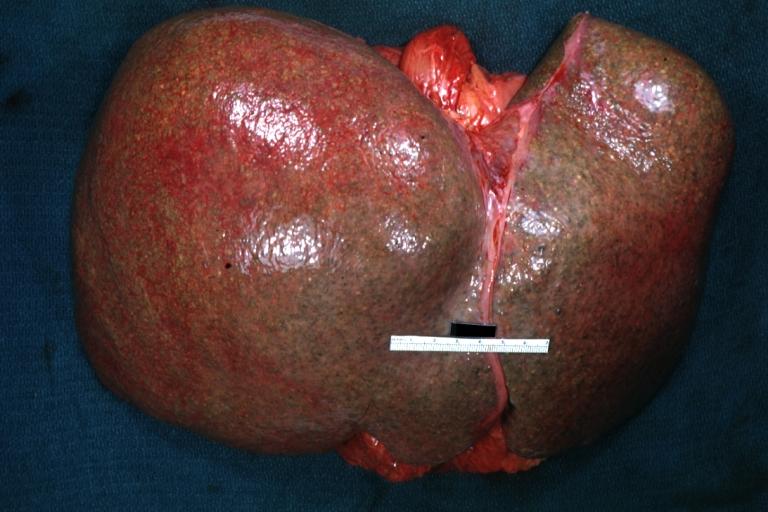
Hepatomegaly
| Hepatomegaly | |
 |
|---|
For patient information on this topic, click here.
|
Hepatomegaly Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Iqra Qamar M.D.[2] Cafer Zorkun, M.D., Ph.D. [3]
Synonyms and keywords: Enlarged liver; liver enlargement
Overview
The liver is an organ present in vertebrates and some other animals. The adult human liver normally weighs between 1.4 - 1.6 kilograms (3.1 - 3.5 pounds), and it is a soft, pinkish-brown "boomerang shaped" organ. It is located on the right side of the upper abdomen below the diaphragm. The liver size increases with age and it ranges between 5 cm to 15 cm in adulthood. A normal liver is less than 16 cm in ultrasound evaluation. Hepatomegaly may be found in physical examination or during imaging studies. Imaging is more accurate in determining liver size.[1][2] In some certain conditions normal liver may be palpated as enlarged liver including thin people, during deep inspiration, right pleural effusion, and when emphysema results in hyperinflation of the chest with diaphragmatic descent and downward displacement of the liver. Common pathologic causes that may result in hepatomegaly are hepatitis, storage disorders, impaired venous outflow, infiltrative disorders, and biliary obstruction.
Causes
Causes of hepatomegaly may be classified on the basis of etiology into hepatitis, storage disorders, impaired venous outflow, infiltrative and obstructive causes.[3][4][5][6][7][8][9][10][11][12][13][14]
| Etiology | Disease | |
|---|---|---|
| Hepatitis | Infections | Acute and chronic viral hepatitis |
| Bacterial liver abscess | ||
| Parasitic infections | ||
| Granulomatous hepatitis | ||
| Ischemia | Ischemic hepatitis ("shock liver") | |
| Toxins | Alcoholic hepatitis | |
| Steatosis | Alcoholic fatty liver disease | |
| Nonalcoholic steatohepatitis | ||
| Drugs/Medications | Drug induced liver injury (DILI) | |
| Immune mediated hepatitis | Autoimmune hepatitis | |
| Copper deposition | Wilson disease | |
| Storage disorders | Glycogen | Glycogen storage disorders |
| Diabetes mellitus | ||
| Lipid | Gaucher disease | |
| Nonalcoholic steatohepatitis | ||
| Protein | Alpha-1 antitrypsin deficiency | |
| Iron | Hemochromatosis | |
| Impaired venous outflow | Cardiac | Right heart failure |
| Constrictive pericarditis | ||
| Hepatic vein | Hepatic vein thrombosis | |
| Inferior vena cava web | ||
| Intrahepatic | Sinusoidal obstruction syndrome | |
| Peliosis hepatis | ||
| Infiltrative diseases | Benign primary liver tumors | Hemangiomas |
| Adenomas | ||
| Focal nodular hyperplasia | ||
| Malignant primary liver tumors | Hepatocellular carcinoma | |
| Cholangiocarcinoma | ||
| Fibrolamellar carcinoma | ||
| Hemangioendothelioma | ||
| Metastatic/disseminated tumors | Myeloma | |
| Lymphoma | ||
| Leukemia | ||
| Metastatic solid tumors | ||
| Biliary obstruction | Primary biliary cirrhosis | |
| Primary sclerosing cholangitis | ||
| Biliary atresia | ||
