Aortic dissection MRI: Difference between revisions
(/* 2010 ACCF/AHA Guideline Recommendations: Diagnosis and Management of Patients with Thoracic Aortic Disease - Recommendations for Aortic Imaging in Genetic Syndromes (DO NOT EDIT) {{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin...) |
No edit summary |
||
| (37 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Template:Aortic dissection}} | {{Template:Aortic dissection}} | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}}; {{RT}} | |||
{{CMG}} ; '''Associate Editor-In-Chief:''' {{CZ}} | |||
==Overview== | ==Overview== | ||
MRI is the imaging modality of choice in the assessment of longstanding aortic disease in a patient who has chronic chest pain who is | [[MRI]] is the imaging modality of choice in the assessment of longstanding [[aortic]] disease in a patient who has [[chronic]] [[chest pain]] who is [[hemodynamic]]ally stable or for the evaluation of a [[chronic]] dissection. | ||
== MRI == | == MRI == | ||
*[[Magnetic resonance imaging]] (MRI) is currently the [[gold standard (test)|gold standard test]] for the detection and assessment of aortic dissection, with a sensitivity of 98% and a specificity of 98%. | *[[Magnetic resonance imaging]] ([[MRI]]) is currently the [[gold standard (test)|gold standard test]] for the detection and assessment of [[aortic]] dissection, with a [[sensitivity]] of 98% and a [[specificity]] of 98%. | ||
*An MRI examination of the aorta will produce a three-dimensional reconstruction of the aorta, allowing the physician to determine the location of the | *An [[MRI]] examination of the [[aorta]] will produce a three-dimensional reconstruction of the [[aorta]], allowing the physician to determine the location of the [[intima]]l tear, the involvement of branch [[vessel]]s, and locate any secondary tears. | ||
*It is a non-invasive test, does not require the use of iodinated contrast material, and can detect and quantitate the degree of [[aortic insufficiency]]. | *It is a non-invasive test, does not require the use of [[iodinated contrast]] material, and can detect and quantitate the degree of [[aortic insufficiency]]. | ||
*The disadvantage of the MRI scan in the face of aortic dissection is that it has limited availability and is often located only in | *The disadvantage of the [[MRI]] scan in the face of [[aortic]] dissection is that it has limited availability and is often located only in larger hospitals, and the scan is relatively time-consuming. | ||
*Due to the high intensity of the magnetic waves used during MRI, an MRI scan is contraindicated in individuals with metallic implants. *In addition, many individuals develop [[claustrophobia]] while in the MRI scanning tube. | *Due to the high intensity of the magnetic waves used during [[MRI]], an [[MRI]] scan is contraindicated in individuals with metallic implants. | ||
*In addition, many individuals develop [[claustrophobia]] while in the [[MRI]] scanning tube. | |||
[[Image:AoDiss MRT.jpg|thumb|left|200px|[[Magnetic resonance imaging|MRI]] of an [[aortic]] dissection. ''1'' [[descending aorta|Aorta descendens]] with dissection. ''2'' [[Aortic]] isthmus.]] | |||
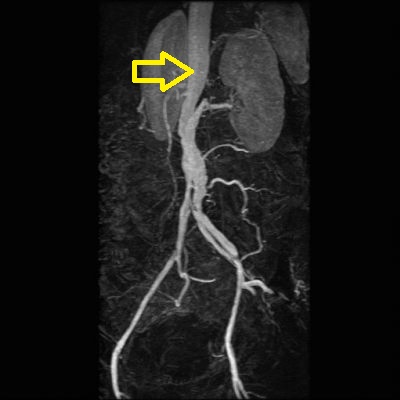
[[File:Iatrogenic-abdominal-aortic-dissection.jpg|thumb|center|300px|[[Magnetic resonance imaging|MRI]] of an [[aortic]] dissection<ref>Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 13757</ref>]] | |||
== 2022 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease<ref name="pmid36334952">{{cite journal| author=Writing Committee Members. Isselbacher EM, Preventza O, Hamilton Black J, Augoustides JG, Beck AW | display-authors=etal| title=2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. | journal=J Am Coll Cardiol | year= 2022 | volume= | issue= | pages= | pmid=36334952 | doi=10.1016/j.jacc.2022.08.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=36334952 }}</ref> == | |||
=== Recommendations for HTAD: Genetic Testing and Screening of Family Members for TAD Referenced studies that support the recommendations are summarized in the Online Data Supplement === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.''' In patients with TAD who have a pathogenic/likely pathogenic variant, genetic testing of at-risk biological relatives (ie, cascade testing) is recommended.6,10,11 In family members who are found by genetic screening to have inherited the pathogenic/likely pathogenic variant, aortic imaging with TTE (if aortic root and ascending aorta are adequately visualized, otherwise with CT or MRI) is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | |||
|} | |||
=== Recommendations for Aortic Imaging Techniques to Determine Presence and Progression of Aortic Disease Referenced studies that support the recommendations are summarized in the Online Data Supplement === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.''' In patients with known or suspected aortic disease, when performing CT or MR imaging, it is recommended that the root and ascending aortic diameters be measured from inner-edge to inner-edge, using an electrocardiographic-synchronized technique. If there are aortic wall abnormalities, such as atherosclerosis or discrete wall thickening (more common in the distal aorta), the outer-edge to outer-edge diameter should be reported''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
|} | |||
