Pre-excitation syndrome: Difference between revisions
Sara Mohsin (talk | contribs) No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}}, '''Associate Editor-In-Chief:''' {{Shivam Singla}} | {{CMG}}, '''Associate Editor-In-Chief:''' {{Shivam Singla}} | ||
[[File:WPW-in-SR (1).jpg|thumb | [[File:WPW-in-SR (1).jpg|thumb]] | ||
== Overview == | ==Overview== | ||
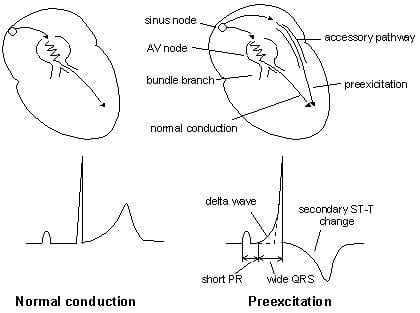
'''Pre-excitation syndrome''' is a condition where [[ventricles]] of the heart | '''Pre-excitation syndrome''' is a condition where [[ventricles]] of the heart depolarize earlier than the normal leading to the premature contraction.. Normally the atria and the ventricles are isolated electrically and only electrical passage existing in between atria and ventricles is at Atrioventricular Node. In all pre-excitation syndromes there is also present an additional conducting pathway besides the AV junction. So the electrical impulses passes to the ventricles even before the normal wave of depolarization that is about to conduct through AV node. This mechanism of depolarization of ventricles through additional by pass pathway much earlier than the usual depolarization pathway (through AV node) is referred to as "Pre- Excitation". The secondary conduction pathways are generally named as Bundle of His. | ||
== Historical Perspective == | ==Historical Perspective== | ||
*In 1930, it was first described by Louis Wolff, John Parkinson, and Paul Dudley White. They found the association of these conditions with a small risk of [[sudden cardiac death]]. | *In 1930, it was first described by Louis Wolff, John Parkinson, and Paul Dudley White. They found the association of these conditions with a small risk of [[sudden cardiac death]]. | ||
== Classification == | ==Classification== | ||
*Pre-excitation syndrome may be classified into sub-types | *Pre-excitation syndrome may be classified into sub-types | ||
{| class="wikitable" | {| class="wikitable" | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Type}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Type}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Conduction pathway}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Conduction pathway}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|PR interval}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|PR interval}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|QRS interval}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|QRS interval}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Delta wave}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Delta wave}} | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wolff-Parkinson-White syndrome]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wolff-Parkinson-White syndrome]] | ||
|[[Bundle of Kent]] (atria to ventricles) | |[[Bundle of Kent]] (atria to ventricles) | ||
|short | |short | ||
| Line 29: | Line 29: | ||
|yes | |yes | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Lown-Ganong-Levine syndrome]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Lown-Ganong-Levine syndrome]] | ||
|"James bundle" (atria to bundle of His) | |"James bundle" (atria to bundle of His) | ||
|short | |short | ||
| Line 35: | Line 35: | ||
|no | |no | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Mahaim-type | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Mahaim-type | ||
|[[Mahaim fibers]] | |[[Mahaim fibers]] | ||
|normal | |normal | ||
| Line 42: | Line 42: | ||
|} | |} | ||
=== WPW Syndrome === | ===WPW Syndrome=== | ||
WPW is a combination of the presence of '''congenital accessory pathways along with episodic [[tachyarrhythmias]]'''. Here the accessory pathways are referred to as ''[[Bundle of Kent]] or [[AV bypass tracts]].'' | WPW is a combination of the presence of '''congenital accessory pathways along with episodic [[tachyarrhythmias]]'''. Here the accessory pathways are referred to as ''[[Bundle of Kent]] or [[AV bypass tracts]].'' | ||
| Line 51: | Line 51: | ||
*Shortened PR interval (Less than 120ms) | *Shortened PR interval (Less than 120ms) | ||
*[[Delta wave]] – slow/slurring in the rise of an initial portion of the QRS | *[[Delta wave]] – slow/slurring in the rise of an initial portion of the QRS | ||
* Widening of QRS complex | *Widening of QRS complex | ||
* ST Segment and T wave discordant changes – i.e. in the opposite direction to the major component of the [[QRS complex]] | *ST Segment and T wave discordant changes – i.e. in the opposite direction to the major component of the [[QRS complex]] | ||
*[[Wolff-Parkinson-White syndrome|WPW]] is mainly categorized as type A or B. | *[[Wolff-Parkinson-White syndrome|WPW]] is mainly categorized as type A or B. | ||
** Type A: ''positive delta wave'' in all precordial leads with R/S > 1 in V1 | **Type A: ''positive delta wave'' in all precordial leads with R/S > 1 in V1 | ||
** Type B: ''negative delta wave'' in leads V1 and V2 | **Type B: ''negative delta wave'' in leads V1 and V2 | ||
=== Lown-Ganong-Levine (LGL) Syndrome === | ===Lown-Ganong-Levine (LGL) Syndrome=== | ||
Here the [[Accessory pathway]] are composed of ''James fibers. '' | Here the [[Accessory pathway]] are composed of ''James fibers. '' | ||
ECG features: | ECG features: | ||
* PR interval <120ms | *PR interval <120ms | ||
* Normal [[QRS morphology]] | *Normal [[QRS morphology]] | ||
The important point to be noted is that this tern is not relevant or shouldn't be used in the absence of [[paroxysmal tachycardia]]. Its existence is disputed and it may not exist. | The important point to be noted is that this tern is not relevant or shouldn't be used in the absence of [[paroxysmal tachycardia]]. Its existence is disputed and it may not exist. | ||
=== Mahaim-Type Pre-excitation === | ===Mahaim-Type Pre-excitation=== | ||
