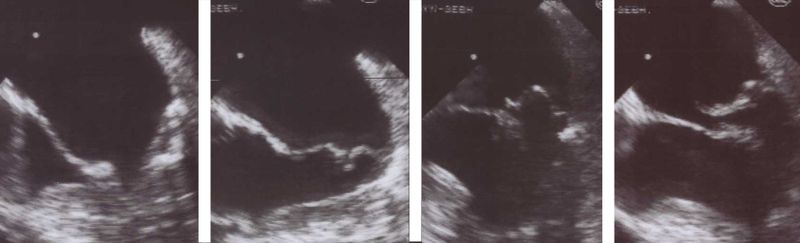
Mitral regurgitation echocardiography
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation echocardiography On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation echocardiography |
|
Risk calculators and risk factors for Mitral regurgitation echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.'; Mohammed A. Sbeih, M.D.[3]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
The echocardiogram is commonly used to confirm the diagnosis of mitral regurgitation. Color doppler flow on the transthoracic echocardiogram (TTE) will reveal a jet of blood flowing from the left ventricle into the left atrium during ventricular systole.
Because of the inability in getting accurate images of the left atrium and the pulmonary veins on the transthoracic echocardiogram, a transesophageal echocardiogram may be necessary to determine the severity of the mitral regurgitation in some cases.
Factors that suggest severe mitral regurgitation on echocardiography include systolic reversal of flow in the pulmonary veins and filling of the entire left atrial cavity by the regurgitant jet of MR.
ACC/AHA Guidelines- Indications for Transthoracic Echocardiography (DO NOT EDIT) [1]
| “ |
Class I1. Transthoracic echocardiography is indicated for baseline evaluation of LV size and function, RV and left atrial size, pulmonary artery pressure, and severity of MR (Table 4) in any patient suspected of having MR. (Level of Evidence: C) 2. Transthoracic echocardiography is indicated for delineation of the mechanism of MR. (Level of Evidence: B) 3. Transthoracic echocardiography is indicated for annual or semiannual surveillance of LV function (estimated by ejection fraction and end-systolic dimension) in asymptomatic patients with moderate to severe MR. (Level of Evidence: C) 4. Transthoracic echocardiography is indicated in patients with MR to evaluate the MV apparatus and LV function after a change in signs or symptoms. (Level of Evidence: C) 5. Transthoracic echocardiography is indicated to evaluate LV size and function and MV hemodynamics in the initial evaluation after MV replacement or MV repair. (Level of Evidence: C) Class IIa1. Exercise Doppler echocardiography is reasonable in asymptomatic patients with severe MR to assess exercise tolerance and the effects of exercise on pulmonary artery pressure and MR severity. (Level of Evidence: C) Class III1. Transthoracic echocardiography is not indicated for routine follow-up evaluation of asymptomatic patients with mild MR and normal LV size and systolic function. (Level of Evidence: C) |
” |
ACC/AHA Guidelines- Indications for Transesophageal Echocardiography (DO NOT EDIT) [1]
| “ |
Class I1. Preoperative or intraoperative transesophageal echocardiography is indicated to establish the anatomic basis for severe MR in patients in whom surgery is recommended to assess feasibility of repair and to guide repair. (Level of Evidence: B) 2. Transesophageal echocardiography is indicated for evaluation of MR patients in whom transthoracic echocardiography provides nondiagnostic information regarding severity of MR, mechanism of MR, and/or status of LV function. (Level of Evidence: B) Class IIa1. Preoperative transesophageal echocardiography is reasonable in asymptomatic patients with severe MR who are considered for surgery to assess feasibility of repair. (Level of Evidence: C) Class III1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve MR. (Level of Evidence: C) |
” |
Aetiology and Morphological Features in 2-D Echocardiography
Rheumatic Mitral Regurgitation
In rheumatic mitral regurgitation, there is some degree of commissural fusion and thickening of the tips visible in 2 dimensional echocardiography. The movement of the valve leaflets is restricted.
Myxomatous Mitral Valve
The leaflets and chordae are thick and reduntant. Reduced tensile strength leads to progressive elongation or rupture of chordae. Ruptured chordae appear as flail segments. To diagnose mitral valve prolapse, the following criteria should be fulfilled during echocardiography - Movement of any part of either leaflet more than 2mm behind the annular plane in parasternal long axis view and movement of point of co-aptation behind the annular plane in apical 4 chamber view.
Annular Calcification
Mitral annulus is usually smaller in systole. The increased rigidity due to annular calcification impairs contraction. In 2D- echocardiography, there is increased echogenicity on the LV side immediately adjacent to the attachment of the posterior mitral valve leaflet. Region of anterior mitral leaflet is only rarely involved. This is common in elderly subjects and younger ones with chronic renal failure and hypertension.
Ischaemic Mitral Regurgitation
Mitral regurgitation can occur in ischemia as a result of regional left ventricular dysfunction with abnormal contraction of papillary muscle or underlying ventricular wall. Myocardial infarction can result in MR at rest while if the underlying cause is ischemia the MR may be intermittent. The echocardiogram is characterized by restricted valve leaflet motion and tenting of mitral valve in systole.
Papillary Muscle Rupture
This is usually a complication of myocardial infarction. If entire papillary muscle is disconnected from the left ventricle severe MR results and few survive. Partial rupture is more common.
Functional Mitral Regurgitation
Functional MR results due to LV dilatation and systolic dysfunction in those with a structurally normal mitral valve apparatus.
 |
- Mitral Ring Dehiscence Post Repair With Severe Mitral Regurgitation
{{#ev:googlevideo|7246533519972889950&hl=en}}
- Severe Mitral Regurgitation From Ring Dehiscence Pulmonary Vein Pulsed Wave Doppler
- Severe Mitral Regurgitation Pulmonary Vein Pulsed Wave Doppler
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [1].
References
- ↑ 1.0 1.1 1.2 Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.