Pulmonary nodule differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Pulmonary_nodule]] | [[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Pulmonary_nodule]] | ||
{{CMG}}; {{AE}} {{Trusha}}, {{MV}} | {{CMG}}; {{AE}} {{Trusha}}, {{JE}}, {{MV}} | ||
==Overview== | ==Overview== | ||
| Line 62: | Line 62: | ||
* <5 mm [[Nodule (medicine)|nodule]] | * <5 mm [[Nodule (medicine)|nodule]] | ||
* [[Ground glass opacification on CT|Ground glass]] | * [[Ground glass opacification on CT|Ground glass]] | ||
[[File: CT of ground glass lung nodule.png|x200px|thumb|CT showing Ground glass opacity nodule. (Picture courtesy: [https://en.wikipedia.org/wiki/Lung_nodule Wikipedia])]] | |||
| style="background: #F5F5F5; padding: 5px;" |[[Fat]] | | style="background: #F5F5F5; padding: 5px;" |[[Fat]] | ||
| Line 75: | Line 76: | ||
* [[Growth rate]] > 18 months | * [[Growth rate]] > 18 months | ||
* [[Cavity]] wall thickness of 1 mm | * [[Cavity]] wall thickness of 1 mm | ||
[[File:Pulmonary hamartoma.jpeg|x200px|thumb|CT showing Pulmonary [[hamartoma]] with well-defined smooth border. Case courtesy of Dr Domenico Nicoletti (Picture courtesy: [https://radiopaedia.org/cases/pulmonary-hamartoma-11?lang=gb Radiopaedia])]] | |||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
* N/A | * N/A | ||
| Line 111: | Line 113: | ||
* Single or multiple | * Single or multiple | ||
* Small or > 2 cm of size | * Small or > 2 cm of size | ||
[[File: Lungca.jpg|x200px|thumb|CT showing bronchogenic carcinoma. Case courtesy of Dr Ahmed Abdrabou (Picture courtesy: [https://radiopaedia.org/cases/bronchogenic-carcinoma-with-upper-lobe-collapse?lang=gb Radiopaedia])]] | |||
| style="background: #F5F5F5; padding: 5px;" |[[Calcification]] | | style="background: #F5F5F5; padding: 5px;" |[[Calcification]] | ||
* [[Amorphous solid|Amorphous]] | * [[Amorphous solid|Amorphous]] | ||
| Line 117: | Line 120: | ||
* Stippled or [[Eccentric Lesion|eccentric]] | * Stippled or [[Eccentric Lesion|eccentric]] | ||
[[Cavity]] | [[Cavity]] | ||
[[Ulcer|Ulceration]] | [[Ulcer|Ulceration]] | ||
[[File: | [[File:Cavitatory bronchogenic lungca.jpeg|x200px|thumb|CT showing bronchogenic [[lung cancer]] with cavity Case courtesy of Dr Ahmed Abdrabou (Picture courtesy: [https://www.wikidoc.org/index.php/File:Cavitatory_bronchogenic_lungca.jpeg Radiopaedia])]] | ||
* | * | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
Latest revision as of 00:49, 22 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Trusha Tank, M.D.[2], Joanna Ekabua, M.D. [3], Maria Fernanda Villarreal, M.D. [4]
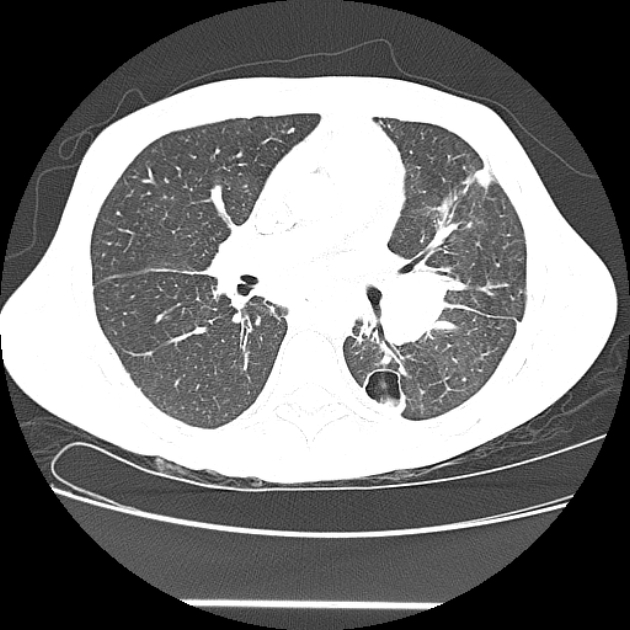
Overview
Pulmonary nodule may be differentiated according to imaging (size, border characteristics, and attenuation), histological, and clinical features, from other diseases that demonstrate similar imaging findings. Common differential diagnoses of pulmonary nodule include hamartoma, granulomas, rheumatoid nodule, and metastatic lesions.