Right-sided [[accessory pathways]] connecting either AV node to ventricles, fascicles to ventricles, or atria to fascicles | Right-sided [[accessory pathways]] connecting either AV node to ventricles, fascicles to ventricles, or atria to fascicles | ||
ECG features: | ECG features: | ||
* Sinus rhythm [[ECG]] may be normal | *Sinus rhythm [[ECG]] may be normal | ||
* May result in variation in ventricular morphology | *May result in variation in ventricular morphology | ||
* Reentry tachycardia typically has [[Left bundle branch block|LBBB morpholog]]<nowiki/>y | *Reentry tachycardia typically has [[Left bundle branch block|LBBB morpholog]]<nowiki/>y | ||
[[File:Basics of pre ex.jpg|thumb | [[File:Basics of pre ex.jpg|thumb|Basics of Pre excitation sydrome]] | ||
== Pathophysiology == | ==Pathophysiology== | ||
* Pathophysiology of Pre-Excitation syndrome | *Pathophysiology of Pre-Excitation syndrome | ||
**[[Pre-excitation of the ventricles|Pre-excitation]] refers to the early activation of the ventricles as a result of impulses bypassing the AV node via an [[accessory pathway]]. The latter are abnormal conduction pathways formed during cardiac development. These can conduct impulses either | **[[Pre-excitation of the ventricles|Pre-excitation]] refers to the early activation of the ventricles as a result of impulses bypassing the AV node via an [[accessory pathway]]. The latter are abnormal conduction pathways formed during cardiac development. These can conduct impulses either | ||
***towards ventricles ([[Anterograde conduction]], rarely seen) , | ***towards ventricles ([[Anterograde conduction]], rarely seen) , | ||
| Line 88: | Line 88: | ||
**The accessory pathways facilitate the formation of [[Tachyarrhythmias]] by mainly forming a reentry circuit, termed as <u>AVRT</u> (80%). Even in cases of direct conduction through the accessory pathways from A to V ( Bypassing AV node), there can be the resultant formation of [[Tachyarrhythmia|Tachyarrhythmias]], seen most frequently in the condition of A. Fib with RVR. | **The accessory pathways facilitate the formation of [[Tachyarrhythmias]] by mainly forming a reentry circuit, termed as <u>AVRT</u> (80%). Even in cases of direct conduction through the accessory pathways from A to V ( Bypassing AV node), there can be the resultant formation of [[Tachyarrhythmia|Tachyarrhythmias]], seen most frequently in the condition of A. Fib with RVR. | ||
== Differentiating Pre-excitation Syndrome from other Diseases == | ==Differentiating Pre-excitation Syndrome from other Diseases== | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Arrhythmia}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Arrhythmia}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Rhythm}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Rhythm}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Rate}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Rate}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|P wave}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|P wave}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|PR Interval}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|PR Interval}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|QRS Complex}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|QRS Complex}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Response to Maneuvers}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Response to Maneuvers}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Epidemiology}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Epidemiology}} | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Co-existing Conditions}} | ! style="background: #4479BA; width: 200px;" |{{fontcolor|#FFF|Co-existing Conditions}} | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Atrial fibrillation|Atrial Fibrillation]] (AFib) | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Atrial fibrillation|Atrial Fibrillation]] (AFib) | ||
| | | | ||
* Irregularly irregular | *Irregularly irregular | ||
| | | | ||
* On a 10-second 12-lead [[The electrocardiogram|EKG]] strip, multiply number of [[QRS complexes]] by 6 | *On a 10-second 12-lead [[The electrocardiogram|EKG]] strip, multiply number of [[QRS complexes]] by 6 | ||
| | | | ||
* Absent | *Absent | ||
* Fibrillatory waves | *Fibrillatory waves | ||
| | | | ||
* Absent | *Absent | ||
| | | | ||
* Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | *Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | ||
| | | | ||
* Does not break with [[adenosine]] or [[vagal maneuvers]] | *Does not break with [[adenosine]] or [[vagal maneuvers]] | ||
| | | | ||
* 2.7–6.1 million people in the United States have AFib | *2.7–6.1 million people in the United States have AFib | ||
* 2% of people younger than age 65 have AFib, while about 9% of people aged 65 years or older have AFib | *2% of people younger than age 65 have AFib, while about 9% of people aged 65 years or older have AFib | ||
| | | | ||
* Elderly | *Elderly | ||
* Following [[Coronary artery bypass surgery|bypass surgery]] | *Following [[Coronary artery bypass surgery|bypass surgery]] | ||
*[[Mitral valve disease]] | *[[Mitral valve disease]] | ||
*[[Hyperthyroidism]] | *[[Hyperthyroidism]] | ||
| Line 128: | Line 128: | ||
*[[Ischemic heart disease]] | *[[Ischemic heart disease]] | ||
*[[Chronic kidney disease]] | *[[Chronic kidney disease]] | ||
* Heavy [[alcohol]] use | *Heavy [[alcohol]] use | ||
* Left chamber enlargement | *Left chamber enlargement | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Atrial Flutter]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Atrial Flutter]]''' | ||
| | | | ||
* Regular or Irregular | *Regular or Irregular | ||
| | | | ||
