Venlafaxine warnings and precautions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Warnings and Precautions
Warnings
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18–24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
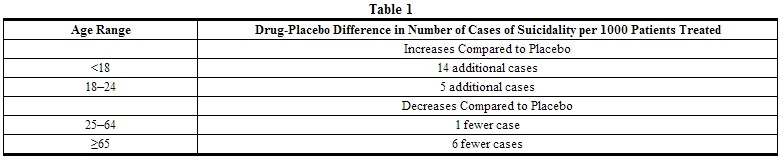 |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms (see PRECAUTIONS and DOSAGE AND ADMINISTRATION, Discontinuation of Treatment with Effexor XR, for a description of the risks of discontinuation of Effexor XR).
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for Effexor XR should be written for the smallest quantity of capsules consistent with good patient management, in order to reduce the risk of overdose.
Bone Fractures
Epidemiological studies show an increased risk of bone fractures in patients receiving serotonin reuptake inhibitors (SRIs) including venlafaxine. The mechanism leading to this risk is not fully understood.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that Effexor XR is not approved for use in treating bipolar depression.
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including Effexor XR, alone but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. John's Wort) and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of Serotonin syndrome.
The concomitant use of Effexor XR with MAOIs intended to treat psychiatric disorders is contraindicated. Effexor XR should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with a MAOI such as linezolid or intravenous methylene blue in a patient taking Effexor XR. Effexor XR should be discontinued before initiating treatment with the MAOI (see CONTRAINDICATIONS and DOSAGE AND ADMINISTRATION).
If concomitant use of Effexor XR with other serotonergic drugs, including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan, and St. John's Wort is clinically warranted, patients should be made aware of a potential increased risk for Serotonin syndrome, particularly during treatment initiation and dose increases.
Treatment with Effexor XR and any concomitant serotonergic agents should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
Sustained Hypertension
Effexor XR treatment is associated with sustained hypertension (defined as treatment-emergent supine diastolic blood pressure (SDBP) ≥90 mm Hg and ≥10 mm Hg above baseline for 3 consecutive on-therapy visits (see Table 2).
An analysis for patients in Effexor (immediate release) studies meeting criteria for sustained hypertension revealed a dose-dependent increase in the incidence of sustained hypertension for Effexor (immediate release) (see Table 3).
An insufficient number of patients received mean doses of Effexor XR over 300 mg/day to fully evaluate the incidence of sustained increases in blood pressure at these higher doses.
 |
In premarketing major depressive disorder studies, 0.7% (5/705) of the Effexor XR-treated patients discontinued treatment because of elevated blood pressure. Among these patients, most of the blood pressure increases were in a modest range (12 to 16 mm Hg, SDBP). In premarketing GAD studies up to 8 weeks and up to 6 months, 0.7% (10/1381) and 1.3% (7/535) of the Effexor XR-treated patients, respectively, discontinued treatment because of elevated blood pressure. Among these patients, most of the blood pressure increases were in a modest range (12 to 25 mm Hg, SDBP up to 8 weeks; 8 to 28 mm Hg up to 6 months). In premarketing Social Anxiety Disorder studies up to 6 months, 0.6% (5/771) of the Effexor XR-treated patients discontinued treatment because of elevated blood pressure. In these patients, the blood pressure increases were modest (1–24 mm Hg, SDBP). In premarketing panic disorder studies up to 12 weeks, 0.5% (5/1001) of the Effexor XR-treated patients discontinued treatment because of elevated blood pressure. In these patients, the blood pressure increases were in a modest range (7 to 19 mm Hg, SDBP).
Sustained increases of SDBP could have adverse consequences. Cases of elevated blood pressure requiring immediate treatment have been reported in post marketing experience. Pre-existing hypertension should be controlled before treatment with venlafaxine. It is recommended that patients receiving Effexor XR have regular monitoring of blood pressure. For patients who experience a sustained increase in blood pressure while receiving venlafaxine, either dose reduction or discontinuation should be considered.
Elevations in Systolic and Diastolic Blood Pressure
In placebo-controlled premarketing studies, there were changes in mean blood pressure (see Table 4 for mean changes in supine systolic and supine diastolic blood pressure). Across most indications, a dose-related increase in supine systolic and diastolic blood pressure was evident in Effexor XR-treated patients.
