COVID-19-associated cytokine storm
| https://www.youtube.com/watch?v=AXP9qQ_a0fw}} |
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Shakiba Hassanzadeh, MD[2] Ramyar Ghandriz MD[3] Ifrah Fatima, M.B.B.S[4]
Synonyms and keywords: IL-6 rise in COVID-19, severe inflammatory response in COVID-19, sars cov-2 related hyperimmune response
Overview
Cytokine storms are suspected to be the major cause of death in the previous influenza virus pandemic of 1918, H5N1 epidemic of 1991 and SARS epidemic of 2003. A cytokine storm is an immune reaction that is characterized by dysregulated and excessive release of pro-inflammatory cytokines. Cytokine storms (dysregulated and excessive release of cytokines) have been associated with ARDS in SARS coronavirus (SARS-CoV) and MERS coronavirus (MERS-CoV) infections. The characteristic of this phenomenon could be considered as an indicator of adverse clinical outcomes such as ARDS, shock, and ARF. It has been reported that in patients with COVID-19 there is increase in IL-1B, IFN-γ, IP-10, and monocyte hemoattractant protein 1 (MCP-1) and COVID-19 patients in the intensive care unit (ICU) have increased levels of granulocyte colony-stimulating factor, IP-10, MCP-1, macrophage inflammatory protein-1A, and TNF-α compared to those in general wards. However, in contrast to SARS infection, patients with COVID-19 infection have high levels of IL-4 and IL-10 (secreted by Th2 cells), which are anti-inflammatory cytokines. Potential therapies suggested for cytokine storm include: Corticosteroids, tocilizumab, etoposide and ruxolitinib.
Historical Perspective
- The etiological agent is SARS-CoV-2, named for the similarity of its symptoms to those induced by the severe acute respiratory syndrome, causing coronavirus disease 2019 (COVID-19), is a virus identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China.[1]
- The rapidly increasing number of patients suggest that human-to-human transmission is actively occurring.[2]
- The outbreak was declared a Public Health Emergency of International Concern on 30 January 2020.
- On March 12, 2020, the World Health Organization declared the COVID-19 outbreak a pandemic.
- The term cytokine storm was first used in 1993 by Ferrera et all, to describe the pathophysiology of graft versus host disease (GVHD). [3][4]
- Later, the term was used for pancreatitis, where there is an excessive release of cytokines.
- It has been implicated in a number of infectious as well as non-infectious diseases.
- In the context of infectious diseases, it was first used to describe influenza encephalopathy in 2003. It was also used to describe the pathophysiology of cytomegalovirus, epstein-Barr virus-associated hemophagocytic lymphohistiocytosis, group A streptococcus, influenza virus, variola virus, and severe acute respiratory syndrome coronavirus (SARS-CoV).
- Cytokine storms are believed to cause a disproportionate number of deaths in young individuals. It is suspected to be the major cause of death in previous viral pandemics :[5]
- It is also implicated in other rare viral diseases like variola infection, hantavirus pulmonary syndrome, marburg virus, ebola viruses, lassa and junin viruses, dengue viruses etc. [7]
Classification
- There is no established system for the classification of COVID-19-associated cytokine storm.
Pathophysiology
- A cytokine storm is an immune reaction that is characterized by dysregulated and excessive release of pro-inflammatory cytokines.
Cytokines Involved in Cytokine Storm
- Cytokines are small proteins that are released for cell signaling.
- Cytokines types and their actions include:[8]
- Interferons (INFs)
- Key role in innate immunity
- Regulation of the production of antiviral proteins
- Regulation of the production of antiproliferative proteins
- Interleukins (ILs)
- Regulation of immune cell differentiation and activation
- May be pro- or anti-inflammatory
- Chemokines
- Act as chemo-attractants
- Recruitment of leukocytes
- Colony-stimulating factors
- Induction of hematopoietic progenitor cell proliferation and differentiation
- Tumor necrosis factor (TNF)
- Interferons (INFs)
Pathogenesis of Cytokine Storm
- A cytokine storm is an immune reaction that is characterized by dysregulated and excessive release of pro-inflammatory cytokines.
