ST elevation myocardial infarction coronary angiography: Difference between revisions
(/* Coronary Angiography in Patients Who Initially Were Managed With Fibrinolytic Therapy or Who Did Not Receive Reperfusion (DO NOT EDIT){{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, et al. |title=2013 ACCF/AHA Guideline for the Manag...) |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ST elevation myocardial infarction}} | {{ST elevation myocardial infarction}} | ||
{{CMG}}; | {{CMG}};{{AE}} {{CZ}} | ||
==Overview== | ==Overview== | ||
| Line 37: | Line 37: | ||
==Interpreting the Coronary Angiogram== | ==Interpreting the Coronary Angiogram== | ||
=== Pathophysiology of Reperfusion=== | === Pathophysiology of Reperfusion=== | ||
The Importance of Restoring and Sustaining Complete Epicardial and Myocardial Perfusion: | |||
Recently, it has become recognized that it is necessary but not sufficient to restore epicardial flow in ST elevation MI. Not all TIMI grade 3 flow is created equally. In addition to epicardial flow, myocardial perfusion must be restored as well. This has been demonstrated in both myocardial contrast echo studies as well as angiographic studies<ref name="pmid4038784">{{cite journal |author= |title=The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group |journal=N. Engl. J. Med. |volume=312 |issue=14 |pages=932–6 |year=1985 |month=April |pmid=4038784 |doi= |url=}}</ref><ref name="pmid7895348">{{cite journal |author=Simes RJ, Topol EJ, Holmes DR, ''et al'' |title=Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators |journal=Circulation |volume=91 |issue=7 |pages=1923–8 |year=1995 |month=April |pmid=7895348 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=7895348}}</ref><ref name="pmid8232430">{{cite journal |author= |title=The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators |journal=N. Engl. J. Med. |volume=329 |issue=22 |pages=1615–22 |year=1993 |month=November |pmid=8232430 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8232430&promo=ONFLNS19}}</ref><ref name="pmid8473646">{{cite journal |author=Vogt A, von Essen R, Tebbe U, Feuerer W, Appel KF, Neuhaus KL |title=Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies |journal=J. Am. Coll. Cardiol. |volume=21 |issue=6 |pages=1391–5 |year=1993 |month=May |pmid=8473646 |doi= |url=}}</ref><ref name="pmid1729317">{{cite journal |author=Karagounis L, Sorensen SG, Menlove RL, Moreno F, Anderson JL |title=Does thrombolysis in myocardial infarction (TIMI) perfusion grade 2 represent a mostly patent artery or a mostly occluded artery? Enzymatic and electrocardiographic evidence from the TEAM-2 study. Second Multicenter Thrombolysis Trial of Eminase in Acute Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=19 |issue=1 |pages=1–10 |year=1992 |month=January |pmid=1729317 |doi= |url=}}</ref><ref name="pmid8504495">{{cite journal |author=Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL |title=TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolysis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM-3 Study |journal=Circulation |volume=87 |issue=6 |pages=1829–39 |year=1993 |month=June |pmid=8504495 |doi= |url=}}</ref><ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref><ref name="pmid10637197">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, ''et al'' |title=Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs |journal=Circulation |volume=101 |issue=2 |pages=125–30 |year=2000 |month=January |pmid=10637197 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10637197}}</ref><ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref><ref name="pmid11804979">{{cite journal |author=Angeja BG, Gunda M, Murphy SA, ''et al'' |title=TIMI myocardial perfusion grade and ST segment resolution: association with infarct size as assessed by single photon emission computed tomography imaging |journal=Circulation |volume=105 |issue=3 |pages=282–5 |year=2002 |month=January |pmid=11804979 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11804979}}</ref><ref name="pmid1572028">{{cite journal |author=Ito H, Tomooka T, Sakai N, ''et al'' |title=Lack of myocardial perfusion immediately after successful thrombolysis. A predictor of poor recovery of left ventricular function in anterior myocardial infarction |journal=Circulation |volume=85 |issue=5 |pages=1699–705 |year=1992 |month=May |pmid=1572028 |doi= |url=}}</ref><ref name="pmid8548892">{{cite journal |author=Ito H, Maruyama A, Iwakura K, ''et al'' |title=Clinical implications of the 'no reflow' phenomenon. A predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction |journal=Circulation |volume=93 |issue=2 |pages=223–8 |year=1996 |month=January |pmid=8548892 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8548892}}</ref>. As a result of this new understanding, the goal of reperfusion therapies has shifted to include reperfusion downstream at the level of capillary bed, and it might be more appropriate that the current reperfusion hypothesis now be termed "the time dependent open muscle hypothesis." This wiki article reviews the angiographic methods used to evaluate myocardial ischemia and infarction and discusses the insights into the pathophysiology of acute coronary syndromes provided by these angiographic indexes of coronary artery blood flow and myocardial perfusion. | |||
Recently, it has become recognized that it is necessary but not sufficient to restore epicardial flow in ST elevation MI. Not all TIMI grade 3 flow is created equally. In addition to epicardial flow, myocardial perfusion must be restored as well. This has been demonstrated in both myocardial contrast echo studies as well as angiographic studies<ref name="pmid4038784">{{cite journal |author= |title=The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group |journal=N. Engl. J. Med. |volume=312 |issue=14 |pages=932–6 |year=1985 |month=April |pmid=4038784 |doi= |url=}}</ref><ref name="pmid7895348">{{cite journal |author=Simes RJ, Topol EJ, Holmes DR, ''et al'' |title=Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators |journal=Circulation |volume=91 |issue=7 |pages=1923–8 |year=1995 |month=April |pmid=7895348 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=7895348}}</ref><ref name="pmid8232430">{{cite journal |author= |title=The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators |journal=N. Engl. J. Med. |volume=329 |issue=22 |pages=1615–22 |year=1993 |month=November |pmid=8232430 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8232430&promo=ONFLNS19}}</ref><ref name="pmid8473646">{{cite journal |author=Vogt A, von Essen R, Tebbe U, Feuerer W, Appel KF, Neuhaus KL |title=Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies |journal=J. Am. Coll. Cardiol. |volume=21 |issue=6 |pages=1391–5 |year=1993 |month=May |pmid=8473646 |doi= |url=}}</ref><ref name="pmid1729317">{{cite journal |author=Karagounis L, Sorensen SG, Menlove RL, Moreno F, Anderson JL |title=Does thrombolysis in myocardial infarction (TIMI) perfusion grade 2 represent a mostly patent artery or a mostly occluded artery? Enzymatic and electrocardiographic evidence from the TEAM-2 study. Second Multicenter Thrombolysis Trial of Eminase in Acute Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=19 |issue=1 |pages=1–10 |year=1992 |month=January |pmid=1729317 |doi= |url=}}</ref><ref name="pmid8504495">{{cite journal |author=Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL |title=TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolysis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM-3 Study |journal=Circulation |volume=87 |issue=6 |pages=1829–39 |year=1993 |month=June |pmid=8504495 |doi= |url=}}</ref><ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref><ref name="pmid10637197">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, ''et al'' |title=Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs |journal=Circulation |volume=101 |issue=2 |pages=125–30 |year=2000 |month=January |pmid=10637197 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10637197}}</ref><ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref><ref name="pmid11804979">{{cite journal |author=Angeja BG, Gunda M, Murphy SA, ''et al'' |title=TIMI myocardial perfusion grade and ST segment resolution: association with infarct size as assessed by single photon emission computed tomography imaging |journal=Circulation |volume=105 |issue=3 |pages=282–5 |year=2002 |month=January |pmid=11804979 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11804979}}</ref><ref name="pmid1572028">{{cite journal |author=Ito H, Tomooka T, Sakai N, ''et al'' |title=Lack of myocardial perfusion immediately after successful thrombolysis. A predictor of poor recovery of left ventricular function in anterior myocardial infarction |journal=Circulation |volume=85 |issue=5 |pages=1699–705 |year=1992 |month=May |pmid=1572028 |doi= |url=}}</ref><ref name="pmid8548892">{{cite journal |author=Ito H, Maruyama A, Iwakura K, ''et al'' |title=Clinical implications of the 'no reflow' phenomenon. A predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction |journal=Circulation |volume=93 |issue=2 |pages=223–8 |year=1996 |month=January |pmid=8548892 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8548892}}</ref>. As a result of this new understanding, the goal of reperfusion therapies has shifted to include reperfusion downstream at the level of capillary bed, and it might be more appropriate that the current reperfusion hypothesis now be termed "the time dependent open muscle hypothesis." This wiki article reviews the angiographic methods used to evaluate myocardial ischemia and infarction and discusses the insights into the pathophysiology of acute coronary syndromes provided by these angiographic indexes of coronary artery blood flow and myocardial perfusion. | |||
===TIMI Flow Grades (TFGs)=== | ===TIMI Flow Grades (TFGs)=== | ||
The Thrombolysis In Myocardial Infarction (TIMI) flow grade classification scheme has been widely used to assess coronary blood flow in acute coronary syndromes <ref name="pmid4038784">{{cite journal |author= |title=The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group |journal=N. Engl. J. Med. |volume=312 |issue=14 |pages=932–6 |year=1985 |month=April |pmid=4038784 |doi= |url=}}</ref>. TFG 0 means the artery is closed; TFG 1 means that dye penetrates the stenosis but does not reach the downstream bed; TFG 2 means that flow is slow down the artery and TFG 3 means that normal flow has been restored. The association of the TFGs with clinical outcomes (including mortality) has been well documented <ref name="pmid7895348">{{cite journal |author=Simes RJ, Topol EJ, Holmes DR, ''et al'' |title=Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators |journal=Circulation |volume=91 |issue=7 |pages=1923–8 |year=1995 |month=April |pmid=7895348 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=7895348}}</ref><ref name="pmid8232430">{{cite journal |author= |title=The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators |journal=N. Engl. J. Med. |volume=329 |issue=22 |pages=1615–22 |year=1993 |month=November |pmid=8232430 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8232430&promo=ONFLNS19}}</ref><ref name="pmid8473646">{{cite journal |author=Vogt A, von Essen R, Tebbe U, Feuerer W, Appel KF, Neuhaus KL |title=Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies |journal=J. Am. Coll. Cardiol. |volume=21 |issue=6 |pages=1391–5 |year=1993 |month=May |pmid=8473646 |doi= |url=}}</ref><ref name="pmid1729317">{{cite journal |author=Karagounis L, Sorensen SG, Menlove RL, Moreno F, Anderson JL |title=Does thrombolysis in myocardial infarction (TIMI) perfusion grade 2 represent a mostly patent artery or a mostly occluded artery? Enzymatic and electrocardiographic evidence from the TEAM-2 study. Second Multicenter Thrombolysis Trial of Eminase in Acute Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=19 |issue=1 |pages=1–10 |year=1992 |month=January |pmid=1729317 |doi= |url=}}</ref><ref name="pmid8504495">{{cite journal |author=Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL |title=TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolysis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM-3 Study |journal=Circulation |volume=87 |issue=6 |pages=1829–39 |year=1993 |month=June |pmid=8504495 |doi= |url=}}</ref><ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref>. | The Thrombolysis In Myocardial Infarction (TIMI) flow grade classification scheme has been widely used to assess coronary blood flow in acute coronary syndromes <ref name="pmid4038784">{{cite journal |author= |title=The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group |journal=N. Engl. J. Med. |volume=312 |issue=14 |pages=932–6 |year=1985 |month=April |pmid=4038784 |doi= |url=}}</ref>. TFG 0 means the artery is closed; TFG 1 means that dye penetrates the stenosis but does not reach the downstream bed; TFG 2 means that flow is slow down the artery and TFG 3 means that normal flow has been restored. The association of the TFGs with clinical outcomes (including mortality) has been well documented <ref name="pmid7895348">{{cite journal |author=Simes RJ, Topol EJ, Holmes DR, ''et al'' |title=Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators |journal=Circulation |volume=91 |issue=7 |pages=1923–8 |year=1995 |month=April |pmid=7895348 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=7895348}}</ref><ref name="pmid8232430">{{cite journal |author= |title=The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators |journal=N. Engl. J. Med. |volume=329 |issue=22 |pages=1615–22 |year=1993 |month=November |pmid=8232430 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=8232430&promo=ONFLNS19}}</ref><ref name="pmid8473646">{{cite journal |author=Vogt A, von Essen R, Tebbe U, Feuerer W, Appel KF, Neuhaus KL |title=Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies |journal=J. Am. Coll. Cardiol. |volume=21 |issue=6 |pages=1391–5 |year=1993 |month=May |pmid=8473646 |doi= |url=}}</ref><ref name="pmid1729317">{{cite journal |author=Karagounis L, Sorensen SG, Menlove RL, Moreno F, Anderson JL |title=Does thrombolysis in myocardial infarction (TIMI) perfusion grade 2 represent a mostly patent artery or a mostly occluded artery? Enzymatic and electrocardiographic evidence from the TEAM-2 study. Second Multicenter Thrombolysis Trial of Eminase in Acute Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=19 |issue=1 |pages=1–10 |year=1992 |month=January |pmid=1729317 |doi= |url=}}</ref><ref name="pmid8504495">{{cite journal |author=Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL |title=TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolysis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM-3 Study |journal=Circulation |volume=87 |issue=6 |pages=1829–39 |year=1993 |month=June |pmid=8504495 |doi= |url=}}</ref><ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref>. | ||