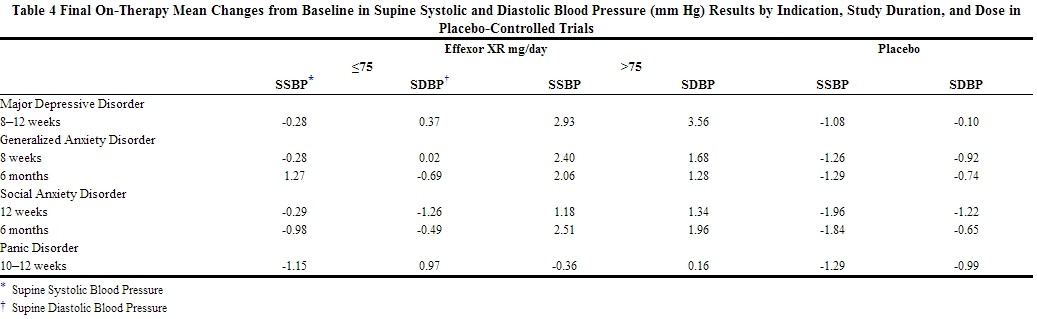 |
Across all clinical trials in MDD, GAD, Social Anxiety Disorder and panic disorder, 1.4% of patients in the Effexor XR-treated groups experienced a ≥15 mm Hg increase in supine diastolic blood pressure with blood pressure ≥105 mm Hg compared to 0.9% of patients in the placebo groups. Similarly, 1% of patients in the Effexor XR-treated groups experienced a ≥20 mm Hg increase in supine systolic blood pressure with blood pressure ≥180 mm Hg compared to 0.3% of patients in the placebo groups.
Mydriasis
Mydriasis has been reported in association with venlafaxine; therefore patients with raised intraocular pressure or those at risk of acute narrow-angle glaucoma (angle-closure glaucoma) should be monitored (see PRECAUTIONS, Information for Patients).
PRECAUTIONS
General
Discontinuation of Treatment with Effexor XR
Discontinuation symptoms have been systematically evaluated in patients taking venlafaxine, to include prospective analyses of clinical trials in Generalized Anxiety Disorder and retrospective surveys of trials in major depressive disorder, and Social Anxiety Disorder. Abrupt discontinuation or dose reduction of venlafaxine at various doses has been found to be associated with the appearance of new symptoms, the frequency of which increased with increased dose level and with longer duration of treatment. Reported symptoms include agitation, anorexia, anxiety, confusion, impaired coordination and balance, diarrhea, dizziness, dry mouth, dysphoric mood, fasciculation, fatigue, flu-like symptoms, headaches, hypomania, insomnia, nausea, nervousness, nightmares, sensory disturbances (including shock-like electrical sensations), somnolence, sweating, tremor, vertigo, and vomiting.
During marketing of Effexor XR, other SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors), and SSRIs (Selective Serotonin Reuptake Inhibitors), there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g. paresthesias such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with Effexor XR. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate (see DOSAGE AND ADMINISTRATION).
insomnia and Nervousness
Treatment-emergent insomnia and nervousness were more commonly reported for patients treated with Effexor XR (venlafaxine hydrochloride) extended-release capsules than with placebo in pooled analyses of short-term major depressive disorder, GAD, [[Social anxiety Disorder]], and panic disorder studies, as shown in Table 5.
 |
insomnia and nervousness each led to drug discontinuation in 0.9% of the patients treated with Effexor XR in major depressive disorder studies.
In GAD trials, insomnia and nervousness led to drug discontinuation in 3% and 2%, respectively, of the patients treated with Effexor XR up to 8 weeks and 2% and 0.7%, respectively, of the patients treated with Effexor XR up to 6 months.
In [[Social anxiety Disorder]] trials, insomnia and nervousness led to drug discontinuation in 2% and 1%, respectively, of the patients treated with Effexor XR up to 12 weeks and 2% and 3% respectively, of the patients treated with Effexor XR up to 6 months.
In panic disorder trials, insomnia and nervousness led to drug discontinuation in 1% and 0.1%, respectively, of the patients treated with Effexor XR up to 12 weeks.