- During sepsis, cytokine storm may be the cause of tissue or organ injury.[9]
- A cytokine storm causes inflammation, which at the beginning of the disease is local and later spreads around by the systemic circulation. This is followed by the repair and restoration of tissues, organs, and their functions. However, in severe or some inflammations, the repair is with fibrosis which may lead to permanent dysfunction of organs.
- Lung damage caused by pathogens (such as SARS-CoV and influenza virus) may lead to acute lung injury (ALI) or acute respiratory distress syndrome (ARDS).
- Cytokines profiles change over time in patients with sepsis:[8]
- In the early stages of the infection (minutes to hours), cytokines such as TNF and IL-1, and chemokines such as IL-8 and MCP-1 (CCL2) increase.
- Then, an increase in IL-6 is followed.
- Later, IL-10 (anti-inflammatory cytokine) increases.
- Pro-inflammatory cytokines that have a role in ARDS include:[10][11][12][13]
- IL-1β
- IL-6
- IL-8 (CXCL8)
- CCL-2 (MCP-1)
- CCL-3 (Macrophage inflammatory protein-1A)
- CCL-5
- IFN-γ-induced protein10 (IP-10, CXCL10)
- Granulocytemacrophage colony-stimulating factor (GM-CSF)
- Cytokine storms (dysregulated and excessive release of cytokines) have been associated with ARDS in SARS coronavirus (SARS-CoV) and MERS coronavirus (MERS-CoV) infections.[14]
- It has been suggested that the pathogenesis of severe COVID-19 infection may be due to cytokine storm and suppression of Th1 antiviral responses since the following findings have been reported to be associated with severe COVID-19 infection:[15][16]
- It has been reported that in patients with COVID-19 there is increase in IL-1B, IFN-γ , IP-10, and monocyte hemoattractant protein 1 (MCP-1) and COVID-19 patients in the intensive care unit (ICU) have increased levels of granulocyte colony-stimulating factor, IP-10, MCP-1, macrophage inflammatory protein-1A, and TNF-α compared to those in general wards. However, in contrast to SARS infection, patients with COVID-19 infection have high levels of IL-4 and IL-10 (secreted by Th2 cells), which are anti-inflammatory cytokines.[17][15][18][17][16]
| Some of The Cytokines Involved in COVID-19-Associated-Cytokine Storm | ||||||||
|---|---|---|---|---|---|---|---|---|
| Proinflammatory | Interferones |
| ||||||
| Interleukines |
| |||||||
| Chemokines |
| |||||||
| Colony-stimulating
factors |
||||||||
| Tumor necrosis
factor |
||||||||
| Anti-inflammatory | Interleukines | |||||||
Causes
- Coronavirus disease 2019 (COVID-19) is caused by a novel coronavirus called SARS-CoV-2 and is the cause of cytokine storm in COVID-19 infection.
Differentiating COVID-19 cytokine storm from other Diseases
- The most appropriate marker of cytokine storm is an increase in IL-6 level.
- Following is a list of diseases that can cause an increase in IL-6 level and cytokine storm :[19]
Epidemiology and Demographics
- Estimation of an accurate number of severe acute inflammation cases is hard due to the lack of a global system to define the severity of the disease.
- Below is a comparison of different studies on the cytokine level of IL-6 in healthy and severely infected individuals:
| Plasma IL-6 concenteration reported in COVID-19 | ||
|---|---|---|
| Report | Total population(IL-6 level range pg/ml) | Severe infection (IL-6 level range pg/ml) |
| Zhou et al[20] | 191 (5-11) | 54 (8-14) |
| Wu et al[21] | 123 (6-9) | 84 (6-11) |
| Mo et al[22] | 155 (17-96) | 85 (31-165) |
Risk Factors
- There are no established risk factors for COVID-19-associated cytokine storm.
Screening
- There is insufficient evidence to recommend routine screening for COVID-19 related cytokine storm.
Natural History, Complications, and Prognosis
- Cytokine storm has no definition, it denotes a hyperactive immune response characterized by release of interferons, interleukins, TNF, chemokines and several other mediators.
- Since SARS-Cov-1, cytokine elevation was associated with various adverse features.[23][24]
- The characteristic of this phenomena could be considered as an indicator of adverse clinical outcomes such as ARDS, shock and ARF.[25]
- Hyper immunity caused by cytokine storm leading to multi-organ failure in COVID-19 is not fully proved yet, but from previous viral epidemics, it is highly suggested to be considered as a reason to this outcome.