* TIMI Flow Grade 0: | * TIMI Flow Grade 0: The artery is blocked. | ||
* TIMI Flow Grade 1: This category is subdivided into: | * TIMI Flow Grade 1: This category is subdivided into: | ||
:* 1.0: dye minimally leaks past the area of obstruction. [http://www.wikidoc.org/images/1/14/LAD_1.swf TIMI Flow Grade 1 - Left Anterior Descending Artery] | :* 1.0: dye minimally leaks past the area of obstruction. [http://www.wikidoc.org/images/1/14/LAD_1.swf TIMI Flow Grade 1 - Left Anterior Descending Artery] | ||
| Line 51: | Line 51: | ||
:* 2.0: TIMI 2 slow flow, dye markedly delayed in opacifying distal vasculature. [http://www.wikidoc.org/images/archive/b/b2/20080125205849%21LAD_2.swf TIMI Flow Grade 2 - Left Anterior Descending Artery] | :* 2.0: TIMI 2 slow flow, dye markedly delayed in opacifying distal vasculature. [http://www.wikidoc.org/images/archive/b/b2/20080125205849%21LAD_2.swf TIMI Flow Grade 2 - Left Anterior Descending Artery] | ||
:* 2.5: TIMI 2 fast flow, dye minimally delayed in opacifying distal vasculature. [http://www.wikidoc.org/images/3/33/2.5TFG.swf TIMI Flow Grade 2.5 - Right Coronary Artery] | :* 2.5: TIMI 2 fast flow, dye minimally delayed in opacifying distal vasculature. [http://www.wikidoc.org/images/3/33/2.5TFG.swf TIMI Flow Grade 2.5 - Right Coronary Artery] | ||
* TIMI Flow Grade 3: | * TIMI Flow Grade 3: Normal flow in the artery. | ||
The association of the TFGs with mortality must be interpreted with caution as there are several confounders: | |||
*The majority of TIMI grade 2 flow is observed in the left anterior descending artery (LAD) territory, whereas the majority of TIMI grade 3 flow is observed in the right coronary artery (RCA)<ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. Thus, the improved mortality observed among patients with TIMI grade 3 flow may be explained at least in part by the fact that inferior myocardial infarction (MI) location is associated with a lower mortality rate <ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. | *The majority of TIMI grade 2 flow is observed in the left anterior descending artery (LAD) territory, whereas the majority of TIMI grade 3 flow is observed in the right coronary artery (RCA)<ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. Thus, the improved mortality observed among patients with TIMI grade 3 flow may be explained at least in part by the fact that inferior myocardial infarction (MI) location is associated with a lower mortality rate <ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. | ||
*The clinical improvement associated with TIMI grade 3 flow may have be nonlinear. For example, greater clinical benefits may be observed if a closed artery (TFG 0/1) is opened (TFG 2) compared with the improvement that might occur if an artery with TFG 2 is converted to TFG 3 flow. | *The clinical improvement associated with TIMI grade 3 flow may have be nonlinear. For example, greater clinical benefits may be observed if a closed artery (TFG 0/1) is opened (TFG 2) compared with the improvement that might occur if an artery with TFG 2 is converted to TFG 3 flow. | ||
*As more arteries with TFG 2 flow are treated with adjunctive percutaneous coronary intervention (PCI), the prognosis associated with this flow grade may improve. The fact that patients who were treated with an inferior fibrinolytic monotherapy strategy faired so well in GUSTO V may be explained in part by the fact that these patients underwent PCI more often<ref name="pmid11551872">{{cite journal |author=Hudson MP, Granger CB, Topol EJ, ''et al'' |title=Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials |journal=Circulation |volume=104 |issue=11 |pages=1229–35 |year=2001 |month=September |pmid=11551872 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11551872}}</ref>. Two-year follow-up in more recent studies indicates that the survival advantage of TFG 3 flow over TFG 2 flow at 2 years may not be as great as it once was in the era before aggressive utilization of rescue and adjunctive (PCI)<ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref>. | *As more arteries with TFG 2 flow are treated with adjunctive percutaneous coronary intervention (PCI), the prognosis associated with this flow grade may improve. The fact that patients who were treated with an inferior fibrinolytic monotherapy strategy faired so well in GUSTO V may be explained in part by the fact that these patients underwent PCI more often<ref name="pmid11551872">{{cite journal |author=Hudson MP, Granger CB, Topol EJ, ''et al'' |title=Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials |journal=Circulation |volume=104 |issue=11 |pages=1229–35 |year=2001 |month=September |pmid=11551872 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11551872}}</ref>. Two-year follow-up in more recent studies indicates that the survival advantage of TFG 3 flow over TFG 2 flow at 2 years may not be as great as it once was in the era before aggressive utilization of rescue and adjunctive (PCI)<ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref>. | ||
===Reocclusion=== | ===Reocclusion=== | ||
| Line 66: | Line 66: | ||
Some of the advantages of the TIMI frame count method are as follows. In contrast to the TFG classification scheme, the CTFC is quantitative rather than qualitative, it is objective rather than subjective, it is a continuous rather than a categorical variable, and it is reproducible<ref name="pmid8598078">{{cite journal|author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. The CTFC demonstrates that flow is not divided into arbitrary slow and fast categories, but rather coronary blood flow is unimodally distributed as a continuous variable<ref name="pmid8598078">{{cite journal|author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. The CTFC has been shown to be quite reproducible with a 1- to 2-frame difference between observers <ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref><ref name="pmid10363873">{{cite journal |author=Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV |title=Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method |journal=Am. J. Cardiol. |volume=83 |issue=11 |pages=1562–5, A7 |year=1999 |month=June |pmid=10363873 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00149-6}}</ref><ref name="pmid10704161">{{cite journal |author=Stankovic G, Manginas A, Voudris V, ''et al'' |title=Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio |journal=Circulation |volume=101 |issue=9 |pages=962–8 |year=2000 |month=March |pmid=10704161 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10704161}}</ref><ref name="pmid12586269">{{cite journal |author=Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A |title=Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters |journal=Am. J. Cardiol. |volume=91 |issue=4 |pages=466–9 |year=2003 |month=February |pmid=12586269 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914902032502}}</ref><ref name="pmid11870267">{{cite journal |author=Umman B, Nisanci Y, Sezer M, ''et al'' |title=The relationship between corrected TIMI frame count and myocardial fractional flow reserve |journal=J Invasive Cardiol |volume=14 |issue=3 |pages=125–8 |year=2002 |month=March|pmid=11870267}}</ref><ref name="pmid9527071">{{cite journal |author=French JK, Ellis CJ, Webber BJ, ''et al'' |title=Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity |journal=Am. J. Cardiol. |volume=81 |issue=6 |pages=665–71 |year=1998 |month=March |pmid=9527071 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997010047}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11275924">{{cite journal |author=Amos DJ, French JK, Andrews J, ''et al'' |title=Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy |journal=Am. Heart J. |volume=141 |issue=4 |pages=586–91 |year=2001 |month=April |pmid=11275924 |doi=10.1067/mhj.2001.113393 |url=}}</ref><ref name="pmid12464786">{{cite journal |author=Sahin M, Basoglu T, Canbaz F, Elcik M, Kosus A |title=The value of the TIMI frame count method in the diagnosis of coronary no-reflow: a comparison with myocardial perfusion SPECT in patients with acute myocardial infarction |journal=Nucl Med Commun |volume=23 |issue=12 |pages=1205–10 |year=2002 |month=December |pmid=12464786 |doi=10.1097/01.mnm.0000046213.83338.9e |url=}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11023929">{{cite journal |author=Topol EJ, Ohman EM, Armstrong PW, ''et al'' |title=Survival outcomes 1 year after reperfusion therapy with either alteplase or reteplase for acute myocardial infarction: results from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) III Trial |journal=Circulation |volume=102 |issue=15 |pages=1761–5 |year=2000 |month=October |pmid=11023929 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11023929}}</ref>. The CTFC is also highly correlated with other measures of flow such as Doppler velocity wire measures of coronary flow reserve, distal velocity, average peak velocity, and volumetric flow, <ref name="pmid10363873">{{cite journal |author=Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV |title=Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method |journal=Am. J. Cardiol. |volume=83 |issue=11 |pages=1562–5, A7 |year=1999 |month=June |pmid=10363873 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00149-6}}</ref><ref name="pmid10704161">{{cite journal |author=Stankovic G, Manginas A, Voudris V, ''et al'' |title=Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio |journal=Circulation |volume=101 |issue=9 |pages=962–8 |year=2000 |month=March |pmid=10704161 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10704161}}</ref><ref name="pmid12586269">{{cite journal |author=Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A |title=Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters |journal=Am. J. Cardiol. |volume=91 |issue=4 |pages=466–9 |year=2003 |month=February |pmid=12586269 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914902032502}}</ref> as well as fractional flow reserve (r=0.85)<ref name="pmid11870267">{{cite journal |author=Umman B, Nisanci Y, Sezer M, ''et al'' |title=The relationship between corrected TIMI frame count and myocardial fractional flow reserve |journal=J Invasive Cardiol |volume=14 |issue=3 |pages=125–8 |year=2002 |month=March |pmid=11870267 |doi= |url=}}</ref>. | Some of the advantages of the TIMI frame count method are as follows. In contrast to the TFG classification scheme, the CTFC is quantitative rather than qualitative, it is objective rather than subjective, it is a continuous rather than a categorical variable, and it is reproducible<ref name="pmid8598078">{{cite journal|author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. The CTFC demonstrates that flow is not divided into arbitrary slow and fast categories, but rather coronary blood flow is unimodally distributed as a continuous variable<ref name="pmid8598078">{{cite journal|author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref>. The CTFC has been shown to be quite reproducible with a 1- to 2-frame difference between observers <ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref><ref name="pmid10363873">{{cite journal |author=Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV |title=Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method |journal=Am. J. Cardiol. |volume=83 |issue=11 |pages=1562–5, A7 |year=1999 |month=June |pmid=10363873 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00149-6}}</ref><ref name="pmid10704161">{{cite journal |author=Stankovic G, Manginas A, Voudris V, ''et al'' |title=Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio |journal=Circulation |volume=101 |issue=9 |pages=962–8 |year=2000 |month=March |pmid=10704161 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10704161}}</ref><ref name="pmid12586269">{{cite journal |author=Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A |title=Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters |journal=Am. J. Cardiol. |volume=91 |issue=4 |pages=466–9 |year=2003 |month=February |pmid=12586269 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914902032502}}</ref><ref