Diabetic foot pathophysiology: Difference between revisions
No edit summary |
|||
| Line 36: | Line 36: | ||
***Conversely, [[diabetes|diabetic]] [[patients]] with [[sensory system|Sensory]] [[neuropathy]] are more prone to [[ulcer]] formation and related [[Complication (medicine)|complications]], since they don't feel [[pain]] with ever-deepening [[ulcers]]. | ***Conversely, [[diabetes|diabetic]] [[patients]] with [[sensory system|Sensory]] [[neuropathy]] are more prone to [[ulcer]] formation and related [[Complication (medicine)|complications]], since they don't feel [[pain]] with ever-deepening [[ulcers]]. | ||
=== | ===Ischemia=== | ||
[[Microvascular disease|Micro]] and [[Macrovascular disease|macrovascular]] [[Complication (medicine)|complications]] are the leading | *[[Atherosclerosis]]:<ref name="pmid9839111">{{cite journal| author=Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM| title=Preventive foot care in people with diabetes. | journal=Diabetes Care | year= 1998 | volume= 21 | issue= 12 | pages= 2161-77 | pmid=9839111 | doi=10.2337/diacare.21.12.2161 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9839111 }} </ref><ref name="pmid6390204">{{cite journal| author=LoGerfo FW, Coffman JD| title=Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care. | journal=N Engl J Med | year= 1984 | volume= 311 | issue= 25 | pages= 1615-9 | pmid=6390204 | doi=10.1056/NEJM198412203112506 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6390204 }} </ref> | ||
**[[Atherosclerosis]] of the [[Limb (anatomy)|lower limb]] is 2 to 3 times more common in [[diabetes|diabetic]] [[patients]], compared to the normal population. | |||
**Investigations reported that [[atherosclerosis]] in [[diabetes|diabetic]] [[patients]] is more prominent in [[Anterior tibial artery|tibial]] and [[fibular arteries]] of the calf and [[artery|arteries]] of the [[foot]] are usually spared. | |||
**It usually occurs due to [[inflammation]] and consequently leads to accumulation of the [[foam cells]]. | |||
*[[Microvascular disease|Micro]] and [[Macrovascular disease|macrovascular]] [[Complication (medicine)|complications]] are one of the leading causes of [[diabetes|diabetic]] [[Complication (medicine)|complications]].<ref name="pmid22623440">{{cite journal| author=Venermo M, Vikatmaa P, Terasaki H, Sugano N| title=Vascular laboratory for critical limb ischaemia. | journal=Scand J Surg | year= 2012 | volume= 101 | issue= 2 | pages= 86-93 | pmid=22623440 | doi=10.1177/145749691210100203 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22623440 }} </ref> | |||
**[[[[Microvascular disease|Microvascular]] [[Complication (medicine)|complications]] cause [[skin]] damage, infection and impaired wound healing. Once a foot ulcer develops, peripheral vascular disease is the most important factor which may contribute to adverse outcomes. Vascular complications are like a positive feedback which worsen the skin and nerve damage in diabetes. | |||
*The vascular changes which are responsible for [[foot]] problems include stiff [[artery|arteries]] due to [[calcification]] of the [[Smooth muscle|smooth muscle cells]] in the [[artery|arterial wall]] (mediasclerosis). | |||
*Most of these changes are discovered by an impaired [[ABI|ankle brachial index]] ([[ABI]]). | |||