| Other | Anatomic variations | Riedel's lobe |
| Cystic liver disease | Polycystic liver disease | |
| Caroli's disease | ||
Differential diagnosis
Patients with hepatomegaly need to be differentiated from other patients presenting with similar complaints such as abdominal pain.[3][4][5][6][7][8][9][10][11][12][13][14]
Abbreviations: RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein, TS= Transferrin saturation, SF= Serum Ferritin, SMA= Superior mesenteric artery, SMV= Superior mesenteric vein, ECG= Electrocardiogram, US = Ultrasound
| Classification of pain in the abdomen based on etiology | Disease | Clinical manifestations | Diagnosis | Comments | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Signs | |||||||||||||
| Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | |||||
| Abdominal causes | Inflammatory causes | Pancreato-biliary disorders | Acute suppurative cholangitis | RUQ | + | + | + | − | + | + | + |
|
|
|
| Acute cholangitis | RUQ | + | − | + | − | − | − | − |
|
|
| |||
| Acute cholecystitis | RUQ | + | + | + | − | − | − | − | Ultrasound shows:
|
|||||
| Acute pancreatitis | Epigastric | + | + | ± | + | ± | − | − |
|
| ||||
| Chronic pancreatitis | Epigastric | − | ± | ± | + | − | − | − | CT scan
|
| ||||
| Pancreatic carcinoma | Epigastric | − | + | + | + | − | − | − |
Skin manifestations may include: | |||||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Primary biliary cirrhosis | RUQ/Epigastric | − | − | + | − | − | − | − |
|
|
| |||
| Primary sclerosing cholangitis | RUQ | + | − | + | − | − | − | − |
|
ERCP and MRCP shows
|
| |||
| Cholelithiasis | RUQ/Epigastric | ± | ± | ± | − | − | − | − |
|
| ||||
| Gastric causes | Peptic ulcer disease | Diffuse | ± | + | − | + | Positive if perforated | Positive if perforated | Positive if perforated |
| ||||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Gastritis | Epigastric | ± | + | − | Positive in chronic gastritis | − | − | − | ||||||
| Gastroesophageal reflux disease | Epigastric | − | ± | − | − | − | − | − | N |
|
| |||
| Gastric outlet obstruction | Epigastric | − | ± | − | + | − | − | − |
|
| ||||
| Gastroparesis | Epigastric | − | + | − | + | ± | − | − |
|
|
| |||
| Gastrointestinal perforation | Diffuse | + | - | ± | − | + | + | ± |
|
|||||
| Dumping syndrome | Lower and then diffuse | − | + | − | + | + | − | − |
|
|
| |||
| Intestinal causes | Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | ||
| Acute appendicitis | Starts in epigastrium, migrates to RLQ | + | + | − | − | Positive in perforated appendicitis | + | + |
|
| ||||
| Acute diverticulitis | LLQ | + | + | − | − | Positive in perforated diverticulitis | + | + |
|
| ||||
| Inflammatory bowel disease | Diffuse | ± | − | ± | + | − | − | − |
Extra intestinal findings: | |||||
| Irritable bowel syndrome | Diffuse | − | − | − | + | − | − | − | Normal | Normal | Symptomatic treatment
| |||
| Whipple's disease | Diffuse | ± | − | ± | + | ± | − | − | Endoscopy is used to confirm diagnosis.