Differentiating Pulmonary Nodule from Other Diseases
- The table below summarizes the findings that differentiate pulmonary nodule from other conditions that cause similar radiological findings on CT scan of the chest.[1][2]
| ABBREVIATIONS:N/A: Not available , SOB: Shortness of breath, M/C: Most common | ||||||||||||||
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard | Additional findings | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical exam | |||||||||||||
| Lab Findings | CT scan | Histopathology | ||||||||||||
| Productive cough | Hemoptysis | Weight loss | SOB | Fever | Other | Auscultation | Sputum analysis | Nodule | Nodule content | Other findings | ||||
| Pulmonary Nodule(benign) | - | - | - | - | - |
|
|
|
 |
Fat
Types:
|
 |
|
|
|
| Pulmonary Nodule (malignant) | ++ | ++ | ++ | + | - |
|
 |
Calcification
 |
|
|
|
|||
| Diseases | Productive cough | Hemoptysis | Weight loss | SOB | Fever | Other | Auscultation | Sputum analysis | Nodule | Content | Other findings | Histopathology | Gold standard | Additional findings |
| Abscess | ++ | - | - | + | ++ |
|
 |
.
|
|
|||||
| Septic pulmonary | - | - | - | ++ | ++ |
|
|
 |
 |
|
|
| ||
| Fungal | +/- | + | - | + | + |
|
 |
|
|
| ||||
| Parasites | +/- | +/- | +/- | _ | + |
|
|
Cyst:
Coin lesion:
|
 |
| ||||
| Diseases | Productive cough | Hemoptysis | Weight loss | SOB | Fever | Other | Auscultation | Sputum analysis | Nodule | Content | Other findings | Histopathology | Gold standard | Additional findings |
| Mycobacterial infections | + | + | + | ++ | +/- |
|
|
 |
|
|
|
| ||
| Chronic inflammatory conditions | +/- | + | - | + | - |
|
 |
|
|
 |
||||
| Diseases | Productive cough | Hemoptysis | Weight loss | SOB | Fever | Other | Auscultation | Sputum analysis | Nodule | Content | Other findings | Histopathology | Gold standard | Additional findings |
| Pulmonary AVMs | - | +/- | - | + | - |
|
 |
 |
|
 | ||||
| Pneumoconiosis | + | - | + | + | - |
|
|
 |
 |
 |
| |||
| ABBREVIATIONS:N/A: Not available , SOB: Shortness of breath, M/C: Most common | ||||||||||||||
References
- ↑ Ost D, Fein AM, Feinsilver SH (2003). "Clinical practice. The solitary pulmonary nodule". N. Engl. J. Med. 348 (25): 2535–42. doi:10.1056/NEJMcp012290. PMID 12815140. Unknown parameter
|month=ignored (help) - ↑ McWilliams A, Tammemagi MC, Mayo JR, et. al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013 Sep 5;369(10):910-9. doi:10.1056/NEJMoa1214726.
- ↑ 3.0 3.1 Khan AN, Al-Jahdali HH, Irion KL, Arabi M, Koteyar SS (October 2011). "Solitary pulmonary nodule: A diagnostic algorithm in the light of current imaging technique". Avicenna J Med. 1 (2): 39–51. doi:10.4103/2231-0770.90915. PMC 3507065. PMID 23210008.
- ↑ Li J, Xia T, Yang X, Dong X, Liang J, Zhong N, Guan Y (April 2018). "Malignant solitary pulmonary nodules: assessment of mass growth rate and doubling time at follow-up CT". J Thorac Dis. 10 (Suppl 7): S797–S806. doi:10.21037/jtd.2018.04.25. PMC 5945695. PMID 29780626.
- ↑ Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D (August 2015). "Lung abscess-etiology, diagnostic and treatment options". Ann Transl Med. 3 (13): 183. doi:10.3978/j.issn.2305-5839.2015.07.08. PMC 4543327. PMID 26366400.
- ↑ Chang E, Lee KH, Yang KY, Lee YC, Perng RP (2009). "Septic pulmonary embolism associated with a peri-proctal abscess in an immunocompetent host". BMJ Case Rep. 2009. doi:10.1136/bcr.07.2008.0592. PMC 3029652. PMID 21686732.
- ↑ Chong, Semin; Lee, Kyung Soo; Yi, Chin A; Chung, Myung Jin; Kim, Tae Sung; Han, Joungho (2006). "Pulmonary fungal infection: Imaging findings in immunocompetent and immunocompromised patients". European Journal of Radiology. 59 (3): 371–383. doi:10.1016/j.ejrad.2006.04.017. ISSN 0720-048X.
- ↑ Kunst H, Mack D, Kon OM, Banerjee AK, Chiodini P, Grant A (June 2011). "Parasitic infections of the lung: a guide for the respiratory physician". Thorax. 66 (6): 528–36. doi:10.1136/thx.2009.132217. PMID 20880867.
- ↑ Ryu YJ (April 2015). "Diagnosis of pulmonary tuberculosis: recent advances and diagnostic algorithms". Tuberc Respir Dis (Seoul). 78 (2): 64–71. doi:10.4046/trd.2015.78.2.64. PMC 4388902. PMID 25861338.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ Kubaisi B, Abu Samra K, Foster CS (May 2016). "Granulomatosis with polyangiitis (Wegener's disease): An updated review of ocular disease manifestations". Intractable Rare Dis Res. 5 (2): 61–9. doi:10.5582/irdr.2016.01014. PMC 4869584. PMID 27195187.
- ↑ Khurshid I, Downie GH (April 2002). "Pulmonary arteriovenous malformation". Postgrad Med J. 78 (918): 191–7. PMC 1742331. PMID 11930021.