**The resting [[ABI]] is the ratio of the [[blood pressure]] in the [[Limb (anatomy)|lower limb]] to the [[blood pressure]] of the [[arms]]. It is calculated by dividing the [[systolic blood pressure]] of the [[ankle]] by the [[systolic blood pressure]] of the [[arm]]. | |||
**It is a non-invasive method to assess the [[Limb (anatomy)|lower extremty]] [[artery|arterial system]] and to detect the presence of [[artery|arterial]] occlusion [[disease]]. | |||
*Even in the presence of [[neuropathy|neuropathic]] [[diabetic foot|foot ulcers]], the reason of non healing [[wounds]] could be due to impaired [[blood]] supply to the [[Tissue (biology)|tissue]], which could be further augmented by [[antihypertensive]] [[medications]].<ref name="pmid22529027">{{cite journal| author=Alexiadou K, Doupis J| title=Management of diabetic foot ulcers. | journal=Diabetes Ther | year= 2012 | volume= 3 | issue= 1 | pages= 4 | pmid=22529027 | doi=10.1007/s13300-012-0004-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22529027 }} </ref>. | |||
[[Image:Microcirculation image.png|500px|Neuropathy and angiopathy in the foot have a positive feedback on each other]] | [[Image:Microcirculation image.png|500px|Neuropathy and angiopathy in the foot have a positive feedback on each other]] | ||
Revision as of 07:33, 10 February 2021
|
Diabetic foot Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Diabetic foot pathophysiology On the Web |
|
American Roentgen Ray Society Images of Diabetic foot pathophysiology |
|
Risk calculators and risk factors for Diabetic foot pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Anahita Deylamsalehi, M.D.[2]Vishnu Vardhan Serla M.B.B.S. [3]
Overview
Pathophysiology
Diabetic foot is an umbrella term for foot problems in patients with diabetes mellitus. There are numerous responsible pathogenesis, such as arterial abnormalities, diabetic neuropathy, delayed wound healing and being more vulnerable to infection or gangrene of the foot. The key components of diabetic foot are neuropathy, angiopathy and trauma. [1]
Neuropathy
- The most important cause of diabetic foot is neuropathy. Based on a study, more than 60% of cases of diabetic foot are due to neuropathy.[2]
- It involves roughly more than half of the patients with diabetes who are older than 60 years old.
- Peripheral neuropathy is usually profound at the point where it leads to formation of a foot ulcer.
- Some metabolic abnormalities due to hyperglycemia leads to ischemia of endoneurial microvessels. In a nutshell, these changes are most likely caused by a combination of factors listed below:
- High blood glucose
- Reactive oxygen species
- Vasculopathy
- Insufficient oxygenation of the nerves
- Presence of inflammation and autoimmunity due to diabetes
- Genetic factors
- Mechanical injury
- Smoking
- Alcohol abuse.
- Generalized symmetric distal polyneuropathy is the most common and widely recognized form of diabetic neuropathy that leads to diabetic foot. It may be either motor, autonomic or sensory, and can involve small fibers, large fibers or both.
- Motor nerve involvement:[3][4]
- Motor nerve involvement can lead to some mechanical changes in the foot of a diabetic patient due to loss of sufficient neural supply and alteration in natural anatomy of the foot. These mechanical changes cause more plantar pressure and higher risk of callus formation, which subsequently lead to higher rate of skin breakdown.
- Moreover, these anatomical changes usually result in wider and thicker foots, which no longer fit in patient's regular shoes and cause more trauma.
- Pathogenesis of some of these mechanical changes are listed below:
- Deprivation of neural supply to the intrinsic muscles of the foot → long flexor and extensor tendons imbalanced → flexion of the foot → high-arched foot and claw-toe deformity.
- Toes hyperextension → overriding of the metatarsal-phalangeal joints and downward displacement of metatarsal heads → Increased prominent of both.
- Toes hyperextension → distal displacement of metatarsal fat pads → altering the natural cushioning of these fat pads.
- Autonomic neuropathy:[5]
- Autonomic neuropathy leads to anhidrosis and impaired function of oil glands. The subsequent dryness of the skin results in higher chance of skin breakdown, ulcer formation and bacterial invasion.