Images used to find complications |
Extra intestinal findings: | ||||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Toxic megacolon | Diffuse | + | − | − | − | + | ± | + |
|
CT and Ultrasound shows:
|
||||
| Tropical sprue | Diffuse | + | − | − | + | − | − | − |
|
Barium studies:
|
| |||
| Celiac disease | Diffuse | − | − | − | + | − | − | − |
|
US:
|
| |||
| Infective colitis | Diffuse | + | ± | − | − | Positive in fulminant colitis | ± | ± |
|
CT scan
|
||||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Colon carcinoma | Diffuse/ RLQ/LLQ | − | − | − | + | ± | − | − |
|
|
| |||
| Hepatic causes | Viral hepatitis | RUQ | + | + | + | + | Positive in fulminant hepatitis | Positive in acute | + |
|
|
| ||
| Liver abscess | RUQ | + | + | + | + | + | + | ± |
|
|
||||
| Hepatocellular carcinoma/Metastasis | RUQ | + | − | + | + | − | − | − |
|
|
Other symptoms: | |||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Budd-Chiari syndrome | RUQ | ± | − | ± | − | − | − | − |
|
|
Ascitic fluid examination shows:
| |||
| Hemochromatosis | RUQ | − | − | − | − | − | − | − |
|
|
Extra intestinal findings:
| |||
| Cirrhosis | RUQ | − | − | + | + | + | − | − |
|
US
|
| |||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Peritoneal causes | Spontaneous bacterial peritonitis | Diffuse | + | − | Positive in cirrhotic patients | − | ± | + | + |
|
|
|||
| Renal causes | Pyelonephritis | Unilateral | + | + | − | − | + | − | − |
|
|
| ||
| Renal colic | Flank pain | − | + | − | − | − | − | − |
|
| ||||
| Hollow Viscous Obstruction | Small bowel obstruction | Diffuse | + | + | − | + | + | + | ± |
|
Abdominal X ray
|
| ||
| Volvulus | Diffuse | - | + | − | − | Positive in perforated cases | + | + | CT scan and abdominal X ray
|
| ||||
| Biliary colic | RUQ | − | + | + | − | − | − | − |
|
|||||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Vascular Disorders | Ischemic causes | Mesenteric ischemia | Periumbilical | Positive if bowel becomes gangrenous | + | − | + | Positive if bowel becomes gangrenous | Positive if bowel becomes gangrenous | − |
|
CT angiography
|
| |
| Acute ischemic colitis | Diffuse | + | + | − | + | + | + | + | Abdominal x-ray
CT scan
|
| ||||
| Hemorrhagic causes | Ruptured abdominal aortic aneurysm | Diffuse | ± | + | − | + | + | − | − |
|
| |||
| Intra-abdominal or retroperitoneal hemorrhage | Diffuse | ± | ± | − | − | + | − | − |
|
|
| |||
| Disease | Abdominal Pain | Fever | Nausea or vomiting | Jaundice | Weight loss | Hypo-
tension |
Guarding | Rebound Tenderness | Lab Findings | Imaging | Comments | |||
| Gynaecological Causes | Tubal causes | Torsion of the cyst/ovary | RLQ / LLQ | − | + | − | − | − | ± | ± |
|
| ||
| Acute salpingitis | RLQ / LLQ | + | − | − | − | − | ± | ± | ||||||
| Cyst rupture | RLQ / LLQ | − | + | − | − | + | ± | ± |
|
|||||
| Pregnancy | Ruptured ectopic pregnancy | RLQ / LLQ | − | + | − | − | + | + | + |
|
|
History of
| ||
| Extra-abdominal causes | Pulmonary disorders | Pleural empyema | RUQ/Epigastric | + | − | − | + | − | − | − | Chest X-ray
|
Physical examination
| ||
| Pulmonary embolism | RUQ/LUQ | ± | − | − | − | ± | − | − |
|
|
| |||
| Pneumonia | RUQ/LUQ | + | + | − | − | + | − | − |
|
|
| |||
| Cardiovascular disorders | Myocardial Infarction | Epigastric | ± | + | − | − | Positive in cardiogenic shock | − | − | ECG
|
Complications:
| |||
Diagnostic workup
References
- ↑ Sapira JD, Williamson DL (1979). "How big is the normal liver?". Arch Intern Med. 139 (9): 971–3. PMID 475535.
- ↑ Niederau C, Sonnenberg A, Müller JE, Erckenbrecht JF, Scholten T, Fritsch WP (1983). "Sonographic measurements of the normal liver, spleen, pancreas, and portal vein". Radiology. 149 (2): 537–40. doi:10.1148/radiology.149.2.6622701. PMID 6622701.
