasculitis, but is not diagnostic.
- Electromyography. It is useful if a systemic vasculitis is suspected and neuromuscular symptoms are present.
- Arteriography. Arteriograms are helpful in vasculitis affecting the large and medium vessels but not helpful in small vessel vasculitis. Angiograms of mesenteri or renal arteries in polyarteritis nodosa may show aneurysms, occlusions, and vascular wall abnormalities. Arteriography are not diagnostic in itself if other accessible areas for biopsy are present. However, in Takayasu's arteritis, where the aorta may be involved, it is unlikely a biopsy will be successful and angiography can be diagnostic.
- Tissue biopsy. This is the gold standard of diagnosis when biopsy is taken from the most involved area.
Pathological Findings
-
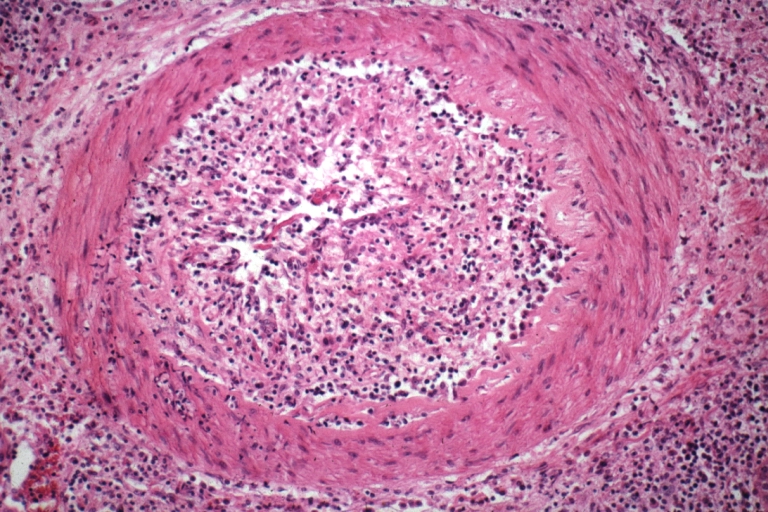
Kidney: Transplant: Micro H&E high mag excellent example acute vasculitis due to rejection
-
Coronary artery: Transplant Rejection: Micro high mag H&E small muscular artery vasculitis
-
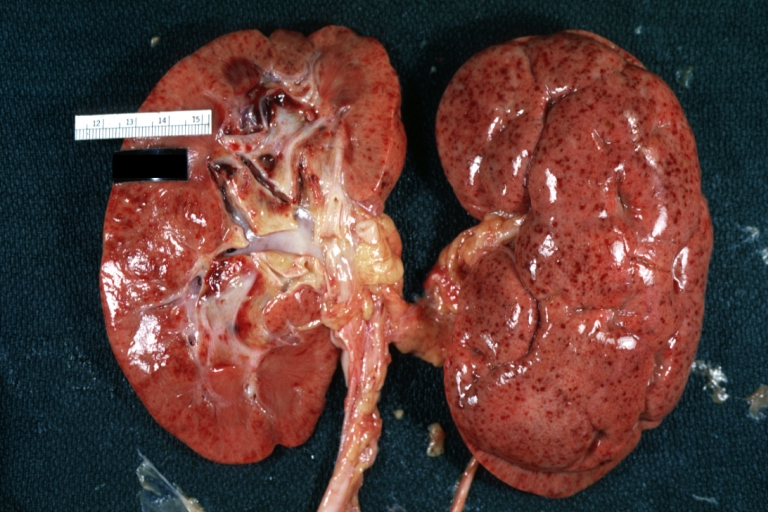
Kidney: Petechiae: Gross natural color, an excellent example of flea bitten kidney case had necrotizing vasculitis
-
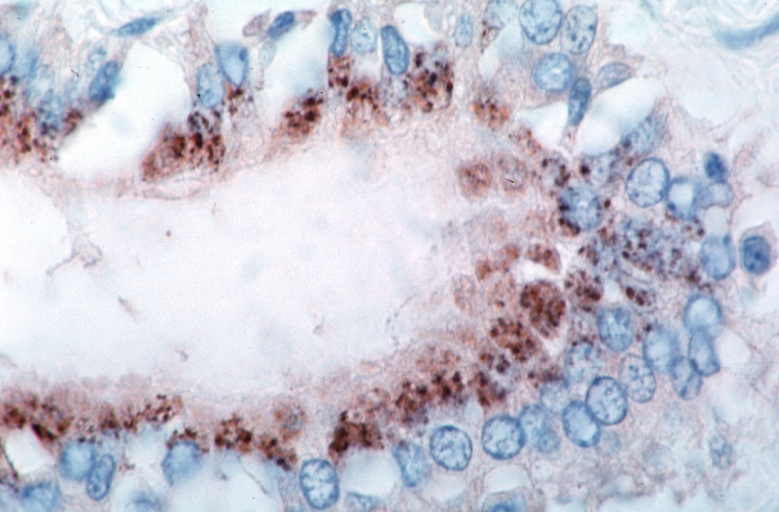
Vasculitis, Rocky Mountain Spotted Fever, immunoperoxidase staining vessels for Rickettsia rickettsii
