Human chorionic gonadotropin
| chorionic gonadotropin, beta polypeptide | |
|---|---|
 HCG polypeptide structure | |
| Identifiers | |
| Symbol | CGB |
| Entrez | 1082 |
| HUGO | 1886 |
| OMIM | 118860 |
| PDB | 1HCN |
| RefSeq | NM_000737 |
| UniProt | P01233 |
| Other data | |
| Locus | Chr. 19 q13.3 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Human chorionic gonadotropin (hCG) is a peptide hormone produced in pregnancy, that is made by the embryo soon after conception and later by the syncytiotrophoblast (part of the placenta). Its role is to prevent the disintegration of the corpus luteum of the ovary and thereby maintain progesterone production that is critical for a pregnancy in humans. hCG may have additional functions, for instance it is thought that it affects the immune tolerance of the pregnancy. Early pregnancy testing generally is based on the detection or measurement of hCG. Because hCG is produced also by some kinds of tumor, hCG is an important tumor marker, but it is not known whether this production is a contributing cause or an effect of tumorigenesis.
- Human chorionic gonadotropin (HCG) is a glycoprotein made by the chorionic cells of the fetal part of the placenta
- HCG is directed at the gonads, and therefore stimulates them
- HCG is important for early diagnosis of pregnancy
- Reference Range: < 3 mU/l in serum
Structure
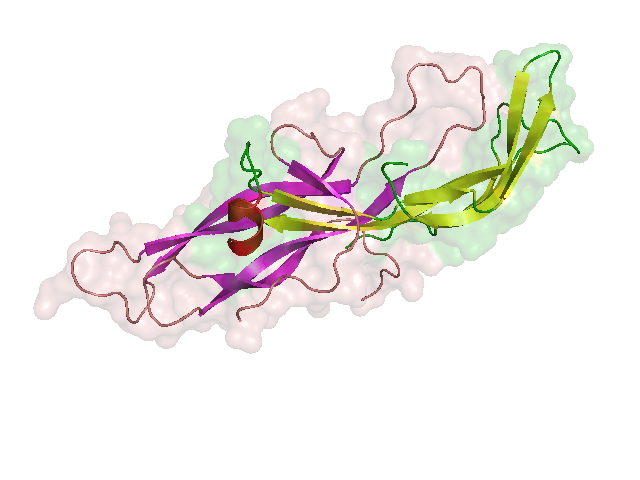
hCG is an oligosaccharide glycoprotein composed of 244 amino acids with a molecular mass of 36.7 kDa. Its total dimensions are 75x35x30 angstroms (7.5x3.5x3 nanometers).
It is heterodimeric, with an α (alpha) subunit identical to that of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and thyroid-stimulating hormone (TSH) and β (beta) subunit that is unique to hCG.
- βhCG is encoded by six highly homologous genes which are arranged in tandem and inverted pairs on chromosome 19q13.3 - CGB(1, 2, 3, 5, 7, 8).
The two subunits create a small hydrophobic core surrounded by a high surface area to volume ratio 2.8 times that of a sphere. The vast majority of the outer amino acids are hydrophilic.
Function
hCG interacts with the LHCG receptor and promotes the maintenance of the corpus luteum during the beginning of [pregnancy]] causing it to secrete the hormone progesterone. Progesterone enriches the uterus with a thick lining of blood vessels and capillaries so that it can sustain the growing fetus. Due to its highly negative charge hCG may repel the immune cells of the mother, protecting the fetus during the first trimester. It has also been hypothesized that hCG may be a placental link for the development of local maternal immunotolerance. For example, hCG-treated endometrial cells induce an increase in T cell apoptosis (dissolution of T-cells). These results suggest that hCG may be a link in the development of peritrophoblastic immune tolerance and may facilitate the trophoblast invasion which is known to expedite fetal development in the endometrium.[1] It has also been suggested that hCG levels are linked to the severity of morning sickness in pregnant women.[2]
Because of its similarity to LH, hCG can also be used clinically to induce ovulation in the ovaries as well as testosterone production in the testes. As the most abundant biological source is women who are presently pregnant, some organizations collect urine from gravidae to extract hCG for use in fertility treatment.
Differential Diagnosis
Increased
- Adenocarcinoma
- Breast Cancer
- Chemotherapy
- Choriocarcinoma
- Colon carcinoma
- Delimitation of the extrauterine pregnancy (EUP)
- Down's Syndrome
- Embryonal cell carcinoma
- Hydatidiform mole
- Islet-cell carcinoma
- Ovarian carcinoma
- Placental chorion carcinoma
- Postmenopausal females with renal insufficiency dependent on dialysis
- Pregnancy
- Progress control in threatening miscarriage
- Renal carcinoma
- Seminoma
Pregnancy testing
Pregnancy tests measure the levels of hCG in the blood or urine to indicate the presence or absence of an implanted embryo.