* 75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) beats per minute (bpm), but 150 is more common | *75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) beats per minute (bpm), but 150 is more common | ||
| | | | ||
* Sawtooth pattern of P waves at 250 to 350 bpm | *Sawtooth pattern of P waves at 250 to 350 bpm | ||
* Biphasic deflection in V1 | *Biphasic deflection in V1 | ||
| | | | ||
* Varies depending upon the magnitude of the block, but is short | *Varies depending upon the magnitude of the block, but is short | ||
| | | | ||
* Less than 0.12 seconds, consistent, and normal in morphology | *Less than 0.12 seconds, consistent, and normal in morphology | ||
| | | | ||
* Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm | *Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm | ||
| | | | ||
*[[Incidence]]: 88 per 100,000 individuals | *[[Incidence]]: 88 per 100,000 individuals | ||
| Line 151: | Line 151: | ||
*[[Alcohol]] | *[[Alcohol]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Atrioventricular nodal reentry tachycardia]] ([[AV nodal reentrant tachycardia|AVNRT]])''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Atrioventricular nodal reentry tachycardia]] ([[AV nodal reentrant tachycardia|AVNRT]])''''''''' | ||
| | | | ||
* Regular | *Regular | ||
| | | | ||
* 140-280 bpm | *140-280 bpm | ||
| | | | ||
* slow-fast AVNRT: | *slow-fast AVNRT: | ||
** Pseudo-S wave in leads II, III, and AVF | **Pseudo-S wave in leads II, III, and AVF | ||
** Pseudo-R' in lead V1. | **Pseudo-R' in lead V1. | ||
* Fast-Slow AVNRT | *Fast-Slow AVNRT | ||
**[[P waves]] between the [[QRS complex|QRS]] and [[T waves]] (QRS-P-T complexes) | **[[P waves]] between the [[QRS complex|QRS]] and [[T waves]] (QRS-P-T complexes) | ||
* Slow-Slow AVNRT | *Slow-Slow AVNRT | ||
** Late [[P waves]] after a [[QRS complex|QRS]] | **Late [[P waves]] after a [[QRS complex|QRS]] | ||
** Often appears as [[atrial tachycardia]]. | **Often appears as [[atrial tachycardia]]. | ||
* Inverted, superimposed on or buried within the [[QRS complex]] (pseudo R prime in V1/pseudo S wave in inferior leads) | *Inverted, superimposed on or buried within the [[QRS complex]] (pseudo R prime in V1/pseudo S wave in inferior leads) | ||
| | | | ||
* Absent ([[P wave]] can appear after the QRS complex and before the T wave, and in atypical AVNRT, the [[P wave]] can appear just before the [[QRS complex]]) | *Absent ([[P wave]] can appear after the QRS complex and before the T wave, and in atypical AVNRT, the [[P wave]] can appear just before the [[QRS complex]]) | ||
| | | | ||
* Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | *Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | ||
*[[QRS complex alternans|QRS alternans]] may be present | *[[QRS complex alternans|QRS alternans]] may be present | ||
| | | | ||
* May break with [[adenosine]] or [[vagal maneuvers]] | *May break with [[adenosine]] or [[vagal maneuvers]] | ||
| | | | ||
* 60%-70% of all [[supraventricular tachycardias]] | *60%-70% of all [[supraventricular tachycardias]] | ||
| | | | ||
*[[Structural heart disease]] | *[[Structural heart disease]] | ||
*[[Atrial tachyarrhythmias]] | *[[Atrial tachyarrhythmias]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Multifocal atrial tachycardia|Multifocal Atrial Tachycardia]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Multifocal atrial tachycardia|Multifocal Atrial Tachycardia]] | ||
| | | | ||
* Irregular | *Irregular | ||
| | | | ||
*[[Atrial]] rate is > 100 beats per minute | *[[Atrial]] rate is > 100 beats per minute | ||
| | | | ||
* Varying morphology from at least three different foci | *Varying morphology from at least three different foci | ||
* Absence of one dominant atrial pacemaker, can be mistaken for [[atrial fibrillation]] if the [[P waves]] are of low amplitude | *Absence of one dominant atrial pacemaker, can be mistaken for [[atrial fibrillation]] if the [[P waves]] are of low amplitude | ||
| | | | ||
* Variable [[PR interval|PR intervals]], RR intervals, and PP intervals | *Variable [[PR interval|PR intervals]], RR intervals, and PP intervals | ||
| | | | ||
* Less than 0.12 seconds, consistent, and normal in morphology | *Less than 0.12 seconds, consistent, and normal in morphology | ||
| | | | ||
* Does not terminate with [[adenosine]] or [[vagal maneuvers]] | *Does not terminate with [[adenosine]] or [[vagal maneuvers]] | ||
| | | | ||
* 0.05% to 0.32% of [[electrocardiograms]] in general hospital admissions | *0.05% to 0.32% of [[electrocardiograms]] in general hospital admissions | ||
| | | | ||
*[[Elderly]] | *[[Elderly]] | ||
*[[Chronic obstructive pulmonary disease]] ([[Chronic obstructive pulmonary disease|COPD]]) | *[[Chronic obstructive pulmonary disease]] ([[Chronic obstructive pulmonary disease|COPD]]) | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Paroxysmal supraventricular tachycardia|Paroxysmal Supraventricular Tachycardia]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Paroxysmal supraventricular tachycardia|Paroxysmal Supraventricular Tachycardia]]''' | ||
| | | | ||
* Regular | *Regular | ||
| | | | ||
* 150 and 240 bpm | *150 and 240 bpm | ||
| | | | ||
* Absent | *Absent | ||
* Hidden in [[QRS complex|QRS]] | *Hidden in [[QRS complex|QRS]] | ||
| | | | ||
* Absent | *Absent | ||
| | | | ||
* Narrow complexes (< 0.12 s) | *Narrow complexes (< 0.12 s) | ||
| | | | ||
* Breaks with [[vagal maneuvers]], [[adenosine]], [[diving reflex]], [[oculocardiac reflex]] | *Breaks with [[vagal maneuvers]], [[adenosine]], [[diving reflex]], [[oculocardiac reflex]] | ||
| | | | ||
*[[Prevalence]]: 0.023 per 100,000 | *[[Prevalence]]: 0.023 per 100,000 | ||
| Line 220: | Line 220: | ||
*[[Nicotine]] | *[[Nicotine]] | ||
*[[Psychological stress]] | *[[Psychological stress]] | ||