name="pmid11870267">{{cite journal |author=Umman B, Nisanci Y, Sezer M, ''et al'' |title=The relationship between corrected TIMI frame count and myocardial fractional flow reserve |journal=J Invasive Cardiol |volume=14 |issue=3 |pages=125–8 |year=2002 |month=March|pmid=11870267}}</ref><ref name="pmid9527071">{{cite journal |author=French JK, Ellis CJ, Webber BJ, ''et al'' |title=Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity |journal=Am. J. Cardiol. |volume=81 |issue=6 |pages=665–71 |year=1998 |month=March |pmid=9527071 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997010047}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11275924">{{cite journal |author=Amos DJ, French JK, Andrews J, ''et al'' |title=Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy |journal=Am. Heart J. |volume=141 |issue=4 |pages=586–91 |year=2001 |month=April |pmid=11275924 |doi=10.1067/mhj.2001.113393 |url=}}</ref><ref name="pmid12464786">{{cite journal |author=Sahin M, Basoglu T, Canbaz F, Elcik M, Kosus A |title=The value of the TIMI frame count method in the diagnosis of coronary no-reflow: a comparison with myocardial perfusion SPECT in patients with acute myocardial infarction |journal=Nucl Med Commun |volume=23 |issue=12 |pages=1205–10 |year=2002 |month=December |pmid=12464786 |doi=10.1097/01.mnm.0000046213.83338.9e |url=}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11023929">{{cite journal |author=Topol EJ, Ohman EM, Armstrong PW, ''et al'' |title=Survival outcomes 1 year after reperfusion therapy with either alteplase or reteplase for acute myocardial infarction: results from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) III Trial |journal=Circulation |volume=102 |issue=15 |pages=1761–5 |year=2000 |month=October |pmid=11023929 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11023929}}</ref>. The CTFC is also highly correlated with other measures of flow such as Doppler velocity wire measures of coronary flow reserve, distal velocity, average peak velocity, and volumetric flow, <ref name="pmid10363873">{{cite journal |author=Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV |title=Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method |journal=Am. J. Cardiol. |volume=83 |issue=11 |pages=1562–5, A7 |year=1999 |month=June |pmid=10363873 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00149-6}}</ref><ref name="pmid10704161">{{cite journal |author=Stankovic G, Manginas A, Voudris V, ''et al'' |title=Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio |journal=Circulation |volume=101 |issue=9 |pages=962–8 |year=2000 |month=March |pmid=10704161 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10704161}}</ref><ref name="pmid12586269">{{cite journal |author=Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A |title=Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters |journal=Am. J. Cardiol. |volume=91 |issue=4 |pages=466–9 |year=2003 |month=February |pmid=12586269 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914902032502}}</ref> as well as fractional flow reserve (r=0.85)<ref name="pmid11870267">{{cite journal |author=Umman B, Nisanci Y, Sezer M, ''et al'' |title=The relationship between corrected TIMI frame count and myocardial fractional flow reserve |journal=J Invasive Cardiol |volume=14 |issue=3 |pages=125–8 |year=2002 |month=March |pmid=11870267 |doi= |url=}}</ref>. | ||
Several technical and physiological variables may impact the CTFC<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref><ref name="pmid9604968">{{cite journal |author=Dodge JT, Rizzo M, Nykiel M, ''et al'' |title=Impact of injection rate on the Thrombolysis in Myocardial Infarction (TIMI) trial frame count |journal=Am. J. Cardiol. |volume=81 |issue=10 |pages=1268–70 |year=1998 |month=May |pmid=9604968 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(98)00138-6}}</ref><ref name="pmid11113418">{{cite journal |author=Gibson CM, Anshelevich M, Murphy S, ''et al'' |title=Impact of injections during diagnostic coronary arteriography on coronary patency in the setting of acute myocardial infarction from the TIMI trials. Thrombolysis In Myocardial Infarction |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1378–9, A5 |year=2000 |month=December |pmid=11113418 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012480}}</ref><ref name="pmid11329210">{{cite journal |author=Gibson CM, Kirtane AJ, Murphy SA, ''et al'' |title=Impact of contrast agent type (ionic versus nonionic) used for coronary angiography on angiographic, electrocardiographic, and clinical outcomes following thrombolytic administration in acute myocardial infarction |journal=Catheter Cardiovasc Interv |volume=53 |issue=1 |pages=6–11 |year=2001 |month=May |pmid=11329210 |doi=10.1002/ccd.1121 |url=}}</ref><ref name="pmid10925348">{{cite journal |author=Faile BA, Guzzo JA, Tate DA, Nichols TC, Smith SC, Dehmer GJ |title=Effect of sex, hemodynamics, body size, and other clinical variables on the corrected thrombolysis in myocardial infarction frame count used as an assessment of coronary blood flow |journal=Am. Heart J. |volume=140 |issue=2 |pages=308–14 |year=2000 |month=August |pmid=10925348 |doi=10.1067/mhj.2000.108003 |url=}}</ref>: | |||
*Injection force: A power injector to change the force of injection (cc/sec) from the 10th to the 90th percentile of human injection rates lowers the CTFC by only 2 frames<ref name="pmid9604968">{{cite journal |author=Dodge JT, Rizzo M, Nykiel M, ''et al'' |title=Impact of injection rate on the Thrombolysis in Myocardial Infarction (TIMI) trial frame count |journal=Am. J. Cardiol. |volume=81 |issue=10 |pages=1268–70 |year=1998 |month=May |pmid=9604968 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(98)00138-6}}</ref>. | *Injection force: A power injector to change the force of injection (cc/sec) from the 10th to the 90th percentile of human injection rates lowers the CTFC by only 2 frames<ref name="pmid9604968">{{cite journal |author=Dodge JT, Rizzo M, Nykiel M, ''et al'' |title=Impact of injection rate on the Thrombolysis in Myocardial Infarction (TIMI) trial frame count |journal=Am. J. Cardiol. |volume=81 |issue=10 |pages=1268–70 |year=1998 |month=May |pmid=9604968 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(98)00138-6}}</ref>. | ||
*Nitrate administration significantly increases the CTFC by 6 frames (P<0.001)<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | *Nitrate administration significantly increases the CTFC by 6 frames (P<0.001)<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | ||
*Dye injection at the beginning of diastole decreases the CTFC by 3 to 6 frames<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | *Dye injection at the beginning of diastole decreases the CTFC by 3 to 6 frames<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | ||
*Increasing the heart rate by 20 beats per minute significantly decreases the CTFC by 5 frames (P<0.001)<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | *Increasing the heart rate by 20 beats per minute significantly decreases the CTFC by 5 frames (P<0.001)<ref name="pmid10577994">{{cite journal |author=Abaci A, Oguzhan A, Eryol NK, Ergin A |title=Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility |journal=Circulation |volume=100 |issue=22 |pages=2219–23 |year=1999 |month=November |pmid=10577994 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10577994}}</ref>. | ||
===Association of the CTFC with Clinical Outcomes=== | ===Association of the CTFC with Clinical Outcomes=== | ||
| Line 77: | Line 77: | ||
Following fibrinolytic administration as well as PCI, the CTFC is related to a variety of clinical outcomes <ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref><ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref><ref name="pmid9527071">{{cite journal |author=French JK, Ellis CJ, Webber BJ, ''et al'' |title=Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity |journal=Am. J. Cardiol. |volume=81 |issue=6 |pages=665–71 |year=1998 |month=March |pmid=9527071 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997010047}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11275924">{{cite journal |author=Amos DJ, French JK, Andrews J, ''et al'' |title=Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy |journal=Am. Heart J. |volume=141 |issue=4 |pages=586–91 |year=2001 |month=April |pmid=11275924 |doi=10.1067/mhj.2001.113393 |url=}}</ref>. Flow in the infarct-related artery in survivors is significantly faster than in patients who die (49.5 versus 69.6 frames; P=0.0003)<ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref>. In NSTEMI and STEMI, the post-PCI culprit flow among survivors is significantly faster than among those patients who died (CTFCs 20.4 versus 33.4 frames, P=0.017)(37). Among patients undergoing PCI, the CTFC has demonstrated greater sensitivity in detecting improvements in epicardial flow compared with the use of TIMI grade 3 flow among patients treated with new device interventions and in the detection of transplant rejection <ref name="pmid10235089">{{cite journal |author=Edep ME, Guarneri EM, Teirstein PS, Phillips PS, Brown DL |title=Differences in TIMI frame count following successful reperfusion with stenting or percutaneous transluminal coronary angioplasty for acute myocardial infarction |journal=Am. J. Cardiol. |volume=83 |issue=9 |pages=1326–9 |year=1999 |month=May |pmid=10235089 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00094-6}}</ref><ref name="pmid11269778">{{cite journal |author=Vrachatis AD, Alpert MA, Georgulas VP, ''et al'' |title=Comparative efficacy of primary angioplasty with stent implantation and thrombolysis in restoring basal coronary artery flow in acute ST segment elevation myocardial infarction: quantitative assessment using the corrected TIMI frame count |journal=Angiology |volume=52 |issue=3 |pages=161–6 |year=2001 |month=March |pmid=11269778 |doi= |url=http://ang.sagepub.com/cgi/pmidlookup?view=long&pmid=11269778}}</ref><ref name="pmid11527614">{{cite journal |author=Hamada S, Nishiue T, Nakamura S, ''et al'' |title=TIMI frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=38 |issue=3 |pages=666–71 |year=2001 |month=September |pmid=11527614 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(01)01424-3}}</ref><ref name="pmid11514995">{{cite journal |author=Capozzolo C, Piscione F, De Luca G, ''et al'' |title=Direct coronary stenting: effect on coronary blood flow, immediate and late clinical results |journal=Catheter Cardiovasc Interv |volume=53 |issue=4 |pages=464–73 |year=2001 |month=August |pmid=11514995 |doi= |url=http://dx.doi.org/10.1002/ccd.1204}}</ref><ref name="pmid12368511">{{cite journal |author=Bickel C, Rupprecht HJ, Maimaitiming A, ''et al'' |title=The superiority of TIMI frame count in detecting coronary flow changes after coronary stenting compared to TIMI Flow Classification |journal=J Invasive Cardiol |volume=14 |issue=10 |pages=590–6 |year=2002 |month=October |pmid=12368511 |doi= |url=}}</ref><ref name="pmid11024410">{{cite journal |author=Fang JC, Kinlay S, Wexberg P, ''et al'' |title=Use of the thrombolysis in myocardial infarction frame count for the quantitative assessment of transplant-associated arteriosclerosis |journal=Am. J. Cardiol. |volume=86 |issue=8 |pages=890–2 |year=2000 |month=October |pmid=11024410 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(00)01115-2}}</ref>. | Following fibrinolytic administration as well as PCI, the CTFC is related to a variety of clinical outcomes <ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref><ref name="pmid11997276">{{cite journal |author=Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E |title=Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction |journal=Circulation |volume=105 |issue=16 |pages=1909–13 |year=2002 |month=April |pmid=11997276 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=11997276}}</ref><ref name="pmid9527071">{{cite journal |author=French JK, Ellis CJ, Webber BJ, ''et al'' |title=Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity |journal=Am. J. Cardiol. |volume=81 |issue=6 |pages=665–71 |year=1998 |month=March |pmid=9527071 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997010047}}</ref><ref name="pmid9922346">{{cite journal |author=French JK, Straznicky IT, Webber BJ, ''et al'' |title=Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction |journal=Heart |volume=81 |issue=2 |pages=128–33 |year=1999 |month=February |pmid=9922346 |pmc=1728934 |doi= |url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=9922346}}</ref><ref name="pmid10807455">{{cite journal |author=French JK, Hyde TA, Straznicky IT, ''et al'' |title=Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=35 |issue=6 |pages=1516–24 |year=2000 |month=May |pmid=10807455 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(00)00577-5}}</ref><ref name="pmid11275924">{{cite journal |author=Amos DJ, French JK, Andrews J, ''et al'' |title=Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy |journal=Am. Heart J. |volume=141 |issue=4 |pages=586–91 |year=2001 |month=April |pmid=11275924 |doi=10.1067/mhj.2001.113393 |url=}}</ref>. Flow in the infarct-related artery in survivors is significantly faster than in patients who die (49.5 versus 69.6 frames; P=0.0003)<ref name="pmid10208996">{{cite journal |author=Gibson CM, Murphy SA, Rizzo MJ, ''et al'' |title=Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group |journal=Circulation |volume=99 |issue=15 |pages=1945–50 |year=1999 |month=April |pmid=10208996 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=10208996}}</ref>. In NSTEMI and STEMI, the post-PCI culprit flow among survivors is significantly faster than among those patients who died (CTFCs 20.4 versus 33.4 frames, P=0.017)(37). Among patients undergoing PCI, the CTFC has demonstrated greater sensitivity in detecting improvements in epicardial flow compared with the use of TIMI grade 3 flow among patients treated with new device interventions and in the detection of transplant rejection <ref name="pmid10235089">{{cite journal |author=Edep ME, Guarneri EM, Teirstein PS, Phillips PS, Brown DL |title=Differences in TIMI frame count following successful reperfusion with stenting or percutaneous transluminal coronary angioplasty for acute myocardial infarction |journal=Am. J. Cardiol. |volume=83 |issue=9 |pages=1326–9 |year=1999 |month=May |pmid=10235089 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(99)00094-6}}</ref><ref name="pmid11269778">{{cite journal |author=Vrachatis AD, Alpert MA, Georgulas VP, ''et al'' |title=Comparative efficacy of primary angioplasty with stent implantation and thrombolysis in restoring basal coronary artery flow in acute ST segment elevation myocardial infarction: quantitative assessment using the corrected TIMI frame count |journal=Angiology |volume=52 |issue=3 |pages=161–6 |year=2001 |month=March |pmid=11269778 |doi= |url=http://ang.sagepub.com/cgi/pmidlookup?view=long&pmid=11269778}}</ref><ref name="pmid11527614">{{cite journal |author=Hamada S, Nishiue T, Nakamura S, ''et al'' |title=TIMI frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=38 |issue=3 |pages=666–71 |year=2001 |month=September |pmid=11527614 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(01)01424-3}}</ref><ref name="pmid11514995">{{cite journal |author=Capozzolo C, Piscione F, De Luca G, ''et al'' |title=Direct coronary stenting: effect on coronary blood flow, immediate and late clinical results |journal=Catheter Cardiovasc Interv |volume=53 |issue=4 |pages=464–73 |year=2001 |month=August |pmid=11514995 |doi= |url=http://dx.doi.org/10.1002/ccd.1204}}</ref><ref name="pmid12368511">{{cite journal |author=Bickel C, Rupprecht HJ, Maimaitiming A, ''et al'' |title=The superiority of TIMI frame count in detecting coronary flow changes after coronary stenting compared to TIMI Flow Classification |journal=J Invasive Cardiol |volume=14 |issue=10 |pages=590–6 |year=2002 |month=October |pmid=12368511 |doi= |url=}}</ref><ref name="pmid11024410">{{cite journal |author=Fang JC, Kinlay S, Wexberg P, ''et al'' |title=Use of the thrombolysis in myocardial infarction frame count for the quantitative assessment of transplant-associated arteriosclerosis |journal=Am. J. Cardiol. |volume=86 |issue=8 |pages=890–2 |year=2000 |month=October |pmid=11024410 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9149(00)01115-2}}</ref>. | ||
===The Pathophysiology of STEMI and UA/NSTEMI Based on measures of | ===The Pathophysiology of STEMI and UA/NSTEMI Based on measures of Epicardial Flow=== | ||
One of the more interesting observations learned with the use of the CTFC is the fact that flow in nonculprit arteries in the setting of acute coronary syndromes is "abnormal." For instance, the CTFC in uninvolved arteries in acute STEMI (30.5 frames) is in fact 40% slower than normal (21 frames, P<0.001)<ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref><ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref><ref name="pmid11006367">{{cite journal |author=Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW |title=Multiple complex coronary plaques in patients with acute myocardial infarction |journal=N. Engl. J. Med. |volume=343 |issue=13 |pages=915–22 |year=2000 |month=September |pmid=11006367 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=11006367&promo=ONFLNS19}}</ref>. Adjunctive and rescue PCI following fibrinolysis restores flow in culprit vessels that is nearly identical to that of nonculprit arteries in the STEMI setting (30.5 versus 30.5 frames, p=NS)<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, but this flow remains slower than normal (21 frames). It is notable that PCI of the culprit lesion is also associated with improvements in the nonculprit artery after the intervention in both the STEMI and UA/NSTEMI settings <ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref><ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref>. Slower flow throughout all 3 arteries in STEMI is associated with a higher risk of adverse outcomes<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, poorer wall motion in remote territories<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, poorer tissue perfusion on digital subtraction angiography (DSA)<ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref>, and a greater magnitude of ST depression in remote territories such as the anterior precordium in inferior MI<ref name="pmid11994554">{{cite journal |author=Gibson CM, Chen M, Angeja BG, ''et al'' |title=Precordial ST-segment depression in inferior myocardial infarction is associated with slow flow in the non-culprit left anterior descending artery |journal=J. Thromb. Thrombolysis |volume=13 |issue=1 |pages=9–12 |year=2002 |month=February |pmid=11994554 |doi= |url=http://www.kluweronline.com/art.pdf?issn=0929-5305&volume=13&page=9}}</ref>. The basis of slowed flow in non-culprit arteries is not clear. It has been speculated that the delayed flow in the non-culprit artery may be the result of spasm in shared territories of microvasculature, or a result of global vasoconstriction mediated through either a local neurohumoral or paracrine mechanism. Gregorini et al<ref name="pmid9927393">{{cite journal |author=Gregorini L, Marco J, Kozàkovà M, ''et al'' |title=Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction |journal=Circulation |volume=99 |issue=4 |pages=482–90 |year=1999 |month=February |pmid=9927393 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=9927393}}</ref> have highlighted the importance of sympathetic storm. Consistent with this hypothesis, they have demonstrated that the CTFC and fractional wall shortening is improved in both the culprit and nonculprit arteries after administration of alpha-blockers. Willerson and others <ref name="pmid6894016">{{cite journal |author=Hirsh PD, Hillis LD, Campbell WB, Firth BG, Willerson JT |title=Release of prostaglandins and thromboxane into the coronary circulation in patients with ischemic heart disease |journal=N. Engl. J. Med. |volume=304 |issue=12 |pages=685–91 |year=1981 |month=March |pmid=6894016 |doi= |url=}}</ref><ref name="pmid6488486">{{cite journal |author=Bush LR, Campbell WB, Kern K, ''et al'' |title=The effects of alpha 2-adrenergic and serotonergic receptor antagonists on cyclic blood flow alterations in stenosed canine coronary arteries |journal=Circ. Res. |volume=55 |issue=5 |pages=642–52 |year=1984 |month=November |pmid=6488486 |doi= |url=}}</ref><ref name="pmid6391133">{{cite journal |author=Willerson JT, Campbell WB, Winniford MD, ''et al'' |title=Conversion from chronic to acute coronary artery disease: speculation regarding mechanisms |journal=Am. J. Cardiol. |volume=54 |issue=10 |pages=1349–54 |year=1984 |month=December |pmid=6391133 |doi= |url=}}</ref><ref name="pmid2988822">{{cite journal |author=Apprill P, Schmitz JM, Campbell WB, ''et al'' |title=Cyclic blood flow variations induced by platelet-activating factor in stenosed canine coronary arteries despite inhibition of thromboxane synthetase, serotonin receptors, and alpha-adrenergic receptors |journal=Circulation |volume=72 |issue=2 |pages=397–405 |year=1985 |month=August |pmid=2988822 |doi= |url=}}</ref><ref name="pmid2521875">{{cite journal |author=Ashton JH, Golino P, McNatt JM, Buja LM, Willerson JT |title=Serotonin S2 and thromboxane A2-prostaglandin H2 receptor blockade provide protection against epinephrine-induced cyclic flow variations in severely narrowed canine coronary arteries |journal=J. Am. Coll. Cardiol. |volume=13 |issue=3 |pages=755–63 |year=1989 |month=March |pmid=2521875 |doi= |url=}}</ref><ref name="pmid2661588">{{cite journal |author=Eidt JF, Allison P, Noble S, ''et al'' |title=Thrombin is an important mediator of platelet aggregation in stenosed canine coronary arteries with endothelial injury |journal=J. Clin. Invest. |volume=84 |issue=1 |pages=18–27 |year=1989 |month=July |pmid=2661588 |pmc=303947 |doi=10.1172/JCI114138 |url=}}</ref><ref name="pmid2661053">{{cite journal |author=Willerson JT, Golino P, Eidt J, Campbell WB, Buja LM |title=Specific platelet mediators and unstable coronary artery lesions. Experimental evidence and potential clinical implications |journal=Circulation |volume=80 |issue=1 |pages=198–205 |year=1989 |month=July |pmid=2661053 |doi= |url=}}</ref> have also demonstrated that a wide range of vasoconstrictors including thromboxane A2, serotonin, endothelin, oxygen-derived free radicals, and thrombin are all released in the setting of vessel injury, thrombosis and reperfusion. While a residual stenosis following PCI in the setting of STEMI may be responsible for the delay in flow, it is important to note that despite a minimal 13% residual stenosis and the relief of intraluminal obstruction with stent placement, flow remains persistently abnormal in 34% of stented vessels<ref name="pmid10551685">{{cite journal |author=Gibson CM, Murphy S, Menown IB, ''et al'' |title=Determinants of coronary blood flow after thrombolytic administration. TIMI Study Group. Thrombolysis in Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=5 |pages=1403–12 |year=1999 |month=November |pmid=10551685 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003976}}</ref>. | One of the more interesting observations learned with the use of the CTFC is the fact that flow in nonculprit arteries in the setting of acute coronary syndromes is "abnormal." For instance, the CTFC in uninvolved arteries in acute STEMI (30.5 frames) is in fact 40% slower than normal (21 frames, P<0.001)<ref name="pmid8598078">{{cite journal |author=Gibson CM, Cannon CP, Daley WL, ''et al'' |title=TIMI frame count: a quantitative method of assessing coronary artery flow |journal=Circulation |volume=93 |issue=5 |pages=879–88 |year=1996 |month=March |pmid=8598078 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598078}}</ref><ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref><ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref><ref name="pmid11006367">{{cite journal |author=Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW |title=Multiple complex coronary plaques in patients with acute myocardial infarction |journal=N. Engl. J. Med. |volume=343 |issue=13 |pages=915–22 |year=2000 |month=September |pmid=11006367 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=11006367&promo=ONFLNS19}}</ref>. Adjunctive and rescue PCI following fibrinolysis restores flow in culprit vessels that is nearly identical to that of nonculprit arteries in the STEMI setting (30.5 versus 30.5 frames, p=NS)<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, but this flow remains slower than normal (21 frames). It is notable that PCI of the culprit lesion is also associated with improvements in the nonculprit artery after the intervention in both the STEMI and UA/NSTEMI settings <ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref><ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref>. Slower flow throughout all 3 arteries in STEMI is associated with a higher risk of adverse outcomes<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, poorer wall motion in remote territories<ref name="pmid10520778">{{cite journal |author=Gibson CM, Ryan KA, Murphy SA, ''et al'' |title=Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=4 |pages=974–82 |year=1999 |month=October |pmid=10520778 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003356}}</ref>, poorer tissue perfusion on digital subtraction angiography (DSA)<ref name="pmid11113417">{{cite journal |author=Gibson CM, Goel M, Murphy SA, ''et al'' |title=Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis |journal=Am. J. Cardiol. |volume=86 |issue=12 |pages=1375–7, A5 |year=2000 |month=December |pmid=11113417 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914900012479}}</ref>, and a greater magnitude of ST depression in remote territories such as the anterior precordium in inferior MI<ref name="pmid11994554">{{cite journal |author=Gibson CM, Chen M, Angeja BG, ''et al'' |title=Precordial ST-segment depression in inferior myocardial infarction is associated with slow flow in the non-culprit left anterior descending artery |journal=J. Thromb. Thrombolysis |volume=13 |issue=1 |pages=9–12 |year=2002 |month=February |pmid=11994554 |doi= |url=http://www.kluweronline.com/art.pdf?issn=0929-5305&volume=13&page=9}}</ref>. The basis of slowed flow in non-culprit arteries is not clear. It has been speculated that the delayed flow in the non-culprit artery may be the result of spasm in shared territories of microvasculature, or a result of global vasoconstriction mediated through either a local neurohumoral or paracrine mechanism. Gregorini et al<ref name="pmid9927393">{{cite journal |author=Gregorini L, Marco J, Kozàkovà M, ''et al'' |title=Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction |journal=Circulation |volume=99 |issue=4 |pages=482–90 |year=1999 |month=February |pmid=9927393 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=9927393}}</ref> have