In particular, most pregnancy tests employ a monoclonal antibody (MAb), which is specific to the β-subunit of hCG (βhCG). This is important so that tests do not make false positives by confusing hCG with LH and FSH. (The latter two are always present at varying levels in the body, while hCG levels are negligible except during pregnancy.)
- The urine test may be a chromatographic immunoassay or any of several other test formats, home-, physician's office-, or laboratory-based.[3] Published detection thresholds range from 20 to 100 mIU/ml (milli International Units per milli-liter), depending on the brand of test.[4] The urine should be the first urine of the morning when hCG levels are highest. If the specific gravity of the urine is above 1.015, the urine should be diluted.
- The serum test, using 2-4 mL of venous blood, is typically a chemiluminescent or fluorimetric immunoassay[3] that can detect βhCG levels as low as 5 mIU/ml and allows quantitation of the βhCG concentration. The ability to quantitate the βhCG level is useful in the evaluation of ectopic pregnancy and in monitoring germ cell and trophoblastic tumors.
Hydatiform moles ("molar pregnancy") may produce high levels of βhCG, despite the absence of an embryo. This, as well as several other conditions, can lead to false positive readings of pregnancy tests.
Tumor marker
β-hCG is also secreted by some cancers including choriocarcinoma, teratoma with elements of choriocarcinoma (this is rare), and islet cell tumor.
Use as medication
hCG is extensively used as a parenteral fertility medication in lieu of luteinizing hormone. In the presence of one or more mature ovarian follicles, ovulation can be triggered by the administration of hCG. As ovulation will happen about 40-45 hours after the injection of hCG, procedures can be scheduled to take advantage of this time sequence. Thus, patients who undergo IVF, typically receive hCG to trigger the ovulation process, but have their eggs retrieved at about 36 hours after injection, a few hours before the eggs actually would be released from the ovary.
As hCG supports the corpus luteum, administration of hCG is used in certain circumstances to enhance the production of progesterone.
In the male, hCG injections are used to stimulate the leydig cells to synthesize testosterone. The intratesticular testosterone is necessary for spermatogenesis from the sertoli cells. Typical uses for hCG in men include hypogonadism and fertility treatment.
Production
Like other gonadotropins, hCG can be extracted from urine or by genetic modification. Pregnyl, Follutein, Profasi, and Novarel use the former method, derived from the urine of pregnant women. Ovidrel, on the other hand, is a product of recombinant DNA. Novarel and hCG from APP are typically considered generics in the United States.
Use with anabolic steroids
In the world of performance enhancing drugs, hCG is increasingly used in combination with various anabolic androgenic steroid (AAS) cycles.
When AAS are put into a male body, the body's natural negative feedback loops cause the body to shut down its own production of testosterone via shutdown of the HPTA (hypothalamic-pituitary-testicular axis). High levels of AASs that mimic the body's natural testosterone trigger the hypothalamus to shut down its production of gonadotropin-releasing hormone (GnRH) from the hypothalamus. Without GnRH the pituitary gland stops releasing luteinizing hormone (LH). LH normally travels from the pituitary via the blood stream to the testes where it triggers the production and release of testosterone. Without LH, the testes shut down their production of testosterone, causing testicular atrophy.
In males, hCG mimics LH and helps restore / maintain testosterone production in the testes. As such, hCG is commonly used during and after steroid cycles to maintain and restore testicular size as well as endogenous testosterone production. However, if hCG is used for too long and in too high a dose, the resulting rise in natural testosterone will eventually inhibit its own production via negative feedback on the hypothalamus and pituitary.
References
- ↑ Kayisli U, Selam B, Guzeloglu-Kayisli O, Demir R, Arici A (2003). "Human chorionic gonadotropin contributes to maternal immunotolerance and endometrial apoptosis by regulating Fas-Fas ligand system". J. Immunol. 171 (5): 2305–13. PMID 12928375.
- ↑ Askling, J (1999 Dec 11). "Sickness in pregnancy and sex of child". The Lancet. 354 (9195): 2053. PMID 10636378. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ 3.0 3.1 Richard A. McPherson, Matthew R. Pincus, (2006). Henry's Clinical Diagnosis and Management by Laboratory Methods (21st edition ed.). Philadelphia: Saunders. ISBN 1-4160-0287-1.
- ↑ Waddell, Rebecca Smith (2006). "FertilityPlus.org". Home Pregnancy Test hCG Levels and FAQ.
de:Humanes Choriongonadotropin
it:Gonadotropina corionica
he:גונדוטרופין כוריוני אנושי
lt:Chorioninis gonadotropinas
ml:എച്ച്.സി.ജി.
nl:Humaan choriongonadotrofine