*[[Wolff-Parkinson-White syndrome]] | *[[Wolff-Parkinson-White syndrome]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Premature atrial contraction|Premature Atrial Contractrions]] ([[Premature atrial contraction|PAC]])''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Premature atrial contraction|Premature Atrial Contractrions]] ([[Premature atrial contraction|PAC]])''' | ||
| | | | ||
* Regular except when disturbed by premature beat(s) | *Regular except when disturbed by premature beat(s) | ||
| | | | ||
* 80-120 bpm | *80-120 bpm | ||
| | | | ||
* Upright | *Upright | ||
| | | | ||
* > 0.12 second | *> 0.12 second | ||
* Maybe shorter than that in normal sinus rhythm (NSR) if the origin of PAC is located closer to the AV node | *Maybe shorter than that in normal sinus rhythm (NSR) if the origin of PAC is located closer to the AV node | ||
* Ashman’s Phenomenon: | *Ashman’s Phenomenon: | ||
**[[Premature atrial contraction|PAC]] displaying a [[right bundle branch block]] pattern | **[[Premature atrial contraction|PAC]] displaying a [[right bundle branch block]] pattern | ||
| | | | ||
* Usually narrow (< 0.12 s) | *Usually narrow (< 0.12 s) | ||
| | | | ||
* Breaks with [[vagal maneuvers]], [[adenosine]], [[diving reflex]], [[oculocardiac reflex]] | *Breaks with [[vagal maneuvers]], [[adenosine]], [[diving reflex]], [[oculocardiac reflex]] | ||
| | | | ||
| | | | ||
| Line 246: | Line 246: | ||
*[[Coronary artery disease]] | *[[Coronary artery disease]] | ||
*[[Stroke]] | *[[Stroke]] | ||
* Increased [[atrial natriuretic peptide]] ([[Atrial natriuretic peptide|ANP]]) | *Increased [[atrial natriuretic peptide]] ([[Atrial natriuretic peptide|ANP]]) | ||
*[[Hypercholesterolemia]] | *[[Hypercholesterolemia]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wolff-Parkinson-White syndrome|Wolff-Parkinson-White Syndrome]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wolff-Parkinson-White syndrome|Wolff-Parkinson-White Syndrome]] | ||
| | | | ||
| | | | ||
* Regular | *Regular | ||
| | | | ||
* Atrial rate is nearly 300 bpm and the ventricular rate is at 150 bpm | *Atrial rate is nearly 300 bpm and the ventricular rate is at 150 bpm | ||
| | | | ||
* With [[orthodromic]] conduction due to a bypass tract, the [[P wave]] generally follows the [[QRS complex]], whereas in [[AVNRT]], the [[P wave]] is generally buried in the [[QRS complex]]. | *With [[orthodromic]] conduction due to a bypass tract, the [[P wave]] generally follows the [[QRS complex]], whereas in [[AVNRT]], the [[P wave]] is generally buried in the [[QRS complex]]. | ||
| | | | ||
* Less than 0.12 seconds | *Less than 0.12 seconds | ||
| | | | ||
* A [[delta wave]] and evidence of [[ventricular]] pre-excitation if there is conduction to the ventricle via ante-grade conduction down an accessory pathway | *A [[delta wave]] and evidence of [[ventricular]] pre-excitation if there is conduction to the ventricle via ante-grade conduction down an accessory pathway | ||
* A [[delta wave]] and pre-excitation may not be present because bypass tracts do not conduct ante-grade. | *A [[delta wave]] and pre-excitation may not be present because bypass tracts do not conduct ante-grade. | ||
| | | | ||
* May break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | *May break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | ||
| | | | ||
* Worldwide [[prevalence]] of [[Wolff-Parkinson-White syndrome|WPW syndrome]] is 100 - 300 per 100,000 | *Worldwide [[prevalence]] of [[Wolff-Parkinson-White syndrome|WPW syndrome]] is 100 - 300 per 100,000 | ||
| | | | ||
*[[Ebstein's anomaly]] | *[[Ebstein's anomaly]] | ||
| Line 274: | Line 274: | ||
*[[Tuberous sclerosis]] | *[[Tuberous sclerosis]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Ventricular fibrillation|Ventricular Fibrillation]] (VF)''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Ventricular fibrillation|Ventricular Fibrillation]] (VF)''' | ||
| | | | ||
* Irregular | *Irregular | ||
| | | | ||
* 150 to 500 bpm | *150 to 500 bpm | ||
| | | | ||
* Absent | *Absent | ||
| | | | ||
* Absent | *Absent | ||
| | | | ||
* Absent (R on T phenomenon in the setting of ischemia) | *Absent (R on T phenomenon in the setting of ischemia) | ||
| | | | ||
* Does not break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | *Does not break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | ||
| | | | ||
* 3-12% cases of [[acute myocardial infarction]] (AMI) | *3-12% cases of [[acute myocardial infarction]] (AMI) | ||
* Out of 356,500 out of hospital cardiac arrests, 23% have VF as initial rhythm | *Out of 356,500 out of hospital cardiac arrests, 23% have VF as initial rhythm | ||
| | | | ||
*[[Myocardial ischemia]] / [[Myocardial infarction|infarction]] | *[[Myocardial ischemia]] / [[Myocardial infarction|infarction]] | ||
*[[Cardiomyopathy]] | *[[Cardiomyopathy]] | ||
* Channelopathies e.g. Long QT (acquired / congenital) | *Channelopathies e.g. Long QT (acquired / congenital) | ||
* Electrolyte abnormalities ([[hypokalemia]]/[[hyperkalemia]], [[hypomagnesemia]]) | *Electrolyte abnormalities ([[hypokalemia]]/[[hyperkalemia]], [[hypomagnesemia]]) | ||
*[[Aortic stenosis]] | *[[Aortic stenosis]] | ||
*[[Aortic dissection]] | *[[Aortic dissection]] | ||
*[[Myocarditis]] | *[[Myocarditis]] | ||
*[[Cardiac tamponade]] | *[[Cardiac tamponade]] | ||
* Blunt trauma (Commotio Cordis) | *Blunt trauma (Commotio Cordis) | ||
*[[Sepsis]] | *[[Sepsis]] | ||
*[[Hypothermia]] | *[[Hypothermia]] | ||
| Line 306: | Line 306: | ||
*[[Stroke]] | *[[Stroke]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Ventricular tachycardia|Ventricular Tachycardia]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Ventricular tachycardia|Ventricular Tachycardia]]''' | ||
| | | | ||
* Regular | *Regular | ||
| | | | ||
