Riedel's thyroiditis pathophysiology: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (25 intermediate revisions by 3 users not shown) | |||
| Line 6: | Line 6: | ||
The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid [[autoantibodies]] and [[lymphoid]] infiltration of the thyroid gland resembling that of [[Hashimoto's thyroiditis]] might indicate an [[autoimmune]] etiology. It is considered that the infiltrating [[lymphocytes]] release [[cytokines]] which are responsible for the activation of [[fibroblasts]] responsible for the fibrosis. Riedel's thyroiditis is characterized by a replacement of the normal [[Parenchyma|thyroid parenchyma]] by a dense [[fibrosis]] that invades adjacent structures of the neck and extends beyond the thyroid capsule. This makes the thyroid gland stone-hard and fixed to adjacent structures. A shared mechanism with [[retroperitoneal fibrosis]] and [[sclerosing cholangitis]] has been suggested. | The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid [[autoantibodies]] and [[lymphoid]] infiltration of the [[thyroid gland]] resembling that of [[Hashimoto's thyroiditis]] might indicate an [[autoimmune]] etiology. It is considered that the infiltrating [[lymphocytes]] release [[cytokines]] which are responsible for the activation of [[fibroblasts]] responsible for the [[fibrosis]]. Riedel's thyroiditis is characterized by a replacement of the normal [[Parenchyma|thyroid parenchyma]] by a dense [[fibrosis]] that invades adjacent structures of the neck and extends beyond the thyroid capsule. This makes the [[thyroid gland]] stone-hard and fixed to adjacent structures. A shared mechanism with [[retroperitoneal fibrosis]] and [[sclerosing cholangitis]] has been suggested. | ||
==Pathophysiology== | ==Pathophysiology== | ||
{| | |||
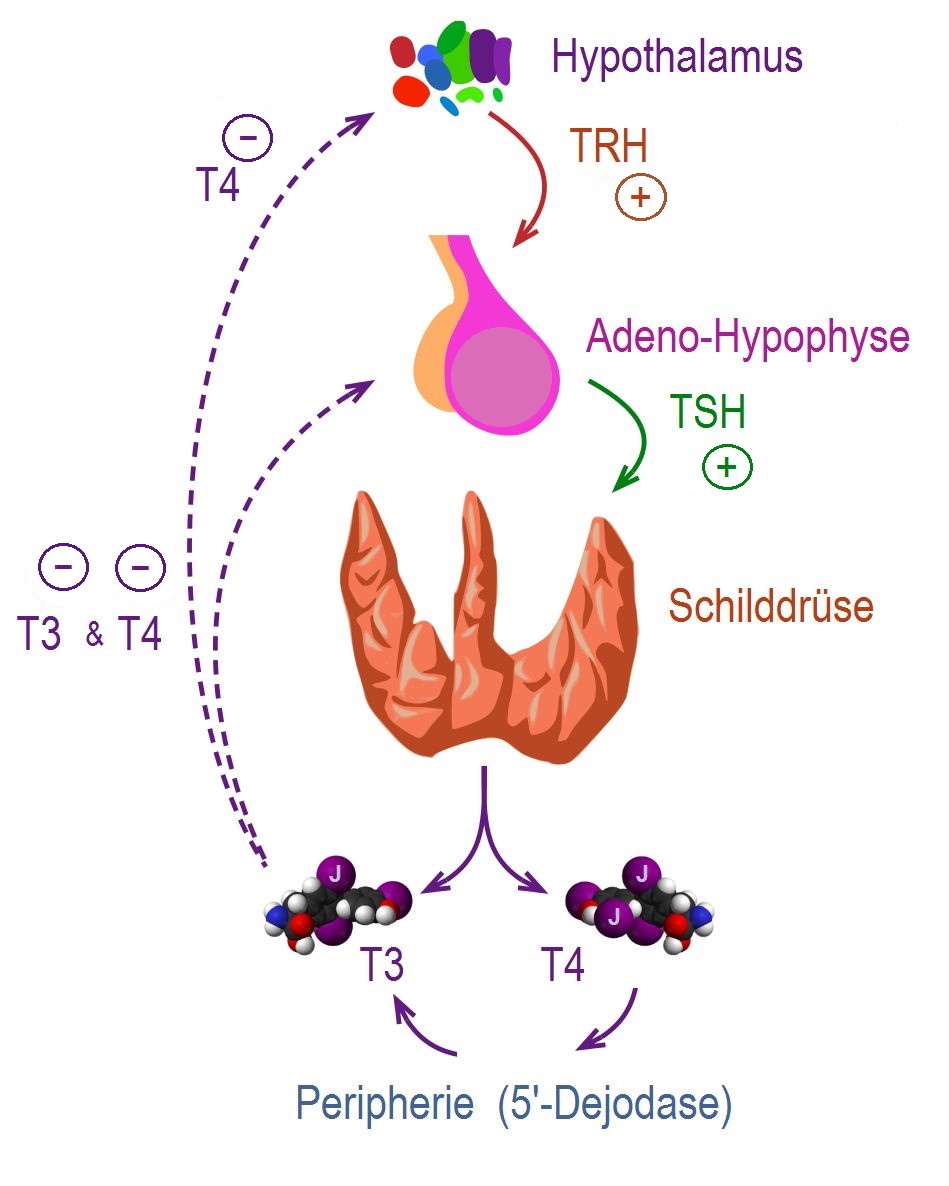
=== | |The control, synthesis, and release of the thyroid hormone is usually controlled by [[hypothalamus]] and [[pituitary gland]].<ref name="pmid25905405">{{cite journal |vauthors=De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J |title=Thyroid Hormone Synthesis And Secretion |journal= |volume= |issue= |pages= |year= |pmid=25905405 |doi= |url=}}</ref><ref name="pmid11949270">{{cite journal |vauthors=Kirsten D |title=The thyroid gland: physiology and pathophysiology |journal=Neonatal Netw |volume=19 |issue=8 |pages=11–26 |year=2000 |pmid=11949270 |doi=10.1891/0730-0832.19.8.11 |url=}}</ref> | ||
The exact | * [[Thyroid hormone|Thyroid hormones (T3 and T4)]] are regulating [[basal metabolic rate]], influence [[oxygen]] consumption by tissues. They are crucial for normal development of the [[brain]] and growth of the body. | ||
* Secretion of [[thyroid hormones]] follows upper control from the [[hypothalamus]] and the [[pituitary]]. [[Thyrotropin-releasing hormone|Thyroid releasing hormone (TRH)]] acts on [[thyrotropes]] releasing cells in the [[pituitary]] causing them to release [[Thyroid-stimulating hormone|thyroid stimulating hormone (TSH)]]. | |||
* [[TSH]] acts on [[thyroid gland]] by binding to specific membrane receptors and activating an [[intracellular]] pathway involving [[cAMP]] that ends in the formation and secretion of [[thyroid hormones]]. | |||
* [[Iodine]] is essential for the synthesis of [[thyroid hormones]]. [[Iodide]] is up taken through a special [[Sodium-iodide symporter]](Na/I) found in the membrane of [[thyroid]] follicular cell. After the [[iodide]] uptake, it goes through a series of organic reactions ending in the formation of the two forms of [[thyroid hormones]]: [[T3]] and [[T4]]. [[T3]] and [[T4]] remain stored in the [[thyroglobulin]] of the follicles and are released in response to further stimulation by [[TSH]] to the [[Thyroid follicle|thyroid follicles]]. | |||
* While [[T3]] is 3 to 5 times more potent than [[T4]], it represents only one-fourth of the total hormone secretion. [[T3]] is thought to be the biologically active form of the hormone. Most of the circulating [[T3]] is due to peripheral conversion of [[T4]] in the liver and peripheral tissues while only a small percentage is secreted directly from the [[thyroid gland]] itself. | |||