- For more information about COVID-19 natural history,complication and prognosis please click here.
Diagnosis
Diagnostic Study of Choice
The most important cytokines that increase are :[26]
The suggested strategy is to measure the so-called cytokines.
History and Symptoms
- COVID-19 infected individuals who go through more adverse clinical manifestations, such as ARDS and high inflammatory states, are more likely to undergo cytokine elevation.
- For COVID-19 associated history and symptoms click here.
Physical Examination
- For COVID-19 Physical examination click here.
Laboratory Findings
- According to many reviews, Interleukin-6 is the best indicator of the cytokine storm.
- IL-6 concentration has been reported by many studies and is believed to be at a maximal cut of 80 pg/ml in a severe form of the disease.
- Patients with higher levels of IL-6 are at a greater chance of severe disease.[22]
Electrocardiogram
- There are no ECG findings regarding COVID-19-associated Cytokine storm.
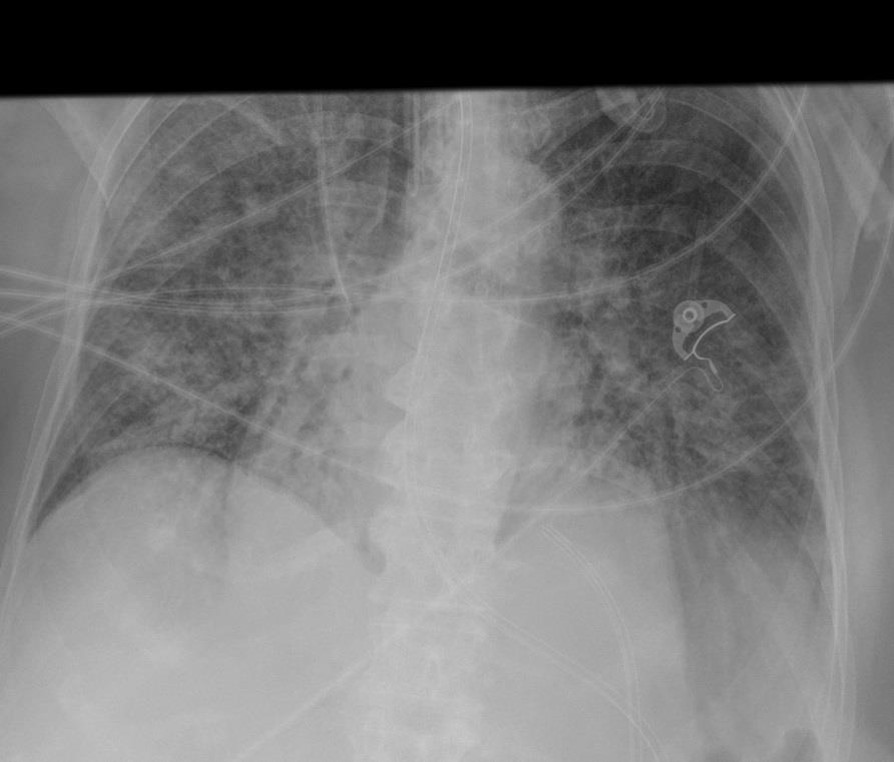
X-ray
- COVID-19 associated cytokine storm leads to Acute respiratory distress syndrome(ARDS).
- X-ray Findings related to COVID-19 ARDS are:
- Ground-glass opacification and consolidation
- Early findings on the chest radiograph include normal or diffuse alveolar opacities (consolidation), which are often bilateral and which obscure the pulmonary vascular markings.
- Later, these opacities progress to more extensive consolidation that is diffuse, and they are often asymmetrical.
Echocardiography or Ultrasound
- There are no echocardiography or ultrasound findings regarding the COVID-19-associated cytokine storm.