* > 100 bpm (150-200 bpm common) | *> 100 bpm (150-200 bpm common) | ||
| | | | ||
* Absent | *Absent | ||
| | | | ||
* Absent | *Absent | ||
* Initial [[R wave]] in V1, initial r > 40 ms in V1/V2, notched S in V1, initial R in aVR, lead II R wave peak time ≥50 ms, no RS in V1-V6, and atrioventricular dissociation | *Initial [[R wave]] in V1, initial r > 40 ms in V1/V2, notched S in V1, initial R in aVR, lead II R wave peak time ≥50 ms, no RS in V1-V6, and atrioventricular dissociation | ||
| | | | ||
* Wide complex, [[QRS complex|QRS]] duration > 120 milliseconds | *Wide complex, [[QRS complex|QRS]] duration > 120 milliseconds | ||
| | | | ||
* Does not break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | *Does not break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]] | ||
| | | | ||
* 5-10% of patients presenting with AMI | *5-10% of patients presenting with AMI | ||
| | | | ||
*[[Coronary artery disease]] | *[[Coronary artery disease]] | ||
| Line 328: | Line 328: | ||
*[[Cardiomyopathy]] | *[[Cardiomyopathy]] | ||
*[[Electrolyte imbalance|Electrolyte imbalances]] (e.g., [[hypokalemia]], [[hypomagnesemia]]) | *[[Electrolyte imbalance|Electrolyte imbalances]] (e.g., [[hypokalemia]], [[hypomagnesemia]]) | ||
* Inherited [[channelopathies]] (e.g., [[long-QT syndrome]]) | *Inherited [[channelopathies]] (e.g., [[long-QT syndrome]]) | ||
*[[Catecholaminergic polymorphic ventricular tachycardia]] | *[[Catecholaminergic polymorphic ventricular tachycardia]] | ||
*[[Arrhythmogenic right ventricular dysplasia]] | *[[Arrhythmogenic right ventricular dysplasia]] | ||
| Line 335: | Line 335: | ||
|} | |} | ||
== Epidemiology and Demographics == | ==Epidemiology and Demographics== | ||
*Incidence 0.1 – 3.0 per 1000 | *Incidence 0.1 – 3.0 per 1000 | ||
| Line 341: | Line 341: | ||
*prognosis is good with [[SCD]] is noted in only 0.1% (rare)<br /> | *prognosis is good with [[SCD]] is noted in only 0.1% (rare)<br /> | ||
== Risk Factors == | ==Risk Factors== | ||
High risk population for [[sudden cardiac death]] in [[Wolff-Parkinson-White syndrome]] include: | High risk population for [[sudden cardiac death]] in [[Wolff-Parkinson-White syndrome]] include: | ||
* Policemen | *Policemen | ||
* Athletes | *Athletes | ||
* Firemen | *Firemen | ||
* Pilots | *Pilots | ||
* Steelworkers | *Steelworkers | ||
Risk factors for the development of [[atrial fibrillation]] in WPW syndrome include: | Risk factors for the development of [[atrial fibrillation]] in WPW syndrome include: | ||
* Male gender | *Male gender | ||
* Age (peak ages for the development of atrial fibrillation include 30 years and 50 years) | *Age (peak ages for the development of atrial fibrillation include 30 years and 50 years) | ||
* Past history of [[syncope]] | *Past history of [[syncope]] | ||
<br /> | <br /> | ||
== Natural History, Complications and Prognosis == | ==Natural History, Complications and Prognosis== | ||
* The majority of patients with [disease name] remain asymptomatic for [duration/years]. | *The majority of patients with [disease name] remain asymptomatic for [duration/years]. | ||
* Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3]. | *Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3]. | ||
* If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3]. | *If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3]. | ||
* Common complications of [disease name] include [complication 1], [complication 2], and [complication 3]. | *Common complications of [disease name] include [complication 1], [complication 2], and [complication 3]. | ||
* Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%]. | *Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%]. | ||
<br /> | <br /> | ||
== Diagnosis == | ==Diagnosis== | ||
====<u>[[Atrioventricular (AV) reentrant tachycardia|Atrioventricular Reentry Tachycardia's (AVRT)]]</u>==== | ====<u>[[Atrioventricular (AV) reentrant tachycardia|Atrioventricular Reentry Tachycardia's (AVRT)]]</u>==== | ||
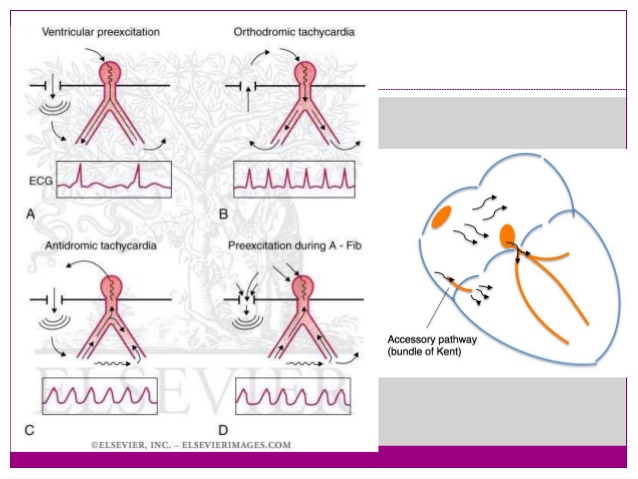
[[File:Orth.gif|thumb|AVRT ( Orthodromic and Antidromic) | [[File:Orth.gif|thumb|AVRT ( Orthodromic and Antidromic)]]AVRT is a form of PSVT. Reentry circuit results from the combination of signal transduction from normal conduction system and [[accessory pathway]].( See: Diagram) | ||
* During tachyarrythmias, the [[accessory pathway]] forms part of the reentry circuit that results in the disappearance of features of tachyarrhythmias. | *During tachyarrythmias, the [[accessory pathway]] forms part of the reentry circuit that results in the disappearance of features of tachyarrhythmias. | ||
*[[AV reentrant tachycardia|AVRT]] are further divided into | *[[AV reentrant tachycardia|AVRT]] are further divided into | ||
** Orthodromic or Antidromic conduction based on ECG morphology and direction of formation of re-entry circuit. | **Orthodromic or Antidromic conduction based on ECG morphology and direction of formation of re-entry circuit. | ||
=== History and Symptoms === | ===History and Symptoms=== | ||
People with Pre- Excitation syndromes may be asymptomatic, however, the individual may experience following symptoms | People with Pre- Excitation syndromes may be asymptomatic, however, the individual may experience following symptoms | ||
| Line 383: | Line 383: | ||
*[[Dyspnea|'''Shortness of breath'''.]] | *[[Dyspnea|'''Shortness of breath'''.]] | ||
*[[Chest pain]] | *[[Chest pain]] | ||
* Fatigue. | *Fatigue. | ||
*[[Anxiety]]. | *[[Anxiety]]. | ||
* Fainting | *Fainting | ||
* Difficulty breathing | *Difficulty breathing | ||
====== 1) AVRT with Orthodromic Conduction ====== | ======1) AVRT with Orthodromic Conduction====== | ||
