Hyperparathyroidism: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
{{SI}} | {{SI}} | ||
{{GS}} | {{GS}} | ||
'''Editor-in-Chief''': Larry Gordon, M.D. | |||
{{Editor Join}} | {{Editor Join}} | ||
Revision as of 18:23, 8 January 2010
| Hyperparathyroidism | |
 | |
|---|---|
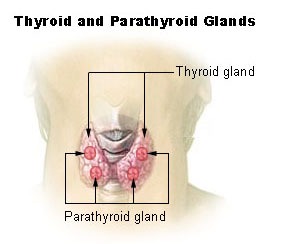
| Thyroid and parathyroid. | |
| ICD-10 | E21 |
| ICD-9 | 252.0 |
| DiseasesDB | 20710 |
| eMedicine | emerg/265 |
| MeSH | D006961 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753 Editor-in-Chief: Larry Gordon, M.D. Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Hyperparathyroidism is overactivity of the parathyroid glands resulting in excess production of parathyroid hormone (PTH). The parathyroid hormone monitors calcium and phosphorus levels and helps to maintain these levels. Overactivity of one or more of the parathyroid glands causes high calcium levels (hypercalcemia) and low levels of phosphorus in the blood [2]. Hyperparathyroidism was first described and treated in the 1930s by Fuller Albright of Massachusetts General Hospital, working at the Mallinckrodt General Clinical Research Center. The oldest known case was found in a cadaver from a Early Neolithic cemetery in southwest Germany.[1]
Classification
Primary hyperparathyroidism
Primary hyperparathyroidism results from a hyperfunction of the parathyroid glands themselves. There is oversecretion of PTH due to adenoma, hyperplasia or, rarely, carcinoma of the parathyroid glands.
Secondary hyperparathyroidism
Secondary hyperparathyroidism is the reaction of the parathyroid glands to a hypocalcemia caused by other than a parathyroid pathology, e.g. chronic renal failure.
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism is a state of excessive secretion of parathyroid hormone (PTH) after a long period of secondary hyperparathyroidism and resulting in hypercalcemia.
Symptoms and signs
Asymptomatic hyperparathyroidism
Many patients presenting with hyperparathyroidism will have no signs or symptoms, with diagnosis being made on further investigation after a coincidental finding of hypercalcemia. It is, however, reported that many patients will report that they feel better after treatment for hyperparathyroidism.
Symptomatic hyperparathyroidism
Of those patients that do present with symptoms, they are commonly associated with the effects of an increased level of calcium. Since calcium is involved in trans-synaptic communication within our nervous system, high blood calcium levels have a direct effect on the nervous system. Thus, most of the symptoms of parathyroid disease are "neurological" in origin. The most common symptom is fatigue and tiredness. Other very common symptoms are lack of energy, memory problems, depression, problems with concentration, and problems sleeping. Other manifestations of hyperparathyroidism usually involve the kidney (stones) and the skeletal system (bone pain due to the development of osteoporosis).
Almost all patients will have symptoms if their calcium is high and the right questions are asked. Removing the parathyroid tumor which is causing the excess parathyroid hormone will eliminate the symptoms in most patients within several days or weeks. Often it is life-changing when the parathyroid tumor is removed.
The symptoms of hyperparathyroidism can be remembered by the rhyme "moans, groans, stones, bones, and psychiatric overtones":
- "moans" (complaints of not feeling well)
- "groans" (abdominal pain, gastroesophageal reflux)
- "stones" (kidney)
- "bones" (bone pain)
- "psychiatric overtones" (lethargy, fatigue, depression, memory problems).
Other symptoms include: headaches, gastroesophageal reflux, decreased sex drive, thinning hair, hypertension, and heart palpitations which are often due to bouts of atrial fibrillation. Additional symptoms reported consist of an increase of thirst and urination as a result of calcium excretion in the urine, stomach ulcers, nausea, and a loss of appetite [3].
Osteoporosis
Unfortunately, medicines are usually not useful for treating the osteoporosis associated with hyperparathyroidism until the parathyroid tumor is removed. Osteoporosis associated with hyperparathyroidism is caused by the high parathyroid hormone that is secreted by the overactive parathyroid gland(s). This excess parathyroid hormone (PTH) acts directly on the bones to remove calcium from the bones. Thus, the high calcium in the blood comes from the bones. Removing the offending parathyroid gland will usually cause a significant improvement in the osteoporosis, often reversing this process back to normal bone density over several years.