* [[T3]] and [[T4]] act on nuclear receptors ([[DNA]] binding [[proteins]]) and cause the regulate the [[transcription]] of many [[proteins]] to regulate the [[metabolic rate]] of the body. | |||
* The higher regulation of [[thyroxine]] secretion follows the [[negative feedback]] role, meaning that high levels of [[T3]] and [[T4]] will suppress [[TRH]] and [[TSH]] secretion and vice versa (Low levels of [[Thyroxin|thyroxine]] will stimulate [[TRH]] and [[TSH]] secretion). This is useful in diagnosing the cause of [[hyperthyroidism]]. | |||
* [[TSH]] will be low in [[hyperthyroidism|primary hyperthyroidism]] where the gland is the source of the excess hormones. In [[hyperthyroidism|secondary hyperthyroidism]], [[TSH]] will be high as the [[pituitary]] or the [[hypothalamus]] are the sources of the disease. | |||
| | |||
[[Image: Regulation der Schilddrüsenfunktion .jpg|right|300px|thumb|'''Regulation of thyroid hormone secretion.''' <small>Source:By CFCF; slightly modified by Geo-Science-International - This file was derived from Thyroid vector.svg:, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=47043638</small>]] | |||
|} | |||
<br clear="left" /> | |||
===Pathogenesis=== | |||
The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid [[autoantibodies]] and lymphoid infiltration of the [[thyroid gland]] resembling that of [[Hashimoto's thyroiditis]] might indicate an [[autoimmune]] etiology.<ref name="pmid3057862">{{cite journal |vauthors=Schwaegerle SM, Bauer TW, Esselstyn CB |title=Riedel's thyroiditis |journal=Am. J. Clin. Pathol. |volume=90 |issue=6 |pages=715–22 |year=1988 |pmid=3057862 |doi= |url=}}</ref> | |||
*It is considered that the infiltrating [[lymphocytes]] (CD4+ and CD8+) release [[cytokines]] which are responsible for the activation of [[fibroblasts]] responsible for the fibrosis.<ref name="pmid8120524">{{cite journal |vauthors=Zimmermann-Belsing T, Feldt-Rasmussen U |title=Riedel's thyroiditis: an autoimmune or primary fibrotic disease? |journal=J. Intern. Med. |volume=235 |issue=3 |pages=271–4 |year=1994 |pmid=8120524 |doi= |url=}}</ref> | *It is considered that the infiltrating [[lymphocytes]] (CD4+ and CD8+) release [[cytokines]] which are responsible for the activation of [[fibroblasts]] responsible for the fibrosis.<ref name="pmid8120524">{{cite journal |vauthors=Zimmermann-Belsing T, Feldt-Rasmussen U |title=Riedel's thyroiditis: an autoimmune or primary fibrotic disease? |journal=J. Intern. Med. |volume=235 |issue=3 |pages=271–4 |year=1994 |pmid=8120524 |doi= |url=}}</ref> | ||
*Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense [[fibrosis]] that invades adjacent structures of the neck and extends beyond the thyroid capsule.This makes the thyroid gland stone-hard and fixed to adjacent structures.<ref name="pmid17603227">{{cite journal |author=Cho MH, Kim CS, Park JS, ''et al'' |title=Riedel's thyroiditis in a patient with recurrent subacute thyroiditis: a case report and review of the literature |journal=Endocr. J. |volume=54 |issue=4 |pages=559–62 |year=2007|pmid=17603227 |doi= |url=http://joi.jlc.jst.go.jp/JST.JSTAGE/endocrj/K06-186?from=PubMed}}</ref> | *Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense [[fibrosis]] that invades adjacent structures of the neck and extends beyond the thyroid capsule.This makes the [[thyroid gland]] stone-hard and fixed to adjacent structures.<ref name="pmid17603227">{{cite journal |author=Cho MH, Kim CS, Park JS, ''et al'' |title=Riedel's thyroiditis in a patient with recurrent subacute thyroiditis: a case report and review of the literature |journal=Endocr. J. |volume=54 |issue=4 |pages=559–62 |year=2007|pmid=17603227 |doi= |url=http://joi.jlc.jst.go.jp/JST.JSTAGE/endocrj/K06-186?from=PubMed}}</ref> | ||