== | === Recommendations for Imaging in Loeys-Dietz Syndrome === | ||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.''' In patients with Loeys-Dietz syndrome and a dilated or dissected aorta and/or arterial branches at baseline, annual surveillance imaging of the affected aorta and arteries with MRI or CT is recommended''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
'''2.''' In patients with Loeys-Dietz syndrome, a baseline MRI or CT from head to pelvis is recommended to evaluate the entire aorta and its branches for aneurysm, dissection, and tortuosity.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-LD]])'' | |||
|} | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
| bgcolor="LemonChiffon" |'''1.'''In patients with Loeys-Dietz syndrome with-out dilation of the aorta distal to the aortic root or ascending aorta and without dilated or dissected arterial branches, surveillance imaging from chest to pelvis with MRI (or CT) every 2 years is reasonable, but imaging may be more frequent depending on family history.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
'''2.'''In patients with Loeys-Dietz syndrome with-out dilation of the cerebral arteries on initial screening, periodic imaging surveillance for cerebral aneurysms with MRI or CT every 2 to 3 years is reasonable.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-EO]])'' | |||
|} | |||
=== Recommendations for Inflammatory Aortitis: Diagnosis and Treatment of Takayasu Arteritis and GCA Referenced studies that support the recommendations are summarized in the Online Data Supplement === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.'''In patients with large vessel vasculitis (LVV), prompt evaluation of the entire aorta and branch vessels with MRI or CT, with or without 18F-FDG positron emission tomography (FDG-PET), is recommended.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C-LD]])'' | |||
|} | |||
=== Recommendations for Long-Term Surveillance Imaging After Aortic Dissection and IMH Referenced studies that support the recommendations are summarized in the Online Data Supplement === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.''' In patients who have had an acute aortic dissection and IMH treated with either open or endovascular aortic repair and have residual aortic disease, surveillance imaging with a CT (or MRI) is recommended after 1 month, 6 months, and 12 months and then, if stable, annually thereafter.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | |||
'''2.''' In patients who have had an acute aortic dissection and IMH that was managed with medical therapy alone, surveillance imaging with a CT (or MRI) is recommended after 1 month, 6 months, and 12 months and then, if stable, annually thereafter.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B-NR]])'' | |||
|} | |||
==2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)<ref name="pmid25173340">{{cite journal |vauthors=Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ |title=2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC) |journal=Eur. Heart J. |volume=35 |issue=41 |pages=2873–926 |date=November 2014 |pmid=25173340 |doi=10.1093/eurheartj/ehu281 |url=}}</ref>== | |||
===Diagnostic Value of MRI in Aortic Dissection=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ESC guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
|bgcolor="LightGreen" |<nowiki>"</nowiki>''In stable [[patients]], [[computed tomography]] or [[magnetic resonance imaging]] are the recommended [[imaging]] studies. prefered modality is chosen according to local availabilty or expertise. ([[ESC guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|- | |||
|bgcolor="LightGreen" |<nowiki>"</nowiki>''In case of initially negative [[imaging]] study, repetitive [[imaging]] study (including [[CT]] or [[MRI]]) is recommended if the suspicion for [[acute aortic syndrome]] is high. ([[ESC guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|- | |||
|bgcolor="LightGreen" |<nowiki>"</nowiki>''Repeated [[imaging]] study (including [[CT]] or [[MRI]]) is recommended in case of uncomplicated medially treated aortic dissection type B in the first few days of treatment. ([[ESC guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|} | |||
==2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>== | |||
===Screening Tests (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>=== | |||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
|bgcolor="LightGreen" |<nowiki>"</nowiki> '''1.''' Urgent and definitive imaging of the aorta using transesophageal echocardiogram, computed tomographic imaging, or magnetic resonance imaging is recommended to identify or exclude thoracic aortic dissection in patients at high risk for the disease by initial screening ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki> | |bgcolor="LightGreen" |<nowiki>"</nowiki>'''1.''' Urgent and definitive imaging of the [[aorta]] using [[transesophageal echocardiogram]], [[computed tomographic imaging]], or [[magnetic resonance imaging]] is recommended to identify or exclude [[thoracic aorta|thoracic]] [[aortic]] dissection in patients at high risk for the disease by initial screening. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki> | ||
|} | |} | ||