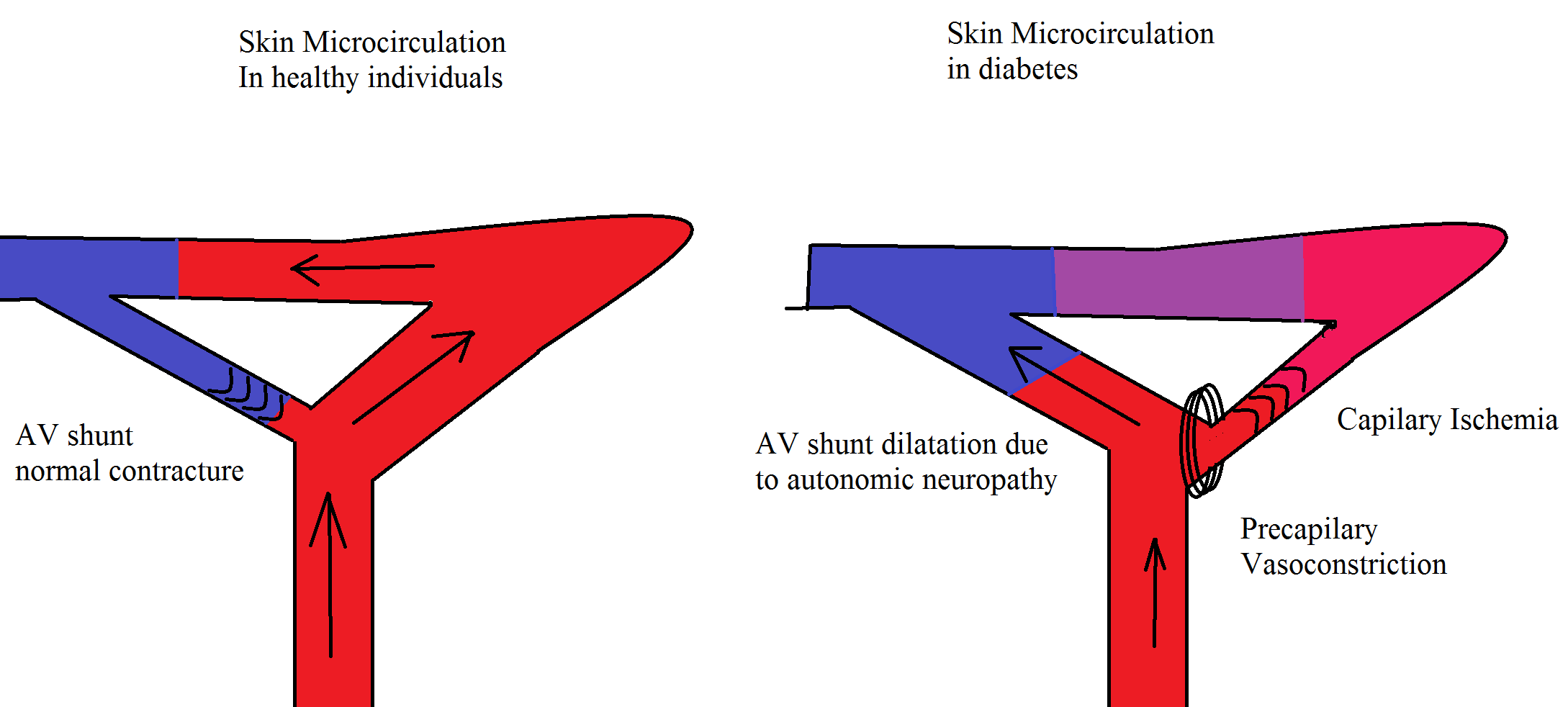
- Autonomic neuropathy also decreases the proper peripheral sympathetic vascular tone which can leads to higher blood flow and pressure in distal arteries. The aforementioned changes plus capillary basement membrane destruction lead to edema. Edema itself increases the risk of ulcer formation.
- Sensory neuropathy:
- Appropriate sensory system helps patients to notice the tiniest fissures or blisters on their skin. This early sensation make it possible for patients to take care of these skin defects and prevent further complications.
- Conversely, diabetic patients with Sensory neuropathy are more prone to ulcer formation and related complications, since they don't feel pain with ever-deepening ulcers.
- Motor nerve involvement:[3][4]
Ischemia
- Atherosclerosis:[6][7]
- Atherosclerosis of the lower limb is 2 to 3 times more common in diabetic patients, compared to the normal population.
- Investigations reported that atherosclerosis in diabetic patients is more prominent in tibial and fibular arteries of the calf and arteries of the foot are usually spared.