*Tissue [[eosinophilia]] and [[Major basic protein]] (MBP) identified in the thyroid gland on the [[histopathological]] analysis are also thought to play a role in the proliferation of [[fibroblasts]].<ref name="urlTissue eosinophilia and eosinophil degranulation in Riedels invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic">{{cite web |url=https://doi.org/10.1210/jcem.81.3.8772560 |title=Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic |format= |work= |accessdate=}}</ref> | *Tissue [[eosinophilia]] and [[Major basic protein]] (MBP) identified in the [[thyroid gland]] on the [[histopathological]] analysis are also thought to play a role in the proliferation of [[fibroblasts]].<ref name="urlTissue eosinophilia and eosinophil degranulation in Riedels invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic">{{cite web |url=https://doi.org/10.1210/jcem.81.3.8772560 |title=Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic |format= |work= |accessdate=}}</ref> | ||
*A shared mechanism with [[retroperitoneal fibrosis]] and [[sclerosing cholangitis]] is also suggested.<ref name="pmid8504980">{{cite journal |author=De Boer WA |title=Riedel's thyroiditis, retroperitoneal fibrosis, and sclerosing cholangitis: diseases with one pathogenesis? |journal=Gut |volume=34 |issue=5 |pages=714 |year=1993|pmid=8504980 |pmc=1374200 |doi= |url=http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=8504980}}</ref> | *A shared mechanism with [[retroperitoneal fibrosis]] and [[sclerosing cholangitis]] is also suggested.<ref name="pmid8504980">{{cite journal |author=De Boer WA |title=Riedel's thyroiditis, retroperitoneal fibrosis, and sclerosing cholangitis: diseases with one pathogenesis? |journal=Gut |volume=34 |issue=5 |pages=714 |year=1993|pmid=8504980 |pmc=1374200 |doi= |url=http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=8504980}}</ref> | ||
=== | ===Hypotheses=== | ||
The following hypotheses regarding the pathogenesis of Riedel's thyroiditis have been proposed:<ref name="pmid15298150">{{cite journal |vauthors=Papi G, LiVolsi VA |title=Current concepts on Riedel thyroiditis |journal=Am. J. Clin. Pathol. |volume=121 Suppl |issue= |pages=S50–63 |year=2004 |pmid=15298150 |doi= |url=}}</ref> | The following hypotheses regarding the pathogenesis of Riedel's thyroiditis have been proposed:<ref name="pmid15298150">{{cite journal |vauthors=Papi G, LiVolsi VA |title=Current concepts on Riedel thyroiditis |journal=Am. J. Clin. Pathol. |volume=121 Suppl |issue= |pages=S50–63 |year=2004 |pmid=15298150 |doi= |url=}}</ref> | ||
====The Systemic Autoimmune Hypothesis==== | ====The Systemic Autoimmune Hypothesis==== | ||
According to this theory, Riedel's thyroiditis might be a primary disease of fibroblasts triggered by autoimmune stimuli. | According to this theory, Riedel's thyroiditis (RT) might be a primary disease of [[fibroblasts]] triggered by autoimmune stimuli.<ref name="pmid15298150">{{cite journal |vauthors=Papi G, LiVolsi VA |title=Current concepts on Riedel thyroiditis |journal=Am. J. Clin. Pathol. |volume=121 Suppl |issue= |pages=S50–63 |year=2004 |pmid=15298150 |doi= |url=}}</ref><ref name="pmid8772560">{{cite journal |vauthors=Heufelder AE, Goellner JR, Bahn RS, Gleich GJ, Hay ID |title=Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis |journal=J. Clin. Endocrinol. Metab. |volume=81 |issue=3 |pages=977–84 |year=1996 |pmid=8772560 |doi=10.1210/jcem.81.3.8772560 |url=}}</ref><ref name="pmid1739138">{{cite journal |vauthors=Noguchi H, Kephart GM, Colby TV, Gleich GJ |title=Tissue eosinophilia and eosinophil degranulation in syndromes associated with fibrosis |journal=Am. J. Pathol. |volume=140 |issue=2 |pages=521–8 |year=1992 |pmid=1739138 |pmc=1886427 |doi= |url=}}</ref><ref name="pmid3538819">{{cite journal |vauthors=Gleich GJ, Adolphson CR |title=The eosinophilic leukocyte: structure and function |journal=Adv. Immunol. |volume=39 |issue= |pages=177–253 |year=1986 |pmid=3538819 |doi= |url=}}</ref><ref name="pmid501097">{{cite journal |vauthors=Gleich GJ, Frigas E, Loegering DA, Wassom DL, Steinmuller D |title=Cytotoxic properties of the eosinophil major basic protein |journal=J. Immunol. |volume=123 |issue=6 |pages=2925–7 |year=1979 |pmid=501097 |doi= |url=}}</ref><ref name="pmid2242067">{{cite journal |vauthors=Seibold JR, Giorno RC, Claman HN |title=Dermal mast cell degranulation in systemic sclerosis |journal=Arthritis Rheum. |volume=33 |issue=11 |pages=1702–9 |year=1990 |pmid=2242067 |doi= |url=}}</ref> | ||