Changes in Weight
Adult Patients
A loss of 5% or more of body weight occurred in 7% of Effexor XR-treated and 2% of placebo-treated patients in the short-term placebo-controlled major depressive disorder trials. The discontinuation rate for weight loss associated with Effexor XR was 0.1% in major depressive disorder studies. In placebo-controlled GAD studies, a loss of 7% or more of body weight occurred in 3% of Effexor XR patients and 1% of placebo patients who received treatment for up to 6 months. The discontinuation rate for weight loss was 0.3% for patients receiving Effexor XR in GAD studies for up to eight weeks. In placebo-controlled [[Social anxiety Disorder]] trials, 4% of the Effexor XR-treated and 1% of the placebo-treated patients sustained a loss of 7% or more of body weight during up to 6 months of treatment. None of the patients receiving Effexor XR in [[Social anxiety Disorder]] studies discontinued for weight loss. In placebo-controlled panic disorder trials, 3% of the Effexor XR-treated and 2% of the placebo-treated patients sustained a loss of 7% or more of body weight during up to 12 weeks of treatment. None of the patients receiving Effexor XR in panic disorder studies discontinued for weight loss.
The safety and efficacy of venlafaxine therapy in combination with weight loss agents, including phentermine, have not been established. Co-administration of Effexor XR and weight loss agents is not recommended. Effexor XR is not indicated for weight loss alone or in combination with other products.
Pediatric Patients
Weight loss has been observed in pediatric patients (ages 6–17) receiving Effexor XR. In a pooled analysis of four eight-week, double-blind, placebo-controlled, flexible dose outpatient trials for major depressive disorder (MDD) and generalized anxiety disorder (GAD), Effexor XR-treated patients lost an average of 0.45 kg (n = 333), while placebo-treated patients gained an average of 0.77 kg (n = 333). More patients treated with Effexor XR than with placebo experienced a weight loss of at least 3.5% in both the MDD and the GAD studies (18% of Effexor XR-treated patients vs. 3.6% of placebo-treated patients; p<0.001). In a 16-week, double-blind, placebo-controlled, flexible dose outpatient trial for [[Social anxiety Disorder]], Effexor XR-treated patients lost an average of 0.75 kg (n = 137), while placebo-treated patients gained an average of 0.76 kg (n = 148). More patients treated with Effexor XR than with placebo experienced a weight loss of at least 3.5% in the [[Social anxiety Disorder]] study (47% of Effexor XR-treated patients vs. 14% of placebo-treated patients; p<0.001). Weight loss was not limited to patients with treatment-emergent anorexia (seePRECAUTIONS, General, Changes in Appetite).
The risks associated with longer-term Effexor XR use were assessed in an open-label MDD study of children and adolescents who received Effexor XR for up to six months. The children and adolescents in the study had increases in weight that were less than expected based on data from age- and sex-matched peers. The difference between observed weight gain and expected weight gain was larger for children (<12 years old) than for adolescents (≥12 years old).
Changes in Height
Pediatric Patients
During the eight-week, placebo-controlled GAD studies, Effexor XR-treated patients (ages 6–17) grew an average of 0.3 cm (n = 122), while placebo-treated patients grew an average of 1.0 cm (n = 132); p=0.041. This difference in height increase was most notable in patients younger than twelve. During the eight-week placebo-controlled MDD studies, Effexor XR-treated patients grew an average of 0.8 cm (n = 146), while placebo-treated patients grew an average of 0.7 cm (n = 147). During the 16-week, placebo-controlled [[Social anxiety Disorder]] study, both the Effexor XR-treated (n = 109) and the placebo-treated (n = 112) patients each grew an average of 1.0 cm. In the six-month, open-label MDD study, children and adolescents had height increases that were less than expected based on data from age- and sex-matched peers. The difference between observed growth rates and expected growth rates was larger for children (<12 years old) than for adolescents (≥12 years old).
Changes in Appetite
Adult Patients
Treatment-emergent anorexia was more commonly reported for Effexor XR-treated (8%) than placebo-treated patients (4%) in the pool of short-term, double-blind, placebo-controlled major depressive disorder studies. The discontinuation rate for anorexia associated with Effexor XR was 1.0% in major depressive disorder studies. Treatment-emergent anorexia was more commonly reported for Effexor XR-treated (8%) than placebo-treated patients (2%) in the pool of short-term, double-blind, placebo-controlled GAD studies. The discontinuation rate for anorexia was 0.9% for patients receiving Effexor XR for up to 8 weeks in GAD studies. Treatment-emergent anorexia was more commonly reported for Effexor XR-treated (17%) than placebo-treated patients (2%) in the pool of short-term, double-blind, placebo-controlled [[Social anxiety Disorder]] studies. The discontinuation rate for anorexia was 0.6% for patients receiving Effexor XR for up to 12 weeks in [[Social anxiety Disorder]] studies; no patients discontinued for anorexia between week 12 and month 6. Treatment-emergent anorexia was more commonly reported for Effexor XR-treated (8%) than placebo-treated patients (3%) in the pool of short-term, double-blind, placebo-controlled panic disorder studies. The discontinuation rate for anorexia was 0.4% for patients receiving Effexor XR for up to 12 weeks in panic disorder studies.
