Glomerular disease: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (103 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Glomerulonephritis_pathophysiology]] | |||
{{CMG}}; {{AE}}{{MJ}}, {{HK}} | |||
< | '''This page contains general information about Glomerular disease.''' | ||
<br>'''For more information on specific types, please visit the pages on:''' | |||
:'''[[Nephritic syndrome]]''' | |||
:'''[[Nephrotic syndrome]]''' | |||
:'''[[Fabry's disease]]''' | |||
:'''[[Post-streptococcal glomerulonephritis]]''' | |||
:'''[[Lupus nephritis|Lupus nephritis]]''' | |||
:'''[[Goodpasture syndrome|Antiglomerular basement membrane disease]]''' | |||
:'''[[Goodpasture syndrome|(Goodpasture's syndrome)]]''' | |||
:'''[[Cryoglobulinemia]]''' | |||
:'''[[Henoch-Schönlein purpura]]''' | |||
:'''[[Amyloidosis]]''' | |||
:'''Pulmonary-renal syndromes ([[vasculitis]])''' | |||
:'''[[Thin basement membrane disease]]''' | |||
:'''[[Alport syndrome|Alport's Syndrome]]''' | |||
:'''[[Goodpasture syndrome|anti-GBM Disease]]''' | |||
:'''[[Hypertensive nephrosclerosis]]''' | |||
:'''[[Subacute bacterial endocarditis]]''' | |||
==Overview== | ==Overview== | ||
Glomerular disease | Glomerular disease is a condition that affects the [[glomerulus]]. It consists of different diseases with different clinical courses and treatment options. Glomerular disease can be isolated [[hematuria]], isolated [[proteinuria]]; [[acute]] or [[chronic]] glomerulonephritis, and [[nephrotic]] or [[Nephritic syndrome|nephritic]] features of glomerulonephritis. The end stage of all of these diseases will be [[glomerulosclerosis]] which is characterized by [[fibrosis]] of the [[glomerulus]], and [[end-stage renal disease]]. | ||
==Classification== | ==Classification== | ||
=== Glomerular dieseases can be classified into several clinical and pathological syndromes as below: === | |||
{| class="wikitable" | |||
!Syndrome | |||
!Disease | |||
|- | |||
|Acute nephritic syndromes | |||
| | |||
* [[Poststreptococcal glomerulonephritis]] | |||
* [[Subacute bacterial endocarditis]] | |||
* [[Lupus nephritis]] | |||
* [[Goodpasture syndrome|Antiglomerular basement membrane disease]] | |||
* [[IgA nephropathy]] | |||
* [[Vasculitis|ANCA Small-Vessel Vasculitis]] | |||
** [[Granulomatosis with polyangiitis|Granulomatosis with Polyangiitis (Wegener's)]] | |||
** [[Microscopic polyangiitis|Microscopic Polyangiitis]] | |||
** [[Eosinophilic granulomatosis with polyangiitis|Churg-Strauss Syndrome]] | |||
* [[Membranoproliferative glomerulonephritis|Membranoproliferative Glomerulonephritis]] | |||
* Mesangioproliferative Glomerulonephritis | |||
|- | |||
|Nephrotic syndrome | |||
| | |||
* [[Minimal change disease|Minimal Change Disease]] | |||
* [[Focal segmental glomerulosclerosis|Focal Segmental Glomerulosclerosis]] | |||
* [[Membranous glomerulonephritis|Membranous Glomerulonephritis]] | |||
* [[Diabetic nephropathy|Diabetic Nephropathy]] | |||
|- | |||
|Glomerular Deposition Diseases | |||
| | |||
* [[Light chain disease|Light Chain Deposition Disease]] | |||
* [[Amyloidosis|Renal Amyloidosis]] | |||
* Fibrillary-Immunotactoid Glomerulopathy | |||
* [[Fabry's disease|Fabry's Disease]] | |||
|- | |||
|Pulmonary-Renal Syndromes: | |||
| | |||
* [[Goodpasture syndrome|Goodpasture's syndrome]] | |||
* [[Granulomatosis with polyangiitis|Granulomatosis with polyangiitis (Wegener's)]] | |||
* [[Microscopic polyangiitis]] | |||
* [[Churg-Strauss syndrome|Churg-Strauss vasculitis]] | |||
* [[Henoch-Schönlein purpura]] | |||
* [[Cryoglobulinemia]] | |||
|- | |||
|Basement Membrane Syndromes | |||
| | |||
* [[Anti-glomerular basement membrane antibody|Anti-GBM Disease]] | |||
* [[Alport syndrome|Alport's Syndrome]] | |||
* [[Thin basement membrane disease|Thin Basement Membrane Disease]] | |||
* [[Nail-patella syndrome|Nail-Patella Syndrome]] | |||
|- | |||
|Glomerular-Vascular Syndromes | |||
| | |||
* Atherosclerotic Nephropathy | |||
* [[Hypertensive nephropathy|Hypertensive nephrosclerosis]] | |||
* [[Cholesterol emboli syndrome|Cholesterol Emboli]] | |||
* [[Sickle-cell disease|Sickle Cell Disease]] | |||
* [[Thrombotic microangiopathies|Thrombotic Microangiopathies]] | |||
* [[Antiphospholipid syndrome|Antiphospholipid Antibody Syndrome]] | |||
|- | |||
|Infectious Disease–Associated Syndromes | |||
| | |||
* [[Post-streptococcal glomerulonephritis|Post-Streptococcal Glomerulonephritis]] | |||
* [[Endocarditis|Subacute bacterial endocarditis]] | |||
* [[Human Immunodeficiency Virus (HIV)|Human Immunodeficiency Virus]] | |||
* [[Hepatitis|Hepatitis B and C]] | |||
* Other Viruses | |||
* [[Syphilis]] | |||
* [[Leprosy]] | |||
* [[Malaria]] | |||
* [[Schistosomiasis]] | |||
* Other Parasites | |||
|} | |||
==== | === Also, glomerular diseases can be classified based on their clinical and urinary pattern in to below types: === | ||
==== Mild nephritc: ==== | |||
This category include mild nephritic sediment that is associated with less than half involvement of glomeruli. | |||
==== | ==== Severe nephritic: ==== | ||
More severe clinical features such as edema, heavy [[proteinuria]], hypertension, and/or [[renal failure]] may occur. | |||
=== | ==== Nephrotic: ==== | ||
This | This syndrome is associated with heavy proteinuria and lipiduria. | ||
==== | === Glomerular diseases also may classified by their presentation as below: === | ||
==== | ====== Glomerular [[hematuria]]: ====== | ||
1- Isolated [[hematuria]] | |||
2- Glomerulonephritis ([[nephritic syndrome]]) | |||
==== | ====== [[Proteinuria]]: ====== | ||
1-Isolated non-nephrotic [[proteinuria]] | |||
2- [[Nephrotic syndrome]] | |||
== | ====== [[Rapidly progressive glomerulonephritis]] ====== | ||
=== | |||
=== Glomerulonephritis === | |||
Glomerulonephritis which is inflammation of the glomeruli can be classified based on pathogenic type into three subtypes: | |||
* '''Immune complex glomerulonephritis: Granular deposit of immune complex.''' | |||
*# Infection mediated types | |||
*# Autoimmune types, eg [[SLE]] | |||
*# MPGN | |||
*# [[IgA nephropathy|IgA nephropathy (Berger nephropathy)]] | |||
*# [[Membranous nephropathy]] | |||
* '''Anti-GBM disease: Linear deposit''' | |||
*# [[Goodpasture syndrome]] (renal and lung involvement) | |||
*# Renal involvement alone | |||
*# Lung involvement alone | |||
* '''ANCA associated, small vessels vasculitis: Few or no deposit''' | |||
*# [[Granulomatosis with polyangiitis]] ([[Granulomatosis with polyangiitis|Wegener granulomatosis]]) | |||
*# [[Eosinophilic granulomatosis with polyangiitis]] ([[Churg-Strauss syndrome]]) | |||
*# [[Microscopic polyangiitis]] | |||
Glomerulonephritis (nephritic syndrome) also may be classified based on disease course into [[Acute nephritic syndrome|acute]] or [[chronic nephritic syndrome]]; primary vs secondary causes; or systemic vs renal limited disease. '''''For more information about nephritic syndrome classifications click [[Nephritic syndrome classification|here]].''''' | |||
==Differential Diagnosis== | |||
The various types of glomerular diseases should be differentiated from each other based on associations, presence of [[pitting edema]], [[hematuria]], [[hypertension]], [[hemoptysis]], [[oliguria]], peri-orbital edema, [[hyperlipidemia]], type of [[antibodies]], [[Light microscope|light]] and [[Electron microscopy|electron microscopic]] features. The following table differentiates between various types of glumerular diseases: | |||
{| class="wikitable" | {| class="wikitable" | ||
! rowspan=" | ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Glomerular diseases | ||
! | ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | ||
! | ! colspan="9" style="background:#4479BA; color: #FFFFFF;" align="center" + |History and Symtoms | ||
! colspan | ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Laboratory Findings | ||
! colspan=" | ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Pathology | ||
|- | |- | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |- | ||
! | ! rowspan="13" style="background:#4479BA; color: #FFFFFF;" align="center" + |Acute Nephritic Syndromes | ||
! colspan="2" |[[Post-streptococcal glomerulonephritis|Poststreptococcal Glomerulonephritis]]<ref name="pmid13022878">{{cite journal| author=GERMUTH FG| title=A comparative histologic and immunologic study in rabbits of induced hypersensitivity of the serum sickness type. | journal=J Exp Med | year= 1953 | volume= 97 | issue= 2 | pages= 257-82 | pmid=13022878 | doi= | pmc=PMC2136196 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13022878 }}</ref><ref name="pmid5031005">{{cite journal| author=Germuth FG, Senterfit LB, Dreesman GR| title=Immune complex disease. V. The nature of the circulating complexes associated with glomerular alterations in the chronic BSA-rabbit system. | journal=Johns Hopkins Med J | year= 1972 | volume= 130 | issue= 6 | pages= 344-57 | pmid=5031005 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=5031005 }}</ref><ref name="pmid22895519">{{cite journal| author=Radhakrishnan J, Cattran DC| title=The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines--application to the individual patient. | journal=Kidney Int | year= 2012 | volume= 82 | issue= 8 | pages= 840-56 | pmid=22895519 | doi=10.1038/ki.2012.280 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22895519 }}</ref> | |||