*It is proposed that the endothelial cells release oxidized low-density lipoprotein from atheromatous plaques following the injury resulting in an allergic hypersensitivity reaction. | *It is proposed that the endothelial cells release oxidized [[Low density lipoprotein|low-density lipoprotein]] from atheromatous plaques following the injury resulting in an [[Allergy|allergic]] [[Hypersensitivity|hypersensitivity reaction]]. | ||
*The natural consequence of this hypothesis is that the antigen initiating fibrosis is not localized within the thyroid but is affected secondarily by a systemic fibroinflammatory process. | *The natural consequence of this hypothesis is that the [[antigen]] initiating [[fibrosis]] is not localized within the thyroid but is affected secondarily by a systemic fibroinflammatory process. | ||
*Thyroid follicular cells, | *Thyroid [[follicular cells]], peri-thyroid muscular cells, or intrathyroidal [[Endothelium|endothelial cells]] express antigens, [[cytokines]], or [[Adhesion molecule|adhesion molecules]] that might contribute to local activation of the disease. The evidence of a [[Perivascular cell|perivascular]] concentration of inflammatory cells in RT (occlusive [[Phlebitis|phlebiti]]<nowiki/>s) might support the theory that the allergic process first involves blood vessels. | ||
*Once the allergic reaction has started, a heavy inflammatory cell population such as B and T lymphocytes, plasma cells, monocytes, and eosinophils infiltrate tissues and produce several cytokines. | *Once the [[allergic reaction]] has started, a heavy inflammatory cell population such as [[B lymphocytes|B]] and [[T lymphocytes]], [[plasma cells]], [[monocytes]], and [[eosinophils]] infiltrate tissues and produce several [[cytokines]]. | ||
*The role of eosinophils in this context probably is central. When eosinophils migrate into the tissues involved by the disease, they degranulate and release cationic toxins into connective tissue including Major basic protein (MBP), eosinophil cationic protein, eosinophil peroxidase, and eosinophil-derived neurotoxin. | *The role of [[eosinophils]] in this context probably is central. When eosinophils migrate into the tissues involved by the disease, they degranulate and release cationic toxins into connective tissue including [[Major basic protein]] (MBP), [[eosinophil cationic protein]], [[eosinophil peroxidase]], and [[eosinophil-derived neurotoxin]]. | ||
*Eosinophils also release cytokines, the most important of which are transforming growth factor β, transforming growth factor α, and granulocyte-macrophage colony-stimulating factor. This stimulates fibroblast proliferation that finally causes fibrosis. | *[[Eosinophils]] also release [[cytokines]], the most important of which are [[transforming growth factor β]], [[Transforming growth factor alpha|transforming growth factor α]], and [[granulocyte-macrophage colony-stimulating factor]]. This stimulates [[fibroblast]] proliferation that finally causes [[fibrosis]]. | ||
====The Genetic Hypothesis==== | ====The Genetic Hypothesis==== | ||
This hypothesis was | This hypothesis was proposed for the [[multifocal fibrosclerosis]] which is associated with Riedel's thyroiditis.<ref name="pmid6025229">{{cite journal |vauthors=Comings DE, Skubi KB, Van Eyes J, Motulsky AG |title=Familial multifocal fibrosclerosis. Findings suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel's thyroiditis, and pseudotumor of the orbit may be different manifestations of a single disease |journal=Ann. Intern. Med. |volume=66 |issue=5 |pages=884–92 |year=1967 |pmid=6025229 |doi= |url=}}</ref> | ||
*The basis of this hypothesis was a report of multifocal fibrosclerotic disease in two brothers, whose parents were first cousins. They developed different combinations of the multifocal fibrosclerotic disease and a familial [[multifocal fibrosclerosis]] was hypothesized. | |||
*It was thought that genetic factors might have played a partial role in an enzymatic defect in the [[tryptophan]] → [[serotonin]] → [[5-Hydroxyindoleacetic acid|5-hydroxyindolacetic acid]] pathway. However, such a relationship has never been proven, and the siblings described remain the only case of familial multifocal fibrosclerosis reported in the literature. | |||
====The Intrathyroidal hypothesis==== | ====The Intrathyroidal hypothesis==== | ||
