Aortic dissection overview: Difference between revisions
No edit summary |
|||
| Line 45: | Line 45: | ||
| colspan=4 bgcolor="#ABCDEF" | <small>Classification of aortic dissection</small> | | colspan=4 bgcolor="#ABCDEF" | <small>Classification of aortic dissection</small> | ||
|} | |} | ||
===Stanford Classification System=== | ===Stanford Classification System=== | ||
| Line 68: | Line 67: | ||
Separating the [[false lumen]] from the true lumen is a layer of intimal tissue. This tissue is known as the '''intimal flap'''. As blood flows down the [[false lumen]], it may cause secondary tears in the [[intima]]. Through these secondary tears, the blood can re-enter the true lumen. | Separating the [[false lumen]] from the true lumen is a layer of intimal tissue. This tissue is known as the '''intimal flap'''. As blood flows down the [[false lumen]], it may cause secondary tears in the [[intima]]. Through these secondary tears, the blood can re-enter the true lumen. | ||
==Causes== | ==Causes== | ||
| Line 88: | Line 86: | ||
*[[Turner's syndrome]] | *[[Turner's syndrome]] | ||
*Vascular inflammation due to conditions such as [[arteritis]] and [[syphilis]] | *Vascular inflammation due to conditions such as [[arteritis]] and [[syphilis]] | ||
==Differentiating Aortic Dissection from other Disorders== | |||
Aortic dissection is a life threatening entity that must be distinguished from other life threatening entities such as [[cardiac tamponade]], [[cardiogenic shock]], [[myocardial infarction]], and [[pulmonary embolism]]. An aortic aneurysm is not synonymous with aortic dissection. Aneurysms are defined as a localized permanent dilation of the aorta to a diameter > 50% of normal. Other disorders that aortic dissection should be differentiated from include the following: | |||
* [[Aortic Regurgitation]] | |||
* [[Aortic Stenosis]] | |||
* [[Cardiac Tamponade]] | |||
* [[Cardiogenic Shock]] | |||
* [[Gastroenteritis]] | |||
* [[Hemorrhagic Shock]] | |||
* [[Hernias]] | |||
* [[Hypertensive Emergencies]] | |||
* [[Hypovolemic Shock]] | |||
* [[Mechanical Back Pain]] | |||
* [[Myocardial Infarction]] | |||
* [[Myocarditis]] | |||
* [[Myopathies]] | |||
* [[Pancreatitis]] | |||
* [[Pericarditis]] | |||
* [[Peripheral Vascular Injuries]] | |||
* [[Pleural Effusion]] | |||
* [[Pulmonary Embolism]] | |||
* [[Thoracic Outlet Syndrome]] | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Revision as of 23:28, 28 October 2012
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Aortic dissection is a tear in the wall of the aorta that causes blood to flow between the layers of the wall of the aorta and force the layers apart. Aortic dissection is a medical emergency and can quickly lead to death, even with optimal treatment. If the dissection tears the aorta completely open (through all three layers) massive and rapid blood loss occurs. Aortic dissections resulting in rupture have a 90% mortality rate even if intervention is timely.
Acute aortic dissection is the most common fatal condition that involves the aorta. The mortality rate has been estimated to be as high as 1% per hour during the first 48 hours. Because of the diverse clinical manifestations of aortic dissection, one needs to maintain a high index of suspicion in patients with not just chest pain, but also those with stroke, congestive heart failure, hoarseness, hemoptysis, claudication, superior vena cava (SVC) syndrome, or upper airway obstruction. Despite the fact that a noninvasive diagnosis can be made in up to 90% of cases, the correct antemortem diagnosis is made less than 50% of the time. Recognition of the condition and vigorous pre-operative management are critical to survival.
Classification
Several different classification systems have been used to describe aortic dissections. The systems commonly in use are either based on either the anatomy of the dissection (proximal, distal) or the duration of onset of symptoms (acute, chronic) prior to presentation.
DeBakey classification system
The DeBakey system is an anatomical description of the aortic dissection. It categorizes the dissection based on where the original intimal tear is located and the extent of the dissection (localized to either the ascending aorta or descending aorta, or involves both the ascending and descending aorta.[1]
- Type I - Originates in ascending aorta, propagates at least to the aortic arch and often beyond it distally.
- Type II – Originates in and is confined to the ascending aorta.
- Type III – Originates in descending aorta, rarely extends proximally.
