Ceftriaxone microbiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
The bactericidal activity of ceftriaxone results from inhibition of cell wall synthesis. Ceftriaxone has a high degree of stability in the presence of beta-lactamases, both penicillinases and cephalosporinases, of gram-negative and gram-positive bacteria.
In an in vitro study antagonistic effects have been observed with the combination of chloramphenicol and ceftriaxone.
Ceftriaxone has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections described in theINDICATIONS AND USAGE section.
Aerobic gram-negative microorganisms: Acinetobacter calcoaceticus Enterobacter aerogenes Enterobacter cloacae Escherichia coli Haemophilus influenzae (including ampicillin-resistant and beta-lactamase producing strains) Haemophilus parainfluenzae Klebsiella oxytoca Klebsiella pneumoniae Moraxella catarrhalis (including beta-lactamase producing strains) Morganella morganii Neisseria gonorrhoeae (including penicillinase and nonpenicillinase producing strains) Neisseria meningitidis Proteus mirabilis Proteus vulgaris Serratia marcescens
Ceftriaxone is also active against many strains of Pseudomonas aeruginosa.
NOTE: Many strains of the above organisms that are resistant to multiple antibiotics, e.g., penicillins, cephalosporins, and aminoglycosides, are susceptible to ceftriaxone.
Aerobic gram-positive microorganisms: Staphylococcus aureus (including penicillinase-producing strains) Staphylococcus epidermidis Streptococcus pneumoniae Streptococcus pyogenes Viridans group streptococci
NOTE: Methicillin-resistant staphylococci are resistant to cephalosporins, including ceftriaxone. Most strains of Group D streptococci and enterococci, e.g.,Enterococcus (Streptococcus) faecalis, are resistant.
Anaerobic microorganisms: Bacteroides fragilis Clostridium species Peptostreptococcus species
NOTE: Most strains of Clostridium difficile are resistant.
The following in vitro data are available, but their clinical significance is unknown.
Ceftriaxone exhibits in vitro minimal inhibitory concentrations (MICs) of ≤1 mcg/mL or less against most strains of the following microorganisms, however, the safety and effectiveness of ceftriaxone in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-negative microorganisms: Citrobacter diversus Citrobacter freundii Providencia species (including [[Providencia rettgeri) Salmonella species (including Salmonella typhi) Shigella species
Aerobic gram-positive microorganisms: Streptococcus agalactiae
Anaerobic microorganisms: Prevotella (Bacteroides) bivius Porphyromonas (Bacteroides) melaninogenicus
Susceptibility Tests
Dilution Techniques: Quantitative methods are used to determine antimicrobial minimal inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure.1 Standardized procedures are based on a dilution method (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of ceftriaxone powder. For details of susceptibility test methodologies,, the most recent documents of the Clinical and Laboratory Standards Institute (CLSI) for antimicrobial susceptibility testing1-3 should be consulted.
The MIC values for aerobic organisms should be interpreted according to the following criteria:
For Enterobacteriaceae:
The following interpretive criteria should be used when testing Haemophilus species using Haemophilus Test Media (HTM)
The absence of resistant strains precludes defining any categories other than “Susceptible”. Strains yielding results suggestive of a “Nonsusceptible” category should be submitted to a reference laboratory for further testing.
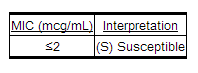
The following interpretive criteria should be used when testing Neisseria gonorrhoeae when using GC agar base and 1% defined growth supplement.
The following interpretive criteria4 should be used when testing Neisseria meningitidis on Mueller-Hinton agar with 5% defribrinated sheep blood:
The absence of resistant neisserial strains precludes defining any categories other than “Susceptible”. Strains yielding results suggestive of a “Nonsusceptible” category should be submitted to a reference laboratory for further testing.
When testing Staphylococcus aureus (methicillin-susceptible, MSSA) the following interpretive criteria should be applied:
For staphylococcal infections, a daily dose of 2 to 4 grams should be administered to achieve >90% target attainment (see DOSAGE AND ADMINISTRATION).
The following interpretive criteria should be used when testing Streptococcus pneumoniae using Mueller-Hinton broth with 2 to 5% lysed horse blood:
Meningitis:
Non-meningitis infections:
For ß-hemolytic streptococci the following interpretive criteria should be used when testing on cation-adjusted Mueller-Hinton broth with 2 to 5% lysed horse blood.
For the Viridians Group streptococci the following interpretive criteria should be applied:
A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of “Intermediate” indicates that the results should be considered equivocal, and if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of the drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standardized ceftriaxone powder should provide the following MIC values:
Diffusion Techniques: Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure3 requires the use of standardized inoculum concentrations. This procedure uses paper discs impregnated with 30 mcg of ceftriaxone to test the susceptibility of microorganisms to ceftriaxone.
Reports from the laboratory providing results of the standard single-disc susceptibility test with a 30 mcg ceftriaxone disc should be interpreted according to the following criteria for aerobic organisms:
For Enterobacteriaceae:
When testing Haemophilus influenzae on Haemophilus Test Media (HTM), the following interpretive criteria should be used:
The absence of resistant strains precludes defining any categories other than “Susceptible”. Strains yielding results suggestive of a “Nonsusceptible” category should be submitted to a reference laboratory for further testing.
The following interpretive criteria should be used when testing Neisseria gonorrhoeae when using GC agar base and 1% defined growth supplement:
For Neisseria meningitidis, the following disc diffusion criteria apply:5
For Straphylococcus aureus (methicillin-susceptibile, MSSA), the following interpretive criteria apply:
The following interpretive criteria should be used when testing ß-hemolytic streptococci using Mueller-Hinton agar supplemented with 5% sheep blood incubated in 5% CO2:
For the Viridians Group streptococci the following criteria apply:
Interpretation should be as stated above for results using dilution techniques. Interpretation involves correlation of the diameter obtained in the disc test with the MIC for ceftriaxone.
Disc diffusion interpretive criteria for ceftriaxone discs against Streptococcus pneumoniae are not available, however, isolates of pneumococci with oxacillin zone diameters of >20 mm are susceptible (MIC ≤0.06 mcg/mL) to penicillin and can be considered susceptible to ceftriaxone. Streptococcus pneumoniae isolates should not be reported as penicillin (ceftriaxone) resistant or intermediate based solely on an oxacillin zone diameter of ≤19 mm. The ceftriaxone MIC should be determined for those isolates with oxacillin zone diameters ≤19 mm.
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms that are used to control the technical aspects of the laboratory procedures. For the diffusion technique, the 30 mcg ceftriaxone disc should provide the following zone diameters in these laboratory test quality control strains:3
Anaerobic Susceptibility Testing by Agar Dilution: For anaerobic bacteria, the susceptibility to ceftriaxone as MICs can be determined by standardized test methods.6 The MIC values obtained should be interpreted according to the following criteria:
As with other susceptibility techniques, the use of laboratory control microorganisms is required to control the technical aspects of the laboratory standardized procedures. Standardized ceftriaxone powder should provide the following MIC values for the indicated standardized anaerobic dilution6testing method:
References
http://www.accessdata.fda.gov/drugsatfda_docs/label/2005/050796lbl.pdf