Hyperkalemia
| Hyperkalemia | |
 | |
|---|---|
| potassium | |
| ICD-10 | E87.5 |
| ICD-9 | 276.7 |
| DiseasesDB | 6242 |
| MedlinePlus | 001179 |
| eMedicine | emerg/261 |
| MeSH | D006947 |
|
WikiDoc Resources for Hyperkalemia |
|
Articles |
|---|
|
Most recent articles on Hyperkalemia Most cited articles on Hyperkalemia |
|
Media |
|
Powerpoint slides on Hyperkalemia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hyperkalemia at Clinical Trials.gov Clinical Trials on Hyperkalemia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hyperkalemia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hyperkalemia Discussion groups on Hyperkalemia Patient Handouts on Hyperkalemia Directions to Hospitals Treating Hyperkalemia Risk calculators and risk factors for Hyperkalemia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hyperkalemia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Hyperkalemia (AE) or Hyperkalaemia (BE) is an elevated blood level (above 5.0 mmol/L) of the electrolyte potassium. The prefix hyper- means high (contrast with hypo-, meaning low). The middle kal refers to kalium, which is Latin for potassium. The end portion of the word, -emia, means "in the blood". Extreme degrees of hyperkalemia are considered a medical emergency due to the risk of potentially fatal arrhythmias.
Signs and symptoms
Symptoms are fairly nonspecific, and generally include malaise, palpitations and muscle weakness; mild breathlessness may indicate metabolic acidosis, one of the settings in which hyperkalemia may occur. Often, however, the problem is detected during screening blood tests for a medical disorder, or it only comes to medical attention after complications have developed, such as cardiac arrhythmia or sudden death.
During the medical history taking, a doctor will dwell on kidney disease and medication use (see below), as these are the main causes. The combination of abdominal pain, hypoglycemia and hyperpigmentation, often in the context of a history of other autoimmune disorders, may be signs of Addison's disease, itself a medical emergency.
Diagnosis
In order to gather enough information for diagnosis, the measurement of potassium needs to be repeated, as the elevation can be due to hemolysis in the first sample. Generally, blood tests for renal function (creatinine, blood urea nitrogen), glucose and occasionally creatine kinase and cortisol will be performed. Calculating the trans-tubular potassium gradient can sometimes help in distinguishing the cause of the hyperkalemia.
In many cases, renal ultrasound will be performed, since hyperkalemia is highly suggestive of renal failure.
Also, electrocardiography (EKG/ECG) may be performed to determine if there is a significant risk of cardiac arrhythmias (see ECG/EKG Findings, below).
Differential diagnosis
Causes include:
Ineffective elimination from the body
- Renal insufficiency
- Medication that interferes with urinary excretion:
- ACE inhibitors and angiotensin receptor blockers
- Potassium-sparing diuretics (e.g. amiloride and spironolactone)
- NSAIDs such as ibuprofen, naproxen, or celecoxib
- The calcineurin inhibitor immunosuppressants ciclosporin and tacrolimus
- The antibiotic trimethoprim
- The antiparasitic drug pentamidine
- Mineralocorticoid deficiency or resistance, such as:
- Addison's disease
- Aldosterone deficiency, including reduced levels due to the blood thinner, heparin
- Some forms of congenital adrenal hyperplasia
- Type IV renal tubular acidosis (resistance of renal tubules to aldosterone)
- Gordon's syndrome (“familial hypertension with hyperkalemia”), a rare genetic disorder caused by defective modulators of salt transporters, including the thiazide-sensitive Na-Cl cotransporter.
Excessive release from cells
- Rhabdomyolysis, burns or any cause of rapid tissue necrosis, including tumor lysis syndrome
- Massive blood transfusion or massive hemolysis
- Shifts/transport out of cells caused by acidosis, low insulin levels, beta-blocker therapy, digoxin overdose, or the paralyzing anesthetic succinylcholine
Excessive intake
- Intoxication with salt-substitute, potassium-containing dietary supplements, or potassium-chloride (KCl) infusion. Note that for a person with normal kidney function and nothing interfering with normal elimination (see above), hyperkalemia by potassium intoxication would be seen only with large infusions of KCl or massive doses of oral KCl supplements.
Lethal injection
Hyperkalemia is intentionally brought about in an execution by lethal injection, potassium chloride being the third and last of the three drugs generally administered to cause death, after sodium thiopental has rendered the subject unconscious, then pancuronium bromide has been added to cause respiratory collapse.