highlighted the importance of sympathetic storm. Consistent with this hypothesis, they have demonstrated that the CTFC and fractional wall shortening is improved in both the culprit and nonculprit arteries after administration of alpha-blockers. Willerson and others <ref name="pmid6894016">{{cite journal |author=Hirsh PD, Hillis LD, Campbell WB, Firth BG, Willerson JT |title=Release of prostaglandins and thromboxane into the coronary circulation in patients with ischemic heart disease |journal=N. Engl. J. Med. |volume=304 |issue=12 |pages=685–91 |year=1981 |month=March |pmid=6894016 |doi= |url=}}</ref><ref name="pmid6488486">{{cite journal |author=Bush LR, Campbell WB, Kern K, ''et al'' |title=The effects of alpha 2-adrenergic and serotonergic receptor antagonists on cyclic blood flow alterations in stenosed canine coronary arteries |journal=Circ. Res. |volume=55 |issue=5 |pages=642–52 |year=1984 |month=November |pmid=6488486 |doi= |url=}}</ref><ref name="pmid6391133">{{cite journal |author=Willerson JT, Campbell WB, Winniford MD, ''et al'' |title=Conversion from chronic to acute coronary artery disease: speculation regarding mechanisms |journal=Am. J. Cardiol. |volume=54 |issue=10 |pages=1349–54 |year=1984 |month=December |pmid=6391133 |doi= |url=}}</ref><ref name="pmid2988822">{{cite journal |author=Apprill P, Schmitz JM, Campbell WB, ''et al'' |title=Cyclic blood flow variations induced by platelet-activating factor in stenosed canine coronary arteries despite inhibition of thromboxane synthetase, serotonin receptors, and alpha-adrenergic receptors |journal=Circulation |volume=72 |issue=2 |pages=397–405 |year=1985 |month=August |pmid=2988822 |doi= |url=}}</ref><ref name="pmid2521875">{{cite journal |author=Ashton JH, Golino P, McNatt JM, Buja LM, Willerson JT |title=Serotonin S2 and thromboxane A2-prostaglandin H2 receptor blockade provide protection against epinephrine-induced cyclic flow variations in severely narrowed canine coronary arteries |journal=J. Am. Coll. Cardiol. |volume=13 |issue=3 |pages=755–63 |year=1989 |month=March |pmid=2521875 |doi= |url=}}</ref><ref name="pmid2661588">{{cite journal |author=Eidt JF, Allison P, Noble S, ''et al'' |title=Thrombin is an important mediator of platelet aggregation in stenosed canine coronary arteries with endothelial injury |journal=J. Clin. Invest. |volume=84 |issue=1 |pages=18–27 |year=1989 |month=July |pmid=2661588 |pmc=303947 |doi=10.1172/JCI114138 |url=}}</ref><ref name="pmid2661053">{{cite journal |author=Willerson JT, Golino P, Eidt J, Campbell WB, Buja LM |title=Specific platelet mediators and unstable coronary artery lesions. Experimental evidence and potential clinical implications |journal=Circulation |volume=80 |issue=1 |pages=198–205 |year=1989 |month=July |pmid=2661053 |doi= |url=}}</ref> have also demonstrated that a wide range of vasoconstrictors including thromboxane A2, serotonin, endothelin, oxygen-derived free radicals, and thrombin are all released in the setting of vessel injury, thrombosis and reperfusion. While a residual stenosis following PCI in the setting of STEMI may be responsible for the delay in flow, it is important to note that despite a minimal 13% residual stenosis and the relief of intraluminal obstruction with stent placement, flow remains persistently abnormal in 34% of stented vessels<ref name="pmid10551685">{{cite journal |author=Gibson CM, Murphy S, Menown IB, ''et al'' |title=Determinants of coronary blood flow after thrombolytic administration. TIMI Study Group. Thrombolysis in Myocardial Infarction |journal=J. Am. Coll. Cardiol. |volume=34 |issue=5 |pages=1403–12 |year=1999 |month=November |pmid=10551685 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735109799003976}}</ref>. | ||
| Line 159: | Line 159: | ||
[[Image:TFC landmark in LAD.jpg|300px|left|thumb|TFC landmark in LAD artery]] | [[Image:TFC landmark in LAD.jpg|300px|left|thumb|TFC landmark in LAD artery]] | ||
<br clear="left"/> | <br clear="left"/> | ||
==2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)<ref name="pmid23247303">{{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, ''et al.'' |title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines |journal=Circulation |volume= |issue= |pages= |year=2012 |month=December |pmid=23247303 |doi=10.1161/CIR.0b013e3182742c84|url=}}</ref>== | ==2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)<ref name="pmid23247303">{{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, ''et al.'' |title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines |journal=Circulation |volume= |issue= |pages= |year=2012 |month=December |pmid=23247303 |doi=10.1161/CIR.0b013e3182742c84|url=}}</ref>== | ||
===Coronary Angiography in Patients Who Initially Were Managed With Fibrinolytic Therapy or Who Did Not Receive Reperfusion (DO NOT EDIT)<ref name="pmid23247303">{{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, ''et al.'' |title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines |journal=Circulation |volume= |issue= |pages= |year=2012 |month=December |pmid=23247303 |doi=10.1161/CIR.0b013e3182742c84|url=}}</ref>=== | ===Coronary Angiography in Patients Who Initially Were Managed With Fibrinolytic Therapy or Who Did Not Receive Reperfusion (DO NOT EDIT)<ref name="pmid23247303">{{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, ''et al.'' |title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines |journal=Circulation |volume= |issue= |pages= |year=2012 |month=December |pmid=23247303 |doi=10.1161/CIR.0b013e3182742c84|url=}}</ref>=== | ||
| Line 200: | Line 168: | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' Cardiac catheterization and coronary angiography with intent to perform revascularization should be performed after STEMI in patients with any of the following:<nowiki>"</nowiki> | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' [[Cardiac catheterization]] and [[coronary angiography]] with intent to perform revascularization should be performed after STEMI in patients with any of the following:<nowiki>"</nowiki> | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''a.''' Cardiogenic shock or acute severe HF that develops after initial presentation <ref name="pmid">{{cite journal |author=Wu AH, Parsons L, Every NR, Bates ER |title=Hospital outcomes in patients presenting with congestive heart failure complicating acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2) |journal=J. Am. Coll. Cardiol. |volume=40 |issue=8 |pages=1389–94 |year=2002 |month=October |pmid= |doi= |url=}}</ref><ref name="pmid">{{cite journal |author=Hochman JS, Sleeper LA, White HD, ''et al.'' |title=One-year survival following early revascularization for cardiogenic shock |journal= |volume=285 |issue=2 |pages=190–2 |year=2001 |month=January |pmid= |doi= |url=}}</ref><ref name="pmid">{{cite journal |author=Steg PG, Kerner A, Van de Werf F, ''et al.'' |title=Impact of in-hospital revascularization on survival in patients with non-ST-elevation acute coronary syndrome and congestive heart failure |journal= |volume=118 |issue=11 |pages=1163–71 |year=2008 |month=September |pmid= |doi=10.1161/CIRCULATIONAHA.108.789685 |url=}}</ref><ref name="pmid">{{cite journal |author=Steg PG, Dabbous OH, Feldman LJ, ''et al.'' |title=Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE) |journal= |volume=109 |issue=4 |pages=494–9 |year=2004 |month=February |pmid= |doi=10.1161/01.CIR.0000109691.16944.DA |url=}}</ref>''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki>; | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''a.''' [[Cardiogenic shock]] or acute severe [[HF]] that develops after initial presentation <ref name="pmid">{{cite journal |author=Wu AH, Parsons L, Every NR, Bates ER |title=Hospital outcomes in patients presenting with congestive heart failure complicating acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2) |journal=J. Am. Coll. Cardiol. |volume=40 |issue=8 |pages=1389–94 |year=2002 |month=October |pmid= |doi= |url=}}</ref><ref name="pmid">{{cite journal |author=Hochman JS, Sleeper LA, White HD, ''et al.'' |title=One-year survival following early revascularization for cardiogenic shock |journal= |volume=285 |issue=2 |pages=190–2 |year=2001 |month=January |pmid= |doi= |url=}}</ref><ref name="pmid">{{cite journal |author=Steg PG, Kerner A, Van de Werf F, ''et al.'' |title=Impact of in-hospital revascularization on survival in patients with non-ST-elevation acute coronary syndrome and congestive heart failure |journal= |volume=118 |issue=11 |pages=1163–71 |year=2008 |month=September |pmid= |doi=10.1161/CIRCULATIONAHA.108.789685 |url=}}</ref><ref name="pmid">{{cite journal |author=Steg PG, Dabbous OH, Feldman LJ, ''et al.'' |title=Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE) |journal= |volume=109 |issue=4 |pages=494–9 |year=2004 |month=February |pmid= |doi=10.1161/01.CIR.0000109691.16944.DA |url=}}</ref>''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki>; | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''b.''' Intermediate- or high-risk findings on predischarge noninvasive ischemia testing<ref name="pmid">{{cite journal |author=Erne P, Schoenenberger AW, Burckhardt D, ''et al.'' |title=Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial |journal=JAMA |volume=297 |issue=18 |pages=1985–91 |year=2007 |month=May |pmid= |doi=10.1001/jama.297.18.1985 |url=}}</ref><ref name="pmid">{{cite journal |author=Madsen JK, Grande P, Saunamäki K, ''et al.'' |title=Danish multicenter randomized study of invasive versus conservative treatment in patients with inducible ischemia after thrombolysis in acute myocardial infarction (DANAMI). DANish trial in Acute Myocardial Infarction |journal=Circulation |volume=96 |issue=3 |pages=748–55 |year=1997 |month=August |pmid= |doi= |url=}}</ref>''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki>; or | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''b.''' Intermediate- or high-risk findings on predischarge noninvasive ischemia testing<ref name="pmid">{{cite journal |author=Erne P, Schoenenberger AW, Burckhardt D, ''et al.'' |title=Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial |journal=JAMA |volume=297 |issue=18 |pages=1985–91 |year=2007 |month=May |pmid= |doi=10.1001/jama.297.18.1985 |url=}}</ref><ref name="pmid">{{cite journal |author=Madsen JK, Grande P, Saunamäki K, ''et al.'' |title=Danish multicenter randomized study of invasive versus conservative treatment in patients with inducible ischemia after thrombolysis in acute myocardial infarction (DANAMI). DANish trial in Acute Myocardial Infarction |journal=Circulation |volume=96 |issue=3 |pages=748–55 |year=1997 |month=August |pmid= |doi= |url=}}</ref>''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki>; or | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''c.''' Myocardial ischemia that is spontaneous or provoked by minimal exertion during hospitalization.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''c.''' [[Myocardial ischemia]] that is spontaneous or provoked by minimal exertion during hospitalization.''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
| Line 219: | Line 187: | ||
==Sources== | ==Sources== | ||
* | * 2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction <ref name="pmid23247303">{{cite journal |author=O'Gara PT, Kushner FG, Ascheim DD, ''et al.'' |title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines |journal=Circulation |volume= |issue= |pages=|year=2012 |month=December |pmid=23247303 |doi=10.1161/CIR.0b013e3182742c84|url=}}</ref> | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Coronary Angiography}} | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
{{ | |||
[[Category:Disease]] | [[Category:Disease]] | ||
| Line 242: | Line 201: | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:Angiopedia]] | |||
Latest revision as of 00:15, 30 July 2020
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction coronary angiography On the Web |
|
FDA on ST elevation myocardial infarction coronary angiography |
|
CDC on ST elevation myocardial infarction coronary angiography |
|
ST elevation myocardial infarction coronary angiography in the news |
|
Blogs on ST elevation myocardial infarction coronary angiography |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction coronary angiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
The goal of coronary angiography in STEMI patients is to identify the obstructed culprit artery and to open it as quickly as possible. The goal is to achieve a door to balloon time in under 90 minutes. This is the time from when a patient arrives at the door of the emergency room until the time that the first device is activated in the coronary artery.
Reducing Door to Balloon Times
The following strategies can be utilized to reduce door to balloon times:
- Have emergency medical service (EMS) personnel activate the cardiac catheterization laboratory directly
- Require that nurses, technicians and physicians remain within 30 minutes of the hospital while on call
- Require that nurses, technicians and physicians sleep in the hospital while on call
- Optimize door to EKG and EKG to decision times
- Activate the cardiac catheterization laboratory team with a single phone call using batch paging
- Have a "sterile table" prepared in the cardiac catheterization laboratory so that no time is wasted gathering equipment and supplies.
- Ask the CCU nurse and or ER nurse to assist the cath lab nurse in transporting and readying the patient for cardiac catheterization.