Laboratory tests
Serum calcium
In cases of primary, tertiary and quintary hyperparathyroidism increased PTH consequently leads to increased serum calcium (hypercalcemia) due to:
- increased bone resorption, allowing flow of calcium from bone to blood
- reduced renal clearance of calcium
- increased intestinal calcium absorption
By contrast, in secondary and quartary hyperparathyroidism effectiveness of PTHis reduced.
Serum phosphorus
In primary hyperparathyroidism, serum phosphorus levels are abnormally low as a result of decreased renal tubular phosphorus reabsorption. This contrasts with secondary hyperparathyroidism, in which serum phosphorus levels are generally elevated because of renal disease.
Alkaline phosphatase
Alkaline phosphatase levels are elevated in all types of hyperparathyroidism.
Etiology
Primary hyperparathyroidism
- The most common cause is a benign parathyroid adenoma that loses its sensitivity to circulating calcium levels. Usually, only one of the four parathyroid glands is affected.
- A less common cause is from multiple endocrine neoplasia (MEN).
Secondary hyperparathyroidism
Secondary hyperparathyroidism is due to resistance to the actions of PTH, usually due to chronic renal failure. The bone disease in secondary parathyroidism along with renal failure is termed renal osteodystrophy.
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism, quartary and quintary hyperparathyroidism are rare forms that are caused by long lasting disorders of the calcium feedback control system. When the hyperparathyroidism can not be corrected by medication one calls it tertiary hyperparathyroidism.
Diagnosis
The gold standard of diagnosis is the PTH immunoassay. Once an elevated PTH has been confirmed, goal of diagnosis is to determine whether the hyperparathyroidism is primary or secondary in origin by obtaining a serum calcium level:
| PTH | serum calcium | likely type |
| high | high | primary hyperparathyroidism |
| high | low or normal | secondary hyperparathyroidism |
Tertiary hyperparathyroidism has a high PTH and a high serum calcium. It is differentiated from primary hyperparathyroidism by a history of chronic kidney failure and secondary hyperparathyroidism.
Treatment/Monitoring
Endocrinologists diagnose diseases affecting glands and should be consulted for hyperparathyroidism. Treatment is first and foremost directed at hypercalcemia, if symptomatic patients are sent for surgery to remove the parathyroid tumor (parathyroid adenoma). (see hypercalcemia) Most experts now believe that almost all patients with hyperparathyroidism should be evaluated for surgery. Watching and waiting has been falling out of vogue since it is being realized that the disease will rarely stay the same. It will almost always progress as the tumor grows.
However, if surgery is not available, the following should be monitored:
- Calcium level: Ask the doctor to monitor your calcium levels via urine tests. The results can be used to provide information regarding kidney functionality as well as how much calcium is being excreted in your urine.
- Bone density: Doctors can determine if you're essentially shrinking by performing bone mineral density tests. These tests can be used to assess the risk of osteoporosis. Some of the different types of tests include dual energy X-ray absorptiometry (DEXA) which measures the density of bones in the hip, wrist, and spine and ultrasounds.
- Check for Kidney Stones: Abdominal X-rays can be used to check for kidney stones.
Prevention
If you choose to monitor symptoms, some recommendations for prevention include [2]:
- Exercise, specifically weight and strength training are beneficial. This helps in the process of decreasing bone loss and building stronger bones.
- Vitamin D - Adequate amounts of vitamin D aid in calcium absorption. Sources of vitamin D come from the foods you eat, sunlight, and from vitamin supplemants.
- Stay hydrated - drinking lots of fluids can aid in preventing the formation of kidney stones.
- No smoking - Besides known negative affects of smoking such as cancer, smoking aids in bone loss
References
General Reading
1. Lawrence Kim, MD, Director of Surgical Endocrinology; Chief of Surgery Central Ark. VA, Department of Surgery, Associate Professor of Surgery, University of Arkansas Hospital, 2005. http://www.emedicine.com/med/topic3200.htm 2. Mayo Clinic: http://www.mayoclinic.com/health/hyperparathyroidism/DS00396 3. Hyperparathyroidism: www.hyperparathyroidism.com
- ↑ Zink AR, Panzer S, Fesq-Martin M, Burger-Heinrich E, Wahl J, Nerlich AG (2005). "Evidence for a 7000-year-old case of primary hyperparathyroidism". JAMA. 293 (1): 40–2. doi:10.1001/jama.293.1.40-c. PMID 15632333.
See also
External links
- Description of parathyroid disease and treatment in detail at www.parathyroid.com
- Section on parathyroid disease at endocrineweb.com
- Overview at Mayo Clinic
- Overview at Endocrine and Metabolic Diseases Information Service