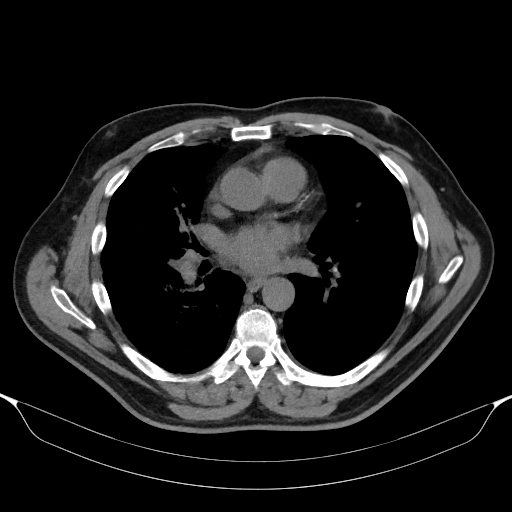
CT scan
- COVID-19 associated cytokine storm Leads to ARDS.
- Multifocal ground glass opacity would be found at both lungs.
MRI
- There are no MRI findings regarding the COVID-19-associated cytokine storm.
Other Imaging Findings
- There are no other imaging findings regarding the COVID-19-associated cytokine storm.
Treatment
Medical Therapy
- Currently, no proven treatment has been suggested.
- Potential therapies for reducing inflammation are:
- Corticosteroids:[29][30]
- Currently in the U.K. there is an ongoing trial (RECOVERY Trial) that Suggest Systemic low dose Dexamethasone decreases mortality by one third.
- Dexamethasone administered as an oral (liquid or tablets) or intravenous preparation. In pregnancy or breastfeeding women, prednisolone (or intravenous hydrocortisone) should be used.
- The suggested dosage is 6 mg once daily for 10 days
- Azithromycin: [31]
- Azithromycin Have shown anti inflammatory effects against Ebola, respiratory syncytial virus and Influenza H1N1.
- Azithromycin 500mg by mouth (or nasogastric tube) or intravenously once daily for 10 days is recommended.
- Remdesivir:[32][33]
- In a first COVID-19 treatment EMA’s human medicines committee (CHMP) recommended remdesivir for EU authorization in a preliminary report.
- A total of 1063 patients underwent randomization in the remdesivir double-blind, placebo-controlled trial.
- Intravenous remdesivir used in adult hospitalized COVID-19 patients in a double-blind, randomized, placebo-controlled trial.
- Dosage of remdesivir is 200 mg loading dose on day 1, which is followed by 100 mg daily for up to 9 additional days or a placebo for up to 10 days in the random trail.
- Preferred regimen in pediatric population who are weighing 3.5 kg to less than 40kg: Remdesivir injection, 100 mg, lyophilized powder which includes a single loading dose of remdesivir 5 mg/kg on Day 1 followed by remdesivir 2.5 mg/kg once daily from Day 2
- Tocilizumab:[34][35][36][37]
- Tocilizumab is an FDA approved drug used for cytokine release syndrome after chimeric antigen receptor infusion, which cause cytokine release storm.
- It is an IL-6 receptor antibody, which is effective in similar clinical manifestations.
- In some off label studies, it has been shown that tocilizumab can cause improvement in patients.
- intravenous infusion with the dose determined by body weight
- 8 mg/kg (maximum: 800 mg/dose) as a single dose; may repeat dose in 8 to 12 hours if signs/symptoms worsen or do not improve.
- 8 mg/kg (maximum: 800 mg/dose) every 12 hours for 2 doses.
- 8 mg/kg as a single dose.
- 4 to 8 mg/kg (usual dose: 400 mg/dose; maximum: 800 mg/dose) as a single dose; may repeat dose in ≥12 hours in patients who remain febrile within 24 hours of initial dose.
- Etoposide:[38]
- Etoposide is used for suppressing cytokine release in hemophagocytic lymphohistiocytosis.
- In patients with severe disease, etoposide can inhibit overwhelming inflammation.
- the suggested dosage is Etoposide 150 mg/m2 daily days 1 and 4
- Ruxolitinib:[39]
- Jack1/2 inhibitor.
- It is used in hemophagocytic lymphohistiocytosis.
- In a prospective randomized trial, it was shown that it reduces the levels of seven cytokines compared to the control group, and resulted in faster improvement in patients with severe infection.
- the suggested dose is 5 mg twice daily.[40]
- Lopinavir-Ritonavir:[41]
- Corticosteroids:[29][30]
Surgery
- Surgical intervention is not recommended for the management of COVID-19-associated cytokine storm.
Primary Prevention
- Since there is no vaccine for COVID-19 there are plenty of primary prevention suggested from CDC such as:[42]
- Hand washing every 10 minutes.