=== | ===Determining the Presence and Progression of Thoracic Aortic Disease (DO NOT EDIT)<ref name="pmid20233780">{{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE et al.| title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. | journal=Circulation | year= 2010 | volume= 121 | issue= 13 | pages= e266-369 | pmid=20233780 | doi=10.1161/CIR.0b013e3181d4739e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20233780 }} </ref>=== | ||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' For measurements taken by [[CT|computed tomographic imaging]] or [[magnetic resonance imaging]], the external diameter should be measured perpendicular to the axis of blood flow. For aortic root measurements, the widest diameter, typically at the mid-sinus level, should be used. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' For measurements taken by [[CT|computed tomographic imaging]] or [[magnetic resonance imaging]], the external diameter should be measured perpendicular to the axis of blood flow. For [[aortic root]] measurements, the widest diameter, typically at the mid-sinus level, should be used. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
=== | ===Genetic Syndromes (DO NOT EDIT)<ref name="pmid20233780">{{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE et al.| title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. | journal=Circulation | year= 2010 | volume= 121 | issue= 13 | pages= e266-369 | pmid=20233780 | doi=10.1161/CIR.0b013e3181d4739e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20233780 }} </ref>=== | ||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' Patients with [[Loeys-Dietz syndrome]] should have yearly [[magnetic resonance imaging]] from the [[cerebrovascular]] [[circulation]] to the [[pelvis]]. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki> | |||
|} | |||
===Takayasu Arteritis and Giant Cell Arteritis (DO NOT EDIT)<ref name="pmid20233780">{{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE et al.| title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. | journal=Circulation | year= 2010 | volume= 121 | issue= 13 | pages= e266-369 | pmid=20233780 | doi=10.1161/CIR.0b013e3181d4739e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20233780 }} </ref>=== | |||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' The initial evaluation of [[Takayasu arteritis]] or [[giant cell arteritis]] should include [[thoracic aorta]] and branch [[vessel]] [[computed tomographic imaging]] or [[magnetic resonance imaging]] to investigate the possibility of [[aneurysm]] or occlusive disease in these [[vessel]]s. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
===Surveillance of Thoracic Aortic Disease or Previously Repaired Patients (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>=== | |||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background: | | colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | ||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' [[Computed tomographic imaging]] or [[magnetic resonance imaging]] of the [[thoracic aorta]] is reasonable after a Type A or B [[aortic]] dissection or after [[prophylaxis|prophylactic]] repair of the [[aortic root]]/ [[ascending aorta]]. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''2.''' [[Computed tomographic imaging]] or [[magnetic resonance imaging]] of the [[aorta]] is reasonable at 1, 3, 6, and 12 months postdissection and, if stable, annually thereafter so that any threatening enlargement can be detected in a timely fashion. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''3.''' When following patients with imaging, utilization of the same modality at the same institution is reasonable, so that similar images of matching [[anatomy|anatomic]] segments can be compared side by side. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|- | |- | ||
| bgcolor=" | |bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''4.''' Surveillance imaging similar to classic [[aortic dissection]] is reasonable in patients with intramural [[hematoma]]. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
== | ==2010 ACC/AHA Guidelines - ACCF/ACR/AHA/NASCI/SCMR 2010 Expert Consensus Document on Cardiovascular Magnetic Resonance (DO NOT EDIT)<ref name="pmid20479157">{{cite journal| author=American College of Cardiology Foundation Task Force on Expert Consensus Documents. Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA et al.| title=ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. | journal=Circulation | year= 2010 | volume= 121 | issue= 22 | pages= 2462-508 | pmid=20479157 | doi=10.1161/CIR.0b013e3181d44a8f | pmc=PMC3034132 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20479157 }} </ref> == | ||
{{cquote| | {{cquote| | ||
Cardiovascular Magnetic Resonance of thoracic aortic disease, CMR may be used for defining the location and extent of [[aortic | [[Cardiovascular magnetic resonance imaging (CMR)|Cardiovascular Magnetic Resonance]] of [[thoracic aorta|thoracic aortic]] disease, [[Cardiovascular magnetic resonance imaging (CMR)|CMR]] may be used for defining the location and extent of [[aortic aneurysm]]s, erosions, [[ulcer]]s, [[dissection]]s; evaluating postsurgical processes involving the [[aorta]] and surrounding structures, and [[aortic]] size blood flow and [[cardiac]] cycle–dependent changes in area. | ||
}} | }} | ||
== References == | == References == | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | {{WH}} | ||
{{WS}} | |||
[[CME Category::Cardiology]] | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Best pages]] | |||
Latest revision as of 00:11, 6 December 2022
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Raviteja Guddeti, M.B.B.S. [3]
Overview
MRI is the imaging modality of choice in the assessment of longstanding aortic disease in a patient who has chronic chest pain who is hemodynamically stable or for the evaluation of a chronic dissection.