Riedel's thyroiditis is associated with Hashimoto's thyroiditis | Riedel's thyroiditis is associated with [[Hashimoto's thyroiditis]] and [[de Quervain's thyroiditis]].<ref name="book">{{cite book |vauthors=Ewing J |title=Neoplastic Diseases 2nd edition |year=1919 |publisher=Saunders; 1922:908}}</ref> | ||
*It is proposed that Riedel's thyroiditis might represent a late [[Fibrosis|fibrotic]] stage of [[Subacute thyroiditis|subacute]] or chronic [[thyroiditis]]. The fundamental concept of this theory is that the fibrosing process of RT is specific to the [[thyroid gland]]. | |||
====The Pharmacologic Hypothesis==== | ====The Pharmacologic Hypothesis==== | ||
This hypothesis is also proposed primarily for [[multifocal fibrosclerosis]]. As Riedel's thyroiditis is associated with [[multifocal fibrosclerosis]] this theory might explain the indirect association of Riedel's thyroiditis with drugs.<ref name="pmid15298150">{{cite journal |vauthors=Papi G, LiVolsi VA |title=Current concepts on Riedel thyroiditis |journal=Am. J. Clin. Pathol. |volume=121 Suppl |issue= |pages=S50–63 |year=2004 |pmid=15298150 |doi= |url=}}</ref><ref name="pmid12045432">{{cite journal |vauthors=Drieskens O, Blockmans D, Van den Bruel A, Mortelmans L |title=Riedel's thyroiditis and retroperitoneal fibrosis in multifocal fibrosclerosis: positron emission tomographic findings |journal=Clin Nucl Med |volume=27 |issue=6 |pages=413–5 |year=2002 |pmid=12045432 |doi= |url=}}</ref> | |||
*The production of fibrosis by the drugs might be determined by an increased serum [[serotonin]] concentration through [[competitive inhibition]] at the [[serotonin receptor]] level and a reaction of [[hypersensitivity]] causing [[Vasculitis|vasculiti]]<nowiki/>s and<nowiki/> plasma exudation resulting in fibrosis. | |||
*Although drugs have been found to cause multi organ [[fibrosis]], there are no reports regarding medication induced Riedel's thyroiditis. This theory might explain the indirect association of Riedel's thyroiditis with drugs as Riedel's thyroiditis is associated with [[multifocal fibrosclerosis]]. | |||
==Associated Conditions== | ==Associated Conditions== | ||
Riedel's thyroiditis is associated various other autoimmune conditions including:<ref name="pmid8120524">{{cite journal |vauthors=Zimmermann-Belsing T, Feldt-Rasmussen U |title=Riedel's thyroiditis: an autoimmune or primary fibrotic disease? |journal=J. Intern. Med. |volume=235 |issue=3 |pages=271–4 |year=1994 |pmid=8120524 |doi= |url=}}</ref><ref name="pmid4413980">{{cite journal |vauthors=Drury MI, Sweeney EC, Heffernan SJ |title=Invasive fibrous (Riedel's) thyroiditis |journal=Ir Med J |volume=67 |issue=14 |pages=388–90 |year=1974 |pmid=4413980 |doi= |url=}}</ref><ref name="urlChronic thyroiditis: A case showing features of both riedels and hashimotos thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library">{{cite web |url=http://dx.doi.org/10.1002/bjs.18003514015 |title=Chronic thyroiditis: A case showing features of both riedel's and hashimoto's thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library |format= |work= |accessdate=}}</ref><ref name="Invasive Fibrous (Riedel's) Thyroiditis">{{cite journal |vauthors=Hines RC, Scheuermann HA, Royster HP |title=Invasive Fibrous (Riedel's) Thyroiditis With Bilateral Fibrous Parotitis.|journal=JAMA|pages=869-871 |year=1970 |doi=10.1001/jama.1970.03170310147054 |url=http://jamanetwork.com/journals/jama/article-abstract/355936}}</ref><ref name="urlRiedels Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic">{{cite web |url=https://doi.org/10.1210/jc.2011-0617 |title=Riedel's Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic |format= |work= |accessdate=}}</ref><ref name="pmid12045432">{{cite journal |vauthors=Drieskens O, Blockmans D, Van den Bruel A, Mortelmans L |title=Riedel's thyroiditis and retroperitoneal fibrosis in multifocal fibrosclerosis: positron emission tomographic findings |journal=Clin Nucl Med |volume=27 |issue=6 |pages=413–5 |year=2002 |pmid=12045432 |doi= |url=}}</ref> | Riedel's thyroiditis is associated various other [[Autoimmune disease|autoimmune conditions]] including:<ref name="pmid8120524">{{cite journal |vauthors=Zimmermann-Belsing T, Feldt-Rasmussen