! | | | ||
* [[Streptococcal infections|Streptococcal]] [[skin]] [[infections]] | |||
* [[Streptococcus|Streptococcal]] [[pharyngitis]] | |||
* 2-3 weeks after [[infection]] | |||
| | |||
| | |||
| | | | ||
* | * [[Fever]] | ||
* | * [[Fatigue]] | ||
* Skin [[rash]] | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| | | | ||
* | * [[Anti-dsDNA antibody|Anti-dsDNA antibodies]] | ||
* | * Anti-C1q antibodies | ||
* [[Antineutrophil cytoplasmic antibodies]] ([[ANCA]]) | |||
* | |||
| | | | ||
* Hypercellular and [[inflamed]] [[glomeruli]] | |||
| | | | ||
- | * Sub-[[epithelial]] [[immune complex]] deposits | ||
* Obliteration of epithelial cell foot processes | |||
| | | | ||
- | * [[Immune]] complex GN | ||
* Granular deposit | |||
|- | |||
! colspan="2" |[[Renal]] disease due to [[Endocarditis|Subacute Bacterial Endocarditis]], or [[cardiac shunt]] (Atrioventricular)<ref name="pmid6380288">{{cite journal |vauthors=Neugarten J, Baldwin DS |title=Glomerulonephritis in bacterial endocarditis |journal=Am. J. Med. |volume=77 |issue=2 |pages=297–304 |date=August 1984 |pmid=6380288 |doi= |url=}}</ref><ref name="pmid6831779">{{cite journal |vauthors=Arze RS, Rashid H, Morley R, Ward MK, Kerr DN |title=Shunt nephritis: report of two cases and review of the literature |journal=Clin. Nephrol. |volume=19 |issue=1 |pages=48–53 |date=January 1983 |pmid=6831779 |doi= |url=}}</ref> | |||
| | | | ||
* History of [[infective endocarditis]] mostly due to ''[[Staphylococcus aureus|S. aureus]]'' | |||
* [[Cardiac shunt]] | |||
| | | | ||
+/- | * [[Fever]] | ||
* [[Fatigue]] | |||
* Weight loss | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| | | | ||
- | * [[Myeloperoxidase (MPO)|ANCA (myeloperoxidase)]] positive in 1/3 | ||
* Activation of the [[alternative complement pathway]] (Decreased [[C3 (complement)|C3]], C4) | |||
* Positive [[RF]] | |||
* Positive [[Anti-glomerular basement membrane antibody|anti-GBM autoantibodies]] | |||
| | | | ||
* [[Rapidly progressive glomerulonephritis|Crescentic]] GN is the most common pathological features | |||
* [[Membranoproliferative glomerulonephritis|Diffuse membranoproliferative glomerulonephritis]] features | |||
* Focal proliferative GN | |||
* Mesangial proliferative GN | |||
| | | | ||
* [[Mesangial cell|Mesangial]] deposits, | |||
* Subendothelial deposits | |||
* Subepithelial "humps," in minority of cases | |||
| | | | ||
- | * Pauci-immune GN | ||
|- | |||
! colspan="2" |[[Lupus nephritis|Lupus Nephritis]]<ref name="pmid14717922">{{cite journal |vauthors=Weening JJ, D'Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M |title=The classification of glomerulonephritis in systemic lupus erythematosus revisited |journal=Kidney Int. |volume=65 |issue=2 |pages=521–30 |date=February 2004 |pmid=14717922 |doi=10.1111/j.1523-1755.2004.00443.x |url=}}</ref> | |||
| | | | ||
* History of [[SLE]] features | |||
| | | | ||
- | * [[Systemic lupus erythematosus|Lupus]] criteria: | ||
** [[Malar rash]] | |||
** [[Arthritis]] | |||
** [[Arthralgia]] | |||
** [[Anemia]] | |||
** Easy bruising | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| | | | ||
- | * Anti-C1q antibodies | ||
* [[Anti-dsDNA antibody|Anti-dsDNA]] | |||
| | | | ||
* | * Differs based on the disease classification | ||
| | | | ||
* | * Differs based on the disease classification | ||
| | | | ||
* Differs based on the disease classification, mostly immune complex GN | |||
* Granular deposit | |||
|- | |- | ||
! | ! colspan="2" |[[Goodpasture syndrome|Antiglomerular Basement Membrane Disease]] [[Goodpasture syndrome|(Goodpasture's syndrome)]]<ref name="pmid8914046">{{cite journal |vauthors=Bolton WK |title=Goodpasture's syndrome |journal=Kidney Int. |volume=50 |issue=5 |pages=1753–66 |date=November 1996 |pmid=8914046 |doi= |url=}}</ref><ref name="pmid1090223">{{cite journal |vauthors=Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P |title=Goodpasture's syndrome: normal renal diagnostic findings |journal=Ann. Intern. Med. |volume=82 |issue=2 |pages=215–8 |date=February 1975 |pmid=1090223 |doi= |url=}}</ref> | ||
| | | | ||
* | * Young adults | ||
| | | | ||
* | * Dry [[cough]] | ||
* [[Hemoptysis]] | |||
* [[Malaise]] | |||
* [[Fever]] and chills | |||
* [[Arthralgia]] | |||
* [[Fatigue]] | |||
* [[Lethargy]] | |||
* [[Pallor]] | |||
* [[Anorexia]] | |||
* Easy [[bruising]] | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | | + | ||
|<nowiki>+</nowiki> | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+</nowiki> | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* | * [[Myeloperoxidase (MPO)|ANCA (myeloperoxidase)]] | ||
* Positive [[Anti-glomerular basement membrane antibody|anti-GBM autoantibodies]] | |||
| | |||
* Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | |||
|Diffuse thickening of the [[glomerular basement membrane]] with absence of sub-[[Epithelial cells|epithelial]] and sub-[[endothelial]] deposits | |||
| | | | ||
* | * Immune complex GN | ||
* Linear deposit | |||
|- | |- | ||
! | ! colspan="2" |[[IgA nephropathy|IgA Nephropathy]]<ref name="pmid21949093">{{cite journal |vauthors=Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA |title=The pathophysiology of IgA nephropathy |journal=J. Am. Soc. Nephrol. |volume=22 |issue=10 |pages=1795–803 |date=October 2011 |pmid=21949093 |pmc=3892742 |doi=10.1681/ASN.2011050464 |url=}}</ref><ref name="pmid23782179">{{cite journal |vauthors=Wyatt RJ, Julian BA |title=IgA nephropathy |journal=N. Engl. J. Med. |volume=368 |issue=25 |pages=2402–14 |date=June 2013 |pmid=23782179 |doi=10.1056/NEJMra1206793 |url=}}</ref> | ||
| | | | ||
* | * Young children | ||
* | * History of [[mucosal]] [[infections]] (e.g. [[gastroenteritis]]) and [[upper respiratory tract infection]] | ||
* 2-3 days after [[infection]] (synpharyngitic) | |||
* | |||
| | | | ||
* Low grade [[fever]] | |||
* [[Flank pain]] | |||
|<nowiki>+</nowiki> | |||
| +/- | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| - | |||
| | |||
* Immune complex deposition | |||
| | |||
* Crescent formation | |||
| | | | ||
* | * [[Mesangial cell|Mesangial]] proliferation | ||
| | | | ||
* | * Immune complex GN, granular deposite | ||
| | |- | ||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |- | ||
! rowspan="3" |[[Vasculitis|ANCA Small-Vessel Vasculitis]]<ref name="pmid8746284">{{cite journal |vauthors=Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC |title=Vasculitis and rapidly progressive glomerulonephritis in the elderly |journal=Postgrad Med J |volume=72 |issue=843 |pages=41–4 |date=January 1996 |pmid=8746284 |pmc=2398323 |doi= |url=}}</ref><ref name="pmid12631105">{{cite journal |vauthors=Jennette JC |title=Rapidly progressive crescentic glomerulonephritis |journal=Kidney Int. |volume=63 |issue=3 |pages=1164–77 |date=March 2003 |pmid=12631105 |doi=10.1046/j.1523-1755.2003.00843.x |url=}}</ref> | |||
! | ! colspan="1" |[[Granulomatosis with polyangiitis|Granulomatosis with Polyangiitis (Wegener's)]]<ref name="pmid18172777">{{cite journal |vauthors=Renaudineau Y, Le Meur Y |title=Renal involvement in Wegener's granulomatosis |journal=Clin Rev Allergy Immunol |volume=35 |issue=1-2 |pages=22–9 |date=October 2008 |pmid=18172777 |doi=10.1007/s12016-007-8066-6 |url=}}</ref><ref name="pmid6384024">{{cite journal |vauthors=Weiss MA, Crissman JD |title=Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis |journal=Hum. Pathol. |volume=15 |issue=10 |pages=943–56 |date=October 1984 |pmid=6384024 |doi= |url=}}</ref><ref name="pmid18524109">{{cite journal |vauthors=Pagnoux C |title=[Wegener's granulomatosis and microscopic polyangiitis] |language=French |journal=Rev Prat |volume=58 |issue=5 |pages=522–32 |date=March 2008 |pmid=18524109 |doi= |url=}}</ref> | ||
| | | | ||
* | * Middle age male | ||
| | | | ||
* | * Constitutional symptoms | ||
* | * [[Dyspnea]] | ||
* [[Purpura]] | |||
* [[Arthralgia|Arthralgias]] | |||
* Neurologic dysfunction | |||
* [[Rhinosinusitis|Sinusitis]] | |||
* [[Otitis media]] | |||
* [[Epistaxis]]. | |||
|<nowiki>+</nowiki> | |||
| + | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| - | | - | ||
| | | | ||
* | * [[ANCA]] | ||
| | | | ||
* | * [[Necrotizing]] and [[Crescentic glomerulonephritis|crescentic]] glomerulonephritis | ||
| | |||
| | | | ||
* | * Subendothelial [[edema]] | ||
* Microthrombosis | |||
* [[Degranulation]] of [[neutrophils]] | |||
| | | | ||
* | * Pauci-immune GN | ||
|- | |||
! colspan="1" |[[Microscopic polyangiitis|Microscopic Polyangiitis]]<ref name="pmid20688249">{{cite journal |vauthors=Chung SA, Seo P |title=Microscopic polyangiitis |journal=Rheum. Dis. Clin. North Am. |volume=36 |issue=3 |pages=545–58 |date=August 2010 |pmid=20688249 |pmc=2917831 |doi=10.1016/j.rdc.2010.04.003 |url=}}</ref> | |||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
| | |||
* Constitutional symptoms | |||
* [[Dyspnea]] | |||
* [[Purpura]] | |||
* [[Arthralgia|Arthralgias]] | |||
* Neurologic dysfunction | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | | + | ||
| | | | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* | * [[P-ANCA]] | ||
| | | | ||
* | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
| | | | ||
* | * Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | ||
| | | | ||
* | * Pauci-immune GN | ||
|- | |||
! colspan="1" |[[Eosinophilic granulomatosis with polyangiitis|Churg-Strauss Syndrome]]<ref name="pmid16632015">{{cite journal |vauthors=Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C |title=Renal involvement in Churg-Strauss syndrome |journal=Am. J. Kidney Dis. |volume=47 |issue=5 |pages=770–9 |date=May 2006 |pmid=16632015 |doi=10.1053/j.ajkd.2006.01.026 |url=}}</ref> | |||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
| | |||
* [[Asthma]] | |||
* [[Rhinosinusitis|Sinusitis]] | |||
* [[Myalgia]] | |||
* [[Arthralgia]] | |||
* [[Purpura]] | |||
* [[Cardiac arrhythmia|Arrythmias]] | |||
* [[Peripheral neuropathy]] | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* Hypercellular and inflamed glomeruli | * [[C-ANCA]] | ||
| | |||
* Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | |||
| | |||
* Hypercellular and [[inflamed]] [[glomeruli]] (Crescent formation) | |||
| | | | ||
* | * Pauci-immune GN | ||
|- | |- | ||
! colspan="2" |[[Membranoproliferative glomerulonephritis|Membranoproliferative Glomerulonephritis]]<ref name="pmid19908070">{{cite journal |vauthors=Alchi B, Jayne D |title=Membranoproliferative glomerulonephritis |journal=Pediatr. Nephrol. |volume=25 |issue=8 |pages=1409–18 |date=August 2010 |pmid=19908070 |pmc=2887509 |doi=10.1007/s00467-009-1322-7 |url=}}</ref><ref name="pmid657595">{{cite journal |vauthors=Davis AE, Schneeberger EE, Grupe WE, McCluskey RT |title=Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children |journal=Clin. Nephrol. |volume=9 |issue=5 |pages=184–93 |date=May 1978 |pmid=657595 |doi= |url=}}</ref> | |||
| | | | ||
* | * [[Idiopathic]] | ||
* [[Hepatitis B]] and [[Hepatitis C|C]] (Type 1) | |||
* C3 nepritic factor (Type2) | |||
| | | | ||
* | * [[Hematuria]] | ||
* [[ | * [[Oliguria]] | ||
* | * [[Periorbital edema]] | ||
* [[ | * [[Hypertension]] | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| | | | ||
* | * Thick [[glomerular basement membrane]] (Tram-track appearance) | ||
| | | | ||
| | * [[Mesangial cell|Mesangial]] proliferation | ||
* [[Leukocytes|Leukocyte]] infiltration | |||
| | |||
* Immune complex GN | |||
* Granular deposite | |||
|- | |- | ||
! colspan="2" |[[Henoch-Schönlein purpura]] <ref name="pmid8023818">{{cite journal |vauthors=Jennette JC, Falk RJ |title=The pathology of vasculitis involving the kidney |journal=Am. J. Kidney Dis. |volume=24 |issue=1 |pages=130–41 |date=July 1994 |pmid=8023818 |doi= |url=}}</ref> | |||
| | | | ||
* | * Most common in young male, following [[Upper respiratory tract|upper respiratory]] [[infections]] | ||
| | | | ||
* | * '''Skin manifestations-''' Palpable [[purpura]] on buttocks | ||
* | * '''Gastrointestinal''' '''manifestations-''' | ||
* | ** [[Abdominal pain]] | ||
| | ** [[Melena]] | ||
** [[Dysentery|Bloody diarrhea]] | |||
** [[Hematemesis]] | |||
* '''Joints''' '''manifestations-''' | |||
** [[Arthralgia]] | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| - | |||
| | |||
* Diffuse mesangial IgA deposits often associated with mesangial hypercellularity | |||
| | |||
* Diffuse mesangial IgA deposits often associated with mesangial hypercellularity | |||
| | |||
* Immune complex GN, granular deposite | |||
|- | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |||
! colspan="2" |[[Cryoglobulinemia]]<ref name="pmid26802335">{{cite journal |vauthors=Fogo AB, Lusco MA, Najafian B, Alpers CE |title=AJKD Atlas of Renal Pathology: Cryoglobulinemic Glomerulonephritis |journal=Am. J. Kidney Dis. |volume=67 |issue=2 |pages=e5–7 |date=February 2016 |pmid=26802335 |doi=10.1053/j.ajkd.2015.12.007 |url=}}</ref> | |||
|Patients having [[cryoglobulinemia]] may have positive history of: | |||
* [[Hepatitis C|Hepatitis C infection]] | |||
* [[Hepatitis B|Hepatitis B infection]] | |||
* Leg ulcers | |||
* Recurrent [[thrombosis]] | |||
|'''Pulmonary symptoms:''' | |||
* [[Difficulty breathing]] | |||
* Cough | |||
'''Cutaneous symptoms:''' | |||
* [[Purpura]] | |||
* [[Skin ulcer]] | |||
'''Gastrointestinal symptoms:''' | |||
* Abdominal pain | |||
'''General symptoms:''' | |||
* Fever | |||
* [[Arthralgia]], | |||
* [[Myalgia]] | |||
* [[Fatigue]] | |||
* [[Blurred vision|Blurring]]/loss of vision | |||
* [[Diplopia]] | |||
* [[Confusion]] | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| | |||
* [[Membranoproliferative glomerulonephritis]] | |||
| | |||
* [[Mesangial cell|Mesangial]] and subendothelial deposits | |||
| | | | ||
+ (C- | * Prominent [[IgM]] and C3 | ||
|- | |||
! rowspan="9" style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic Syndrome | |||
! colspan="2" |[[Minimal change disease|Minimal Change Disease]]<ref name="pmid17195422">{{cite journal |vauthors=Saha TC, Singh H |title=Minimal change disease: a review |journal=South. Med. J. |volume=99 |issue=11 |pages=1264–70 |date=November 2006 |pmid=17195422 |doi=10.1097/01.smj.0000243183.87381.c2 |url=}}</ref><ref name="pmid27092244">{{cite journal |vauthors=Saleem MA, Kobayashi Y |title=Cell biology and genetics of minimal change disease |journal=F1000Res |volume=5 |issue= |pages= |date=2016 |pmid=27092244 |pmc=4821284 |doi=10.12688/f1000research.7300.1 |url=}}</ref> | |||
| colspan="2" | | |||
* Young children | |||
* Recent [[infection]] and [[immunization]] | |||
* [[Atopy]] | |||
* [[Hodgkin's lymphoma|Hodgkin lymphoma]] | |||
* [[Thrombosis]] (due to [[Urinary system|urinary]] loss of [[Antithrombin III|antithrombin-III]]) | |||
| - | |||
| + | |||
| - | |||
| + | |||
| +/- | |||
| + | |||
| - | |||
| + | |||
| | |||
| | |||
* Normal | |||
| | |||
* Fusion of [[podocytes]] | |||
| - | |||
|- | |||
! colspan="2" |[[Focal segmental glomerulosclerosis|Focal Segmental Glomerulosclerosis]]<ref name="pmid28242845">{{cite journal |vauthors=Rosenberg AZ, Kopp JB |title=Focal Segmental Glomerulosclerosis |journal=Clin J Am Soc Nephrol |volume=12 |issue=3 |pages=502–517 |date=March 2017 |pmid=28242845 |pmc=5338705 |doi=10.2215/CJN.05960616 |url=}}</ref><ref name="pmid25168829">{{cite journal |vauthors=Jefferson JA, Shankland SJ |title=The pathogenesis of focal segmental glomerulosclerosis |journal=Adv Chronic Kidney Dis |volume=21 |issue=5 |pages=408–16 |date=September 2014 |pmid=25168829 |pmc=4149756 |doi=10.1053/j.ackd.2014.05.009 |url=}}</ref><ref name="pmid2429634">{{cite journal |vauthors=Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT |title=Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens |journal=Arch. Pathol. Lab. Med. |volume=110 |issue=10 |pages=902–5 |date=October 1986 |pmid=2429634 |doi= |url=}}</ref> | |||
| colspan="2" | | |||
* Idiopathic | |||
* [[Human Immunodeficiency Virus (HIV)|HIV]] | |||
* [[Heroine hydrochloride|Heroine]] use | |||
* [[Sickle-cell disease|Sickle cell disease]] | |||
* [[Interferon]] | |||
* Severe [[obesity]] | |||
* [[Cryoglobulinemia|Mixed cryoglobulinemia]] ([[Hepatitis C]]) | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| + | |||
| | |||
| | |||
* Focal (some [[glomeruli]]) and segmental (only part of [[glomerulus]]) | |||
| | | | ||
* | * Effacement of [[podocytes]] | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
! colspan="2" |[[Membranous glomerulonephritis|Membranous Glomerulonephritis]]<ref name="pmid25558821">{{cite journal |vauthors=Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ |title=Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment |journal=J. Formos. Med. Assoc. |volume=114 |issue=2 |pages=102–11 |date=February 2015 |pmid=25558821 |doi=10.1016/j.jfma.2014.11.002 |url=}}</ref><ref name="pmid10495797">{{cite journal |vauthors=Wasserstein AG |title=Membranous glomerulonephritis |journal=J. Am. Soc. Nephrol. |volume=8 |issue=4 |pages=664–74 |date=April 1997 |pmid=10495797 |doi= |url=}}</ref> | |||
| colspan="2" | | |||
* [[Idiopathic]] | |||
* [[Hepatitis B]] and [[Hepatitis C|C]] | |||
* [[Solid tumors]] | |||
* [[Systemic lupus erythematosus]] | |||
* Drugs ([[NSAIDS]], pencilamine, [[gold]], [[captopril]]) | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
| + | |||
|Immune complex deposition | |||
| | | | ||
* | * Thick [[glomerular basement membrane]] | ||
| | | | ||
* | * Sub-[[Epithelial cells|epithelial]] [[immune complex]] depositis with 'spike and dome' appearance | ||
|Immune complex GN, granular deposite | |||
|- | |||