Pseudohyperkalemia
Pseudohyperkalemia is a rise in the amount of potassium that occurs due to excessive leakage of potassium from cells, during or after blood is drawn. It is a laboratory artifact rather than a biological abnormality and can be misleading to doctors.[1] Pseudohyperkalemia is typically caused by hemolysis during venipuncture (by either excessive vacuum of the blood draw or by a syringe needle that is of too fine a gauge); excessive tournequet time or fist clenching during phlebotomy (which presumably leads to efflux of potassium from the muscle cells into the bloodstream).[2]; or by a delay in the processing of the blood specimen. It can also occur in specimens from patients with abnormally high numbers of platelets (>1,000,000/mm³), leukocytes (> 100 000/mm³), or erythrocytes (hematocrit > 55%). People with "leakier" cell membranes have been found, whose blood must be separated immediately to avoid pseudohyperkalemia.[3]
Complete Differential Diagnosis of Hyperkalemia
Decreased Renal Potassium Excretion
- Acute Renal Failure
- Addison's Disease
- Bilateral adrenalectomy
- Chronic Renal Failure
- Congestive Heart Failure
- Drugs
- Gordon's Syndrome
- Graft-versus-host disease of the kidney
- Hyporeninemic hypoaldosteronism
- Postuterojejunostomy
- Primary defect in potassium transport
- Renal tubular acidosis
- Specific enzyme defect
- Tubular unresponsivness
Increased Potassium Cellular Release
- Burns
- Chemotherapy
- Crush Syndrome
- Depolarizing muscle paralysis
- Diabetic ketoacidosis
- Drugs
- Heavy exercise
- Hyperkalemic periodic paralysis
- Hyperosmolar states
- Hypoinsulinemia
- Insulin Deficiency
- Intravascular hemolysis
- Mannitol hyperosmolality
- Metabolic Acidosis
- Radiocontrast hyperosmolality
- Respiratory Acidosis
- Rhabdomyolysis
- Tourniquet Syndrome
- Trauma
- Tumor Lysis Syndrome
Pseudohyperkalemia
- Delayed centrifugation hemolysis
- Extravascular hemolysis
- Leukocytosis
- Rapid aspiration hemolysis
- Stagnation hemolysis
- Thrombocytosis
Excess Potassium Intake
- Dietary excess
- IV potassium replacement
- KCl
- Oral potassium intake
- Potassium-containing drugs
- Transfusion
Pathophysiology
Potassium is the most abundant intracellular cation. It is critically important for many physiologic processes, including maintenance of cellular membrane potential, homeostasis of cell volume, and transmission of action potentials in nerve cells. Its main dietary sources are vegetables (tomato and potato), fruits (orange and banana) and meat. Elimination is through the gastrointestinal tract and the kidney.
The renal elimination of potassium is passive (through the glomeruli), and resorption is active in the proximal tubule and the ascending limb of the loop of Henle. There is active excretion of potassium in the distal tubule and the collecting duct; both are controlled by aldosterone.
Hyperkalemia develops when there is excessive production (oral intake, tissue breakdown) or ineffective elimination of potassium. Ineffective elimination can be hormonal (in aldosterone deficiency) or due to causes in the renal parenchyma that impair excretion.
Increased extracellular potassium levels result in depolarization of the membrane potentials of cells. This depolarization opens some voltage-gated sodium channels, but not enough to generate an action potential. After a short while, the open sodium channels inactivate and become refractory, increasing the threshold to generate an action potential. This leads to the impairment of neuromuscular, cardiac, and gastrointestinal organ systems. Of most concern is the impairment of cardiac conduction which can result in ventricular fibrillation or asystole.
Patients with the rare hereditary condition of hyperkalemic periodic paralysis appear to have a heightened sensitivity of muscular symptoms that are associated with transient elevation of potassium levels. Episodes of muscle weakness and spasms can be precipitated by exercise or fasting in these subjects.
Laboratory Evaluation
Initial
- Calcium
- Phosphate
- Magnesium
- Blood urea nitrogen (BUN)/creatinine
Extensive Evaluation
- Cortisol
- Renin
- Aldosterone levels
- Transtubular potassium gradient (by assessing potassium+ secretion)
Electrocardiographic Findings
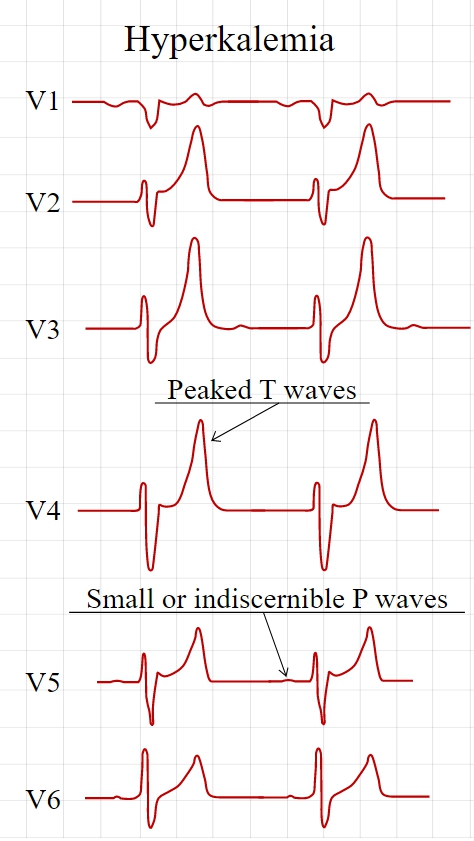
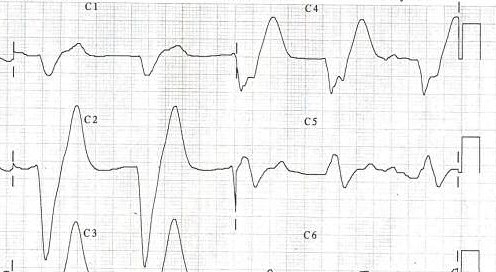
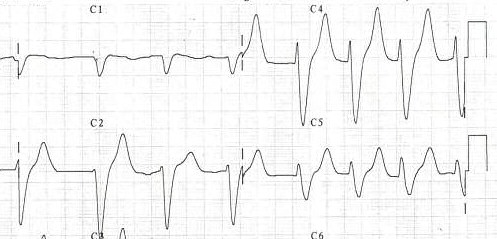
Electrocardiography (ECG) is generally done early to identify any influences on the heart, as hyperkalemia may cause fatal arrhythmias. With moderate hyperkalemia, there is reduction of the size of the P wave and development of tent-shaped T waves. Further hyperkalemia will lead to widening of the QRS complex, that ultimately may become sinusoidal in shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. Also, (as noted above), hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex.