U |title=Riedel's thyroiditis: an autoimmune or primary fibrotic disease? |journal=J. Intern. Med. |volume=235 |issue=3 |pages=271–4 |year=1994 |pmid=8120524 |doi= |url=}}</ref><ref name="pmid4413980">{{cite journal |vauthors=Drury MI, Sweeney EC, Heffernan SJ |title=Invasive fibrous (Riedel's) thyroiditis |journal=Ir Med J |volume=67 |issue=14 |pages=388–90 |year=1974 |pmid=4413980 |doi= |url=}}</ref><ref name="urlChronic thyroiditis: A case showing features of both riedels and hashimotos thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library">{{cite web |url=http://dx.doi.org/10.1002/bjs.18003514015 |title=Chronic thyroiditis: A case showing features of both riedel's and hashimoto's thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library |format= |work= |accessdate=}}</ref><ref name="Invasive Fibrous (Riedel's) Thyroiditis">{{cite journal |vauthors=Hines RC, Scheuermann HA, Royster HP |title=Invasive Fibrous (Riedel's) Thyroiditis With Bilateral Fibrous Parotitis.|journal=JAMA|pages=869-871 |year=1970 |doi=10.1001/jama.1970.03170310147054 |url=http://jamanetwork.com/journals/jama/article-abstract/355936}}</ref><ref name="urlRiedels Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic">{{cite web |url=https://doi.org/10.1210/jc.2011-0617 |title=Riedel's Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic |format= |work= |accessdate=}}</ref><ref name="pmid12045432">{{cite journal |vauthors=Drieskens O, Blockmans D, Van den Bruel A, Mortelmans L |title=Riedel's thyroiditis and retroperitoneal fibrosis in multifocal fibrosclerosis: positron emission tomographic findings |journal=Clin Nucl Med |volume=27 |issue=6 |pages=413–5 |year=2002 |pmid=12045432 |doi= |url=}}</ref> | ||
*[[Graves’ disease]] | *[[Graves’ disease]] | ||
*[[Hashimoto's thyroiditis|Hashimoto’s thyroiditis]] | *[[Hashimoto's thyroiditis|Hashimoto’s thyroiditis]] | ||
*Multifocal idiopathic fibrosclerosis | *[[Multifocal fibrosclerosis|Multifocal idiopathic fibrosclerosis]] | ||
*[[Addison's disease|Addison’s disease]] | *[[Addison's disease|Addison’s disease]] | ||
*[[Pernicious anemia]] | *[[Pernicious anemia]] | ||
| Line 44: | Line 64: | ||
==Gross Pathology== | ==Gross Pathology== | ||
On gross pathology the following findings are characteristic of Riedel's thyroiditis:<ref name="urlRiedel’s Thyroiditis | American Journal of Clinical Pathology | Oxford Academic">{{cite web |url=https://doi.org/10.1093/ajcp/90.6.715 |title=Riedel’s Thyroiditis | American Journal of Clinical Pathology | Oxford Academic |format= |work= |accessdate=}}</ref> | |||
*Dense, [[avascular]] white fibrous tissue | |||
*Absence of a [[Capsule (anatomy)|capsule]] | |||
*Absence [[thyroid]] tissue | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
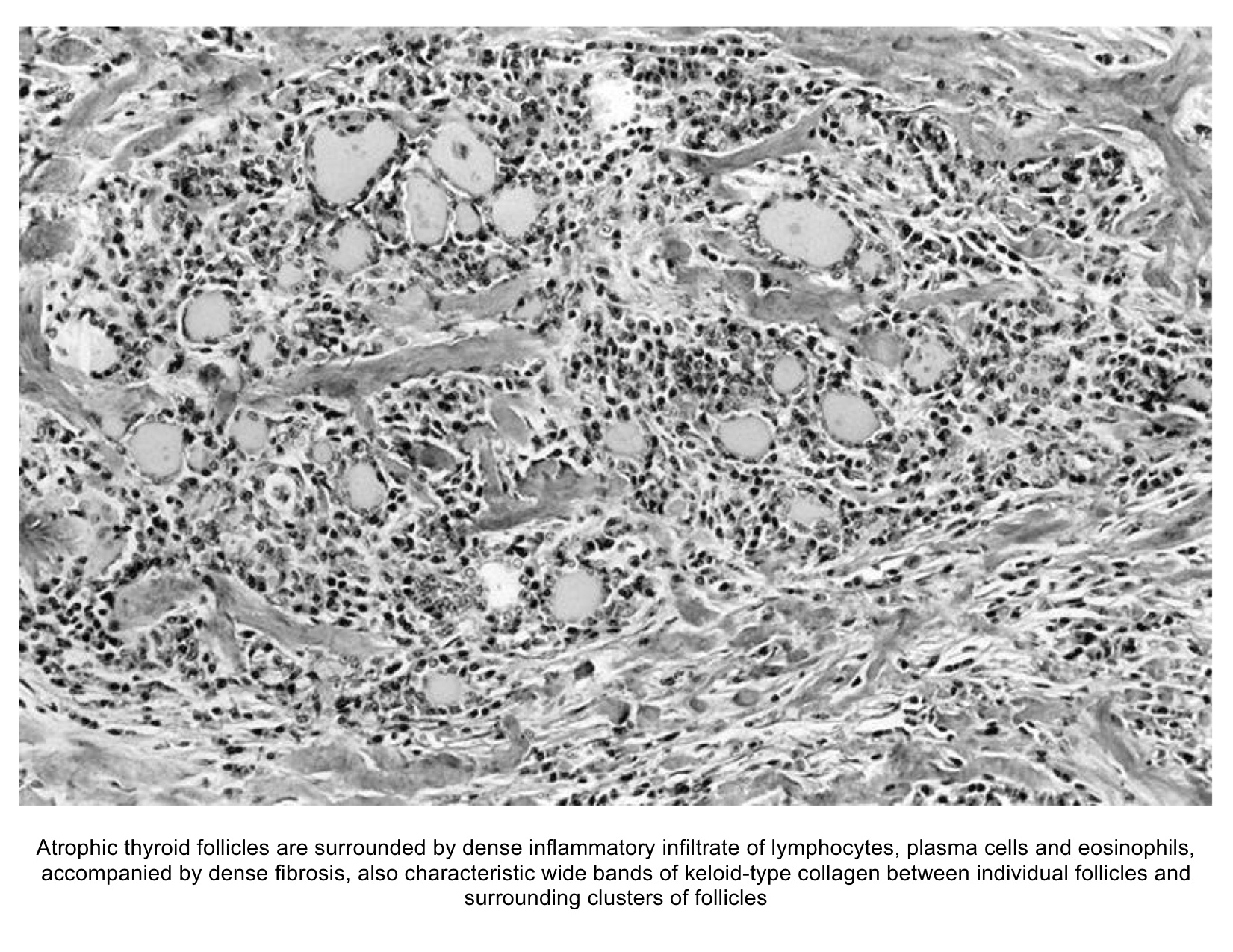
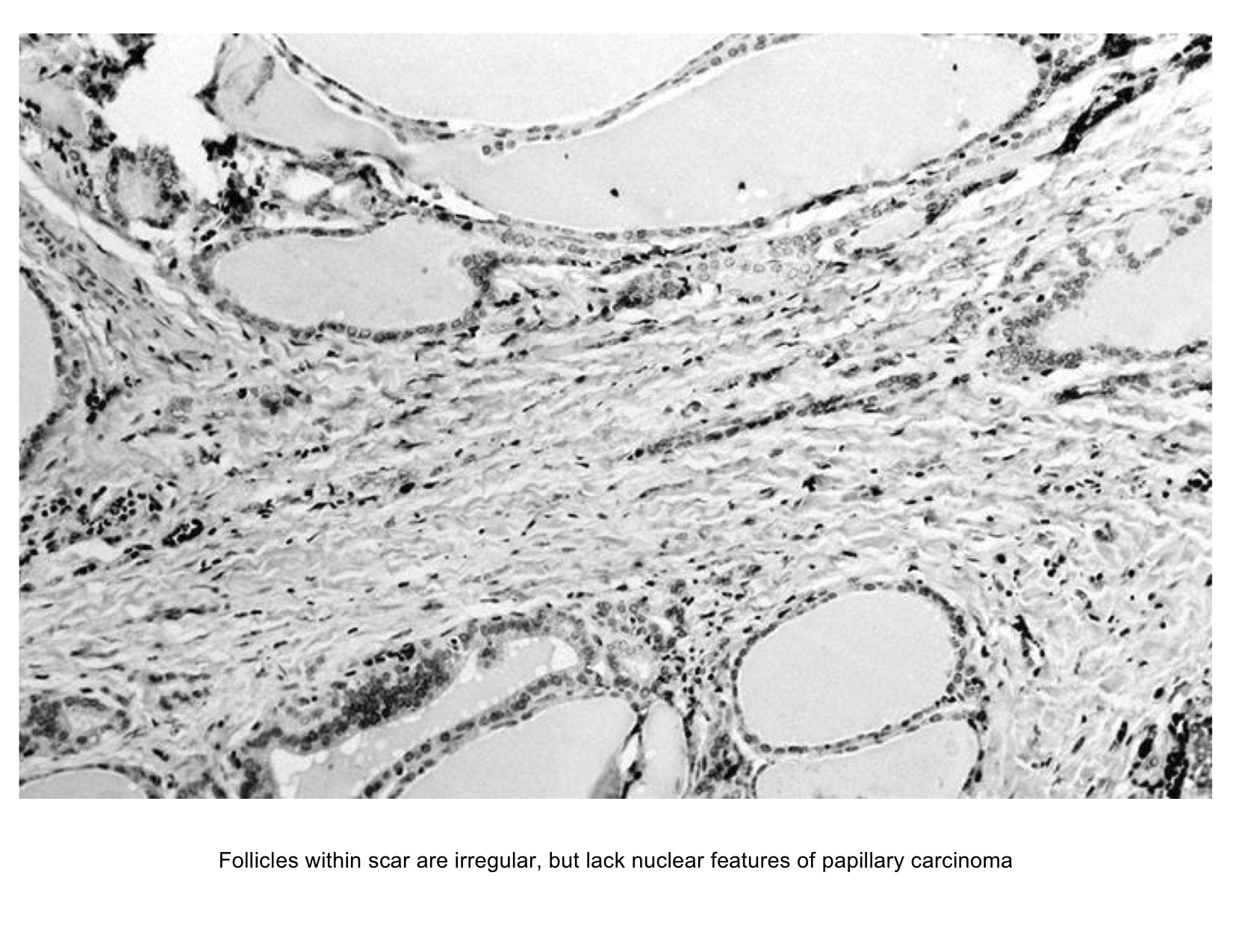
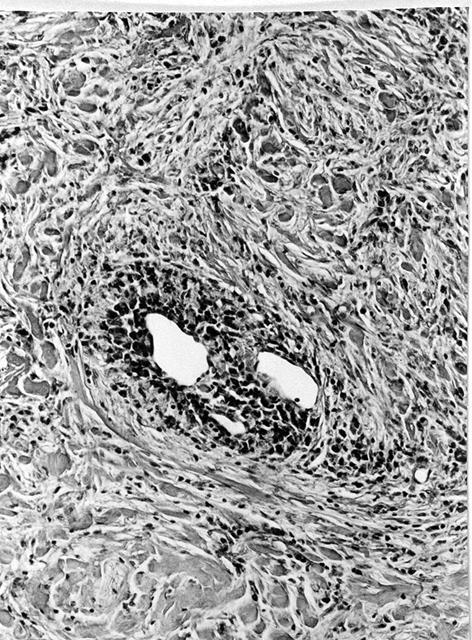
On microscopic [[histopathological]] analysis the following findings are usually seen:<ref name="urlRedirecting">{{cite web |url=https://doi.org/10.1016/S1001-9294(10)60036-3 |title=Redirecting |format= |work= |accessdate=}}</ref><ref name="pmid15298150">{{cite journal |vauthors=Papi G, LiVolsi VA |title=Current concepts on Riedel thyroiditis |journal=Am. J. Clin. Pathol. |volume=121 Suppl |issue= |pages=S50–63 |year=2004 |pmid=15298150 |doi= |url=}}</ref> | |||
*Destruction of thyroid follicle by inflammatory cells | |||
*Inflammatory cells including [[lymphocytes]], [[plasma cells]], and [[eosinophils]] in a dense matrix of hyalinized [[connective tissue]] | |||
*Fibrous tissues and invasion of surrounding structures | |||
==Gallery== | ==Gallery== | ||
| Line 66: | Line 92: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
| |||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 00:01, 30 July 2020
|
Riedel's thyroiditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Riedel's thyroiditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Riedel's thyroiditis pathophysiology |
|