! colspan="2" |[[Diabetic nephropathy|Diabetic Nephropathy]]<ref name="pmid11978659">{{cite journal| author=Drummond K, Mauer M, International Diabetic Nephropathy Study Group| title=The early natural history of nephropathy in type 1 diabetes: II. Early renal structural changes in type 1 diabetes. | journal=Diabetes | year= 2002 | volume= 51 | issue= 5 |pages= 1580-7 | pmid=11978659 | doi= | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11978659 }}</ref><ref name="pmid3699305">{{cite journal| author=Hørlyck A, Gundersen HJ, Osterby R| title=The cortical distribution pattern of diabetic glomerulopathy. | journal=Diabetologia | year= 1986 | volume= 29| issue= 3 | pages= 146-50 | pmid=3699305 | doi= | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3699305 }}</ref><ref name="pmid21422926">{{cite journal| author=Alpers CE, Hudkins KL| title=Mouse models of diabetic nephropathy. | journal=Curr Opin Nephrol Hypertens | year= 2011 | volume= 20 | issue= 3 |pages= 278-84 | pmid=21422926 | doi=10.1097/MNH.0b013e3283451901 | pmc=PMC3658822 |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21422926 }}</ref><ref name="pmid19970254">{{cite journal| author=Kimmelstiel P, Wilson C| title=Intercapillary Lesions in the Glomeruli of the Kidney. | journal=Am J Pathol | year= 1936 | volume= 12 | issue= 1 |pages= 83-98.7 | pmid=19970254 | doi= | pmc=PMC1911022 |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19970254 }}</ref><ref name="pmid2766585">{{cite journal| author=Alpers CE, Biava CG| title=Idiopathic lobular glomerulonephritis (nodular mesangial sclerosis): a distinct diagnostic entity. | journal=Clin Nephrol | year= 1989 | volume= 32 | issue= 2 | pages= 68-74 | pmid=2766585 | doi= | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2766585 }}</ref><ref name="pmid17536064">{{cite journal| author=Toyoda M, Najafian B, Kim Y, Caramori ML, Mauer M| title=Podocyte detachment and reduced glomerular capillary endothelial fenestration in human type 1 diabetic nephropathy. | journal=Diabetes | year= 2007 | volume= 56 | issue= 8 | pages= 2155-60 |pmid=17536064 | doi=10.2337/db07-0019 | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17536064 }}</ref><ref name="pmid16565248">{{cite journal| author=Najafian B, Crosson JT, Kim Y, Mauer M| title=Glomerulotubular junction abnormalities are associated with proteinuria in type 1 diabetes. | journal=J Am Soc Nephrol | year= 2006 | volume= 17 | issue= 4 Suppl 2 | pages= S53-60| pmid=16565248 | doi=10.1681/ASN.2005121342 | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16565248 }}</ref><ref name="pmid12660325">{{cite journal| author=Najafian B, Kim Y, Crosson JT, Mauer M| title=Atubular glomeruli and glomerulotubular junction abnormalities in diabetic nephropathy. | journal=J Am Soc Nephrol | year= 2003 | volume= 14 | issue= 4 | pages= 908-17 | pmid=12660325 | doi= | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12660325 }}</ref><ref name="pmid21659756">{{cite journal| author=Najafian B, Alpers CE, Fogo AB| title=Pathology of human diabetic nephropathy. |journal=Contrib Nephrol | year= 2011 | volume= 170 | issue= | pages= 36-47 | pmid=21659756 |doi=10.1159/000324942 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21659756 }}</ref><ref name="pmid216597562">{{cite journal| author=Najafian B, Alpers CE, Fogo AB| title=Pathology of human diabetic nephropathy. |journal=Contrib Nephrol | year= 2011 | volume= 170 | issue= | pages= 36-47 | pmid=21659756 |doi=10.1159/000324942 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21659756 }}</ref> | |||
| colspan="2" |'''''For more information on diabetes [[Diabetes mellitus|click here]]'''.'' | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |<nowiki>+/-</nowiki> | ||
| + | |||
|<nowiki>-</nowiki> | |||
| + | |||
| | |||
| | |||
* Diffuse [[Mesangial cell|mesangial]] matrix expansion (nodular glomerulosclerosis) | |||
* Increased [[Mesangial cell|mesangial]] hypercellularity | |||
* Prominent glomerular basement membranes | |||
* Thick [[basement membrane]] without any deposit | |||
| | |||
* Nodular glomerulosclerosis | |||
| - | |||
|- | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |||
! rowspan="4" | [[Glomerular deposition disease|Glomerular Deposition Diseases]] | |||
![[Light chain nephropathy|Light Chain Deposition Disease]]<ref name="pmid21511832">{{cite journal |vauthors=Hutchison CA, Cockwell P, Stringer S, Bradwell A, Cook M, Gertz MA, Dispenzieri A, Winters JL, Kumar S, Rajkumar SV, Kyle RA, Leung N |title=Early reduction of serum-free light chains associates with renal recovery in myeloma kidney |journal=J. Am. Soc. Nephrol. |volume=22 |issue=6 |pages=1129–36 |date=June 2011 |pmid=21511832 |pmc=3103732 |doi=10.1681/ASN.2010080857 |url=}}</ref> | |||
| | |||
* Occurs in the setting of high tumor burden | |||
| - | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
| + | |||
| - | |||
| | |||
* Light-chain deposits | |||
| | |||
* Granular deposits on electron microscopy | |||
| | |||
* Detection of light chain deposits using anti–light chain antibody | |||
|- | |||
![[Amyloidosis|Renal Amyloidosis]]<ref name="pmid23227278">{{cite journal |vauthors=Baker KR, Rice L |title=The amyloidoses: clinical features, diagnosis and treatment |journal=Methodist Debakey Cardiovasc J |volume=8 |issue=3 |pages=3–7 |date=2012 |pmid=23227278 |pmc=3487569 |doi= |url=}}</ref><ref name="pmid23979488">{{cite journal |vauthors=Gillmore JD, Hawkins PN |title=Pathophysiology and treatment of systemic amyloidosis |journal=Nat Rev Nephrol |volume=9 |issue=10 |pages=574–86 |date=October 2013 |pmid=23979488 |doi=10.1038/nrneph.2013.171 |url=}}</ref><ref name="pmid26155101">{{cite journal |vauthors=Jerzykowska S, Cymerys M, Gil LA, Balcerzak A, Pupek-Musialik D, Komarnicki MA |title=Primary systemic amyloidosis as a real diagnostic challenge - case study |journal=Cent Eur J Immunol |volume=39 |issue=1 |pages=61–6 |date=2014 |pmid=26155101 |pmc=4439975 |doi=10.5114/ceji.2014.42126 |url=}}</ref><ref name="pmid16409147">{{cite journal |vauthors=Pepys MB |title=Amyloidosis |journal=Annu. Rev. Med. |volume=57 |issue= |pages=223–41 |date=2006 |pmid=16409147 |doi=10.1146/annurev.med.57.121304.131243 |url=}}</ref> | |||
| | |||
* For the secondary causes of amloidosis: | |||
* [[Tuberculosis]] | |||
* [[Familial mediterranean fever|Familial Mediterranean fever]] | |||
* [[Rheumatoid arthritis]] | |||
* [[Multiple myeloma]] | |||
| | |||
* [[Dyspnea]] | |||
* [[Lethargy]] | |||
* Weight loss | |||
* [[Hemorrhagic diathesis|Bleeding tendency]] | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+ | |<nowiki>+/-</nowiki> | ||
| + | |||
| | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| + | |||
| - | |||
| | |||
* Diffuse glomerular deposition of amorphous hyaline material (nodular pattern), in mesangium (weakly staining with periodic acid-Schiff (PAS) | |||
| | |||
* Nodular deposit | |||
| | |||
* AA amyloidosis type: negative for immunoglobulins and complement | |||
* AL amyloidosis type: Positive for lambda or kappa light chains | |||
|- | |||
!Fibrillary-Immunotactoid Glomerulopathy<ref name="pmid1996564">{{cite journal |vauthors=Korbet SM, Schwartz MM, Lewis EJ |title=Immunotactoid glomerulopathy |journal=Am. J. Kidney Dis. |volume=17 |issue=3 |pages=247–57 |date=March 1991 |pmid=1996564 |doi= |url=}}</ref> | |||
| | |||
* [[Malignancy]] | |||
* [[Monoclonal gammopathy]] | |||
* [[Autoimmunity|Autoimmune]] disease | |||
| - | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| - | |||
| | |||
* Diffuse sclerosing glomerulonephritis | |||
* Diffuse proliferative glomerulonephritis | |||
* Membranoproliferative glomerulonephritis | |||
* Mesangioproliferative/sclerosing disease | |||
* Membranous glomerulonephritis | |||
| | |||
* Large fibrillar deposits in the mesangium randomly | |||
* Glomerular capillary walls different from amloidosis | |||
* No staining with Congo red or thioflavine-T or with antibodies to a specific type | |||
| | |||
* Positive for immunoglobulin G (IgG), C3 | |||
* [[Light chain|Kappa]] and lambda (ie, polyclonal) light chains | |||
|- | |||
![[Fabry's disease|Fabry's Disease]]<ref name="pmid12068025">{{cite journal |vauthors=Alroy J, Sabnis S, Kopp JB |title=Renal pathology in Fabry disease |journal=J. Am. Soc. Nephrol. |volume=13 Suppl 2 |issue= |pages=S134–8 |date=June 2002 |pmid=12068025 |doi= |url=}}</ref><ref name="pmid9918480">{{cite journal |author=Meikle PJ, Hopwood JJ, Clague AE, Carey WF |title=Prevalence of lysosomal storage disorders |journal=[[JAMA : the Journal of the American Medical Association]] |volume=281 |issue=3 |pages=249–54 |year=1999 |month=January |pmid=9918480 |doi= |url=}}</ref><ref name="pmid11889412">{{cite journal |author=Branton MH, Schiffmann R, Sabnis SG, ''et al.'' |title=Natural history of Fabry renal disease: influence of alpha-galactosidase A activity and genetic mutations on clinical course |journal=[[Medicine]] |volume=81 |issue=2 |pages=122–38 |year=2002 |month=March |pmid=11889412 |doi= |url=}}</ref> | |||
| | |||
* [[Family history]] suggestive of the disorder | |||
| | |||
* [[Anhidrosis]] or decreased sweating | |||
* [[Fatigue (medical)|Fatigue]] | |||
* [[Angiokeratoma|Angiokeratomas]] | |||
* Burning pain of the extremities | |||
* Corneal opacities. | |||
* [[Dysphagia]] | |||
* [[Abdominal pain]] | |||
* [[Steatorrhea]] | |||
* [[Delayed puberty]] | |||
* [[Raynaud's phenomenon]] | |||
* [[Hearing loss]] | |||
* [[Telangiectasis]] | |||
* [[Ataxia]] | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| + | | + | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| + | |||
| - | |||
| | | | ||
* | * Vacuolization of visceral glomerular epithelial cells (podocytes) and distal tubular epithelial cells | ||
| | * Glycolipid accumulation | ||
| | |||