- It usually occurs due to inflammation and consequently leads to accumulation of the foam cells.
- Micro and macrovascular complications are one of the leading causes of diabetic complications.[8]
- [[Microvascular complications cause skin damage, infection and impaired wound healing. Once a foot ulcer develops, peripheral vascular disease is the most important factor which may contribute to adverse outcomes. Vascular complications are like a positive feedback which worsen the skin and nerve damage in diabetes.
- The vascular changes which are responsible for foot problems include stiff arteries due to calcification of the smooth muscle cells in the arterial wall (mediasclerosis).
- Most of these changes are discovered by an impaired ankle brachial index (ABI).
- The resting ABI is the ratio of the blood pressure in the lower limb to the blood pressure of the arms. It is calculated by dividing the systolic blood pressure of the ankle by the systolic blood pressure of the arm.
- It is a non-invasive method to assess the lower extremty arterial system and to detect the presence of arterial occlusion disease.
- Even in the presence of neuropathic foot ulcers, the reason of non healing wounds could be due to impaired blood supply to the tissue, which could be further augmented by antihypertensive medications.[9].
Trauma
- Trauma to the foot is frequently the trigger of diabetic foot ulcer development and repetitive trauma and pressure to the area prevent [Wound healing|healing]].[10]
- Excessive plantar pressure is related to limited joint mobility and foot deformities (such as charcot foot and hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated to an increased risk of ulceration.[9]
- Poor vision and sensory neuropathy further put diabetic patients at risk of foot ulceration, as they not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls.[9]
Genetics
Associated Conditions
Conditions associated with [disease name] include:
- [Condition 1]
- [Condition 2]
- [Condition 3]
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants (2002). "On your feet! Workshop on the diabetic foot". J Diabetes Complications. 16 (2): 183–94. PMID 12039404.
- ↑ Grunfeld C (1992). "Diabetic foot ulcers: etiology, treatment, and prevention". Adv Intern Med. 37: 103–32. PMID 1557993.
- ↑ Younger DS, Rosoklija G, Hays AP (1998). "Diabetic peripheral neuropathy". Semin Neurol. 18 (1): 95–104. doi:10.1055/s-2008-1040865. PMID 9562671.
- ↑ Borssén B, Bergenheim T, Lithner F (1990). "The epidemiology of foot lesions in diabetic patients aged 15-50 years". Diabet Med. 7 (5): 438–44. doi:10.1111/j.1464-5491.1990.tb01420.x. PMID 2142042.
- ↑ Ebenezer GJ, O'Donnell R, Hauer P, Cimino NP, McArthur JC, Polydefkis M (2011). "Impaired neurovascular repair in subjects with diabetes following experimental intracutaneous axotomy". Brain. 134 (Pt 6): 1853–63. doi:10.1093/brain/awr086. PMC 3140859. PMID 21616974.
- ↑ Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM (1998). "Preventive foot care in people with diabetes". Diabetes Care. 21 (12): 2161–77. doi:10.2337/diacare.21.12.2161. PMID 9839111.
- ↑ LoGerfo FW, Coffman JD (1984). "Current concepts. Vascular and microvascular disease of the foot in diabetes. Implications for foot care". N Engl J Med. 311 (25): 1615–9. doi:10.1056/NEJM198412203112506. PMID 6390204.
- ↑ Venermo M, Vikatmaa P, Terasaki H, Sugano N (2012). "Vascular laboratory for critical limb ischaemia". Scand J Surg. 101 (2): 86–93. doi:10.1177/145749691210100203. PMID 22623440.
- ↑ 9.0 9.1 9.2 Alexiadou K, Doupis J (2012). "Management of diabetic foot ulcers". Diabetes Ther. 3 (1): 4. doi:10.1007/s13300-012-0004-9. PMID 22529027.
- ↑ Noor S, Zubair M, Ahmad J (2015). "Diabetic foot ulcer--A review on pathophysiology, classification and microbial etiology". Diabetes Metab Syndr. 9 (3): 192–9. doi:10.1016/j.dsx.2015.04.007. PMID 25982677.