Risk calculators and risk factors for Riedel's thyroiditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid autoantibodies and lymphoid infiltration of the thyroid gland resembling that of Hashimoto's thyroiditis might indicate an autoimmune etiology. It is considered that the infiltrating lymphocytes release cytokines which are responsible for the activation of fibroblasts responsible for the fibrosis. Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense fibrosis that invades adjacent structures of the neck and extends beyond the thyroid capsule. This makes the thyroid gland stone-hard and fixed to adjacent structures. A shared mechanism with retroperitoneal fibrosis and sclerosing cholangitis has been suggested.
Pathophysiology
The control, synthesis, and release of the thyroid hormone is usually controlled by hypothalamus and pituitary gland.[1][2]
|
 |
Pathogenesis
The exact pathogenesis of Riedel's thyroiditis is not fully understood. The presence of thyroid autoantibodies and lymphoid infiltration of the thyroid gland resembling that of Hashimoto's thyroiditis might indicate an autoimmune etiology.[3]
- It is considered that the infiltrating lymphocytes (CD4+ and CD8+) release cytokines which are responsible for the activation of fibroblasts responsible for the fibrosis.[4]
- Riedel's thyroiditis is characterized by a replacement of the normal thyroid parenchyma by a dense fibrosis that invades adjacent structures of the neck and extends beyond the thyroid capsule.This makes the thyroid gland stone-hard and fixed to adjacent structures.[5]
- Tissue eosinophilia and Major basic protein (MBP) identified in the thyroid gland on the histopathological analysis are also thought to play a role in the proliferation of fibroblasts.[6]
- A shared mechanism with retroperitoneal fibrosis and sclerosing cholangitis is also suggested.[7]
Hypotheses
The following hypotheses regarding the pathogenesis of Riedel's thyroiditis have been proposed:[8]
The Systemic Autoimmune Hypothesis
According to this theory, Riedel's thyroiditis (RT) might be a primary disease of fibroblasts triggered by autoimmune stimuli.[8][9][10][11][12][13]
- It is proposed that the endothelial cells release oxidized low-density lipoprotein from atheromatous plaques following the injury resulting in an allergic hypersensitivity reaction.
- The natural consequence of this hypothesis is that the antigen initiating fibrosis is not localized within the thyroid but is affected secondarily by a systemic fibroinflammatory process.
- Thyroid follicular cells, peri-thyroid muscular cells, or intrathyroidal endothelial cells express antigens, cytokines, or adhesion molecules that might contribute to local activation of the disease. The evidence of a perivascular concentration of inflammatory cells in RT (occlusive phlebitis) might support the theory that the allergic process first involves blood vessels.
- Once the allergic reaction has started, a heavy inflammatory cell population such as B and T lymphocytes, plasma cells, monocytes, and eosinophils infiltrate tissues and produce several cytokines.
- The role of eosinophils in this context probably is central. When eosinophils migrate into the tissues involved by the disease, they degranulate and release cationic toxins into connective tissue including Major basic protein (MBP), eosinophil cationic protein, eosinophil peroxidase, and eosinophil-derived neurotoxin.
- Eosinophils also release cytokines, the most important of which are transforming growth factor β, transforming growth factor α, and granulocyte-macrophage colony-stimulating factor. This stimulates fibroblast proliferation that finally causes fibrosis.
The Genetic Hypothesis
This hypothesis was proposed for the multifocal fibrosclerosis which is associated with Riedel's thyroiditis.[14]
- The basis of this hypothesis was a report of multifocal fibrosclerotic disease in two brothers, whose parents were first cousins. They developed different combinations of the multifocal fibrosclerotic disease and a familial multifocal fibrosclerosis was hypothesized.
- It was thought that genetic factors might have played a partial role in an enzymatic defect in the tryptophan → serotonin → 5-hydroxyindolacetic acid pathway. However, such a relationship has never been proven, and the siblings described remain the only case of familial multifocal fibrosclerosis reported in the literature.