MRI
- Magnetic resonance imaging (MRI) is currently the gold standard test for the detection and assessment of aortic dissection, with a sensitivity of 98% and a specificity of 98%.
- An MRI examination of the aorta will produce a three-dimensional reconstruction of the aorta, allowing the physician to determine the location of the intimal tear, the involvement of branch vessels, and locate any secondary tears.
- It is a non-invasive test, does not require the use of iodinated contrast material, and can detect and quantitate the degree of aortic insufficiency.
- The disadvantage of the MRI scan in the face of aortic dissection is that it has limited availability and is often located only in larger hospitals, and the scan is relatively time-consuming.
- Due to the high intensity of the magnetic waves used during MRI, an MRI scan is contraindicated in individuals with metallic implants.
- In addition, many individuals develop claustrophobia while in the MRI scanning tube.

2022 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease[2]
Recommendations for HTAD: Genetic Testing and Screening of Family Members for TAD Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1. In patients with TAD who have a pathogenic/likely pathogenic variant, genetic testing of at-risk biological relatives (ie, cascade testing) is recommended.6,10,11 In family members who are found by genetic screening to have inherited the pathogenic/likely pathogenic variant, aortic imaging with TTE (if aortic root and ascending aorta are adequately visualized, otherwise with CT or MRI) is recommended.(Level of Evidence: B-NR) |
Recommendations for Aortic Imaging Techniques to Determine Presence and Progression of Aortic Disease Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1. In patients with known or suspected aortic disease, when performing CT or MR imaging, it is recommended that the root and ascending aortic diameters be measured from inner-edge to inner-edge, using an electrocardiographic-synchronized technique. If there are aortic wall abnormalities, such as atherosclerosis or discrete wall thickening (more common in the distal aorta), the outer-edge to outer-edge diameter should be reported(Level of Evidence: C-EO) |
Recommendations for Imaging in Loeys-Dietz Syndrome
| Class I |
| 1. In patients with Loeys-Dietz syndrome and a dilated or dissected aorta and/or arterial branches at baseline, annual surveillance imaging of the affected aorta and arteries with MRI or CT is recommended(Level of Evidence: C-EO)
2. In patients with Loeys-Dietz syndrome, a baseline MRI or CT from head to pelvis is recommended to evaluate the entire aorta and its branches for aneurysm, dissection, and tortuosity.(Level of Evidence: C-LD) |
| Class IIa |
| 1.In patients with Loeys-Dietz syndrome with-out dilation of the aorta distal to the aortic root or ascending aorta and without dilated or dissected arterial branches, surveillance imaging from chest to pelvis with MRI (or CT) every 2 years is reasonable, but imaging may be more frequent depending on family history.(Level of Evidence: C-EO)
2.In patients with Loeys-Dietz syndrome with-out dilation of the cerebral arteries on initial screening, periodic imaging surveillance for cerebral aneurysms with MRI or CT every 2 to 3 years is reasonable.(Level of Evidence: C-EO) |
Recommendations for Inflammatory Aortitis: Diagnosis and Treatment of Takayasu Arteritis and GCA Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1.In patients with large vessel vasculitis (LVV), prompt evaluation of the entire aorta and branch vessels with MRI or CT, with or without 18F-FDG positron emission tomography (FDG-PET), is recommended.(Level of Evidence: C-LD) |
Recommendations for Long-Term Surveillance Imaging After Aortic Dissection and IMH Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1. In patients who have had an acute aortic dissection and IMH treated with either open or endovascular aortic repair and have residual aortic disease, surveillance imaging with a CT (or MRI) is recommended after 1 month, 6 months, and 12 months and then, if stable, annually thereafter.(Level of Evidence: B-NR)
2. In patients who have had an acute aortic dissection and IMH that was managed with medical therapy alone, surveillance imaging with a CT (or MRI) is recommended after 1 month, 6 months, and 12 months and then, if stable, annually thereafter.(Level of Evidence: B-NR) |
2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)[3]
Diagnostic Value of MRI in Aortic Dissection
| Class I |