- Do not perform right heart catheterization or left heart catheterization before the intervention
- Only obtain venous access if the patient is hemodynamically unstable or if there is likely going to be the need to a temporary pacemaker
- Perform angiography of the culprit lesion first. There is a lack of consensus on this point. Some operators prefer to perform angiography of the non-culprit lesion first to assess the extent of disease. The Editor-In-Chief, CM Gibson prefers to assess the non-culprit lesion first. The non-culprit lesion may in fact turn out to be the culprit lesion.
View used to Assess the Coronary Anatomy during Emergency Angiography
For the left system either a right anterior oblique (RAO) caudal projection or an anteroposterior (AP) caudal projection is often chosen for the first injection. These two views provide an assessment of the left main, the left anterior descending artery and the left circumflex artery. This view is often chosen as the first view in case the patient should sustain a cardiac arrest following the first injection. It provides the most data in a single injection should the operator need to proceed with percutaneous coronary intervention (PCI) after this first injection. Likewise for the right coronary artery, the first injection should be an LAO cranial injection which lays out the distal bifurcation of the RCA into the posterolateral and the posterior descending arteries well. For a complete discussion of views to obtain during cardiac catheterization, please see the chapter entitled: Suggested angiographic projections.
Preparing for Percutaneous Intervention
Once a culprit lesion has been identified on coronary angiography, preparation begins for percutaneous coronary intervention. The strategy of the Editor-In-Chief C. Michael Gibson, M.S., M.D. is as follows:
- Review the medications the patient was administered prior to cardiac catheterization
- Confirm that the patient has received a full 325 mg PO dose of non-enteric coated aspirin
- Confirm that the patient has received a 600 mg loading of dose of clopidogrel
- Administer an antithrombin if this has not yet been done so (either bivalirudin or unfractionated heparin, preferably bivalirudin)
- Administer a glycoprotein IIbIIIa inhibitor if this has not been done so
- If the patient has a totally occluded RCA, or a totally occluded dominant circumflex, open the fluids up wide open, have a temporary pacemaker at the bedside, and have atropine prepared for administration.
- Consider placement of an intraaortic balloon pump in patients with cardiogenic shock or high risk anatomy
- Make sure blood is typed and crossed in case of bleeding
- Upsize to a larger sheath if neccessary
- Check an ACT after the antithrombin is administered
Interpreting the Coronary Angiogram
Pathophysiology of Reperfusion
The Importance of Restoring and Sustaining Complete Epicardial and Myocardial Perfusion:
Recently, it has become recognized that it is necessary but not sufficient to restore epicardial flow in ST elevation MI. Not all TIMI grade 3 flow is created equally. In addition to epicardial flow, myocardial perfusion must be restored as well. This has been demonstrated in both myocardial contrast echo studies as well as angiographic studies[1][2][3][4][5][6][7][8][9][10][11][12][13]. As a result of this new understanding, the goal of reperfusion therapies has shifted to include reperfusion downstream at the level of capillary bed, and it might be more appropriate that the current reperfusion hypothesis now be termed "the time dependent open muscle hypothesis." This wiki article reviews the angiographic methods used to evaluate myocardial ischemia and infarction and discusses the insights into the pathophysiology of acute coronary syndromes provided by these angiographic indexes of coronary artery blood flow and myocardial perfusion.
TIMI Flow Grades (TFGs)
The Thrombolysis In Myocardial Infarction (TIMI) flow grade classification scheme has been widely used to assess coronary blood flow in acute coronary syndromes [1]. TFG 0 means the artery is closed; TFG 1 means that dye penetrates the stenosis but does not reach the downstream bed; TFG 2 means that flow is slow down the artery and TFG 3 means that normal flow has been restored. The association of the TFGs with clinical outcomes (including mortality) has been well documented [2][3][4][5][6][7][8].
- TIMI Flow Grade 0: The artery is blocked.
- TIMI Flow Grade 1: This category is subdivided into:
- 1.0: dye minimally leaks past the area of obstruction. TIMI Flow Grade 1 - Left Anterior Descending Artery
- 1.5: dye leaks well past the area of obstruction but fails to opacify the entire coronary bed. TIMI Flow Grade 1.5 - Left Anterior Descending Artery
- TIMI Flow Grade 2: This category is subdivided into:
- 2.0: TIMI 2 slow flow, dye markedly delayed in opacifying distal vasculature. TIMI Flow Grade 2 - Left Anterior Descending Artery
- 2.5: TIMI 2 fast flow, dye minimally delayed in opacifying distal vasculature. TIMI Flow Grade 2.5 - Right Coronary Artery
- TIMI Flow Grade 3: Normal flow in the artery.
The association of the TFGs with mortality must be interpreted with caution as there are several confounders:
- The majority of TIMI grade 2 flow is observed in the left anterior descending artery (LAD) territory, whereas the majority of TIMI grade 3 flow is observed in the right coronary artery (RCA)[7]. Thus, the improved mortality observed among patients with TIMI grade 3 flow may be explained at least in part by the fact that inferior myocardial infarction (MI) location is associated with a lower mortality rate [7].
- The clinical improvement associated with TIMI grade 3 flow may have be nonlinear. For example, greater clinical benefits may be observed if a closed artery (TFG 0/1) is opened (TFG 2) compared with the improvement that might occur if an artery with TFG 2 is converted to TFG 3 flow.
- As more arteries with TFG 2 flow are treated with adjunctive percutaneous coronary intervention (PCI), the prognosis associated with this flow grade may improve. The fact that patients who were treated with an inferior fibrinolytic monotherapy strategy faired so well in GUSTO V may be explained in part by the fact that these patients underwent PCI more often[14]. Two-year follow-up in more recent studies indicates that the survival advantage of TFG 3 flow over TFG 2 flow at 2 years may not be as great as it once was in the era before aggressive utilization of rescue and adjunctive (PCI)[10].
Reocclusion
While PCI may obviously improve epicardial flow, another often unrecognized benefit is the fact that rescue PCI (dilating a closed artery) and adjunctive PCI (dilating an open artery) following fibrinolytic administration may reduce the risk of reocclusion. Reinfarction doubles early mortality by 30 days[14][15]. Controversy has surrounded the use of PCI immediately following PCI, and for many years, immediate PCI was classified as a class III contraindication. These early trials preceded the use of stents, thienopyridines, platelet GP IIb/IIIa inhibitors, and the monitoring of activated clotting times. Among 20,101 STEMI patients treated with fibrinolysis, the performance of PCI during the index hospitalization was associated with a lower rate of in-hospital recurrent MI (1.6% versus 4.5%, P<0.001) and a lower 2-year mortality (5.6% versus 11.6%, P<0.001)[15][16]. Poor flow and the presence of thrombus are two variables that are correlated with a higher risk of angiographic reocclusion [17].
The TIMI Frame Count: A More Precise Angiographic Index of Coronary Blood Flow
There are several limitations to the TFG classification scheme[7]. To overcome these limitations, Gibson developed a more objective and precise index of coronary blood flow called the corrected TIMI frame count (CTFC). In this method, the number of cineframes required for dye to reach standardized distal landmarks are counted. Each frame is 1/30th of a second, and the angiogram is therefore essentially a measure of the time for dye to go down the artery[7][8][10]. In the first frame used for TIMI frame counting, a column of dye touches both borders of the coronary artery and moves forward[7]. In the last frame, dye begins to enter (but does not necessarily fill) a standard distal landmark in the artery. These standard distal landmarks are as follows: in the RCA, the first branch of the posterolateral artery; in the circumflex system, the most distal branch of the obtuse marginal branch, which includes the culprit lesion in the dye path; and in the LAD, the distal bifurcation, which is also known as the "moustache," "pitchfork" or "whale’s tail". These frame counts are corrected for the longer length of the LAD by dividing by 1.7 to arrive at the CTFC [7]. Knowing the time for dye to go down the artery from the CTFC (CTFC/30=seconds), and length of the artery (either from an angioplasty guide wire or by planimetry), dye velocity (cm/s) can also be calculated in a more refined fashion.19 This refined measure allows calculation of the velocity proximal and distal to the lesion[18].
Some of the advantages of the TIMI frame count method are as follows. In contrast to the TFG classification scheme, the CTFC is quantitative rather than qualitative, it is objective rather than subjective, it is a continuous rather than a categorical variable, and it is reproducible[7]. The CTFC demonstrates that flow is not divided into arbitrary slow and fast categories, but rather coronary blood flow is unimodally distributed as a continuous variable[7]. The CTFC has been shown to be quite reproducible with a 1- to 2-frame difference between observers [19][20][21][22][23][24][25][26][27][28][25][26][29]. The CTFC is also highly correlated with other measures of flow such as Doppler velocity wire measures of coronary flow reserve, distal velocity, average peak velocity, and volumetric flow, [20][21][22] as well as fractional flow reserve (r=0.85)[23].
Several technical and physiological variables may impact the CTFC[19][30][31][32][33]:
- Injection force: A power injector to change the force of injection (cc/sec) from the 10th to the 90th percentile of human injection rates lowers the CTFC by only 2 frames[30].
- Nitrate administration significantly increases the CTFC by 6 frames (P<0.001)[19].
- Dye injection at the beginning of diastole decreases the CTFC by 3 to 6 frames[19].
- Increasing the heart rate by 20 beats per minute significantly decreases the CTFC by 5 frames (P<0.001)[19].
Association of the CTFC with Clinical Outcomes
Following fibrinolytic administration as well as PCI, the CTFC is related to a variety of clinical outcomes [7][8][10][24][25][26][27]. Flow in the infarct-related artery in survivors is significantly faster than in patients who die (49.5 versus 69.6 frames; P=0.0003)[8]. In NSTEMI and STEMI, the post-PCI culprit flow among survivors is significantly faster than among those patients who died (CTFCs 20.4 versus 33.4 frames, P=0.017)(37). Among patients undergoing PCI, the CTFC has demonstrated greater sensitivity in detecting improvements in epicardial flow compared with the use of TIMI grade 3 flow among patients treated with new device interventions and in the detection of transplant rejection [34][35][36][37][38][39].
The Pathophysiology of STEMI and UA/NSTEMI Based on measures of Epicardial Flow
One of the more interesting observations learned with the use of the CTFC is the fact that flow in nonculprit arteries in the setting of acute coronary syndromes is "abnormal." For instance, the CTFC in uninvolved arteries in acute STEMI (30.5 frames) is in fact 40% slower than normal (21 frames, P<0.001)[7][40][41][42]. Adjunctive and rescue PCI following fibrinolysis restores flow in culprit vessels that is nearly identical to that of nonculprit arteries in the STEMI setting (30.5 versus 30.5 frames, p=NS)[40], but this flow remains slower than normal (21 frames). It is notable that PCI of the culprit lesion is also associated with improvements in the nonculprit artery after the intervention in both the STEMI and UA/NSTEMI settings [40][41]. Slower flow throughout all 3 arteries in STEMI is associated with a higher risk of adverse outcomes[40], poorer wall motion in remote territories[40], poorer tissue perfusion on digital subtraction angiography (DSA)[41], and a greater magnitude of ST depression in remote territories such as the anterior precordium in inferior MI[43]. The basis of slowed flow in non-culprit arteries is not clear. It has been speculated that the delayed flow in the non-culprit artery may be the result of spasm in shared territories of microvasculature, or a result of global vasoconstriction mediated through either a local neurohumoral or paracrine mechanism. Gregorini et al[44] have highlighted the importance of sympathetic storm. Consistent with this hypothesis, they have demonstrated that the CTFC and fractional wall shortening is improved in both the culprit and nonculprit arteries after administration of alpha-blockers. Willerson and others [45][46][47][48][49][50][51] have also demonstrated that a wide range of vasoconstrictors including thromboxane A2, serotonin, endothelin, oxygen-derived free radicals, and thrombin are all released in the setting of vessel injury, thrombosis and reperfusion. While a residual stenosis following PCI in the setting of STEMI may be responsible for the delay in flow, it is important to note that despite a minimal 13% residual stenosis and the relief of intraluminal obstruction with stent placement, flow remains persistently abnormal in 34% of stented vessels[52].