* Myeloid or zebra bodies: Gb3 deposition within enlarged secondary lysosomes as lamellated membrane structures | |||
* Inclusions, composed of concentric layers (onion skin appearance) | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |- | ||
! | ! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Basement Membrane Syndrome | ||
! colspan="2" |[[Alport syndrome|Alport's Syndrome]]<ref name="pmid111374282">{{cite journal| author=McCarthy PA, Maino DM| title=Alport syndrome: a review. | journal=Clin Eye Vis Care | year= 2000 | volume= 12 | issue= 3-4 | pages= 139-150 | pmid=11137428 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11137428 }}</ref><ref name="pmid84141532">{{cite journal| author=Chugh KS, Sakhuja V, Agarwal A, Jha V, Joshi K, Datta BN et al.| title=Hereditary nephritis (Alport's syndrome)--clinical profile and inheritance in 28 kindreds. | journal=Nephrol Dial Transplant | year= 1993 | volume= 8 | issue= 8 | pages= 690-5 | pmid=8414153 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8414153 }}</ref><ref name="pmid8414153">{{cite journal| author=Chugh KS, Sakhuja V, Agarwal A, Jha V, Joshi K, Datta BN et al.| title=Hereditary nephritis (Alport's syndrome)--clinical profile and inheritance in 28 kindreds. | journal=Nephrol Dial Transplant | year= 1993 | volume= 8 | issue= 8 | pages= 690-5 | pmid=8414153 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8414153 }}</ref><ref name="pmid11137428">{{cite journal| author=McCarthy PA, Maino DM| title=Alport syndrome: a review. | journal=Clin Eye Vis Care | year= 2000 | volume= 12 | issue= 3-4 | pages= 139-150 | pmid=11137428 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11137428 }}</ref><ref name="pmid7819734">{{cite journal| author=Amari F, Segawa K, Ando F| title=Lens coloboma and Alport-like glomerulonephritis. | journal=Eur J Ophthalmol | year= 1994 | volume= 4 | issue= 3 | pages= 181-3 | pmid=7819734 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7819734 }}</ref><ref name="pmid6871140">{{cite journal| author=Govan JA| title=Ocular manifestations of Alport's syndrome: a hereditary disorder of basement membranes? | journal=Br J Ophthalmol | year= 1983 | volume= 67 | issue= 8 | pages= 493-503 | pmid=6871140 | doi= | pmc=PMC1040106 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6871140 }}</ref> | |||
| | | | ||
* | * Positive family history | ||
* | |'''Auditary:''' | ||
* | *Early [[Tinnitus]] | ||
| | *[[Vertigo]] | ||
* | *High-frequency progressive bilateral [[Hearing impairment|hearing loss]] | ||
* | |||
* | '''Occular problems:''' | ||
* | * Refractory Error | ||
| | *Arcus | ||
| | *[[Glaucoma]] | ||
|<nowiki> | *Band Keratopathy | ||
*[[Lenticonus]] | |||
| | *[[Weill-Marchesani syndrome|Spherophakia]] | ||
*[[Cataract|Cataracts]] | |||
|<nowiki>-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| + | |||
| - | |||
| | |||
* Early stage: unremarkable | |||
* Late stages: [[glomerulosclerosis]], [[interstitial fibrosis]], and interstitial [[foam cells]] (due to prolonged [[proteinuria]]). | |||
| | |||
* Within [[glomerular basement membrane]] ([[GBM]]): longitudinal splitting of the lamina densa | |||
| | |||
* Absence of staining of the alpha-3, alpha-4, and alpha-5 (IV) chains in the [[glomerular basement membrane]] | |||
* Minimal binding to a glomerulus in indirect [[immunofluorescence]] microscopy with [[Anti-glomerular basement membrane antibody|anti-glomerular basement membrane]] antibodies | |||
|- | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |||
! colspan="2" |[[Thin basement membrane disease|Thin Basement Membrane Disease]]<ref name="pmid12969134">{{cite journal |author=Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY |title=Thin basement membrane nephropathy |journal=Kidney Int. |volume=64 |issue=4 |pages=1169–78 |year=2003 |month=October |pmid=12969134 |doi=10.1046/j.1523-1755.2003.00234.x}}</ref><ref name="pmid17726307">{{cite journal |author=Hou P, Chen Y, Ding J, Li G, Zhang H |title=A novel mutation of COL4A3 presents a different contribution to Alport syndrome and thin basement membrane nephropathy |journal=Am. J. Nephrol. |volume=27 |issue=5 |pages=538–44 |year=2007 |pmid=17726307 |doi=10.1159/000107666 |url=http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=000107666}}</ref> | |||
| | |||
* Positive [[family history]] | |||
* Gross [[hematuria]] following [[upper respiratory tract infection]] | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
| - | |||
| + | |||
| -/+ | |||
| - | |||
|<nowiki>-/+</nowiki> | |||
| - | |||
| -/+ | |||
| - | |||
| - | |||
| - | |||
|Diffuse thinning of the [[Glomerular basement membrane|glomerular basement membranes]] (GBM) | |||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|- | |||
! colspan="2" |[[Nail-patella syndrome|Nail-Patella Syndrome]]<ref name="pmid28941488">{{cite journal |vauthors=Najafian B, Smith K, Lusco MA, Alpers CE, Fogo AB |title=AJKD Atlas of Renal Pathology: Nail-Patella Syndrome-Associated Nephropathy |journal=Am. J. Kidney Dis. |volume=70 |issue=4 |pages=e19–e20 |date=October 2017 |pmid=28941488 |doi=10.1053/j.ajkd.2017.08.001 |url=}}</ref><ref name="pmid1960197">{{cite journal |vauthors=Guidera KJ, Satterwhite Y, Ogden JA, Pugh L, Ganey T |title=Nail patella syndrome: a review of 44 orthopaedic patients |journal=J Pediatr Orthop |volume=11 |issue=6 |pages=737–42 |date=1991 |pmid=1960197 |doi= |url=}}</ref> | |||
| | |||
* Positive family history | |||
| | |||
* Poorly developed [[fingernails]], toe nails, and patellae (kneecaps). | |||
* [[Elbow]] deformities | |||
* Abnormally shaped [[pelvis]] bone ([[hip]] bone) | |||
* [[Knee]] may be small, deformed or absent | |||
|<nowiki>+</nowiki> | |<nowiki>+</nowiki> | ||
| + | |||
| - | |||
| - | |||
| - | |||
| - | |||
| - | |||
| - | |||
| - | |||
| | |||
* Mostly unremarkable changes | |||
* Secondary FSGS | |||
* Late stages: | |||
** Global glomerulosclerosis, | |||
** Tubulointerstitial fibrosis | |||
| | |||
* [[Glomerular basement membrane|Glomerular basement membranes (GBMs)]]: Focal or diffuse irregular thickening with electron-lucent areas (moth-eaten appearance) containing type III collagen bundles. | |||
* Similar collagen fibrils can be seen in mesangial matrix. | |||
* Podocytes: Segmental effacement of foot processes. | |||
| | |||
* [[Immunofluorescence]] studies are typically negative. | |||
* Nonspecific [[IgM]] and C3 deposition may be seen in sclerotic glomeruli. | |||
|- | |||
! rowspan="6" style="background:#4479BA; color: #FFFFFF;" align="center" + | Glomerular-Vascular Syndromes | |||
! colspan="2" |[[Hypertensive nephropathy|Hypertensive Nephrosclerosis]]<ref name="pmid24327566">{{cite journal |vauthors=Hughson MD, Puelles VG, Hoy WE, Douglas-Denton RN, Mott SA, Bertram JF |title=Hypertension, glomerular hypertrophy and nephrosclerosis: the effect of race |journal=Nephrol. Dial. Transplant. |volume=29 |issue=7 |pages=1399–409 |date=July 2014 |pmid=24327566 |pmc=4071048 |doi=10.1093/ndt/gft480 |url=}}</ref> | |||
|Chronic [[hypertension]] | |||
| | |||
* [[Hypertensive retinopathy|Hypertensive retinal]] changes. | |||
* High [[jugular venous pressure]] | |||
* [[Rales]] from [[pulmonary edema]] on auscultation | |||
* .Signs of [[left ventricular hypertrophy]] | |||
* [[Left ventricle|Left ventricular]] heave | |||
* Shifting of apex towards the left | |||
* [[S3]] and [[gallop rhythm]] | |||
* Loud S2 | |||
* [[Ascites]] | |||
* [[Paralysis]] from [[stroke]] secondary to [[hypertension]] | |||
* Inferior limb [[edema]] | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| - | |||
| +/- | |||
| - | |||
| colspan="3" | | |||
* Interstitial [[fibrosis]] and atrophy | |||
* Medial thickening and intimal fibrosis of medium-sized and larger vessels | |||
* Arteriolar thickening, and hyalinosis | |||
* Chronic stages: | |||
** Global sclerosis | |||
** Focal segmental [[sclerosis]] | |||
|- | |||
! colspan="2" |[[Cholesterol emboli syndrome|Cholesterol Emboli]]<ref name="pmid27012950">{{cite journal |vauthors=Lusco MA, Najafian B, Alpers CE, Fogo AB |title=AJKD Atlas of Renal Pathology: Cholesterol Emboli |journal=Am. J. Kidney Dis. |volume=67 |issue=4 |pages=e23–4 |date=April 2016 |pmid=27012950 |doi=10.1053/j.ajkd.2016.02.034 |url=}}</ref> | |||
| | | | ||
* | * [[Atherosclerotic]] [[cardiovascular disease]] | ||
* [[Anticoagulation therapy]] | |||
* [[Cardiopulmonary]] [[resuscitation]] | |||
* [[Hypertension]] | |||
* [[Aortic aneurysm]] | |||
* [[Hypercholesterolemia]] | |||
* Smoking history | |||
* Male sex | |||
* Age over 55 years | |||
* [[Vascular]] procedures | |||
* Invasive [[angiography]] | |||
* [[Aortic aneurysm]] rupture or surgery | |||
* [[Vascular]] surgery | |||
| | | | ||
* | * Depends on the organ involved | ||
|<nowiki>+ ( | |<nowiki>+/-</nowiki> | ||
|<nowiki>+/-</nowiki> | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| - | |||
| +/- | |||
| - | |||
| | |||
* Atheroemboli are seen in interlobular and arcuate arteries, as lance-shaped clefts, due to dissolution of [[cholesterol]] crystals | |||
* Acute lesions: | |||
** Atheroemboli are surrounded by red blood cells, fibrin, and leukocytes, with multinucleated giant cell reactions | |||
* Chronic lesions: | |||
