|
|
| (11 intermediate revisions by 5 users not shown) |
| Line 5: |
Line 5: |
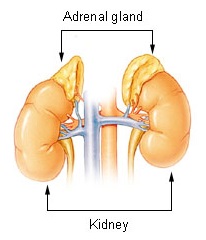
| | Caption = Adrenal gland | | | Caption = Adrenal gland |
| }} | | }} |
| {{Adrenal insufficiency}} | | {{Secondary adrenal insufficiency}} |
|
| |
|
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
|
| {{CMG}} | | {{CMG}} {{AE}} {{ADS}} |
|
| |
|
| {{SK}} hypocortisolism; hypocorticism; adrenocortical hypofunction | | {{SK}} hypocortisolism; hypocorticism; adrenocortical hypofunction |
|
| |
|
| ==[[Adrenal insufficiency overview|Overview]]== | | ==[[Secondary adrenal insufficiency overview|Overview]]== |
|
| |
|
| ==[[Adrenal insufficiency historical perspective|Historical Perspective]]== | | ==[[Secondary adrenal insufficiency historical perspective|Historical Perspective]]== |
|
| |
|
| Primary adrenal insufficiency was first described in 1849 by Thomas Addison, demonstrating that the adrenal cortex is essential for life. On Thursday, March 15, 1849 almost a century ago, President John Hilton requested that, Dr. Addison, describe his latest medical findings before the South London Medical Society. These were Dr. Addison’s introductory comments, "A remarkable form of anemia, which, although incidentally noticed by various writers, had not attracted, as he thought, by any means the attention it really deserved…It was a state of general anemia incident to adult males, and had for several years past been with him a subject of earnest inquiry and of deep interest. It usually occurs between the ages of 20 and 60; sometimes proceeding to an extreme degree in a few weeks, but more frequently commencing insidiously, and proceeding very slowly, so as to occupy a period of several weeks, or even months, before any very serious alarm is taken either by the patient or by the patient's friends. Its approach is first indicated by a certain amount of languor and restlessness, to which presently succeed a manifest paleness of the countenance, loss of muscular strength, general relaxation or feebleness of the whole frame, and indisposition to, or incapacity for, bodily or mental exertion. These symptoms go on increasing with greater or less rapidity: the face, lips, conjunctive, and external surface of the body, become more and more bloodless; the tongue appears pale and flabby; the heart's action gets exceedingly enfeebled, with a weak, soft, unusually large, but always strikingly compressible pulse; the appetite may or may not be lost; the patient experiences a distressing and increasing sense of helplessness and faintness; the heart is excited, or rendered tumultuous in its action, the breathing painfully hurried by the slightest exertion, whilst the whole surface bears some resemblance to a bad wax figure: the patient is no longer able to rise from his bed; slight edema perhaps shows itself about the ankles; the feeling of faintness and weakness becomes extreme, and he dies either from sheer exhaustion, or death is preceded by signs of passive effusion or cerebral compression.” [1]
| | ==[[Secondary adrenal insufficiency classification|Classification]]== |
|
| |
|
| ==[[Adrenal insufficiency classification|Classification]]== | | ==[[Secondary adrenal insufficiency pathophysiology|Pathophysiology]]== |
|
| |
|
| Three major types:
| | ==[[Secondary adrenal insufficiency causes|Causes]]== |
| *'''Primary adrenal insufficiency'''
| |
|
| |
|
| It is due to impairment of the adrenal glands.
| | ==[[Differentiating Secondary adrenal insufficiency from other diseases|Differentiating Adrenal Insufficiency from other Diseases]]== |
| 80% are due to an autoimmune disease called Addison's disease or autoimmune adrenalitis.
| |
| One subtype is called idiopathic, meaning of unknown cause.
| |
| Other cases are due to congenital adrenal hyperplasia or an adenoma (tumor) of the adrenal gland.
| |
|
| |
|
| *'''Secondary adrenal insufficiency'''
| | ==[[Secondary adrenal insufficiency epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| caused by impairment of the pituitary gland or hypothalamus.[2] Its principal causes include pituitary adenoma (which can suppress production of adrenocorticotropic hormone (ACTH) and lead to adrenal deficiency unless the endogenous hormones are replaced); and Sheehan's syndrome, which is associated with impairment of only the pituitary gland.