Assessment of Myocardial Perfusion on the Angiogram: The TIMI Myocardial Perfusion Grade (TMPG)
Studies of myocardial constrast echocardiography (MCE) [12][13] and angiography [9] [10] [53] have demonstrated that restoration of epicardial flow does not necessarily lead to restoration of tissue level or microvascular perfusion . Perfusion of the myocardium can also be assessed using the angiogram. In the TMPG system, TMPG 0 represents minimal or no myocardial blush; in TMPG 1, dye stains the myocardium, and this stain persists on the next injection; in TMPG 2, dye enters the myocardium but washes out slowly so that dye is strongly persistent at the end of the injection but gone by the next injection approximately 30 seconds later; and in TMPG 3, there is normal entrance and exit of dye in the myocardium. Another method of assessing myocardial perfusion on the angiogram is the myocardial blush grade (MBG) developed by van’t Hof et al.[53] A grade of 0 (no blush) and a grade of 3 (normal blush) are the same in the TMPG and MBG systems. An MBG grade 1 or 2 represents diminished intensity in the myocardium and corresponds to a value of 0.5 in the expanded TMPG grading system. A TMPG of 1 or a stain in the TIMI system is subsumed within the value of a 0 in the MBG system. Thus, normal perfusion in the myocardium carries a score of 3 in both the TMPG and MBG systems, and a closed muscle carries a score of 0 in both systems.
Independent of flow in the epicardial artery and other covariates such as age, blood pressure, and pulse, the TMPG has been shown to be multivariate predictors of mortality in acute STEMI at 2 years.[10] The TMPG permits risk stratification even within epicardial TIMI grade 3 flow. Despite achieving epicardial patency with normal TIMI grade 3 flow, those patients whose microvasculature fails to open (TMPG 0/1) have a 7-fold increase in mortality compared with those patients with both TIMI grade 3 flow in the epicardial artery. Achievement of both TIMI grade 3 flow in both the artery and the myocardium is associated with a mortality under 1%[54] (Figure 4). Likewise, in the setting of primary PCI, both van’t Hof et al57 and Haager et al59 have demonstrated an association between impaired myocardial perfusion and early and late mortality. These improvements in early and late mortality may be mediated by improvements in myocardial salvage.60 As Dibra et al60 have demonstrated, restoration of TMPG 2/3 is associated with a higher salvage index (0.49±0.42 versus 0.34±0.49, P=0.01) and a smaller final infarct size (15.4±15.5% versus 22.1±16.2% of the left ventricle, P=0.001). Indeed, second only to stent placement, restoration of TMPG 2/3 was the next most powerful independent determinant of the myocardial salvage index, and was more closely associated with higher salvage indexes than the TFGs.
Examples of Myocardial Perfusion Grades
Myocardial Perfusion Grade 0
TMPG or myocardial perfusion grade 0 in the LAD distribution. The LAD is open, but the anterior myocardium is pale on the left compared with that the posterior circulation to the right.
Myocardial Perfusion Grade 1
TMPG or myocardial perfusion grade 1 in the RCA distribution. This angiogram demonstrates staining or the persistence of dye in the myocardium before the injection begins. This is seen as the U shaped pattern of dye on the right in the angiogram. The failure of dye to exit the myocardium by the next injection constitutes TMPG 1.
Myocardial Perfusion Grade 2
TMPG or myocardial perfusion grade 2 in the RCA distribution. This angiogram demonstrates slow or delayed dye transit through the myocardium. Dye in the myocardium does not fade by the next injection and is stronlgy persistent at the end of the injection. However, by the time the next injection is made, dye has faded from the myocardium.
Myocardial Perfusion Grade 3
TMPG or myocardial perfusion grade 3 in the RCA distribution. This angiogram demonstrates normal dye transit through the myocardium. Dye enters the myocardium and then fades or washes out from the myocardium briskly.
Tips for TIMI Frame Count Evaluations
How do I pick the first frame?
In frame zero, dye touches either none of the borders or only one of the borders as shown below:
We find that in some injections dye will dribble down on border of the artery and these frames are not selected as the first frame. In frame number one, dye extends across at least 70% of the artery and moves forward as shown below:
How do I pick the last frame?
In the last frame, the dye first enters the distal landmark. This frame is included in the frame count. For example, in frame 20 in the RCA shown below, dye has not yet entered the first branch off of the posterolateral:
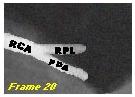
In frame 21 shown below, the dye has begun to enter the first branch off of the posterolateral artery. This is the last frame counted:
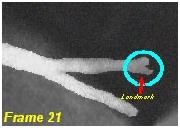
In frame 22, dye begins to fill more completely the distal landmark as shown below:
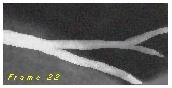
What are the Distal Landmarks Used for TIMI Frame Counting?
In the RCA it is the first branch off of the posterolateral artery:
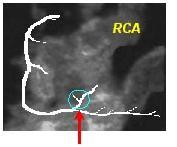
In the circumflex, it is the last branch off of the most distal obtuse marginal as shown below:

In the LAD, it is the bifurcation of the LAD at the apex which is also known as the pitchfork, or the whale’s tail as shown below:

2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction (DO NOT EDIT)[55]
Coronary Angiography in Patients Who Initially Were Managed With Fibrinolytic Therapy or Who Did Not Receive Reperfusion (DO NOT EDIT)[55]
| Class I |
| "1. Cardiac catheterization and coronary angiography with intent to perform revascularization should be performed after STEMI in patients with any of the following:" |
| "a. Cardiogenic shock or acute severe HF that develops after initial presentation [56][56][56][56](Level of Evidence: B)"; |
| "b. Intermediate- or high-risk findings on predischarge noninvasive ischemia testing[56][56](Level of Evidence: B)"; or |
| "c. Myocardial ischemia that is spontaneous or provoked by minimal exertion during hospitalization.(Level of Evidence: C)" |
| Class IIa |
| "1. Coronary angiography with intent to perform revascularization is reasonable for patients with evidence of failed reperfusion or reocclusion after fibrinolytic therapy. Angiography can be performed as soon as logistically feasible.[56][56][8][10][56][57][56] (Level of Evidence: B)" |
| "2. Coronary angiography is reasonable before hospital discharge in stable patients with STEMI after successful fibrinolytic therapy. Angiography can be performed as soon as logistically feasible, and ideally within 24 hours, but should not be performed within the first 2 to 3 hours after administration of fibrinolytic therapy.[56][58][56][59][60][61][56] (Level of Evidence: B)" |
Sources
- 2013 Revised ACCF/AHA Guidelines for the Management of ST-Elevation Myocardial Infarction [55]
References
- ↑ 1.0 1.1 "The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group". N. Engl. J. Med. 312 (14): 932–6. 1985. PMID 4038784. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Simes RJ, Topol EJ, Holmes DR; et al. (1995). "Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators". Circulation. 91 (7): 1923–8. PMID 7895348. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 "The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators". N. Engl. J. Med. 329 (22): 1615–22. 1993. PMID 8232430. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 Vogt A, von Essen R, Tebbe U, Feuerer W, Appel KF, Neuhaus KL (1993). "Impact of early perfusion status of the infarct-related artery on short-term mortality after thrombolysis for acute myocardial infarction: retrospective analysis of four German multicenter studies". J. Am. Coll. Cardiol. 21 (6): 1391–5. PMID 8473646. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Karagounis L, Sorensen SG, Menlove RL, Moreno F, Anderson JL (1992). "Does thrombolysis in myocardial infarction (TIMI) perfusion grade 2 represent a mostly patent artery or a mostly occluded artery? Enzymatic and electrocardiographic evidence from the TEAM-2 study. Second Multicenter Thrombolysis Trial of Eminase in Acute Myocardial Infarction". J. Am. Coll. Cardiol. 19 (1): 1–10. PMID 1729317. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL (1993). "TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolysis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM-3 Study". Circulation. 87 (6): 1829–39. PMID 8504495. Unknown parameter
|month=ignored (help) - ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 Gibson CM, Cannon CP, Daley WL; et al. (1996). "TIMI frame count: a quantitative method of assessing coronary artery flow". Circulation. 93 (5): 879–88. PMID 8598078. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Gibson CM, Murphy SA, Rizzo MJ; et al. (1999). "Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis In Myocardial Infarction (TIMI) Study Group". Circulation. 99 (15): 1945–50. PMID 10208996. Unknown parameter
|month=ignored (help) - ↑ 9.0 9.1 Gibson CM, Cannon CP, Murphy SA; et al. (2000). "Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs". Circulation. 101 (2): 125–30. PMID 10637197. Unknown parameter
|month=ignored (help) - ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E (2002). "Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction". Circulation. 105 (16): 1909–13. PMID 11997276. Unknown parameter
|month=ignored (help) - ↑ Angeja BG, Gunda M, Murphy SA; et al. (2002). "TIMI myocardial perfusion grade and ST segment resolution: association with infarct size as assessed by single photon emission computed tomography imaging". Circulation. 105 (3): 282–5. PMID 11804979. Unknown parameter
|month=ignored (help) - ↑ 12.0 12.1 Ito H, Tomooka T, Sakai N; et al. (1992). "Lack of myocardial perfusion immediately after successful thrombolysis. A predictor of poor recovery of left ventricular function in anterior myocardial infarction". Circulation. 85 (5): 1699–705. PMID 1572028. Unknown parameter
|month=ignored (help) - ↑ 13.0 13.1 Ito H, Maruyama A, Iwakura K; et al. (1996). "Clinical implications of the 'no reflow' phenomenon. A predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction". Circulation. 93 (2): 223–8. PMID 8548892. Unknown parameter
|month=ignored (help) - ↑ 14.0 14.1 Hudson MP, Granger CB, Topol EJ; et al. (2001). "Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials". Circulation. 104 (11): 1229–35. PMID 11551872. Unknown parameter
|month=ignored (help) - ↑ 15.0 15.1 Gibson CM, Karha J, Murphy SA; et al. (2003). "Early and long-term clinical outcomes associated with reinfarction following fibrinolytic administration in the Thrombolysis in Myocardial Infarction trials". J. Am. Coll. Cardiol. 42 (1): 7–16. PMID 12849652. Unknown parameter
|month=ignored (help) - ↑ Gibson CM (2000). "A union in reperfusion: the concept of facilitated percutaneous coronary intervention". J. Am. Coll. Cardiol. 36 (5): 1497–9. PMID 11079648. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Cannon CP, Piana RN; et al. (1995). "Angiographic predictors of reocclusion after thrombolysis: results from the Thrombolysis in Myocardial Infarction (TIMI) 4 trial". J. Am. Coll. Cardiol. 25 (3): 582–9. PMID 7860900. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Dodge JT, Goel M; et al. (1997). "Angioplasty guidewire velocity: a new simple method to calculate absolute coronary blood velocity and flow". Am. J. Cardiol. 80 (12): 1536–9. PMID 9416931. Unknown parameter
|month=ignored (help) - ↑ 19.0 19.1 19.2 19.3 19.4 Abaci A, Oguzhan A, Eryol NK, Ergin A (1999). "Effect of potential confounding factors on the thrombolysis in myocardial infarction (TIMI) trial frame count and its reproducibility". Circulation. 100 (22): 2219–23. PMID 10577994. Unknown parameter
|month=ignored (help) - ↑ 20.0 20.1 Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV (1999). "Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method". Am. J. Cardiol. 83 (11): 1562–5, A7. PMID 10363873. Unknown parameter
|month=ignored (help) - ↑ 21.0 21.1 Stankovic G, Manginas A, Voudris V; et al. (2000). "Prediction of restenosis after coronary angioplasty by use of a new index: TIMI frame count/minimal luminal diameter ratio". Circulation. 101 (9): 962–8. PMID 10704161. Unknown parameter