- Using alcoholic hand sanitizer.
- Self quarantine for two weeks if symptomatic.
- To view the primary prevention measures of COVID-19, click here.
Secondary Prevention
- WHO recommends home care for patients with suspected COVID-19 who present with mild symptoms:[43]
- Family members of an infected patient are better to wear masks.
- Using separate bathroom and bedroom by the infected person.
- Using antipyretics and analgesics for fever, myalgias, and headaches
- To view the secondary prevention measures of COVID-19, click here.
References
- ↑ Lu, Jian; Cui, Jie; Qian, Zhaohui; Wang, Yirong; Zhang, Hong; Duan, Yuange; Wu, Xinkai; Yao, Xinmin; Song, Yuhe; Li, Xiang; Wu, Changcheng; Tang, Xiaolu (2020). "On the origin and continuing evolution of SARS-CoV-2". National Science Review. doi:10.1093/nsr/nwaa036. ISSN 2095-5138.
- ↑ Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ Clark IA (2007). "The advent of the cytokine storm". Immunol Cell Biol. 85 (4): 271–3. doi:10.1038/sj.icb.7100062. PMID 17551531.
- ↑ Ferrara JL, Abhyankar S, Gilliland DG (1993). "Cytokine storm of graft-versus-host disease: a critical effector role for interleukin-1". Transplant Proc. 25 (1 Pt 2): 1216–7. PMID 8442093.
- ↑ Osterholm MT (2005). "Preparing for the next pandemic". N Engl J Med. 352 (18): 1839–42. doi:10.1056/NEJMp058068. PMID 15872196.
- ↑ Huang KJ, Su IJ, Theron M, Wu YC, Lai SK, Liu CC; et al. (2005). "An interferon-gamma-related cytokine storm in SARS patients". J Med Virol. 75 (2): 185–94. doi:10.1002/jmv.20255. PMC 7166886 Check
|pmc=value (help). PMID 15602737. - ↑ Mori M, Rothman AL, Kurane I, Montoya JM, Nolte KB, Norman JE; et al. (1999). "High levels of cytokine-producing cells in the lung tissues of patients with fatal hantavirus pulmonary syndrome". J Infect Dis. 179 (2): 295–302. doi:10.1086/314597. PMID 9878011.
- ↑ 8.0 8.1 Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG (2012). "Into the eye of the cytokine storm". Microbiol Mol Biol Rev. 76 (1): 16–32. doi:10.1128/MMBR.05015-11. PMC 3294426. PMID 22390970.
- ↑ Chousterman BG, Swirski FK, Weber GF (2017). "Cytokine storm and sepsis disease pathogenesis". Semin Immunopathol. 39 (5): 517–528. doi:10.1007/s00281-017-0639-8. PMID 28555385.
- ↑ Jiang Y, Xu J, Zhou C, Wu Z, Zhong S, Liu J; et al. (2005). "Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome". Am J Respir Crit Care Med. 171 (8): 850–7. doi:10.1164/rccm.200407-857OC. PMID 15657466.
- ↑ Cameron MJ, Bermejo-Martin JF, Danesh A, Muller MP, Kelvin DJ (2008). "Human immunopathogenesis of severe acute respiratory syndrome (SARS)". Virus Res. 133 (1): 13–9. doi:10.1016/j.virusres.2007.02.014. PMC 7114310 Check
|pmc=value (help). PMID 17374415. - ↑ Reghunathan R, Jayapal M, Hsu LY, Chng HH, Tai D, Leung BP; et al. (2005). "Expression profile of immune response genes in patients with Severe Acute Respiratory Syndrome". BMC Immunol. 6: 2. doi:10.1186/1471-2172-6-2. PMC 546205. PMID 15655079.