| "In stable patients, computed tomography or magnetic resonance imaging are the recommended imaging studies. prefered modality is chosen according to local availabilty or expertise. (Level of Evidence: C)" |
| "In case of initially negative imaging study, repetitive imaging study (including CT or MRI) is recommended if the suspicion for acute aortic syndrome is high. (Level of Evidence: C)" |
| "Repeated imaging study (including CT or MRI) is recommended in case of uncomplicated medially treated aortic dissection type B in the first few days of treatment. (Level of Evidence: C)" |
2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease (DO NOT EDIT)[4]
Screening Tests (DO NOT EDIT)[4]
| Class I |
| "1. Urgent and definitive imaging of the aorta using transesophageal echocardiogram, computed tomographic imaging, or magnetic resonance imaging is recommended to identify or exclude thoracic aortic dissection in patients at high risk for the disease by initial screening. (Level of Evidence: B)" |
Determining the Presence and Progression of Thoracic Aortic Disease (DO NOT EDIT)[4]
| Class I |
| "1. For measurements taken by computed tomographic imaging or magnetic resonance imaging, the external diameter should be measured perpendicular to the axis of blood flow. For aortic root measurements, the widest diameter, typically at the mid-sinus level, should be used. (Level of Evidence: C)" |
Genetic Syndromes (DO NOT EDIT)[4]
| Class I |
| "1. Patients with Loeys-Dietz syndrome should have yearly magnetic resonance imaging from the cerebrovascular circulation to the pelvis. (Level of Evidence: B)" |
Takayasu Arteritis and Giant Cell Arteritis (DO NOT EDIT)[4]
| Class I |
| "1. The initial evaluation of Takayasu arteritis or giant cell arteritis should include thoracic aorta and branch vessel computed tomographic imaging or magnetic resonance imaging to investigate the possibility of aneurysm or occlusive disease in these vessels. (Level of Evidence: C)" |
Surveillance of Thoracic Aortic Disease or Previously Repaired Patients (DO NOT EDIT)[4]
| Class IIa |
| "1. Computed tomographic imaging or magnetic resonance imaging of the thoracic aorta is reasonable after a Type A or B aortic dissection or after prophylactic repair of the aortic root/ ascending aorta. (Level of Evidence: C)" |
| "2. Computed tomographic imaging or magnetic resonance imaging of the aorta is reasonable at 1, 3, 6, and 12 months postdissection and, if stable, annually thereafter so that any threatening enlargement can be detected in a timely fashion. (Level of Evidence: C)" |
| "3. When following patients with imaging, utilization of the same modality at the same institution is reasonable, so that similar images of matching anatomic segments can be compared side by side. (Level of Evidence: C)" |
| "4. Surveillance imaging similar to classic aortic dissection is reasonable in patients with intramural hematoma. (Level of Evidence: C)" |
2010 ACC/AHA Guidelines - ACCF/ACR/AHA/NASCI/SCMR 2010 Expert Consensus Document on Cardiovascular Magnetic Resonance (DO NOT EDIT)[5]
| “ |
Cardiovascular Magnetic Resonance of thoracic aortic disease, CMR may be used for defining the location and extent of aortic aneurysms, erosions, ulcers, dissections; evaluating postsurgical processes involving the aorta and surrounding structures, and aortic size blood flow and cardiac cycle–dependent changes in area. |
” |
References
- ↑ Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 13757
- ↑ Writing Committee Members. Isselbacher EM, Preventza O, Hamilton Black J, Augoustides JG, Beck AW; et al. (2022). "2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines". J Am Coll Cardiol. doi:10.1016/j.jacc.2022.08.004. PMID 36334952 Check
|pmid=value (help). - ↑ Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ (November 2014). "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC)". Eur. Heart J. 35 (41): 2873–926. doi:10.1093/eurheartj/ehu281. PMID 25173340.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Hiratzka LF, Bakris GL, Beckman JA; et al. (2010). "2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine". Circulation. 121 (13): e266–369. doi:10.1161/CIR.0b013e3181d4739e. PMID 20233780. Unknown parameter
|month=ignored (help) - ↑ American College of Cardiology Foundation Task Force on Expert Consensus Documents. Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA; et al. (2010). "ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents". Circulation. 121 (22): 2462–508. doi:10.1161/CIR.0b013e3181d44a8f. PMC 3034132. PMID 20479157.