** Cholesterol clefts are surrounded by intimal fibrosis | |||
** Vessel recanalization of chronic lesions can occur. | |||
* Global and segmental sclerosis of glomeruli may be present. | |||
| | |||
* Extensive foot process effacement can be seen | |||
| | |||
* Not specific changes | |||
|- | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |History | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Systemic symptoms | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hemeturia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Proteinuria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hypertension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Pitting edema | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Oliguria | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephrotic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Nephritic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Hyperlipidemia and hypercholesterolemia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Auto-antibodies, | |||
Complements | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Light microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Electron microscope | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Immunoflourescence pattern | |||
|- | |||
! colspan="2" |[[Sickle-cell disease|Sickle Cell Disease]]<ref name="pmid12028473">{{cite journal |vauthors=Wesson DE |title=The initiation and progression of sickle cell nephropathy |journal=Kidney Int. |volume=61 |issue=6 |pages=2277–86 |date=June 2002 |pmid=12028473 |doi=10.1046/j.1523-1755.2002.00363.x |url=}}</ref> | |||
| | |||
* Positive family history | |||
| | |||
* [[Pain and nociception|Pain]] and/or [[bone pain]] | |||
* [[Dactylitis]] | |||
* [[Blurry vision]] | |||
* [[Priapism|Persistent and painful erection]] | |||
* [[Numbness]] | |||
* [[Tingling]] | |||
* Motor skill loss | |||
* [[Aphasia|Speech deficits]] | |||
* [[Gait disturbance]] | |||
* Leg [[ulceration]] | |||
* [[Jaundice]] | |||
|<nowiki>+/-</nowiki> | |||
|<nowiki>+/-</nowiki> | |||
| +/- | |||
| - | |||
| - | |||
| - | |||
| - | |||
| - | |||
| - | |||
| colspan="3" | | |||
* [[Glomerulus|Glomerular]] hypertrophy | |||
* [[Hemosiderin]] deposits | |||
* Focal areas of hemorrhage or necrosis | |||
* Chronic stage: interstitial inflammation, edema, fibrosis, tubular atrophy, and [[papillary]] infarcts | |||
* Glomerular enlargement and focal segmental glomerulosclerosis ([[Focal segmental glomerulosclerosis|FSGS]]) | |||
|- | |||
! colspan="2" |[[Thrombotic microangiopathies|Thrombotic Microangiopathies]]<ref name="pmid27884283">{{cite journal |vauthors=Lusco MA, Fogo AB, Najafian B, Alpers CE |title=AJKD Atlas of Renal Pathology: Thrombotic Microangiopathy |journal=Am. J. Kidney Dis. |volume=68 |issue=6 |pages=e33–e34 |date=December 2016 |pmid=27884283 |doi=10.1053/j.ajkd.2016.10.006 |url=}}</ref> | |||
| colspan="2" |'''''Click for more information on [[Thrombotic microangiopathies|Thrombotic Microangiopathies]].''''' | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
| +/- | |||
| +/- | |||
| +/- | |||
| - | |||
| - | |||
| - | |||
| | |||
* Acute stage: | |||
** Inravasculr fibrin thrombi | |||
* Chronic stage: | |||
** Endocapillary hypercellularity. | |||
** Intimal proliferation of [[Arteriole|arterioles]] | |||
| | |||
* Swollen glomerular endothelial cells with loss of [[Fenestration|fenestrations]] | |||
* Chronic stage: interposed cells with new [[GBM]] matrix material deposition. | |||
| | |||
* [[Thrombus|Thrombi]] stain positive for [[fibrinogen]] | |||
|- | |||
! colspan="2" |[[Antiphospholipid syndrome|Antiphospholipid Antibody Syndrome]] <ref name="pmid24684307">{{cite journal| author=Jayakody Arachchillage D, Greaves M| title=The chequered history of the antiphospholipid syndrome. | journal=Br J Haematol | year= 2014 | volume= 165 | issue= 5 | pages= 609-17 | pmid=24684307 | doi=10.1111/bjh.12848 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24684307 }}</ref><ref name="pmid246843072">{{cite journal| author=Jayakody Arachchillage D, Greaves M| title=The chequered history of the antiphospholipid syndrome. | journal=Br J Haematol | year= 2014 | volume= 165 | issue= 5 | pages= 609-17 | pmid=24684307 | doi=10.1111/bjh.12848 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24684307 }}</ref><ref name="pmid18714484">{{cite journal| author=Popa A, Voinea L, Pop M, Stana D, Dascalu AM, Alexandrescu C et al.| title=[Primary antiphospholipid syndrome]. | journal=Oftalmologia | year= 2008 | volume= 52 | issue= 1 | pages= 13-7 | pmid=18714484 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18714484 }}</ref> | |||
| | |||
* [[Thrombosis]] | |||
* [[Miscarriage]] | |||
* History of [[nephropathy]] | |||
* History of [[Hematology|hematologic]] abnormalities | |||
* Nonthrombotic neurologic symptoms, such as [[migraine]] headaches | |||
* [[Pulmonary hypertension]] | |||
| | |||
*[[Fatigue]] | |||
*[[Fever]] | |||
*[[Weight loss]] | |||
*[[Venous thrombosis]] | |||
*[[Arterial thrombosis]] | |||
*[[Thrombocytopenia]] | |||
*Recurrent fetal loss | |||
| + | |||
|<nowiki>+/-</nowiki> | |||
| + | |||
| +/- | |||
| +/- | |||
| +/- | |||
| - | |||
| - | |||
| - | |||
| | |||
* Acute stage: | |||
** Inravasculr fibrin [[Thrombus|thrombi]] | |||
* Chronic stage: | |||
** [[Endocapillary proliferative glomerulonephritis|Endocapillary]] hypercellularity. | |||
** Intimal proliferation of [[Arteriole|arterioles]] | |||
| | |||
* Swollen glomerular endothelial cells with loss of fenestrations | |||
* Chronic stage: interposed cells with new GBM matrix material deposition. | |||
| | |||
* [[Thrombus|Thrombi]] stain positive for [[fibrinogen]] | |||
|} | |} | ||
<small> | |||
'''Some infectious diseases such as [[HIV]], [[Hepatitis B virus|HBV]], [[Hepatitis C|HCV]], [[syphilis]], [[leprosy]], [[malaria]], and [[schistosomiasis]] may cause glomerular diseases.''' | |||
==Images== | |||
[http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
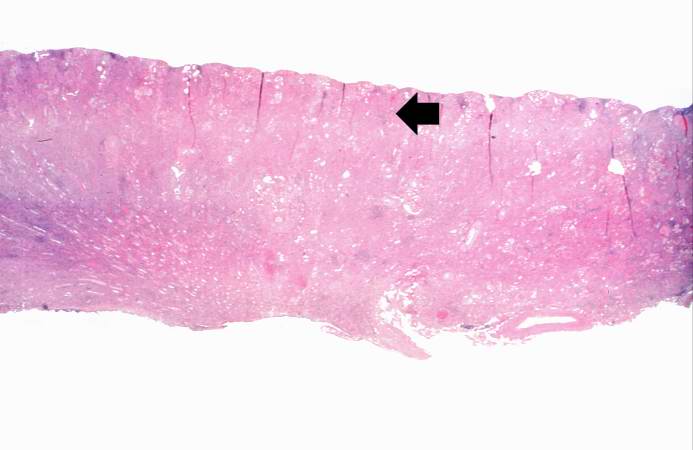
Image:Glomerulonephritis case 1.jpg|This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow). | |||
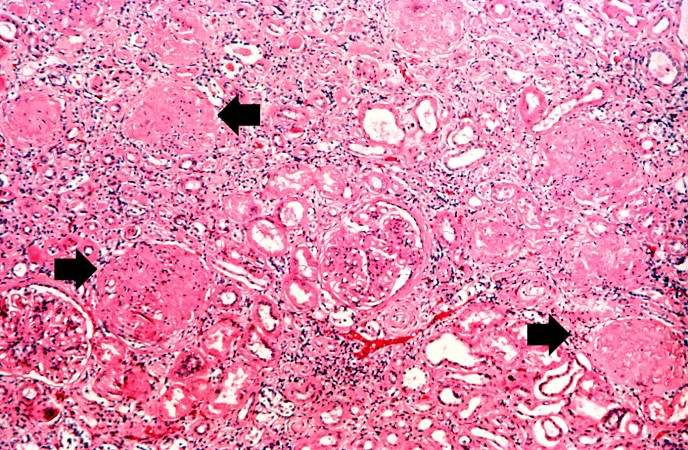
Image:Glomerulonephritis case 2.jpg|This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes. | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
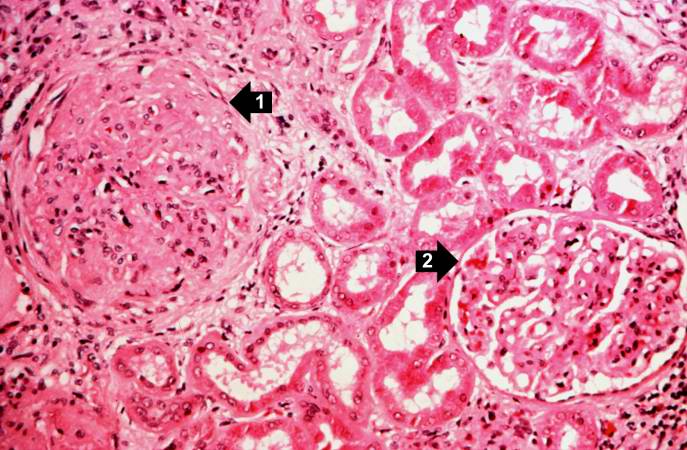
Image:Glomerulonephritis case 3.jpg|This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2). | |||
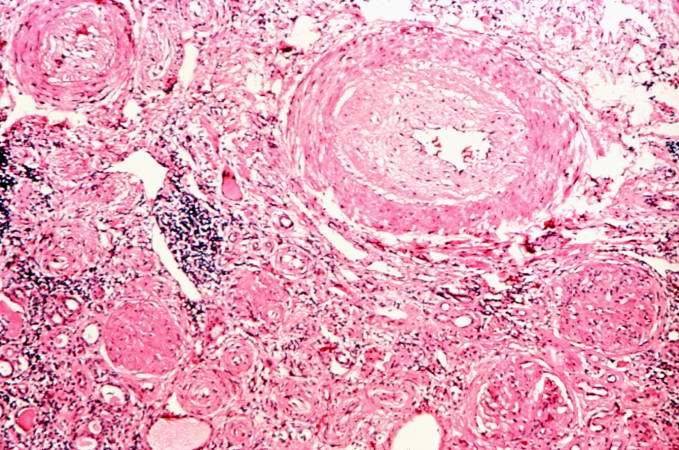
Image:Glomerulonephritis case 4.jpg|This is a photomicrograph of interstitial and vascular lesions in end stage renal disease. | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
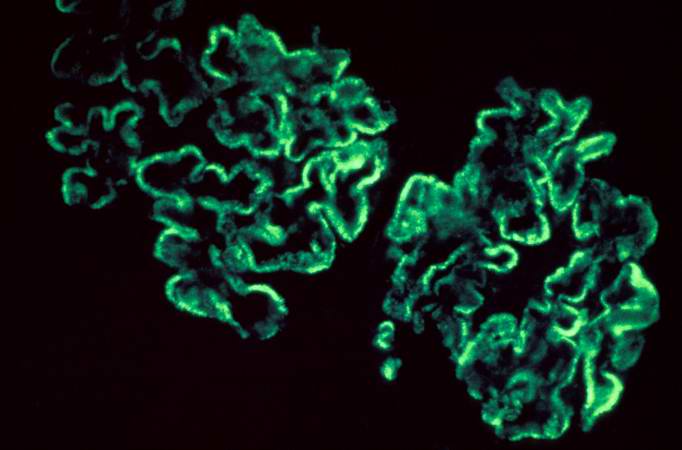
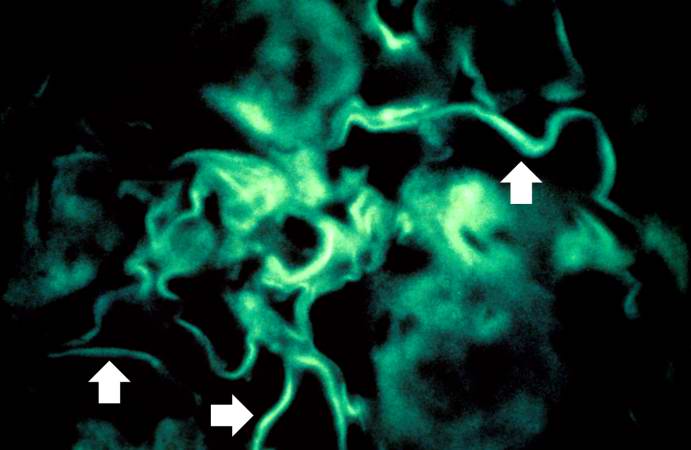
Image:Glomerulonephritis case 5.jpg|This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG. | |||
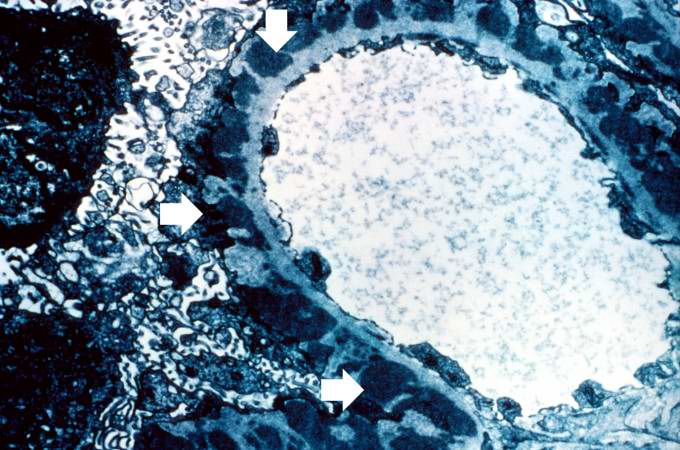
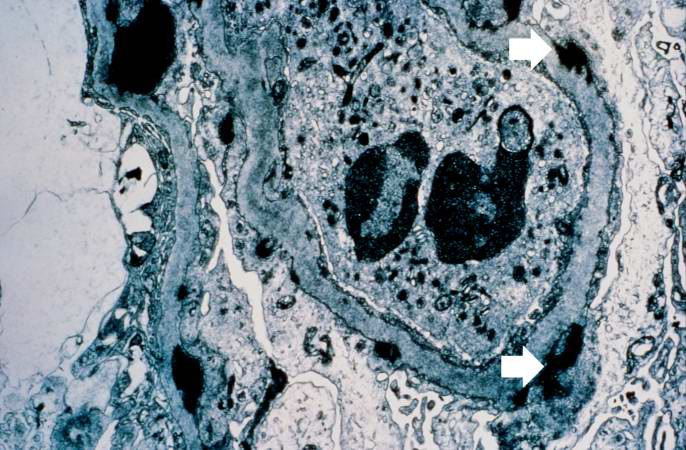
Image:Glomerulonephritis case 6.jpg|This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image. | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
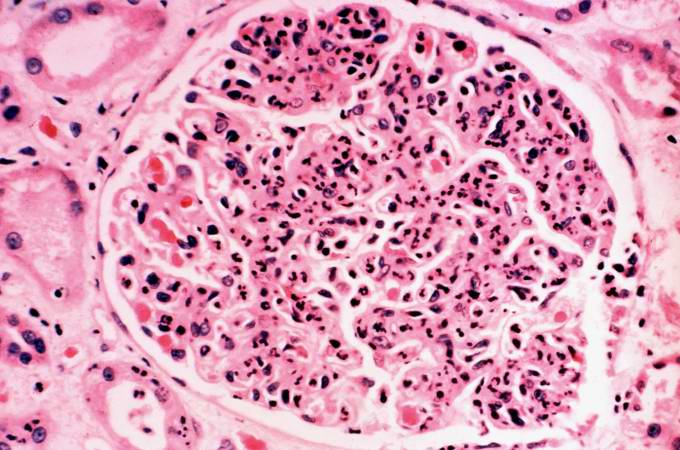
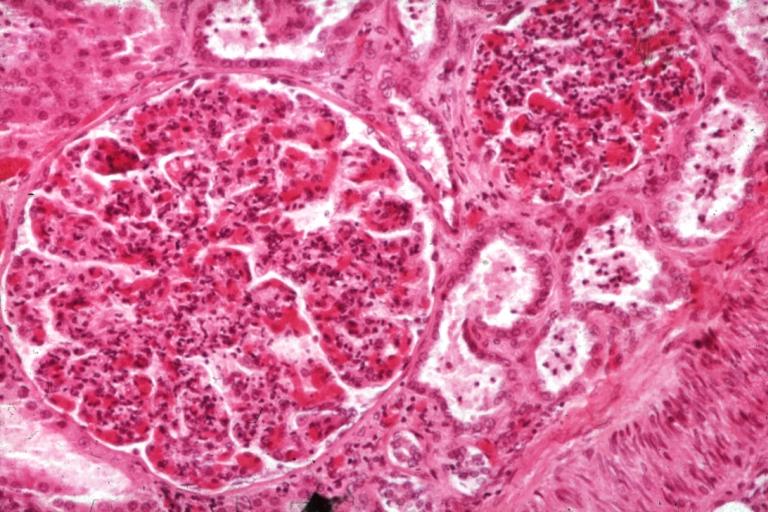
Image:Glomerulonephritis case 7.jpg|This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus. | |||
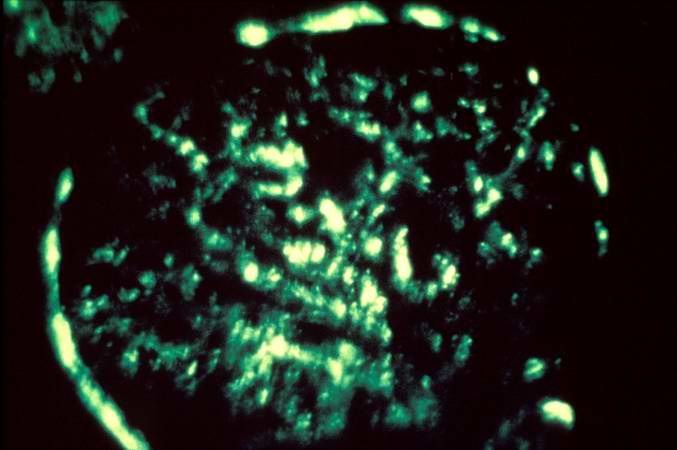
Image:Glomerulonephritis case 8.jpg|This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern. | |||
</gallery> | |||
</div> | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
Image:Glomerulonephritis case 9.jpg|This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen. | |||
Image:Glomerulonephritis case 10.jpg|For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome. | |||
</gallery> | |||
</div> | |||
===Microscopic Pathology=== | |||
[http://www.peir.net Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | |||
<div align="left"> | |||
<gallery heights="175" widths="175"> | |||
image:Acute GN 1.jpg|Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils | |||
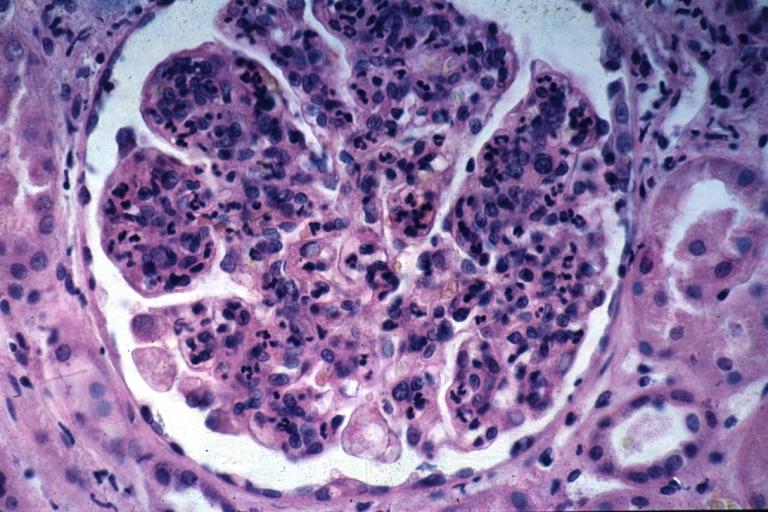
image:Acute GN 2.jpg|Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. | |||
</gallery> | |||
</div> | |||
<br> | |||
===Glomerulonephritis Videos=== | |||
====Rapidly progressive glomerulonephritis==== | |||
{{#ev:youtube|CqSyj4cVZPE}} | |||
====Chronic glomerulonephritis==== | |||
{{#ev:youtube|eA1vYarRAWo}} | |||
===Images:=== | |||
*[http://www.pathologyatlas.ro/Crescentic%20Glomerulonephritis.html Crescentic GN] | |||
*[http://www.pathologyatlas.ro/Chronic%20Glomerulonephritis1.html Chronic GN] | |||
==References== | ==References== | ||
| Line 441: | Line 1,143: | ||
{{Nephrology}} | {{Nephrology}} | ||
{{WH}} | |||
{{WS}} | |||
<references /> | |||
[[Category:Disease]] | [[Category:Disease]] | ||
| Line 446: | Line 1,151: | ||
[[Category:Inflammations]] | [[Category:Inflammations]] | ||
[[Category:Kidney diseases]] | [[Category:Kidney diseases]] | ||
Latest revision as of 21:53, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2], Syed Hassan A. Kazmi BSc, MD [3]
This page contains general information about Glomerular disease.