- ↑ Ye Q, Wang B, Mao J (2020). "The pathogenesis and treatment of the `Cytokine Storm' in COVID-19". J Infect. 80 (6): 607–613. doi:10.1016/j.jinf.2020.03.037. PMC 7194613 Check
|pmc=value (help). PMID 32283152 Check|pmid=value (help). - ↑ Channappanavar R, Perlman S (2017). "Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology". Semin Immunopathol. 39 (5): 529–539. doi:10.1007/s00281-017-0629-x. PMC 7079893 Check
|pmc=value (help). PMID 28466096. - ↑ 15.0 15.1 Liu J, Li S, Liu J, Liang B, Wang X, Wang H; et al. (2020). "Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients". EBioMedicine. 55: 102763. doi:10.1016/j.ebiom.2020.102763. PMC 7165294 Check
|pmc=value (help). PMID 32361250 Check|pmid=value (help). - ↑ 16.0 16.1 Kuppalli K, Rasmussen AL (2020). "A glimpse into the eye of the COVID-19 cytokine storm". EBioMedicine. 55: 102789. doi:10.1016/j.ebiom.2020.102789. PMC 7204696 Check
|pmc=value (help). PMID 32388462 Check|pmid=value (help). - ↑ 17.0 17.1 Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y; et al. (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299 Check
|pmc=value (help). PMID 31986264. - ↑ Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M (2020). "The cytokine storm in COVID-19: An overview of the involvement of the chemokine/chemokine-receptor system". Cytokine Growth Factor Rev. 53: 25–32. doi:10.1016/j.cytogfr.2020.05.003. PMC 7211650 Check
|pmc=value (help). PMID 32446778 Check|pmid=value (help). - ↑ Magro, Giuseppe (2020). "Cytokine Storm: Is it the only major death factor in COVID-19 patients? Coagulation role". Medical Hypotheses. 142: 109829. doi:10.1016/j.mehy.2020.109829. ISSN 0306-9877.
- ↑ Zhou, Fei; Yu, Ting; Du, Ronghui; Fan, Guohui; Liu, Ying; Liu, Zhibo; Xiang, Jie; Wang, Yeming; Song, Bin; Gu, Xiaoying; Guan, Lulu; Wei, Yuan; Li, Hui; Wu, Xudong; Xu, Jiuyang; Tu, Shengjin; Zhang, Yi; Chen, Hua; Cao, Bin (2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". The Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. ISSN 0140-6736.
- ↑ Wu, Chaomin; Chen, Xiaoyan; Cai, Yanping; Xia, Jia’an; Zhou, Xing; Xu, Sha; Huang, Hanping; Zhang, Li; Zhou, Xia; Du, Chunling; Zhang, Yuye; Song, Juan; Wang, Sijiao; Chao, Yencheng; Yang, Zeyong; Xu, Jie; Zhou, Xin; Chen, Dechang; Xiong, Weining; Xu, Lei; Zhou, Feng; Jiang, Jinjun; Bai, Chunxue; Zheng, Junhua; Song, Yuanlin (2020). "Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China". JAMA Internal Medicine. 180 (7): 934. doi:10.1001/jamainternmed.2020.0994. ISSN 2168-6106.
- ↑ 22.0 22.1 Zhang, Yongxi; Wang, Fan; Cao, Qian; Zheng, Ruiying; Chen, Xiaoping; Ma, Zhiyong; Song, Shihui; Chen, Tielong; Luo, Mingqi; Liang, Ke; Gao, Shicheng; Cheng, Zhenshun; Xiong, Yong; Wang, Hongling; Zhao, Qiu; Deng, Liping; Xiao, Yu; Xing, Yuanyuan; Mo, Pingzheng (2020). "Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China". Clinical Infectious Diseases. doi:10.1093/cid/ciaa270. ISSN 1058-4838.
- ↑ Calfee, Carolyn S; Delucchi, Kevin; Parsons, Polly E; Thompson, B Taylor; Ware, Lorraine B; Matthay, Michael A (2014). "Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials". The Lancet Respiratory Medicine. 2 (8): 611–620. doi:10.1016/S2213-2600(14)70097-9. ISSN 2213-2600.
- ↑ Famous, Katie R.; Delucchi, Kevin; Ware, Lorraine B.; Kangelaris, Kirsten N.; Liu, Kathleen D.; Thompson, B. Taylor; Calfee, Carolyn S. (2017). "Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy". American Journal of Respiratory and Critical Care Medicine. 195 (3): 331–338. doi:10.1164/rccm.201603-0645OC. ISSN 1073-449X.
- ↑ Sinha, Pratik; Delucchi, Kevin L.; Thompson, B. Taylor; McAuley, Daniel F.; Matthay, Michael A.; Calfee, Carolyn S. (2018). "Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study". Intensive Care Medicine. 44 (11): 1859–1869. doi:10.1007/s00134-018-5378-3. ISSN 0342-4642.
