Adrenal carcinoma: Difference between revisions
Sara Mohsin (talk | contribs) |
Sara Mohsin (talk | contribs) |
||
| Line 233: | Line 233: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Weiss [[criteria]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Weiss [[criteria]]''' | ||
| | | | ||
[[Adrenocortical carcinoma]] can be [[Diagnose|diagnosed]] by the [[Presenting symptom|presence]] of '''at least 3 of the 9''' Weiss [[criteria]]: | |||
#'''High nuclear grade''' (III or IV) | #'''High [[nuclear]] [[Grading (tumors)|grade]]''' (III or IV) | ||
#'''High mitotic rate''' i.e. presence of >5 mitotic figures/50 high-power fields, definition suffers from | #'''High [[Mitotic index|mitotic rate]]''' i.e. [[Presenting symptom|presence]] of >5 [[mitotic]] figures/50 high-[[Power (communication)|power]] [[Field of view|fields]], definition suffers from [[HPFH|HPF]]<nowiki/>itis (counting 10 [[random]] [[Field of view|fields]] in [[area]] of greatest [[number]] of [[Mitotic spindle|mitotic figures]] on 5 [[slides]] with the greatest [[number]] of [[mitosis]]) | ||
#'''Atypical mitoses''' (abnormal distribution of [[chromosomes]] or excessive number of [[Mitotic spindle|mitotic spindles]]) | #'''Atypical [[mitoses]]''' ([[abnormal]] [[Distribution (pharmacology)|distribution]] of [[chromosomes]] or [[Excess risk|excessive]] [[number]] of [[Mitotic spindle|mitotic spindles]]) | ||
#'''Cleared or vacuolated cytoplasm''' in >/= 25% of the tumor cells | #'''Cleared or [[Vacuole|vacuolated]] [[cytoplasm]]''' in >/= 25% of the [[Tumor cell|tumor cells]] | ||
#'''Sheeting''' ('''diffuse architecture''' of patternless sheets of cells)) in >= 1/3 of tumor cells | #'''Sheeting''' ('''[[diffuse]] architecture''' of patternless sheets of [[Cells (biology)|cells]])) in >= 1/3 of [[Tumor cell|tumor cells]] | ||
#'''Necrosis in nests''' ([[microscopic]] [[necrosis]]) | #'''[[Necrosis]] in nests''' ([[microscopic]] [[necrosis]]) | ||
#'''Venous invasion''' ([[veins]] must have [[Smooth muscle|smooth muscles]] in wall; [[tumor]] | #'''[[Venous]] [[invasion]]''' ([[veins]] must have [[Smooth muscle|smooth muscles]] in [[Vessel wall|wall]]; [[tumor cell]] [[Cluster (epidemiology)|clusters]] or sheets forming [[Polypoidy|polypoid]] [[Projection areas|projections]] into the [[Blood vessel|vessel]] [[lumen]] or [[Polypoidy|polypoid]] [[tumor]] [[thrombi]] covered by [[Endothelium|endothelial]] layer) | ||
#'''Adrenal sinusoid invasion''' ([[sinusoid]] is [[endothelial]] lined [[vessel]] in [[adrenal gland]] with little supportive [[Tissue (anatomy)|tissue]]; consider only [[sinusoids]] within [[tumor]]) | #'''[[Adrenal]] [[Sinusoid (blood vessel)|sinusoid]] [[invasion]]''' ([[sinusoid]] is [[endothelial]] [[Line|lined]] [[vessel]] in [[adrenal gland]] with little [[Support|supportive]] [[Tissue (anatomy)|tissue]]; consider only [[sinusoids]] within [[tumor]]) | ||
#'''Capsular invasion''' (nests or cords of [[tumor]] extending into or through [[capsule]] with a [[stromal]] reaction); either incomplete or complete) | #'''[[Capsule (anatomy)|Capsular]] [[invasion]]''' (nests or [[Cord|cords]] of [[tumor]] [[Extend|extending]] into or through [[capsule]] with a [[stromal]] [[reaction]]); either incomplete or complete) | ||
==== Modified Weiss criteria (score of 3 or more suggests malignancy): ==== | ==== Modified Weiss [[criteria]] ([[Score test|score]] of 3 or more [[Suggestion|suggests]] [[malignancy]]): ==== | ||
*[[Mitotic spindle|Mitotic rate]] >5 per 50 high-power fields | *[[Mitotic spindle|Mitotic rate]] >5 per 50 high-[[Power (communication)|power]] [[Field of view|fields]] | ||
*[[Cytoplasm]] (clear cells comprising 25% or less of the [[tumor]]) | *[[Cytoplasm]] ([[Clear cell|clear cells]] comprising 25% or less of the [[tumor]]) | ||
*Abnormal [[mitoses]] | *[[Abnormal]] [[mitoses]] | ||
*[[Necrosis]] | *[[Necrosis]] | ||
*[[Capsule|Capsular]] [[invasion]] | *[[Capsule|Capsular]] [[invasion]] | ||
Revision as of 16:53, 12 August 2019
For patient information, click here
|
Adrenal Carcinoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Adrenal carcinoma On the Web |
|
American Roentgen Ray Society Images of Adrenal carcinoma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
Adrenocortical carcinoma, also adrenal cortical carcinoma (ACC) and adrenal cortex cancer, is an aggressive cancer originating in the cortex (steroid hormone-producing tissue) of the adrenal gland. Adenocortical carcinoma is remarkable for the many hormonal syndromes which can occur in patients with steroid hormone-producing ("functional") tumors, including Cushing's syndrome, Conn syndrome, virilization, and feminization.