Spcific findings include the following:
Tall, narrow, and peaked T waves
- Earliest sign of hyperkalemia
- Occurs with K > 5.5 meq/li
- Differential diagnosis of this EKG change includes the T wave changes of bradycardia or stroke. Prominent U waves and QTc prolongation are more consistent with stroke than hyperkalemia.
Intraventricular conduction defect
Decrease of the amplitude of the P wave or an absent P wave
- Decreased P wave amplitude occurs when the K is > 7.0 meq/li
- P waves may be absent when the K is > 8.8 meq/li
- The impulses are still being generated in the SA node and are conducted to the ventricles through specialized atrial fibers without depolarizing the atrial muscle
ST segment changes simulating current of injury
- Have been labeled the dialyzable current of injury
Cardiac arrhythmias: bradyarrhythmias, tachyarrhythmias, atrioventricular conduction defects
- Occurs with severe hyperkalemia, not mild to moderate hyperkalemia
-
Tall, symmetric, narrow based T waves in a hyperkalemic patient.
-
A patient's EKG with hyperkalemia.
-
Same patient's EKG during treatment.
Treatment
When arrhythmias occur, or when potassium levels exceed 6.5 mmol/l, emergency lowering of potassium levels is mandated. Several agents are used to lower K levels. Choice depends on the degree and cause of the hyperkalemia, and other aspects of the patient's condition.
- Calcium supplementation (calcium gluconate 10% (10ml), preferably through a central venous catheter as the calcium may cause phlebitis) does not lower potassium but decreases myocardial excitability, protecting against life threatening arrhythmias.
- Insulin (e.g. intravenous injection of 10-15u of (short acting) insulin (e.g. Actrapid) {along with 50ml of 50% dextrose to prevent hypoglycemia}) will lead to a shift of potassium ions into cells, secondary to increased activity of the sodium-potassium ATPase.
- Bicarbonate therapy (e.g. 1 ampule (45mEq) infused over 5 minutes) is effective in cases of metabolic acidosis. The bicarbonate ion will stimulate an exchange of cellular H+ for Na+, thus leading to stimulation of the sodium-potassium ATPase.
- Salbutamol (albuterol, Ventolin®) is a β2-selective catacholamine that is administered by nebuliser (e.g. 10-20 mg). This drug promotes movement of K into cells, lowering the blood levels.
- Polystyrene sulfonate (Calcium Resonium, Kayexalate) is a binding resin that binds K within the intestine and removes it from the body by defecation. Calcium Resonium (15g three times a day in water) can be given by mouth. Kayexelate can be given by mouth or as an enema. In both cases, the resin absorbs K within the intestine and carries it out of the body by defecation. This medication may cause diarrhea.
- Refractory or severe cases may need dialysis to remove the potassium from the circulation.
- Preventing recurrence of hyperkalemia typically involves reduction of dietary potassium, removal of an offending medication, and/or the addition of a diuretic (such as furosemide (Lasix®) or hydrochlorothiazide).
See also
References
- ↑ Sevastos N et al. (2006) Pseudohyperkalemia in serum: the phenomenon and its clinical magnitude. J Lab Clin Med, 147(3):139-44; PMID 16503244.
- ↑ Don BR et al. (1990) Pseudohyperkalemia caused by fist clenching during phlebotomy. N Engl J Med, 322(18):1290-2; PMID 2325722.
- ↑ Iolascon A et al. (1999) Familial pseudohyperkalemia maps to the same locus as dehydrated hereditary stomatocytosis. Blood, 93(9):3120-3; PMID 10216110.
additional Resources
- Schaefer TJ, Wolford RW (2005). Disorders of potassium. Emerg Med Clin North Am, 23(3), 723-47; PMID 15982543.
- Kasper DL et al (Eds). Harrison's Principles of Internal Medicine, 16th ed, chapter 41, pages 258-61; ISBN 0-07-140235-7.
- Rose, B.D. and T.W. Post, Clinical Physiology of Acid-Base and Electrolyte Disorders, 5th ed. 2001, pages 888-930; ISBN 0-07-134682-1.
Template:Endocrine, nutritional and metabolic pathology