In this, the anterograde conduction occurs via the [[AV node]] and retrograde conduction occurs via an accessory pathway. | In this, the anterograde conduction occurs via the [[AV node]] and retrograde conduction occurs via an accessory pathway. | ||
ECG features of [[AV reentrant tachycardia|AVRT]] with orthodromic conduction | ECG features of [[AV reentrant tachycardia|AVRT]] with orthodromic conduction | ||
* Rate usually 200 – 300 bpm | *Rate usually 200 – 300 bpm | ||
* P waves may be buried in QRS complex or retrograde | *P waves may be buried in QRS complex or retrograde | ||
* QRS Complex usually <120 ms unless pre-existing bundle branch block, or rate-related aberrant conduction | *QRS Complex usually <120 ms unless pre-existing bundle branch block, or rate-related aberrant conduction | ||
*[[QRS complex alternans|QRS Alternans]] – phasic variation in QRS amplitude associated with AVNRT and AVRT, distinguished from electrical altrens by a normal QRS amplitude | *[[QRS complex alternans|QRS Alternans]] – phasic variation in QRS amplitude associated with AVNRT and AVRT, distinguished from electrical altrens by a normal QRS amplitude | ||
* T wave inversion common | *T wave inversion common | ||
*[[ST segment depression]] | *[[ST segment depression]] | ||
<br /> | <br /> | ||
==== 2) AVRT with Antidromic Conduction ==== | ====2) AVRT with Antidromic Conduction==== | ||
In this, the anterograde conduction occurs via the accessory pathway and retrograde conduction via the AV node. Occurring only in-app. 5% of patients with WPW. | In this, the anterograde conduction occurs via the accessory pathway and retrograde conduction via the AV node. Occurring only in-app. 5% of patients with WPW. | ||
ECG features are: | ECG features are: | ||
* Rate usually 200 – 300 bpm. | *Rate usually 200 – 300 bpm. | ||
*[[Wide QRS complexes]] due to abnormal accessory pathway ventricular depolarisation. | *[[Wide QRS complexes]] due to abnormal accessory pathway ventricular depolarisation. | ||
*Due to wide complex, Commonly mistaken for [[Ventricular tachycardia|Ventricular Tachycardia.]] | *Due to wide complex, Commonly mistaken for [[Ventricular tachycardia|Ventricular Tachycardia.]] | ||
<br /> | <br /> | ||
==== 3) Atrial Fib/Atrial Flutter in WPW ==== | ====3) Atrial Fib/Atrial Flutter in WPW==== | ||
* In 20% of the patients WPW Atrial fibrillation can occur and in approx 7% of patients with [[Wolff-Parkinson-White syndrome|WPW]] [[atrial flutter]] can occur. Accessory pathways plays major role by allowing the rapid conduction of impulses directly to the ventricles without involving [[Atrioventricular node|AV node]], in extreme cases may lead to VT or VF. | *In 20% of the patients WPW Atrial fibrillation can occur and in approx 7% of patients with [[Wolff-Parkinson-White syndrome|WPW]] [[atrial flutter]] can occur. Accessory pathways plays major role by allowing the rapid conduction of impulses directly to the ventricles without involving [[Atrioventricular node|AV node]], in extreme cases may lead to VT or VF. | ||
ECG features are: | ECG features are: | ||
* Rate > 200 bpm | *Rate > 200 bpm | ||
*[[Irregular rhythm]] | *[[Irregular rhythm]] | ||
* Wide QRS complexes due to abnormal ventricular depolarisation via an accessory pathway | *Wide QRS complexes due to abnormal ventricular depolarisation via an accessory pathway | ||
* QRS Complexes change in shape and morphology | *QRS Complexes change in shape and morphology | ||
* Axis remains stable unlike [[Ventricular tachycardia classification|Polymorphic VT]] | *Axis remains stable unlike [[Ventricular tachycardia classification|Polymorphic VT]] | ||
*[[Atrial flutter|Atrial Flutter]] presents with same features as atrial fibrillation in WPW except rhythm is regular and commonly mistaken for VT | *[[Atrial flutter|Atrial Flutter]] presents with same features as atrial fibrillation in WPW except rhythm is regular and commonly mistaken for VT | ||
<br /> | <br /> | ||
== Treatment == | ==Treatment== | ||
=== Medical Treatment | ===Medical Treatment=== | ||
==== Orthodromic AVRT ==== | ====Orthodromic AVRT==== | ||
* Hemodynamically Unstable patients (Low BP, Altered mental state, pulmonary edema)- Synchronized DC Cardioversion. | *Hemodynamically Unstable patients (Low BP, Altered mental state, pulmonary edema)- Synchronized DC Cardioversion. | ||
* Hemodynamically stable- Vagal maneuvers, Adenosine, CCB, and DC cardioversion as a last resort only if the patient not responding to medical therapy. | *Hemodynamically stable- Vagal maneuvers, Adenosine, CCB, and DC cardioversion as a last resort only if the patient not responding to medical therapy. | ||
===== Antidromic AVRT ===== | =====Antidromic AVRT===== | ||
* Hemodynamically unstable patients:- Urgent synchronized DC cardioversion. | *Hemodynamically unstable patients:- Urgent synchronized DC cardioversion. | ||
* Hemodynamically stable patients:- Amiodarone, procainamide, or ibutilide. | *Hemodynamically stable patients:- Amiodarone, procainamide, or ibutilide. | ||
====== AF with WPW ====== | ======AF with WPW====== | ||
* Hemodynamically unstable patients: Urgent synchronized DC cardioversion | *Hemodynamically unstable patients: Urgent synchronized DC cardioversion | ||
* Hemodynamically stable patients:- Procainamide or ibutilide. | *Hemodynamically stable patients:- Procainamide or ibutilide. | ||
* <u>'''Caution''':</u> Adenosine, CCB, Beta blockers enhances conduction via accessory pathway resulting in worsening & possible degeneration into VT or VF | *<u>'''Caution''':</u> Adenosine, CCB, Beta blockers enhances conduction via accessory pathway resulting in worsening & possible degeneration into VT or VF | ||
=== Surgery === | ===Surgery=== | ||
* Surgery is the mainstay of therapy for [disease name]. | *Surgery is the mainstay of therapy for [disease name]. | ||