- ↑ Schultz, Duane R.; Arnold, Patricia I. (1990). "Properties of four acute phase proteins: C-reactive protein, serum amyloid a protein, α1-acid glycoprotein, and fibrinogen". Seminars in Arthritis and Rheumatism. 20 (3): 129–147. doi:10.1016/0049-0172(90)90055-K. ISSN 0049-0172.
- ↑ name="urlCOVID-19 - rapidly progressive acute respiratory distress syndrome (ARDS) | Radiology Case | Radiopaedia.org">"COVID-19 - rapidly progressive acute respiratory distress syndrome (ARDS) | Radiology Case | Radiopaedia.org".
- ↑ name="urlCOVID-19 pneumonia | Radiology Case | Radiopaedia.org">"COVID-19 pneumonia | Radiology Case | Radiopaedia.org".
- ↑ Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ Horby, Peter; Lim, Wei Shen; Emberson, Jonathan; Mafham, Marion; Bell, Jennifer; Linsell, Louise; Staplin, Natalie; Brightling, Christopher; Ustianowski, Andrew; Elmahi, Einas; Prudon, Benjamin; Green, Christopher; Felton, Timothy; Chadwick, David; Rege, Kanchan; Fegan, Christopher; Chappell, Lucy C; Faust, Saul N; Jaki, Thomas; Jeffery, Katie; Montgomery, Alan; Rowan, Kathryn; Juszczak, Edmund; Baillie, J Kenneth; Haynes, Richard; Landray, Martin J (2020). doi:10.1101/2020.06.22.20137273. Missing or empty
|title=(help) - ↑ Bleyzac, Nathalie; Goutelle, Sylvain; Bourguignon, Laurent; Tod, Michel (2020). "Azithromycin for COVID-19: More Than Just an Antimicrobial?". Clinical Drug Investigation. 40 (8): 683–686. doi:10.1007/s40261-020-00933-3. ISSN 1173-2563.
- ↑ Beigel, John H.; Tomashek, Kay M.; Dodd, Lori E.; Mehta, Aneesh K.; Zingman, Barry S.; Kalil, Andre C.; Hohmann, Elizabeth; Chu, Helen Y.; Luetkemeyer, Annie; Kline, Susan; Lopez de Castilla, Diego; Finberg, Robert W.; Dierberg, Kerry; Tapson, Victor; Hsieh, Lanny; Patterson, Thomas F.; Paredes, Roger; Sweeney, Daniel A.; Short, William R.; Touloumi, Giota; Lye, David Chien; Ohmagari, Norio; Oh, Myoung-don; Ruiz-Palacios, Guillermo M.; Benfield, Thomas; Fätkenheuer, Gerd; Kortepeter, Mark G.; Atmar, Robert L.; Creech, C. Buddy; Lundgren, Jens; Babiker, Abdel G.; Pett, Sarah; Neaton, James D.; Burgess, Timothy H.; Bonnett, Tyler; Green, Michelle; Makowski, Mat; Osinusi, Anu; Nayak, Seema; Lane, H. Clifford (2020). "Remdesivir for the Treatment of Covid-19 — Preliminary Report". New England Journal of Medicine. doi:10.1056/NEJMoa2007764. ISSN 0028-4793.
- ↑ Beigel, John H.; Tomashek, Kay M.; Dodd, Lori E.; Mehta, Aneesh K.; Zingman, Barry S.; Kalil, Andre C.; Hohmann, Elizabeth; Chu, Helen Y.; Luetkemeyer, Annie; Kline, Susan; Lopez de Castilla, Diego; Finberg, Robert W.; Dierberg, Kerry; Tapson, Victor; Hsieh, Lanny; Patterson, Thomas F.; Paredes, Roger; Sweeney, Daniel A.; Short, William R.; Touloumi, Giota; Lye, David Chien; Ohmagari, Norio; Oh, Myoung-don; Ruiz-Palacios, Guillermo M.; Benfield, Thomas; Fätkenheuer, Gerd; Kortepeter, Mark G.; Atmar, Robert L.; Creech, C. Buddy; Lundgren, Jens; Babiker, Abdel G.; Pett, Sarah; Neaton, James D.; Burgess, Timothy H.; Bonnett, Tyler; Green, Michelle; Makowski, Mat; Osinusi, Anu; Nayak, Seema; Lane, H. Clifford (2020). "Remdesivir for the Treatment of Covid-19 — Preliminary Report". New England Journal of Medicine. doi:10.1056/NEJMoa2007764. ISSN 0028-4793.