For more information on specific types, please visit the pages on:
- Nephritic syndrome
- Nephrotic syndrome
- Fabry's disease
- Post-streptococcal glomerulonephritis
- Lupus nephritis
- Antiglomerular basement membrane disease
- (Goodpasture's syndrome)
- Cryoglobulinemia
- Henoch-Schönlein purpura
- Amyloidosis
- Pulmonary-renal syndromes (vasculitis)
- Thin basement membrane disease
- Alport's Syndrome
- anti-GBM Disease
- Hypertensive nephrosclerosis
- Subacute bacterial endocarditis
Overview
Glomerular disease is a condition that affects the glomerulus. It consists of different diseases with different clinical courses and treatment options. Glomerular disease can be isolated hematuria, isolated proteinuria; acute or chronic glomerulonephritis, and nephrotic or nephritic features of glomerulonephritis. The end stage of all of these diseases will be glomerulosclerosis which is characterized by fibrosis of the glomerulus, and end-stage renal disease.
Classification
Glomerular dieseases can be classified into several clinical and pathological syndromes as below:
| Syndrome | Disease |
|---|---|
| Acute nephritic syndromes |
|
| Nephrotic syndrome | |
| Glomerular Deposition Diseases |
|
| Pulmonary-Renal Syndromes: | |
| Basement Membrane Syndromes | |
| Glomerular-Vascular Syndromes |
|
| Infectious Disease–Associated Syndromes |
Also, glomerular diseases can be classified based on their clinical and urinary pattern in to below types:
Mild nephritc:
This category include mild nephritic sediment that is associated with less than half involvement of glomeruli.
Severe nephritic:
More severe clinical features such as edema, heavy proteinuria, hypertension, and/or renal failure may occur.
Nephrotic:
This syndrome is associated with heavy proteinuria and lipiduria.
Glomerular diseases also may classified by their presentation as below:
Glomerular hematuria:
1- Isolated hematuria
2- Glomerulonephritis (nephritic syndrome)
Proteinuria:
1-Isolated non-nephrotic proteinuria
Rapidly progressive glomerulonephritis
Glomerulonephritis
Glomerulonephritis which is inflammation of the glomeruli can be classified based on pathogenic type into three subtypes:
- Immune complex glomerulonephritis: Granular deposit of immune complex.
- Infection mediated types
- Autoimmune types, eg SLE
- MPGN
- IgA nephropathy (Berger nephropathy)
- Membranous nephropathy
- Anti-GBM disease: Linear deposit
- Goodpasture syndrome (renal and lung involvement)
- Renal involvement alone
- Lung involvement alone
- ANCA associated, small vessels vasculitis: Few or no deposit
Glomerulonephritis (nephritic syndrome) also may be classified based on disease course into acute or chronic nephritic syndrome; primary vs secondary causes; or systemic vs renal limited disease. For more information about nephritic syndrome classifications click here.
Differential Diagnosis
The various types of glomerular diseases should be differentiated from each other based on associations, presence of pitting edema, hematuria, hypertension, hemoptysis, oliguria, peri-orbital edema, hyperlipidemia, type of antibodies, light and electron microscopic features. The following table differentiates between various types of glumerular diseases:
| Glomerular diseases | Disease | History and Symtoms | Laboratory Findings | Pathology | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | |||
| Acute Nephritic Syndromes | Poststreptococcal Glomerulonephritis[1][2][3] |
|
+/- | + | +/- | +/- | +/- | +/- | +/- | +/- |
|
|
| |||
| Renal disease due to Subacute Bacterial Endocarditis, or cardiac shunt (Atrioventricular)[4][5] |
|
+/- | + | +/- | +/- | +/- | +/- | +/- | +/- |
|
|
|
| |||
| Lupus Nephritis[6] |
|
|
+/- | + | +/- | +/- | +/- | +/- | +/- | +/- |
|
|
|
| ||
| Antiglomerular Basement Membrane Disease (Goodpasture's syndrome)[7][8] |
|
|
+ | + | + | + | + | + | - | - | Diffuse thickening of the glomerular basement membrane with absence of sub-epithelial and sub-endothelial deposits |
| ||||
| IgA Nephropathy[9][10] |
|
|
+ | +/- | + | +/- | + | - | + | - |
|
|
|
| ||
| Disease | History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | ||
| ANCA Small-Vessel Vasculitis[11][12] | Granulomatosis with Polyangiitis (Wegener's)[13][14][15] |
|
|
+ | + | + | +/- | + | - | + | - |
|
|
| ||
| Microscopic Polyangiitis[16] | +/- |
|
+ | + | + | + | + | + | - |
| ||||||
| Churg-Strauss Syndrome[17] | +/- | + | + | + | + | + | + | - |
| |||||||
| Membranoproliferative Glomerulonephritis[18][19] |
|
+ | + | + | +/- | + | + | - | - | - |
|
| ||||
| Henoch-Schönlein purpura [20] |
|
|
+ | + | + | +/- | + | + | - | - | - |
|
|
| ||
| Disease | History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | ||
| Cryoglobulinemia[21] | Patients having cryoglobulinemia may have positive history of:
|
Pulmonary symptoms:
Cutaneous symptoms: Gastrointestinal symptoms:
General symptoms:
|
+/- | + | +/- | + | +/- | +/- | +/- | +/- | +/- |
|
| |||
| Nephrotic Syndrome | Minimal Change Disease[22][23] |
|
- | + | - | + | +/- | + | - | + |
|
|
- | |||
| Focal Segmental Glomerulosclerosis[24][25][26] |
|
- | + | - | + | +/- | + | - | + |
|
|
- | ||||
| Membranous Glomerulonephritis[27][28] |
|
- | + | - | + | +/- | + | - | + | Immune complex deposition |
|
Immune complex GN, granular deposite | ||||
| Diabetic Nephropathy[29][30][31][32][33][34][35][36][37][38] | For more information on diabetes click here. | - | + | - | + | +/- | + | - | + |
|
|
- | ||||
| Disease | History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | ||
| Glomerular Deposition Diseases | Light Chain Deposition Disease[39] |
|
- | - | + | - | + | +/- | + | - | + | - |
|
|
| |
| Renal Amyloidosis[40][41][42][43] |
|
- | + | - | + | +/- | + | - | + | - |
|
|
| |||
| Fibrillary-Immunotactoid Glomerulopathy[44] | - | +/- | + | +/- | +/- | +/- | + | +/- | +/- | - |
|
|
| |||
| Fabry's Disease[45][46][47] |
|
|
- | + | - | + | +/- | + | - | + | - |
|
|
- | ||
| Basement Membrane Syndrome | Alport's Syndrome[48][49][50][51][52][53] |
|
Auditary:
Occular problems:
|
- | + | - | + | +/- | + | - | + | - |
|
|
| |
| Disease | History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | ||
| Thin Basement Membrane Disease[54][55] |
|
- | - | + | -/+ | - | -/+ | - | -/+ | - | - | - | Diffuse thinning of the glomerular basement membranes (GBM) | - | ||
| Nail-Patella Syndrome[56][57] |
|
|
+ | + | - | - | - | - | - | - | - |
|
|
| ||
| Glomerular-Vascular Syndromes | Hypertensive Nephrosclerosis[58] | Chronic hypertension |
|
+/- | +/- | + | +/- | +/- | +/- | - | +/- | - | ||||
| Cholesterol Emboli[59] |
|
|
+/- | +/- | + | +/- | +/- | +/- | - | +/- | - |
|
|
| ||
| Disease | History | Systemic symptoms | Hemeturia | Proteinuria | Hypertension | Pitting edema | Oliguria | Nephrotic features | Nephritic features | Hyperlipidemia and hypercholesterolemia | Auto-antibodies,
Complements |
Light microscope | Electron microscope | Immunoflourescence pattern | ||
| Sickle Cell Disease[60] |
|
|
+/- | +/- | +/- | - | - | - | - | - | - |
| ||||
| Thrombotic Microangiopathies[61] | Click for more information on Thrombotic Microangiopathies. | + | +/- | + | +/- | +/- | +/- | - | - | - |
|
|
| |||
| Antiphospholipid Antibody Syndrome [62][63][64] |
|
|
+ | +/- | + | +/- | +/- | +/- | - | - | - |
|
|
| ||
Some infectious diseases such as HIV, HBV, HCV, syphilis, leprosy, malaria, and schistosomiasis may cause glomerular diseases.
Images
-
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Microscopic Pathology
-
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Images:
References
- ↑ GERMUTH FG (1953). "A comparative histologic and immunologic study in rabbits of induced hypersensitivity of the serum sickness type". J Exp Med. 97 (2): 257–82. PMC 2136196. PMID 13022878.
- ↑ Germuth FG, Senterfit LB, Dreesman GR (1972). "Immune complex disease. V. The nature of the circulating complexes associated with glomerular alterations in the chronic BSA-rabbit system". Johns Hopkins Med J. 130 (6): 344–57. PMID 5031005.
- ↑ Radhakrishnan J, Cattran DC (2012). "The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines--application to the individual patient". Kidney Int. 82 (8): 840–56. doi:10.1038/ki.2012.280. PMID 22895519.
- ↑ Neugarten J, Baldwin DS (August 1984). "Glomerulonephritis in bacterial endocarditis". Am. J. Med. 77 (2): 297–304. PMID 6380288.
- ↑ Arze RS, Rashid H, Morley R, Ward MK, Kerr DN (January 1983). "Shunt nephritis: report of two cases and review of the literature". Clin. Nephrol. 19 (1): 48–53. PMID 6831779.
- ↑ Weening JJ, D'Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, Nagata M (February 2004). "The classification of glomerulonephritis in systemic lupus erythematosus revisited". Kidney Int. 65 (2): 521–30. doi:10.1111/j.1523-1755.2004.00443.x. PMID 14717922.
- ↑ Bolton WK (November 1996). "Goodpasture's syndrome". Kidney Int. 50 (5): 1753–66. PMID 8914046.
- ↑ Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P (February 1975). "Goodpasture's syndrome: normal renal diagnostic findings". Ann. Intern. Med. 82 (2): 215–8. PMID 1090223.
- ↑ Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA (October 2011). "The pathophysiology of IgA nephropathy". J. Am. Soc. Nephrol. 22 (10): 1795–803. doi:10.1681/ASN.2011050464. PMC 3892742. PMID 21949093.
- ↑ Wyatt RJ, Julian BA (June 2013). "IgA nephropathy". N. Engl. J. Med. 368 (25): 2402–14. doi:10.1056/NEJMra1206793. PMID 23782179.
- ↑ Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC (January 1996). "Vasculitis and rapidly progressive glomerulonephritis in the elderly". Postgrad Med J. 72 (843): 41–4. PMC 2398323. PMID 8746284.
- ↑ Jennette JC (March 2003). "Rapidly progressive crescentic glomerulonephritis". Kidney Int. 63 (3): 1164–77. doi:10.1046/j.1523-1755.2003.00843.x. PMID 12631105.
- ↑ Renaudineau Y, Le Meur Y (October 2008). "Renal involvement in Wegener's granulomatosis". Clin Rev Allergy Immunol. 35 (1–2): 22–9. doi:10.1007/s12016-007-8066-6. PMID 18172777.
- ↑ Weiss MA, Crissman JD (October 1984). "Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis". Hum. Pathol. 15 (10): 943–56. PMID 6384024.