|month=ignored (help) - ↑ 22.0 22.1 Barcin C, Denktas AE, Garratt KN, Higano ST, Holmes DR, Lerman A (2003). "Relation of Thrombolysis in Myocardial Infarction (TIMI) frame count to coronary flow parameters". Am. J. Cardiol. 91 (4): 466–9. PMID 12586269. Unknown parameter
|month=ignored (help) - ↑ 23.0 23.1 Umman B, Nisanci Y, Sezer M; et al. (2002). "The relationship between corrected TIMI frame count and myocardial fractional flow reserve". J Invasive Cardiol. 14 (3): 125–8. PMID 11870267. Unknown parameter
|month=ignored (help) - ↑ 24.0 24.1 French JK, Ellis CJ, Webber BJ; et al. (1998). "Abnormal coronary flow in infarct arteries 1 year after myocardial infarction is predicted at 4 weeks by corrected Thrombolysis in Myocardial Infarction (TIMI) frame count and stenosis severity". Am. J. Cardiol. 81 (6): 665–71. PMID 9527071. Unknown parameter
|month=ignored (help) - ↑ 25.0 25.1 25.2 French JK, Straznicky IT, Webber BJ; et al. (1999). "Angiographic frame counts 90 minutes after streptokinase predict left ventricular function at 48 hours following myocardial infarction". Heart. 81 (2): 128–33. PMC 1728934. PMID 9922346. Unknown parameter
|month=ignored (help) - ↑ 26.0 26.1 26.2 French JK, Hyde TA, Straznicky IT; et al. (2000). "Relationship between corrected TIMI frame counts at three weeks and late survival after myocardial infarction". J. Am. Coll. Cardiol. 35 (6): 1516–24. PMID 10807455. Unknown parameter
|month=ignored (help) - ↑ 27.0 27.1 Amos DJ, French JK, Andrews J; et al. (2001). "Corrected TIMI frame counts correlate with stenosis severity and infarct zone wall motion after thrombolytic therapy". Am. Heart J. 141 (4): 586–91. doi:10.1067/mhj.2001.113393. PMID 11275924. Unknown parameter
|month=ignored (help) - ↑ Sahin M, Basoglu T, Canbaz F, Elcik M, Kosus A (2002). "The value of the TIMI frame count method in the diagnosis of coronary no-reflow: a comparison with myocardial perfusion SPECT in patients with acute myocardial infarction". Nucl Med Commun. 23 (12): 1205–10. doi:10.1097/01.mnm.0000046213.83338.9e. PMID 12464786. Unknown parameter
|month=ignored (help) - ↑ Topol EJ, Ohman EM, Armstrong PW; et al. (2000). "Survival outcomes 1 year after reperfusion therapy with either alteplase or reteplase for acute myocardial infarction: results from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) III Trial". Circulation. 102 (15): 1761–5. PMID 11023929. Unknown parameter
|month=ignored (help) - ↑ 30.0 30.1 Dodge JT, Rizzo M, Nykiel M; et al. (1998). "Impact of injection rate on the Thrombolysis in Myocardial Infarction (TIMI) trial frame count". Am. J. Cardiol. 81 (10): 1268–70. PMID 9604968. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Anshelevich M, Murphy S; et al. (2000). "Impact of injections during diagnostic coronary arteriography on coronary patency in the setting of acute myocardial infarction from the TIMI trials. Thrombolysis In Myocardial Infarction". Am. J. Cardiol. 86 (12): 1378–9, A5. PMID 11113418. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Kirtane AJ, Murphy SA; et al. (2001). "Impact of contrast agent type (ionic versus nonionic) used for coronary angiography on angiographic, electrocardiographic, and clinical outcomes following thrombolytic administration in acute myocardial infarction". Catheter Cardiovasc Interv. 53 (1): 6–11. doi:10.1002/ccd.1121. PMID 11329210. Unknown parameter
|month=ignored (help) - ↑ Faile BA, Guzzo JA, Tate DA, Nichols TC, Smith SC, Dehmer GJ (2000). "Effect of sex, hemodynamics, body size, and other clinical variables on the corrected thrombolysis in myocardial infarction frame count used as an assessment of coronary blood flow". Am. Heart J. 140 (2): 308–14. doi:10.1067/mhj.2000.108003. PMID 10925348. Unknown parameter
|month=ignored (help) - ↑ Edep ME, Guarneri EM, Teirstein PS, Phillips PS, Brown DL (1999). "Differences in TIMI frame count following successful reperfusion with stenting or percutaneous transluminal coronary angioplasty for acute myocardial infarction". Am. J. Cardiol. 83 (9): 1326–9. PMID 10235089. Unknown parameter
|month=ignored (help) - ↑ Vrachatis AD, Alpert MA, Georgulas VP; et al. (2001). "Comparative efficacy of primary angioplasty with stent implantation and thrombolysis in restoring basal coronary artery flow in acute ST segment elevation myocardial infarction: quantitative assessment using the corrected TIMI frame count". Angiology. 52 (3): 161–6. PMID 11269778. Unknown parameter
|month=ignored (help) - ↑ Hamada S, Nishiue T, Nakamura S; et al. (2001). "TIMI frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction". J. Am. Coll. Cardiol. 38 (3): 666–71. PMID 11527614. Unknown parameter
|month=ignored (help) - ↑ Capozzolo C, Piscione F, De Luca G; et al. (2001). "Direct coronary stenting: effect on coronary blood flow, immediate and late clinical results". Catheter Cardiovasc Interv. 53 (4): 464–73. PMID 11514995. Unknown parameter
|month=ignored (help) - ↑ Bickel C, Rupprecht HJ, Maimaitiming A; et al. (2002). "The superiority of TIMI frame count in detecting coronary flow changes after coronary stenting compared to TIMI Flow Classification". J Invasive Cardiol. 14 (10): 590–6. PMID 12368511. Unknown parameter
|month=ignored (help) - ↑ Fang JC, Kinlay S, Wexberg P; et al. (2000). "Use of the thrombolysis in myocardial infarction frame count for the quantitative assessment of transplant-associated arteriosclerosis". Am. J. Cardiol. 86 (8): 890–2. PMID 11024410. Unknown parameter
|month=ignored (help) - ↑ 40.0 40.1 40.2 40.3 40.4 Gibson CM, Ryan KA, Murphy SA; et al. (1999). "Impaired coronary blood flow in nonculprit arteries in the setting of acute myocardial infarction. The TIMI Study Group. Thrombolysis in myocardial infarction". J. Am. Coll. Cardiol. 34 (4): 974–82. PMID 10520778. Unknown parameter
|month=ignored (help) - ↑ 41.0 41.1 41.2 Gibson CM, Goel M, Murphy SA; et al. (2000). "Global impairment of coronary blood flow in the setting of acute coronary syndromes (a RESTORE substudy). Randomized Efficacy Study of Tirofiban for Outcomes and Restenosis". Am. J. Cardiol. 86 (12): 1375–7, A5. PMID 11113417. Unknown parameter
|month=ignored (help) - ↑ Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW (2000). "Multiple complex coronary plaques in patients with acute myocardial infarction". N. Engl. J. Med. 343 (13): 915–22. PMID 11006367. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Chen M, Angeja BG; et al. (2002). "Precordial ST-segment depression in inferior myocardial infarction is associated with slow flow in the non-culprit left anterior descending artery" (PDF). J. Thromb. Thrombolysis. 13 (1): 9–12. PMID 11994554. Unknown parameter
|month=ignored (help) - ↑ Gregorini L, Marco J, Kozàkovà M; et al. (1999). "Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction". Circulation. 99 (4): 482–90. PMID 9927393. Unknown parameter
|month=ignored (help) - ↑ Hirsh PD, Hillis LD, Campbell WB, Firth BG, Willerson JT (1981). "Release of prostaglandins and thromboxane into the coronary circulation in patients with ischemic heart disease". N. Engl. J. Med. 304 (12): 685–91. PMID 6894016. Unknown parameter
|month=ignored (help) - ↑ Bush LR, Campbell WB, Kern K; et al. (1984). "The effects of alpha 2-adrenergic and serotonergic receptor antagonists on cyclic blood flow alterations in stenosed canine coronary arteries". Circ. Res. 55 (5): 642–52. PMID 6488486. Unknown parameter
|month=ignored (help) - ↑ Willerson JT, Campbell WB, Winniford MD; et al. (1984). "Conversion from chronic to acute coronary artery disease: speculation regarding mechanisms". Am. J. Cardiol. 54 (10): 1349–54. PMID 6391133. Unknown parameter
|month=ignored (help) - ↑ Apprill P, Schmitz JM, Campbell WB; et al. (1985). "Cyclic blood flow variations induced by platelet-activating factor in stenosed canine coronary arteries despite inhibition of thromboxane synthetase, serotonin receptors, and alpha-adrenergic receptors". Circulation. 72 (2): 397–405. PMID 2988822. Unknown parameter
|month=ignored (help) - ↑ Ashton JH, Golino P, McNatt JM, Buja LM, Willerson JT (1989). "Serotonin S2 and thromboxane A2-prostaglandin H2 receptor blockade provide protection against epinephrine-induced cyclic flow variations in severely narrowed canine coronary arteries". J. Am. Coll. Cardiol. 13 (3): 755–63. PMID 2521875. Unknown parameter
|month=ignored (help) - ↑ Eidt JF, Allison P, Noble S; et al. (1989). "Thrombin is an important mediator of platelet aggregation in stenosed canine coronary arteries with endothelial injury". J. Clin. Invest. 84 (1): 18–27. doi:10.1172/JCI114138. PMC 303947. PMID 2661588. Unknown parameter
|month=ignored (help) - ↑ Willerson JT, Golino P, Eidt J, Campbell WB, Buja LM (1989). "Specific platelet mediators and unstable coronary artery lesions. Experimental evidence and potential clinical implications". Circulation. 80 (1): 198–205. PMID 2661053. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Murphy S, Menown IB; et al. (1999). "Determinants of coronary blood flow after thrombolytic administration. TIMI Study Group. Thrombolysis in Myocardial Infarction". J. Am. Coll. Cardiol. 34 (5): 1403–12. PMID 10551685. Unknown parameter
|month=ignored (help) - ↑ 53.0 53.1 van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F (1998). "Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group". Circulation. 97 (23): 2302–6. PMID 9639373. Unknown parameter
|month=ignored (help) - ↑ Gibson CM, Cannon CP, Murphy SA, et al. Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation. 2002; 105: 1909–1913.
- ↑ 55.0 55.1 55.2 O'Gara PT, Kushner FG, Ascheim DD; et al. (2012). "2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0b013e3182742c84. PMID 23247303. Unknown parameter
|month=ignored (help) - ↑ 56.00 56.01 56.02 56.03 56.04 56.05 56.06 56.07 56.08 56.09 56.10 56.11 56.12 Wu AH, Parsons L, Every NR, Bates ER (2002). "Hospital outcomes in patients presenting with congestive heart failure complicating acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2)". J. Am. Coll. Cardiol. 40 (8): 1389–94. Unknown parameter
|month=ignored (help) - ↑ Wijeysundera HC, Vijayaraghavan R, Nallamothu BK; et al. (2007). "Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials". J. Am. Coll. Cardiol. 49 (4): 422–30. doi:10.1016/j.jacc.2006.09.033. PMID 17258087. Unknown parameter
|month=ignored (help) - ↑ Borgia F, Goodman SG, Halvorsen S; et al. (2010). "Early routine percutaneous coronary intervention after fibrinolysis vs. standard therapy in ST-segment elevation myocardial infarction: a meta-analysis". Eur. Heart J. 31 (17): 2156–69. doi:10.1093/eurheartj/ehq204. PMID 20601393. Unknown parameter
|month=ignored (help) - ↑ Sosnowski C (2008). "[Commentary to the article: Di Mario C, Dudek D, Piscione F, et al.; CARESS-in-AMI (Combined Abciximab RE-teplase Stent Study in Acute Myocardial Infarction) Investigators. Immediate angioplasty versus standard therapy with rescue angioplasty after thrombolysis in the Combined Abciximab REteplase Stent Study in Acute Myocardial Infarction (CARESS-in-AMI): an open, prospective, randomised, multicentre trial. Lancet 2008; 371: 559-68]". Kardiol Pol (in Polish). 66 (4): 461–4, discussion 465–6. PMID 18634182. Unknown parameter
|month=ignored (help) - ↑ Fernandez-Avilés F, Alonso JJ, Castro-Beiras A; et al. (2004). "Routine invasive strategy within 24 hours of thrombolysis versus ischaemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1): a randomised controlled trial". Lancet. 364 (9439): 1045–53. doi:10.1016/S0140-6736(04)17059-1. PMID 15380963.
- ↑ White HD (2008). "Systems of care: need for hub-and-spoke systems for both primary and systematic percutaneous coronary intervention after fibrinolysis". Circulation. 118 (3): 219–22. doi:10.1161/CIRCULATIONAHA.108.790170. PMID 18625904. Unknown parameter
|month=ignored (help)
- Pages with reference errors
- Pages with citations using unsupported parameters
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- CS1 maint: Unrecognized language
- Pages with broken file links
- Disease
- Cardiology
- Ischemic heart diseases
- Intensive care medicine
- Emergency medicine
- Up-To-Date
- Up-To-Date cardiology
- Mature chapter
- Angiopedia