-
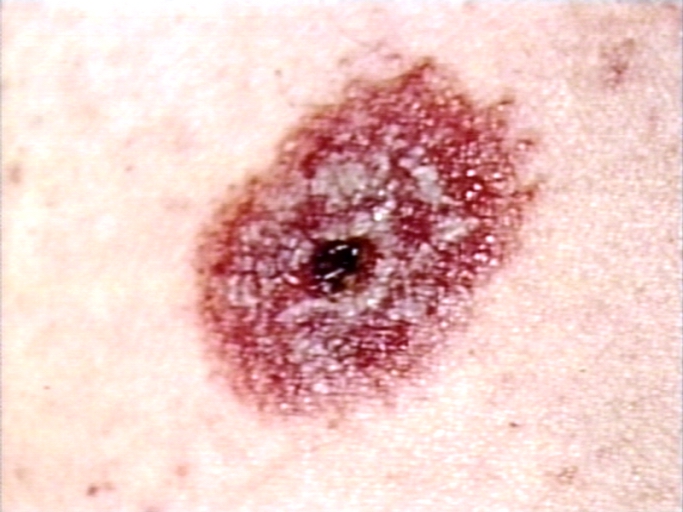
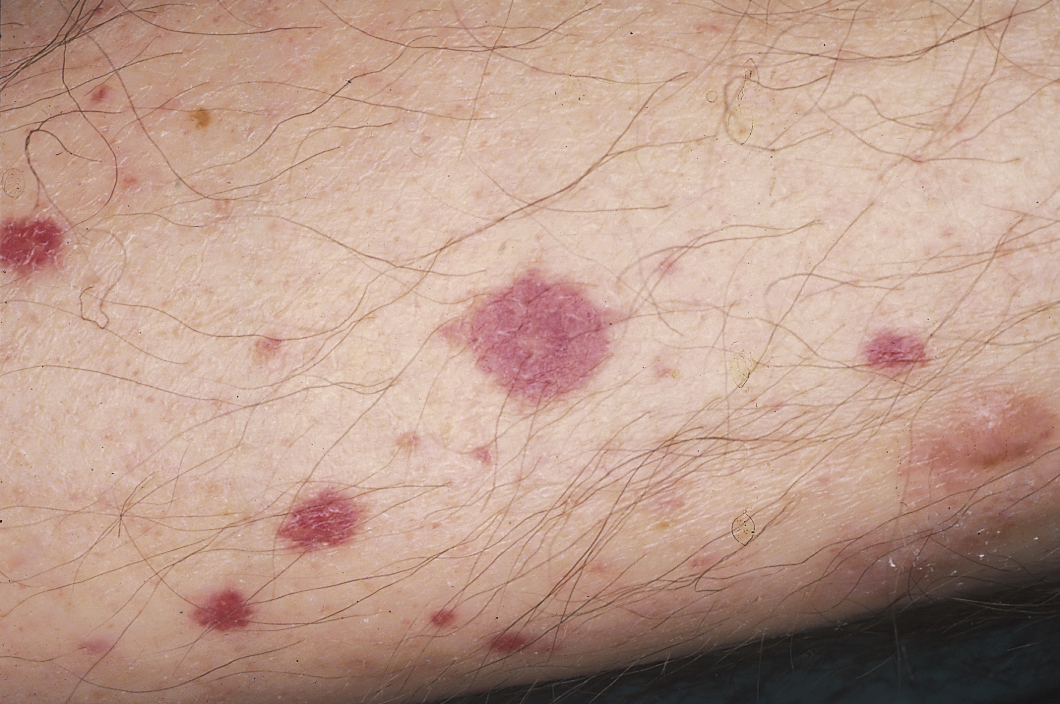
Skin:Leucocytolastic vasculitis; a close up view
-
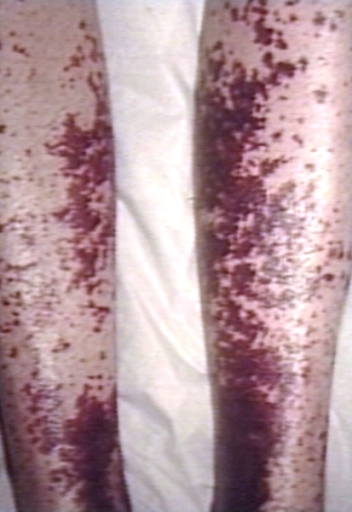
Skin:Leucocytolastic vasculitis; legs
-
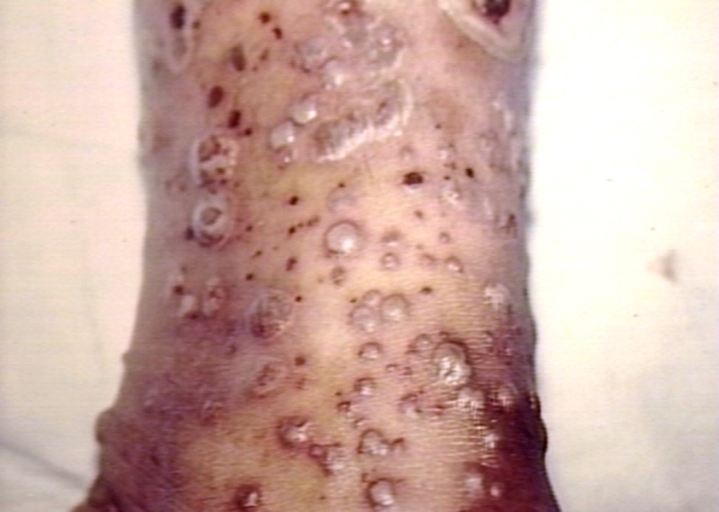
Leucocytoclastic vasculitis; pustular type
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Vasculitis: In this instance, the vasculitic skin lesions were secondary to Haemophilus endocarditis.
-
Vasculitis: In this instance, the vasculitic skin lesions were secondary to Haemophilus endocarditis.
-
Vasculitis: In this instance, idiopathic with palpable purpura.
-
Vasculitis: Palpable Purpura: Secondary to idiopathic leukocytoplastic vasculitis.
-
Vasculitis: In this instance, idiopathic.
-
Vasculitis: In this instance, idiopathic with palpable purpura.
Complete Differential Diagnosis for Vasculitis
Large-sized vessel
Medium-sized vessel
Small-sized vessel
- Churg-Strauss Syndrome
- Cutaneous leukocytoclastic vasculitis
- Essential cryoglobulinemic vasculitis
- Henoch-Schonlein Purpura
- Microscopic polyangiitis
- Wegener's Granulomatosis
Treatment