- ↑ Pagnoux C (March 2008). "[Wegener's granulomatosis and microscopic polyangiitis]". Rev Prat (in French). 58 (5): 522–32. PMID 18524109.
- ↑ Chung SA, Seo P (August 2010). "Microscopic polyangiitis". Rheum. Dis. Clin. North Am. 36 (3): 545–58. doi:10.1016/j.rdc.2010.04.003. PMC 2917831. PMID 20688249.
- ↑ Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C (May 2006). "Renal involvement in Churg-Strauss syndrome". Am. J. Kidney Dis. 47 (5): 770–9. doi:10.1053/j.ajkd.2006.01.026. PMID 16632015.
- ↑ Alchi B, Jayne D (August 2010). "Membranoproliferative glomerulonephritis". Pediatr. Nephrol. 25 (8): 1409–18. doi:10.1007/s00467-009-1322-7. PMC 2887509. PMID 19908070.
- ↑ Davis AE, Schneeberger EE, Grupe WE, McCluskey RT (May 1978). "Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children". Clin. Nephrol. 9 (5): 184–93. PMID 657595.
- ↑ Jennette JC, Falk RJ (July 1994). "The pathology of vasculitis involving the kidney". Am. J. Kidney Dis. 24 (1): 130–41. PMID 8023818.
- ↑ Fogo AB, Lusco MA, Najafian B, Alpers CE (February 2016). "AJKD Atlas of Renal Pathology: Cryoglobulinemic Glomerulonephritis". Am. J. Kidney Dis. 67 (2): e5–7. doi:10.1053/j.ajkd.2015.12.007. PMID 26802335.
- ↑ Saha TC, Singh H (November 2006). "Minimal change disease: a review". South. Med. J. 99 (11): 1264–70. doi:10.1097/01.smj.0000243183.87381.c2. PMID 17195422.
- ↑ Saleem MA, Kobayashi Y (2016). "Cell biology and genetics of minimal change disease". F1000Res. 5. doi:10.12688/f1000research.7300.1. PMC 4821284. PMID 27092244.
- ↑ Rosenberg AZ, Kopp JB (March 2017). "Focal Segmental Glomerulosclerosis". Clin J Am Soc Nephrol. 12 (3): 502–517. doi:10.2215/CJN.05960616. PMC 5338705. PMID 28242845.
- ↑ Jefferson JA, Shankland SJ (September 2014). "The pathogenesis of focal segmental glomerulosclerosis". Adv Chronic Kidney Dis. 21 (5): 408–16. doi:10.1053/j.ackd.2014.05.009. PMC 4149756. PMID 25168829.
- ↑ Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT (October 1986). "Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens". Arch. Pathol. Lab. Med. 110 (10): 902–5. PMID 2429634.
- ↑ Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ (February 2015). "Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment". J. Formos. Med. Assoc. 114 (2): 102–11. doi:10.1016/j.jfma.2014.11.002. PMID 25558821.
- ↑ Wasserstein AG (April 1997). "Membranous glomerulonephritis". J. Am. Soc. Nephrol. 8 (4): 664–74. PMID 10495797.
- ↑ Drummond K, Mauer M, International Diabetic Nephropathy Study Group (2002). "The early natural history of nephropathy in type 1 diabetes: II. Early renal structural changes in type 1 diabetes". Diabetes. 51 (5): 1580–7. PMID 11978659.
- ↑ Hørlyck A, Gundersen HJ, Osterby R (1986). "The cortical distribution pattern of diabetic glomerulopathy". Diabetologia. 29 (3): 146–50. PMID 3699305.
- ↑ Alpers CE, Hudkins KL (2011). "Mouse models of diabetic nephropathy". Curr Opin Nephrol Hypertens. 20 (3): 278–84. doi:10.1097/MNH.0b013e3283451901. PMC 3658822. PMID 21422926.
- ↑ Kimmelstiel P, Wilson C (1936). "Intercapillary Lesions in the Glomeruli of the Kidney". Am J Pathol. 12 (1): 83–98.7. PMC 1911022. PMID 19970254.
- ↑ Alpers CE, Biava CG (1989). "Idiopathic lobular glomerulonephritis (nodular mesangial sclerosis): a distinct diagnostic entity". Clin Nephrol. 32 (2): 68–74. PMID 2766585.
- ↑ Toyoda M, Najafian B, Kim Y, Caramori ML, Mauer M (2007). "Podocyte detachment and reduced glomerular capillary endothelial fenestration in human type 1 diabetic nephropathy". Diabetes. 56 (8): 2155–60. doi:10.2337/db07-0019. PMID 17536064.
- ↑ Najafian B, Crosson JT, Kim Y, Mauer M (2006). "Glomerulotubular junction abnormalities are associated with proteinuria in type 1 diabetes". J Am Soc Nephrol. 17 (4 Suppl 2): S53–60. doi:10.1681/ASN.2005121342. PMID 16565248.
- ↑ Najafian B, Kim Y, Crosson JT, Mauer M (2003). "Atubular glomeruli and glomerulotubular junction abnormalities in diabetic nephropathy". J Am Soc Nephrol. 14 (4): 908–17. PMID 12660325.
- ↑ Najafian B, Alpers CE, Fogo AB (2011). "Pathology of human diabetic nephropathy". Contrib Nephrol. 170: 36–47. doi:10.1159/000324942. PMID 21659756.
- ↑ Najafian B, Alpers CE, Fogo AB (2011). "Pathology of human diabetic nephropathy". Contrib Nephrol. 170: 36–47. doi:10.1159/000324942. PMID 21659756.
- ↑ Hutchison CA, Cockwell P, Stringer S, Bradwell A, Cook M, Gertz MA, Dispenzieri A, Winters JL, Kumar S, Rajkumar SV, Kyle RA, Leung N (June 2011). "Early reduction of serum-free light chains associates with renal recovery in myeloma kidney". J. Am. Soc. Nephrol. 22 (6): 1129–36. doi:10.1681/ASN.2010080857. PMC 3103732. PMID 21511832.
- ↑ Baker KR, Rice L (2012). "The amyloidoses: clinical features, diagnosis and treatment". Methodist Debakey Cardiovasc J. 8 (3): 3–7. PMC 3487569. PMID 23227278.
- ↑ Gillmore JD, Hawkins PN (October 2013). "Pathophysiology and treatment of systemic amyloidosis". Nat Rev Nephrol. 9 (10): 574–86. doi:10.1038/nrneph.2013.171. PMID 23979488.
- ↑ Jerzykowska S, Cymerys M, Gil LA, Balcerzak A, Pupek-Musialik D, Komarnicki MA (2014). "Primary systemic amyloidosis as a real diagnostic challenge - case study". Cent Eur J Immunol. 39 (1): 61–6. doi:10.5114/ceji.2014.42126. PMC 4439975. PMID 26155101.
- ↑ Pepys MB (2006). "Amyloidosis". Annu. Rev. Med. 57: 223–41. doi:10.1146/annurev.med.57.121304.131243. PMID 16409147.
- ↑ Korbet SM, Schwartz MM, Lewis EJ (March 1991). "Immunotactoid glomerulopathy". Am. J. Kidney Dis. 17 (3): 247–57. PMID 1996564.
- ↑ Alroy J, Sabnis S, Kopp JB (June 2002). "Renal pathology in Fabry disease". J. Am. Soc. Nephrol. 13 Suppl 2: S134–8. PMID 12068025.
- ↑ Meikle PJ, Hopwood JJ, Clague AE, Carey WF (1999). "Prevalence of lysosomal storage disorders". JAMA : the Journal of the American Medical Association. 281 (3): 249–54. PMID 9918480. Unknown parameter
|month=ignored (help) - ↑ Branton MH, Schiffmann R, Sabnis SG; et al. (2002). "Natural history of Fabry renal disease: influence of alpha-galactosidase A activity and genetic mutations on clinical course". Medicine. 81 (2): 122–38. PMID 11889412. Unknown parameter
|month=ignored (help) - ↑ McCarthy PA, Maino DM (2000). "Alport syndrome: a review". Clin Eye Vis Care. 12 (3–4): 139–150. PMID 11137428.
- ↑ Chugh KS, Sakhuja V, Agarwal A, Jha V, Joshi K, Datta BN; et al. (1993). "Hereditary nephritis (Alport's syndrome)--clinical profile and inheritance in 28 kindreds". Nephrol Dial Transplant. 8 (8): 690–5. PMID 8414153.
- ↑ Chugh KS, Sakhuja V, Agarwal A, Jha V, Joshi K, Datta BN; et al. (1993). "Hereditary nephritis (Alport's syndrome)--clinical profile and inheritance in 28 kindreds". Nephrol Dial Transplant. 8 (8): 690–5. PMID 8414153.
- ↑ McCarthy PA, Maino DM (2000). "Alport syndrome: a review". Clin Eye Vis Care. 12 (3–4): 139–150. PMID 11137428.
- ↑ Amari F, Segawa K, Ando F (1994). "Lens coloboma and Alport-like glomerulonephritis". Eur J Ophthalmol. 4 (3): 181–3. PMID 7819734.
- ↑ Govan JA (1983). "Ocular manifestations of Alport's syndrome: a hereditary disorder of basement membranes?". Br J Ophthalmol. 67 (8): 493–503. PMC 1040106. PMID 6871140.
- ↑ Savige J, Rana K, Tonna S, Buzza M, Dagher H, Wang YY (2003). "Thin basement membrane nephropathy". Kidney Int. 64 (4): 1169–78. doi:10.1046/j.1523-1755.2003.00234.x. PMID 12969134. Unknown parameter
|month=ignored (help) - ↑ Hou P, Chen Y, Ding J, Li G, Zhang H (2007). "A novel mutation of COL4A3 presents a different contribution to Alport syndrome and thin basement membrane nephropathy". Am. J. Nephrol. 27 (5): 538–44. doi:10.1159/000107666. PMID 17726307.
- ↑ Najafian B, Smith K, Lusco MA, Alpers CE, Fogo AB (October 2017). "AJKD Atlas of Renal Pathology: Nail-Patella Syndrome-Associated Nephropathy". Am. J. Kidney Dis. 70 (4): e19–e20. doi:10.1053/j.ajkd.2017.08.001. PMID 28941488.
- ↑ Guidera KJ, Satterwhite Y, Ogden JA, Pugh L, Ganey T (1991). "Nail patella syndrome: a review of 44 orthopaedic patients". J Pediatr Orthop. 11 (6): 737–42. PMID 1960197.
- ↑ Hughson MD, Puelles VG, Hoy WE, Douglas-Denton RN, Mott SA, Bertram JF (July 2014). "Hypertension, glomerular hypertrophy and nephrosclerosis: the effect of race". Nephrol. Dial. Transplant. 29 (7): 1399–409. doi:10.1093/ndt/gft480. PMC 4071048. PMID 24327566.
- ↑ Lusco MA, Najafian B, Alpers CE, Fogo AB (April 2016). "AJKD Atlas of Renal Pathology: Cholesterol Emboli". Am. J. Kidney Dis. 67 (4): e23–4. doi:10.1053/j.ajkd.2016.02.034. PMID 27012950.
- ↑ Wesson DE (June 2002). "The initiation and progression of sickle cell nephropathy". Kidney Int. 61 (6): 2277–86. doi:10.1046/j.1523-1755.2002.00363.x. PMID 12028473.
- ↑ Lusco MA, Fogo AB, Najafian B, Alpers CE (December 2016). "AJKD Atlas of Renal Pathology: Thrombotic Microangiopathy". Am. J. Kidney Dis. 68 (6): e33–e34. doi:10.1053/j.ajkd.2016.10.006. PMID 27884283.
- ↑ Jayakody Arachchillage D, Greaves M (2014). "The chequered history of the antiphospholipid syndrome". Br J Haematol. 165 (5): 609–17. doi:10.1111/bjh.12848. PMID 24684307.
- ↑ Jayakody Arachchillage D, Greaves M (2014). "The chequered history of the antiphospholipid syndrome". Br J Haematol. 165 (5): 609–17. doi:10.1111/bjh.12848. PMID 24684307.
- ↑ Popa A, Voinea L, Pop M, Stana D, Dascalu AM, Alexandrescu C; et al. (2008). "[Primary antiphospholipid syndrome]". Oftalmologia. 52 (1): 13–7. PMID 18714484.