- ↑ 3.0 3.1 Wolf AD, Lavine JE (2000). "Hepatomegaly in neonates and children". Pediatr Rev. 21 (9): 303–10. PMID 10970452.
- ↑ 4.0 4.1 Chau TN, Lai ST, Tse C, Ng TK, Leung VK, Lim W, Ng MH (2006). "Epidemiology and clinical features of sporadic hepatitis E as compared with hepatitis A". Am. J. Gastroenterol. 101 (2): 292–6. doi:10.1111/j.1572-0241.2006.00416.x. PMID 16454833.
- ↑ 5.0 5.1 Bernstein DL, Hülkova H, Bialer MG, Desnick RJ (2013). "Cholesteryl ester storage disease: review of the findings in 135 reported patients with an underdiagnosed disease". J. Hepatol. 58 (6): 1230–43. doi:10.1016/j.jhep.2013.02.014. PMID 23485521.
- ↑ 6.0 6.1 Torbenson M, Chen YY, Brunt E, Cummings OW, Gottfried M, Jakate S, Liu YC, Yeh MM, Ferrell L (2006). "Glycogenic hepatopathy: an underrecognized hepatic complication of diabetes mellitus". Am. J. Surg. Pathol. 30 (4): 508–13. PMID 16625098.
- ↑ 7.0 7.1 Chatila R, West AB (1996). "Hepatomegaly and abnormal liver tests due to glycogenosis in adults with diabetes". Medicine (Baltimore). 75 (6): 327–33. PMID 8982149.
- ↑ 8.0 8.1 Mukewar S, Sharma A, Lackore KA, Enders FT, Torbenson MS, Kamath PS, Roberts LR, Kudva YC (2017). "Clinical, Biochemical, and Histopathology Features of Patients With Glycogenic Hepatopathy". Clin. Gastroenterol. Hepatol. 15 (6): 927–933. doi:10.1016/j.cgh.2016.11.038. PMID 28043933.
- ↑ 9.0 9.1 Charrow J, Andersson HC, Kaplan P, Kolodny EH, Mistry P, Pastores G, Rosenbloom BE, Scott CR, Wappner RS, Weinreb NJ, Zimran A (2000). "The Gaucher registry: demographics and disease characteristics of 1698 patients with Gaucher disease". Arch. Intern. Med. 160 (18): 2835–43. PMID 11025794.
- ↑ 10.0 10.1 Drebber U, Kasper HU, Ratering J, Wedemeyer I, Schirmacher P, Dienes HP, Odenthal M (2008). "Hepatic granulomas: histological and molecular pathological approach to differential diagnosis--a study of 442 cases". Liver Int. 28 (6): 828–34. doi:10.1111/j.1478-3231.2008.01695.x. PMID 18312287.
- ↑ 11.0 11.1 Park MA, Mueller PS, Kyle RA, Larson DR, Plevak MF, Gertz MA (2003). "Primary (AL) hepatic amyloidosis: clinical features and natural history in 98 patients". Medicine (Baltimore). 82 (5): 291–8. doi:10.1097/01.md.0000091183.93122.c7. PMID 14530778.
- ↑ 12.0 12.1 Cooke CB, Krenacs L, Stetler-Stevenson M, Greiner TC, Raffeld M, Kingma DW, Abruzzo L, Frantz C, Kaviani M, Jaffe ES (1996). "Hepatosplenic T-cell lymphoma: a distinct clinicopathologic entity of cytotoxic gamma delta T-cell origin". Blood. 88 (11): 4265–74. PMID 8943863.
- ↑ 13.0 13.1 Long RG, Scheuer PJ, Sherlock S (1977). "Presentation and course of asymptomatic primary biliary cirrhosis". Gastroenterology. 72 (6): 1204–7. PMID 870368.
- ↑ 14.0 14.1 "EASL Clinical Practice Guidelines: management of cholestatic liver diseases". J. Hepatol. 51 (2): 237–67. 2009. doi:10.1016/j.jhep.2009.04.009. PMID 19501929.