| | ==[[Secondary adrenal insufficiency risk factors|Risk Factors]]== |
|
| |
|
| *'''Tertiary adrenal insufficiency'''
| | ==[[Secondary adrenal insufficiency natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| | |
| due to hypothalamic disease and a decrease in the release of corticotropin releasing hormone (CRH).[3] Causes can include brain tumors and sudden withdrawal from long-term exogenous steroid use (which is the most common cause).[4]
| |
| | |
| ==[[Adrenal insufficiency pathophysiology|Pathophysiology]]==
| |
| | |
| ==[[Adrenal insufficiency causes|Causes]]==
| |
| | |
| ==[[Differentiating Adrenal insufficiency from other diseases|Differentiating Adrenal Insufficiency from other Diseases]]==
| |
| | |
| Adrenal insufficiency can be difficult to diagnose in its initial stages. Medical history and symptoms is the cornerstone of diagnosis for the physician and confirmation through hormonal blood tests and urine tests further support preliminary diagnosis.
| |
| The steps for the diagnosis of adrenal insufficiency allow the health care provider to distinguish between it and other diseases, therefore the steps of diagnosis are critical. Firstly, cortisol levels are determined followed by the establishment of the cause. In order to determine the cause imaging studies of the adrenal and pituitary glands are used. [2] [3]
| |
| Adrenal insufficiency (Addison disease) may be difficult to differentiate from other conditions if the onset is gradual e.g. chronic fatigue syndrome and depression). [4][5]
| |
| Physicians should consider in their differential diagnosis of adrenal insufficiency patients with suggestive symptoms, such as chronic fatigue, anorexia, nausea, vomiting, diarrhea, unexplained weight loss, dehydration, hypoglycemia, and hypotension. Physicians caring for patients with other known autoimmune disorders should consider these relevant diagnoses. Other conditions that must be considered include adrenocorticotropic hormone (ACTH) receptor defect, adrenoleukodystrophy and adrenomyeloneuropathy, autoimmune polyglandular endocrinopathy syndromes, infectious adrenalitis e.g. in association with human immunodeficiency [HIV] virus or tuberculosis (TB), adrenal hemorrhage, lipoid adrenal hyperplasia and Wolman disease.
| |
| Antiphospholipid syndrome occasionally results in acute adrenal insufficiency secondary to bilateral adrenal hemorrhage. [6]
| |
| | |
| Differential Diagnoses:
| |
| | |
| • 3-Beta-Hydroxysteroid Dehydrogenase Deficiency
| |
| • Adrenal Hypoplasia
| |
| • Birth Trauma
| |
| • Chronic Fatigue Syndrome (CFS)
| |
| • Congenital Adrenal Hyperplasia
| |
| • Familial Glucocorticoid Deficiency
| |
| • Pediatric Hypopituitarism
| |
| • Pseudohypoaldosteronism
| |
| | |
| ==[[Adrenal insufficiency epidemiology and demographics|Epidemiology and Demographics]]==
| |
| | |
| In the United States, the prevalence of Addison’s disease per 1 million population is around 40-60 cases. Internationally, the occurrence of adrenal insufficiency is rare. In countries were epidemiological data is collected, the prevalence changes to 39 cases per 1 million population in the UK, 60 cases per 1 million population in Denmark. In Iceland, a study was conducted by Olafsson and Sigurjonsdottir that found a higher prevalence in this region, around 22.1 per 100,000 population. [7]
| |
| Morbidity and mortality associated with Addison disease are usually due to an inability to determine a diagnosis or a delay in diagnosing a patient with adrenal insufficiency or a failure to provide the patient with the adequate hormonal replacement therapy they need i.e. glucorticoid and mineralocorticoid replacement. [8]
| |
| Death may occur if acute addisonian crisis occurs without being promptly treated. This serious complication may occur as a new event (de novo) occurring in the presence of an adrenal haemorrhage or acutely on top of an inadequately treated adrenocortical insufficiency or a chronic case of insufficiency.
| |
| With insidious chronic Addison disease debilitating symptoms may occur albeit low level and nonspecific.