Pediatric Patients
Decreased appetite has been observed in pediatric patients receiving Effexor XR. In the placebo-controlled trials for GAD and MDD, 10% of patients aged 6-17 treated with Effexor XR for up to eight weeks and 3% of patients treated with placebo reported treatment-emergent anorexia (decreased appetite). None of the patients receiving Effexor XR discontinued for anorexia or weight loss. In the placebo-controlled trial for [[Social anxiety Disorder]], 22% and 3% of patients aged 8-17 treated for up to 16 weeks with Effexor XR and placebo, respectively, reported treatment-emergent anorexia (decreased appetite). The discontinuation rates for anorexia were 0.7% and 0.0% for patients receiving Effexor XR and placebo, respectively; the discontinuation rates for weight loss were 0.7% for patients receiving either Effexor XR or placebo.
Activation of Mania/Hypomania
During premarketing major depressive disorder studies, mania or hypomania occurred in 0.3% of Effexor XR-treated patients and no placebo patients. In premarketing GAD studies, no Effexor XR-treated patients and 0.2% of placebo-treated patients experienced mania or hypomania. In premarketing [[Social anxiety Disorder]] studies, 0.2% Effexor XR-treated patients and no placebo-treated patients experienced mania or hypomania. In premarketing panic disorder studies, 0.1% of Effexor XR-treated patients and no placebo-treated patients experienced mania or hypomania. In all premarketing major depressive disorder trials with Effexor (immediate release), mania or hypomania occurred in 0.5% of venlafaxine-treated patients compared with no placebo patients.Mania/hypomania has also been reported in a small proportion of patients with mood disorders who were treated with other marketed drugs to treat major depressive disorder. As with all drugs effective in the treatment of major depressive disorder, Effexor XR should be used cautiously in patients with a history of mania.
Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including Effexor XR. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted may be at greater risk (see PRECAUTIONS, Geriatric Use). Discontinuation of Effexor XR should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
Seizures
During premarketing experience, no seizures occurred among 705 Effexor XR-treated patients in the major depressive disorder studies, among 1381 Effexor XR-treated patients in GAD studies, or among 819 Effexor XR-treated patients in [[Social anxiety Disorder]] studies. In panic disorder studies, 1 seizure occurred among 1,001 Effexor XR-treated patients. In all premarketing major depressive disorder trials with Effexor (immediate release), seizures were reported at various doses in 0.3% (8/3082) of venlafaxine-treated patients. Effexor XR, like many antidepressants, should be used cautiously in patients with a history of seizures and should be discontinued in any patient who develops seizures.
Abnormal Bleeding
SSRIs and SNRIs, including Effexor XR, may increase the risk of bleeding events, ranging from ecchymoses, hematomas, epistaxis, petechiae, and gastrointestinal hemorrhage to life-threatening hemorrhage. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anti-coagulants or other drugs known to affect platelet function may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding.
Patients should be cautioned about the risk of bleeding associated with the concomitant use of Effexor XR and NSAIDs, aspirin, or other drugs that affect coagulation.
Serum Cholesterol Elevatio
Clinically relevant increases in serum cholesterol were recorded in 5.3% of venlafaxine-treated patients and 0.0% of placebo-treated patients treated for at least 3 months in placebo-controlled trials (see ADVERSE REACTIONS-Laboratory Changes). Measurement of serum cholesterol levels should be considered during long-term treatment.
Interstitial Lung Disease and Eosinophilic Pneumonia
Interstitial lung disease and eosinophilic pneumonia associated with venlafaxine therapy have been rarely reported. The possibility of these adverse events should be considered in venlafaxine-treated patients who present with progressive dyspnea, cough or chest discomfort. Such patients should undergo a prompt medical evaluation, and discontinuation of venlafaxine therapy should be considered.[1]