* [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name]. | *[Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name]. | ||
* [Surgical procedure] can only be performed for patients with [disease stage] [disease name]. | *[Surgical procedure] can only be performed for patients with [disease stage] [disease name]. | ||
<br /> | <br /> | ||
== Prevention == | ==Prevention== | ||
For preventing the recurrence of episodes major options available are | For preventing the recurrence of episodes major options available are | ||
*[[Radiofrequency ablation|Radio frequency ablation]] | *[[Radiofrequency ablation|Radio frequency ablation]] | ||
** Ablation of [[Accessory pathway|accessory pathway tracts]] | **Ablation of [[Accessory pathway|accessory pathway tracts]] | ||
** cures 95% of the time | **cures 95% of the time | ||
* Surgery. | *Surgery. | ||
** Success rate for surgical ablation is around 100 percent along with lower complication rates. Radiofrequency ablation is a less invasive option and preferred over surgery. | **Success rate for surgical ablation is around 100 percent along with lower complication rates. Radiofrequency ablation is a less invasive option and preferred over surgery. | ||
** Surgery can be considered if a patient is undergoing cardiac surgery for other reasons such as [[Coronary artery bypass surgery|CABG]] or other heart valve surgery. | **Surgery can be considered if a patient is undergoing cardiac surgery for other reasons such as [[Coronary artery bypass surgery|CABG]] or other heart valve surgery. | ||
* Medications | *Medications | ||
** Although Medications can prevent recurrent episodes of tachycardia they are only used on patients who are not the candidates for ablation or surgery. | **Although Medications can prevent recurrent episodes of tachycardia they are only used on patients who are not the candidates for ablation or surgery. | ||
** These patients must be taught to perform Valsalva maneuvers that can relieve tachycardia during the episodes.<br /> | **These patients must be taught to perform Valsalva maneuvers that can relieve tachycardia during the episodes.<br /> | ||
== References == | ==References== | ||
<references /> | <references /> | ||
Revision as of 01:56, 25 August 2020
|
Pre-excitation syndrome Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor-In-Chief: Shivam Singla, M.D.[2]
Overview
Pre-excitation syndrome is a condition where ventricles of the heart depolarize earlier than the normal leading to the premature contraction.. Normally the atria and the ventricles are isolated electrically and only electrical passage existing in between atria and ventricles is at Atrioventricular Node. In all pre-excitation syndromes there is also present an additional conducting pathway besides the AV junction. So the electrical impulses passes to the ventricles even before the normal wave of depolarization that is about to conduct through AV node. This mechanism of depolarization of ventricles through additional by pass pathway much earlier than the usual depolarization pathway (through AV node) is referred to as "Pre- Excitation". The secondary conduction pathways are generally named as Bundle of His.
Historical Perspective
- In 1930, it was first described by Louis Wolff, John Parkinson, and Paul Dudley White. They found the association of these conditions with a small risk of sudden cardiac death.
Classification
- Pre-excitation syndrome may be classified into sub-types
| Type | Conduction pathway | PR interval | QRS interval | Delta wave |
|---|---|---|---|---|
| Wolff-Parkinson-White syndrome | Bundle of Kent (atria to ventricles) | short | long | yes |
| Lown-Ganong-Levine syndrome | "James bundle" (atria to bundle of His) | short | normal | no |
| Mahaim-type | Mahaim fibers | normal | long |
WPW Syndrome
WPW is a combination of the presence of congenital accessory pathways along with episodic tachyarrhythmias. Here the accessory pathways are referred to as Bundle of Kent or AV bypass tracts.
The features of pre-excitation are subtle, intermittent, and are aggravated by an increase in vagal tone ( Valsalva maneuver, AV blockage by drugs).
ECG Features of WPW
- Shortened PR interval (Less than 120ms)
- Delta wave – slow/slurring in the rise of an initial portion of the QRS
- Widening of QRS complex
- ST Segment and T wave discordant changes – i.e. in the opposite direction to the major component of the QRS complex
- WPW is mainly categorized as type A or B.
- Type A: positive delta wave in all precordial leads with R/S > 1 in V1
- Type B: negative delta wave in leads V1 and V2
Lown-Ganong-Levine (LGL) Syndrome
Here the Accessory pathway are composed of James fibers.
ECG features:
- PR interval <120ms
- Normal QRS morphology
The important point to be noted is that this tern is not relevant or shouldn't be used in the absence of paroxysmal tachycardia. Its existence is disputed and it may not exist.
Mahaim-Type Pre-excitation
Right-sided accessory pathways connecting either AV node to ventricles, fascicles to ventricles, or atria to fascicles
ECG features:
- Sinus rhythm ECG may be normal
- May result in variation in ventricular morphology
- Reentry tachycardia typically has LBBB morphology
Pathophysiology
- Pathophysiology of Pre-Excitation syndrome
- Pre-excitation refers to the early activation of the ventricles as a result of impulses bypassing the AV node via an accessory pathway. The latter are abnormal conduction pathways formed during cardiac development. These can conduct impulses either
- towards ventricles (Anterograde conduction, rarely seen) ,
- Away from the ventricles (Retrograde conduction, in approx 15%),
- in both the directions ( Majority of cases).
- In WPW syndrome which is a type of pre-excitation syndrome the abnormal conduction pathways are called Bundle of Kent or AV bypass tract.