| |
| Despite diagnosis and adequate management, the risk of death in a patient with Addison disease is two times more likely, usually due to cardiovascular, malignant and infectious disease. [9]
| |
| | |
| The prevalence and risk factors for patients with Addison disease were analysed using surveys by the authors White and Arlt. The following countries were included; United Kingdom, Canada, Australia, and New Zealand. The surveys found that about 8% of those that were diagnosed with Addison’s disease were hospitalized annually for adrenal crisis. Furthermore the authors White and Arlt, found that patients suffering from Asthma, Diabetes Mellitus or had previously a GIT infection had an increased risk of getting Addison disease. [10][11]
| |
| Moreover, a study by Chantzichristos et al indicated that patients who had type 1 or 2 diabetes, were likely to have higher mortality rates if they had Addison disease concomitantly over those that had diabetes alone. These same patients were followed up for almost 6 years and were found to have a mortality rate of 28% vs. 10% for those with diabetes and Addison vs. diabetes alone. Although it must be noted that cardiovascular deaths accounted for the highest mortality rate in both groups, nonetheless the relative overall mortality rate for one group over the other was estimated at 3.89. Other conditions such as diabetic complications, infectious disease and unknown causes along with Addison’s disease all tend to exacerbate the mortality rates versus diabetes alone. [12]
| |
| | |
| *Race
| |
| Addison disease has no specific predilection to any race.
| |
| | |
| *Sex
| |
| Addison disease that is autoimmune in origin and tending to be idiopathic is more commonly found in females and children.
| |
| | |
| *Age
| |
| Commonly, the age of presrntation is between 30-50 years of age., however, the disease may present itself earlier in association with other syndromes such as congenital adrenal hyperplasia, polyglandular syndromes or if the onset of Addison is secondary to a disorder of long chain fatty acid metabolism.
| |
| | |
| ==[[Adrenal insufficiency risk factors|Risk Factors]]==
| |
| | |
| ==[[Adrenal insufficiency natural history, complications and prognosis|Natural History, Complications and Prognosis]]==
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| [[Adrenal insufficiency history and symptoms| History and Symptoms]] | [[Adrenal insufficiency physical examination | Physical Examination]] | [[Adrenal insufficiency laboratory findings|Laboratory Findings]] | [[Adrenal insufficiency electrocardiogram|Electrocardiogram]] | [[Adrenal insufficiency chest x ray|Chest X Ray]] | [[Adrenal insufficiency CT|CT]] | [[Adrenal insufficiency MRI|MRI]] | [[Adrenal insufficiency ultrasound|Ultrasound]] | [[Adrenal insufficiency other imaging findings|Other Imaging Findings]] | [[Adrenal insufficiency other diagnostic studies|Other Diagnostic Studies]] | | [[Secondary adrenal insufficiency history and symptoms| History and Symptoms]] | [[Secondary adrenal insufficiency physical examination | Physical Examination]] | [[Secondary adrenal insufficiency laboratory findings|Laboratory Findings]] | [[Secondary adrenal insufficiency electrocardiogram|Electrocardiogram]] | [[Secondary adrenal insufficiency chest x ray|Chest X Ray]] | [[Secondary adrenal insufficiency CT|CT]] | [[Secondary adrenal insufficiency MRI|MRI]] | [[Secondary adrenal insufficiency ultrasound|Ultrasound]] | [[Secondary adrenal insufficiency other imaging findings|Other Imaging Findings]] | [[Secondary adrenal insufficiency other diagnostic studies|Other Diagnostic Studies]] |
|
| |
|
| ==Treatment== | | ==Treatment== |
| [[Adrenal insufficiency medical therapy|Medical Therapy]] | [[Adrenal insufficiency surgery|Surgery]] | [[Adrenal insufficiency primary prevention|Primary Prevention]] | [[Adrenal insufficiency secondary prevention|Secondary Prevention]] | [[Adrenal insufficiency cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Adrenal insufficiency future or investigational therapies|Future or Investigational Therapies]] | | [[Secondary adrenal insufficiency medical therapy|Medical Therapy]] | [[Secondary adrenal insufficiency surgery|Surgery]] | [[Secondary adrenal insufficiency primary prevention|Primary Prevention]] | [[Secondary adrenal insufficiency secondary prevention|Secondary Prevention]] | [[Secondary adrenal insufficiency cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Secondary adrenal insufficiency future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| ==Case Studies== | | ==Case Studies== |
| [[Adrenal insufficiency case study one|Case#1]] | | [[Secondary adrenal insufficiency case study one|Case#1]] |
|
| |
|
| ==Related Chapters== | | ==Related Chapters== |