Treatment is targeted to the underlying cause. However, most vasculitis in general are treated with steroids (e.g. methylprednisolone) because the underlying cause of the vasculitis is due to hyperactive immunological damage. Immunosuppressants such as cyclophosphamide and azathioprine may also be given.
A systematic review of antineutrophil cytoplasmic antibody (ANCA) positive vasculitis indentified best treatments depending on whether the goal is to induce remission or maintenance and depending on severity of the vasculitis.[5]
References
- ↑ Jennette JC, Falk RJ, Andrassy K; et al. (1994). "Nomenclature of systemic vasculitides. Proposal of an international consensus conference". Arthritis Rheum. 37 (2): 187–92. PMID 8129773.
- ↑ Jennette JC, Falk RJ (1997). "Small-vessel vasculitis". N. Engl. J. Med. 337 (21): 1512–23. PMID 9366584.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Bosch X, Guilabert A, Espinosa G, Mirapeix E (2007). "Treatment of antineutrophil cytoplasmic antibody associated vasculitis: a systematic review". JAMA. 298 (6): 655–69. doi:10.1001/jama.298.6.655. PMID 17684188.
External links
- Mayo Clinic on vasculitis.
- European Vasculitis Study Group
- Johns Hopkins Vasculitis Center
- Vasculitis Foundation
Template:Vascular diseases Template:Systemic connective tissue disorders Template:Inflammation
de:Vaskulitis nl:Vasculitis no:Vaskulitt fi:Vaskuliitti sv:Kärlinflammation