- The accessory pathways facilitate the formation of Tachyarrhythmias by mainly forming a reentry circuit, termed as AVRT (80%). Even in cases of direct conduction through the accessory pathways from A to V ( Bypassing AV node), there can be the resultant formation of Tachyarrhythmias, seen most frequently in the condition of A. Fib with RVR.
- Pre-excitation refers to the early activation of the ventricles as a result of impulses bypassing the AV node via an accessory pathway. The latter are abnormal conduction pathways formed during cardiac development. These can conduct impulses either
Differentiating Pre-excitation Syndrome from other Diseases
| Arrhythmia | Rhythm | Rate | P wave | PR Interval | QRS Complex | Response to Maneuvers | Epidemiology | Co-existing Conditions | |
|---|---|---|---|---|---|---|---|---|---|
| Atrial Fibrillation (AFib) |
|
|
|
|
|
|
|
| |
| Atrial Flutter |
|
|
|
|
|
|
|
||
| Atrioventricular nodal reentry tachycardia (AVNRT)'''' |
|
|
|
|
|
|
|
||
| Multifocal Atrial Tachycardia |
|
|
|
|
|
|
|
||
| Paroxysmal Supraventricular Tachycardia |
|
|
|
|
|
|
|
||
| Premature Atrial Contractrions (PAC) |
|
|
|
|
|
|
|||
| Wolff-Parkinson-White Syndrome |
|
|
|
|
|
|
|
| |
| Ventricular Fibrillation (VF) |
|
|
|
|
|
|
|
| |
| Ventricular Tachycardia |
|
|
|
|
|
|
|
|
Epidemiology and Demographics
- Incidence 0.1 – 3.0 per 1000
- LGL syndrome is a rare Man > woman.
- prognosis is good with SCD is noted in only 0.1% (rare)
Risk Factors
High risk population for sudden cardiac death in Wolff-Parkinson-White syndrome include:
- Policemen
- Athletes
- Firemen
- Pilots
- Steelworkers
Risk factors for the development of atrial fibrillation in WPW syndrome include:
- Male gender
- Age (peak ages for the development of atrial fibrillation include 30 years and 50 years)
- Past history of syncope
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis
Atrioventricular Reentry Tachycardia's (AVRT)
AVRT is a form of PSVT. Reentry circuit results from the combination of signal transduction from normal conduction system and accessory pathway.( See: Diagram)
- During tachyarrythmias, the accessory pathway forms part of the reentry circuit that results in the disappearance of features of tachyarrhythmias.
- AVRT are further divided into
- Orthodromic or Antidromic conduction based on ECG morphology and direction of formation of re-entry circuit.
History and Symptoms
People with Pre- Excitation syndromes may be asymptomatic, however, the individual may experience following symptoms
- Palpitations
- Dizziness or lightheadedness.
- Shortness of breath.
- Chest pain
- Fatigue.
- Anxiety.
- Fainting
- Difficulty breathing
1) AVRT with Orthodromic Conduction
In this, the anterograde conduction occurs via the AV node and retrograde conduction occurs via an accessory pathway.
ECG features of AVRT with orthodromic conduction
- Rate usually 200 – 300 bpm
- P waves may be buried in QRS complex or retrograde
- QRS Complex usually <120 ms unless pre-existing bundle branch block, or rate-related aberrant conduction
- QRS Alternans – phasic variation in QRS amplitude associated with AVNRT and AVRT, distinguished from electrical altrens by a normal QRS amplitude
- T wave inversion common
- ST segment depression
2) AVRT with Antidromic Conduction
In this, the anterograde conduction occurs via the accessory pathway and retrograde conduction via the AV node. Occurring only in-app. 5% of patients with WPW.
ECG features are:
- Rate usually 200 – 300 bpm.
- Wide QRS complexes due to abnormal accessory pathway ventricular depolarisation.
- Due to wide complex, Commonly mistaken for Ventricular Tachycardia.
3) Atrial Fib/Atrial Flutter in WPW
- In 20% of the patients WPW Atrial fibrillation can occur and in approx 7% of patients with WPW atrial flutter can occur. Accessory pathways plays major role by allowing the rapid conduction of impulses directly to the ventricles without involving AV node, in extreme cases may lead to VT or VF.
ECG features are:
- Rate > 200 bpm
- Irregular rhythm
- Wide QRS complexes due to abnormal ventricular depolarisation via an accessory pathway
- QRS Complexes change in shape and morphology
- Axis remains stable unlike Polymorphic VT
- Atrial Flutter presents with same features as atrial fibrillation in WPW except rhythm is regular and commonly mistaken for VT
Treatment
Medical Treatment
Orthodromic AVRT
- Hemodynamically Unstable patients (Low BP, Altered mental state, pulmonary edema)- Synchronized DC Cardioversion.
- Hemodynamically stable- Vagal maneuvers, Adenosine, CCB, and DC cardioversion as a last resort only if the patient not responding to medical therapy.
Antidromic AVRT
- Hemodynamically unstable patients:- Urgent synchronized DC cardioversion.
- Hemodynamically stable patients:- Amiodarone, procainamide, or ibutilide.
AF with WPW
- Hemodynamically unstable patients: Urgent synchronized DC cardioversion
- Hemodynamically stable patients:- Procainamide or ibutilide.
- Caution: Adenosine, CCB, Beta blockers enhances conduction via accessory pathway resulting in worsening & possible degeneration into VT or VF
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
For preventing the recurrence of episodes major options available are
- Radio frequency ablation
- Ablation of accessory pathway tracts
- cures 95% of the time
- Surgery.
- Success rate for surgical ablation is around 100 percent along with lower complication rates. Radiofrequency ablation is a less invasive option and preferred over surgery.
- Surgery can be considered if a patient is undergoing cardiac surgery for other reasons such as CABG or other heart valve surgery.
- Medications
- Although Medications can prevent recurrent episodes of tachycardia they are only used on patients who are not the candidates for ablation or surgery.
- These patients must be taught to perform Valsalva maneuvers that can relieve tachycardia during the episodes.