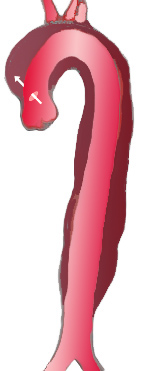
|
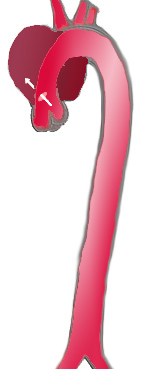
|

| |
| Percentage | 60 % | 10-15 % | 25-30 % |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Stanford A | Stanford B | ||
| Proximal | Distal | ||
| Classification of aortic dissection | |||
Stanford Classification System
Divided into 2 groups; A and B depending on whether the ascending aorta is involved.[2]
- A = Type I and II DeBakey
- B = Type III Debakey
Pathophysiology
Initial Intimal Tear
- Aortic dissection begins as a tear in the aortic wall in > 95% of patients.
- It is usually transverse, extends through the intima and halfway through the media and involves ~50% of the aortic circumference.
- Location of dissections:
- The initial tear is usually within 100 mm of the aortic valve.
- 65% of dissections originate in the ascending aorta, distal to the aortic valve and coronary ostia
- 10% arise in the transverse aortic arch
- 20% in the proximal descending aorta
- 5% in the more distal descending aorta
Propagation of the Intimal Tear
In an aortic dissection, blood penetrates the intima and enters the media layer. The high pressure rips the tissue of the media apart, allowing more blood to enter. This can propagate along the length of the aorta for a variable distance, dissecting either towards or away from the heart or both. Once a tear develops, blood then passes into the media, and a false lumen is dissected in the outer layer of aortic media involving ~50% of the aortic circumference. This false lumen can enlarge, and compress the true lumen, as well as extend proximally or distally and occlude aortic branches. For some unknown reason, the right lateral wall of the ascending aorta is the most common site for dissection. The right coronary artery can become occluded as a result of this propagation.
Separating the false lumen from the true lumen is a layer of intimal tissue. This tissue is known as the intimal flap. As blood flows down the false lumen, it may cause secondary tears in the intima. Through these secondary tears, the blood can re-enter the true lumen.
Causes
Age related changes due to atherosclerosis and hypertension are associated with spontaneous dissection, while blunt trauma injury and sudden deceleration in a motor vehicle accident is a major cause of aortic dissection.
Other risk factors and conditions associated with the development of aortic dissection include:
- Aging
- Bicuspid aortic valve
- Chest trauma
- Coarctation of the aorta
- Connective tissue disorders
- Ehlers-Danlos syndrome
- Heart surgery or procedures
- Marfan syndrome
- Third trimester of pregnancy
- Pseudoxanthoma elasticum
- Tertiary syphilis
- Turner's syndrome
- Vascular inflammation due to conditions such as arteritis and syphilis
Differentiating Aortic Dissection from other Disorders
Aortic dissection is a life threatening entity that must be distinguished from other life threatening entities such as cardiac tamponade, cardiogenic shock, myocardial infarction, and pulmonary embolism. An aortic aneurysm is not synonymous with aortic dissection. Aneurysms are defined as a localized permanent dilation of the aorta to a diameter > 50% of normal. Other disorders that aortic dissection should be differentiated from include the following:
- Aortic Regurgitation
- Aortic Stenosis
- Cardiac Tamponade
- Cardiogenic Shock
- Gastroenteritis
- Hemorrhagic Shock
- Hernias
- Hypertensive Emergencies
- Hypovolemic Shock
- Mechanical Back Pain
- Myocardial Infarction
- Myocarditis
- Myopathies
- Pancreatitis
- Pericarditis
- Peripheral Vascular Injuries
- Pleural Effusion
- Pulmonary Embolism
- Thoracic Outlet Syndrome
Epidemiology and Demographics
There are approximately 2,000 cases of aortic dissection in the US per year, and aortic dissection accounts for 3-4% of sudden deaths. The peak incidence is in the sixth and seventh decades, and males predominate 2:1.
Risk Factors
Aging, atherosclerosis, diabetes, hypertension and trauma are common risk factors for aortic dissection. Uncommon risk factors include bicuspid aortic valve, cocaine, coarctation of the aorta, cystic medial necrosis, Ehlers-Danlos syndrome, Giant cell arteritis, heart surgery, Marfan’s syndrome, pseudoxanthoma elasticum, Turner's syndrome, tertiary syphilis and the third trimester of pregnancy.
References
- ↑ DeBakey ME, Henly WS, Cooley DA, Morris GC Jr, Crawford ES, Beall AC Jr. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg 1965;49:130-49. PMID 14261867.
- ↑ Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg 1970;10:237-47. PMID 5458238.