The Intrathyroidal hypothesis
Riedel's thyroiditis is associated with Hashimoto's thyroiditis and de Quervain's thyroiditis.[15]
- It is proposed that Riedel's thyroiditis might represent a late fibrotic stage of subacute or chronic thyroiditis. The fundamental concept of this theory is that the fibrosing process of RT is specific to the thyroid gland.
The Pharmacologic Hypothesis
This hypothesis is also proposed primarily for multifocal fibrosclerosis. As Riedel's thyroiditis is associated with multifocal fibrosclerosis this theory might explain the indirect association of Riedel's thyroiditis with drugs.[8][16]
- The production of fibrosis by the drugs might be determined by an increased serum serotonin concentration through competitive inhibition at the serotonin receptor level and a reaction of hypersensitivity causing vasculitis and plasma exudation resulting in fibrosis.
- Although drugs have been found to cause multi organ fibrosis, there are no reports regarding medication induced Riedel's thyroiditis. This theory might explain the indirect association of Riedel's thyroiditis with drugs as Riedel's thyroiditis is associated with multifocal fibrosclerosis.
Associated Conditions
Riedel's thyroiditis is associated various other autoimmune conditions including:[4][17][18][19][20][16]
- Graves’ disease
- Hashimoto’s thyroiditis
- Multifocal idiopathic fibrosclerosis
- Addison’s disease
- Pernicious anemia
- Type 1 diabetes
Gross Pathology
On gross pathology the following findings are characteristic of Riedel's thyroiditis:[21]
Microscopic Pathology
On microscopic histopathological analysis the following findings are usually seen:[22][8]
- Destruction of thyroid follicle by inflammatory cells
- Inflammatory cells including lymphocytes, plasma cells, and eosinophils in a dense matrix of hyalinized connective tissue
- Fibrous tissues and invasion of surrounding structures
Gallery
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
-
Histology of Riedel's thyroiditis (Image courtesy of AFIP and PathologyOutlines.com; http://www.pathologyoutlines.com/topic/thyroidriedel.html )
References
- ↑ De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J. "Thyroid Hormone Synthesis And Secretion". PMID 25905405.
- ↑ Kirsten D (2000). "The thyroid gland: physiology and pathophysiology". Neonatal Netw. 19 (8): 11–26. doi:10.1891/0730-0832.19.8.11. PMID 11949270.
- ↑ Schwaegerle SM, Bauer TW, Esselstyn CB (1988). "Riedel's thyroiditis". Am. J. Clin. Pathol. 90 (6): 715–22. PMID 3057862.
- ↑ 4.0 4.1 Zimmermann-Belsing T, Feldt-Rasmussen U (1994). "Riedel's thyroiditis: an autoimmune or primary fibrotic disease?". J. Intern. Med. 235 (3): 271–4. PMID 8120524.
- ↑ Cho MH, Kim CS, Park JS; et al. (2007). "Riedel's thyroiditis in a patient with recurrent subacute thyroiditis: a case report and review of the literature". Endocr. J. 54 (4): 559–62. PMID 17603227.
- ↑ "Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ De Boer WA (1993). "Riedel's thyroiditis, retroperitoneal fibrosis, and sclerosing cholangitis: diseases with one pathogenesis?". Gut. 34 (5): 714. PMC 1374200. PMID 8504980.
- ↑ 8.0 8.1 8.2 8.3 Papi G, LiVolsi VA (2004). "Current concepts on Riedel thyroiditis". Am. J. Clin. Pathol. 121 Suppl: S50–63. PMID 15298150.
- ↑ Heufelder AE, Goellner JR, Bahn RS, Gleich GJ, Hay ID (1996). "Tissue eosinophilia and eosinophil degranulation in Riedel's invasive fibrous thyroiditis". J. Clin. Endocrinol. Metab. 81 (3): 977–84. doi:10.1210/jcem.81.3.8772560. PMID 8772560.
- ↑ Noguchi H, Kephart GM, Colby TV, Gleich GJ (1992). "Tissue eosinophilia and eosinophil degranulation in syndromes associated with fibrosis". Am. J. Pathol. 140 (2): 521–8. PMC 1886427. PMID 1739138.
- ↑ Gleich GJ, Adolphson CR (1986). "The eosinophilic leukocyte: structure and function". Adv. Immunol. 39: 177–253. PMID 3538819.
- ↑ Gleich GJ, Frigas E, Loegering DA, Wassom DL, Steinmuller D (1979). "Cytotoxic properties of the eosinophil major basic protein". J. Immunol. 123 (6): 2925–7. PMID 501097.
- ↑ Seibold JR, Giorno RC, Claman HN (1990). "Dermal mast cell degranulation in systemic sclerosis". Arthritis Rheum. 33 (11): 1702–9. PMID 2242067.
- ↑ Comings DE, Skubi KB, Van Eyes J, Motulsky AG (1967). "Familial multifocal fibrosclerosis. Findings suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel's thyroiditis, and pseudotumor of the orbit may be different manifestations of a single disease". Ann. Intern. Med. 66 (5): 884–92. PMID 6025229.
- ↑ Ewing J (1919). Neoplastic Diseases 2nd edition. Saunders; 1922:908.
- ↑ 16.0 16.1 Drieskens O, Blockmans D, Van den Bruel A, Mortelmans L (2002). "Riedel's thyroiditis and retroperitoneal fibrosis in multifocal fibrosclerosis: positron emission tomographic findings". Clin Nucl Med. 27 (6): 413–5. PMID 12045432.
- ↑ Drury MI, Sweeney EC, Heffernan SJ (1974). "Invasive fibrous (Riedel's) thyroiditis". Ir Med J. 67 (14): 388–90. PMID 4413980.
- ↑ "Chronic thyroiditis: A case showing features of both riedel's and hashimoto's thyroiditis - Merrington - 1948 - British Journal of Surgery - Wiley Online Library".
- ↑ Hines RC, Scheuermann HA, Royster HP (1970). "Invasive Fibrous (Riedel's) Thyroiditis With Bilateral Fibrous Parotitis". JAMA: 869–871. doi:10.1001/jama.1970.03170310147054.
- ↑ "Riedel's Thyroiditis: A Clinical Review | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ "Riedel's Thyroiditis | American Journal of Clinical Pathology | Oxford Academic".
- ↑ "Redirecting".