- ↑ Le, Robert Q.; Li, Liang; Yuan, Weishi; Shord, Stacy S.; Nie, Lei; Habtemariam, Bahru A.; Przepiorka, Donna; Farrell, Ann T.; Pazdur, Richard (2018). "FDA Approval Summary: Tocilizumab for Treatment of Chimeric Antigen Receptor T Cell‐Induced Severe or Life‐Threatening Cytokine Release Syndrome". The Oncologist. 23 (8): 943–947. doi:10.1634/theoncologist.2018-0028. ISSN 1083-7159.
- ↑ Xu, Xiao-Jun; Tang, Yong-Min (2014). "Cytokine release syndrome in cancer immunotherapy with chimeric antigen receptor engineered T cells". Cancer Letters. 343 (2): 172–178. doi:10.1016/j.canlet.2013.10.004. ISSN 0304-3835.
- ↑ Campins L, Boixeda R, Perez-Cordon L, Aranega R, Lopera C, Force L (2020). "Early tocilizumab treatment could improve survival among COVID-19 patients". Clin Exp Rheumatol. 38 (3): 578. PMID 32456769 Check
|pmid=value (help). - ↑ Morena, Valentina; Milazzo, Laura; Oreni, Letizia; Bestetti, Giovanna; Fossali, Tommaso; Bassoli, Cinzia; Torre, Alessandro; Cossu, Maria Vittoria; Minari, Caterina; Ballone, Elisabetta; Perotti, Andrea; Mileto, Davide; Niero, Fosca; Merli, Stefania; Foschi, Antonella; Vimercati, Stefania; Rizzardini, Giuliano; Sollima, Salvatore; Bradanini, Lucia; Galimberti, Laura; Colombo, Riccardo; Micheli, Valeria; Negri, Cristina; Ridolfo, Anna Lisa; Meroni, Luca; Galli, Massimo; Antinori, Spinello; Corbellino, Mario (2020). "Off-label use of tocilizumab for the treatment of SARS-CoV-2 pneumonia in Milan, Italy". European Journal of Internal Medicine. 76: 36–42. doi:10.1016/j.ejim.2020.05.011. ISSN 0953-6205.
- ↑ La Rosée, Paul (2015). "Treatment of hemophagocytic lymphohistiocytosis in adults". Hematology. 2015 (1): 190–196. doi:10.1182/asheducation-2015.1.190. ISSN 1520-4391.
- ↑ Cao, Yang; Wei, Jia; Zou, Liang; Jiang, Tiebin; Wang, Gaoxiang; Chen, Liting; Huang, Liang; Meng, Fankai; Huang, Lifang; Wang, Na; Zhou, Xiaoxi; Luo, Hui; Mao, Zekai; Chen, Xing; Xie, Jungang; Liu, Jing; Cheng, Hui; Zhao, Jianping; Huang, Gang; Wang, Wei; Zhou, Jianfeng (2020). "Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): A multicenter, single-blind, randomized controlled trial". Journal of Allergy and Clinical Immunology. 146 (1): 137–146.e3. doi:10.1016/j.jaci.2020.05.019. ISSN 0091-6749.
- ↑ La Rosée, F.; Bremer, H. C.; Gehrke, I.; Kehr, A.; Hochhaus, A.; Birndt, S.; Fellhauer, M.; Henkes, M.; Kumle, B.; Russo, S. G.; La Rosée, P. (2020). "The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation". Leukemia. 34 (7): 1805–1815. doi:10.1038/s41375-020-0891-0. ISSN 0887-6924.
- ↑ "A Trial of Lopinavir–Ritonavir in Covid-19". New England Journal of Medicine. 382 (21): e68. 2020. doi:10.1056/NEJMc2008043. ISSN 0028-4793.
- ↑ https://www.cdc.gov/coronavirus/2019-ncov/index.html. Missing or empty
|title=(help) - ↑ "Home care for patients with COVID-19 presenting with mild symptoms and management of their contacts".