Historical perspective
- In 2017, WHO presented an update on recent classification of adrenal tumors (in fourth edition of the World Health Organization classification of endocrine tumors)[1]
Classification
- Adrenal cancer is subclassified according to its activity into:[2]
- Functional
- Non-functional
- In 2017, WHO presented the following updated classification of adrenal tumors in fourth edition of the World Health Organization classification of endocrine tumors:[1][3][4][5][6][7][8]
| Tumors of adrenal gland | |
|---|---|
| Tumors of adrenal cortex | |
| Tumors of the adrenal medulla
and extra-adrenal paraganglia |
|
| |
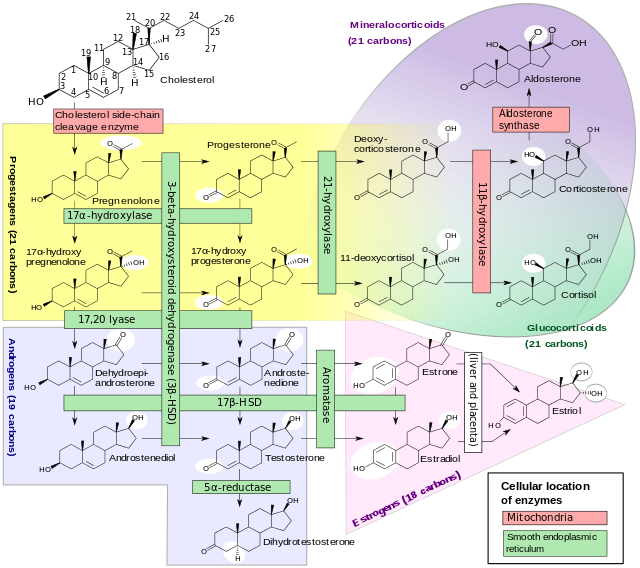
Pathophysiology
Normal anatomy and physiology of adrenal glands
- Adrenal glands are the 2 small glands located above the kidneys on either side (that's why also known as suprarenal glands)
- Normal anatomy and physiology of adrenal glands are given in the table below:
 |
{{#ev:youtube|https://www.youtube.com/watch?v=JlI5N2N4d-k}} |
Epigenetics
- Adrenal tumors are usually not biopsied prior to surgery, hence, the diagnosis is confirmed on examination of the surgical specimen by a pathologist[9][10][11][12][13][5][14]
- Following genes are involved in the development of adrenal tumors:
- IGF2 gene (increased expression at 11p15 locus-adrenocortical carcinoma)[15]
- Steroidogenic genes (increased expression-adrenocortical adenoma)
- p53
- CTNNB1 (Wnt pathway)
- Beta-catenin
- ACTH receptor
- BUB1B
- PINK1
- DLG7
- MEN1
- IGF2R
- p16
- p16ink/ p14arf
- CDKN2A
- Fibroblast growth factor 4 (FGF4)
- Cyclin-dependent kinase 4 (CDK4)
- Cyclin E1 (CCNE1)
- H19 (11p15 locus)
- PLAGL1
- G0S2
- NDRG2
- IGF1R
- RPTOR
- FRAP1
- Alterations in the following chromosomal regions are associated with adrenal tumors:
- 11q13
- 12q
- 5q
- 1p
- 7p
- 13q
- 16q
- 22q
- 19
- 20
- Loss of heterozygosity (LOH) at the following loci is strongly associated with high malignant potential of adrenal tumors:
- miRNAs involved in the pathogenesis of adrenal tumors are as follows:
- miR-184 (upregulated)
- miR-210 (upregulated)
- miR-503 (upregulated)
- miR-214 (downregulated)
- miR-375 (downregulated)
- miR-511 (downregulated)
- miR-483 (significant upregulation in pediatric adrenocortical carcinoma)
- miR-99a
- miR-100
 |
 |
 |
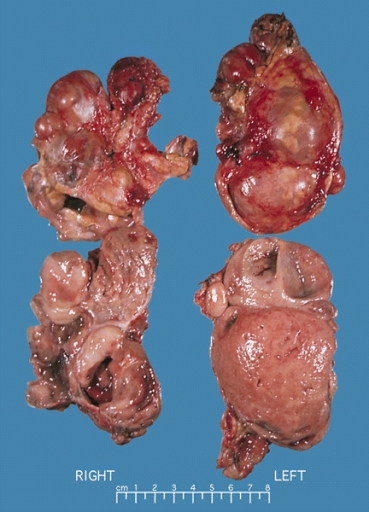
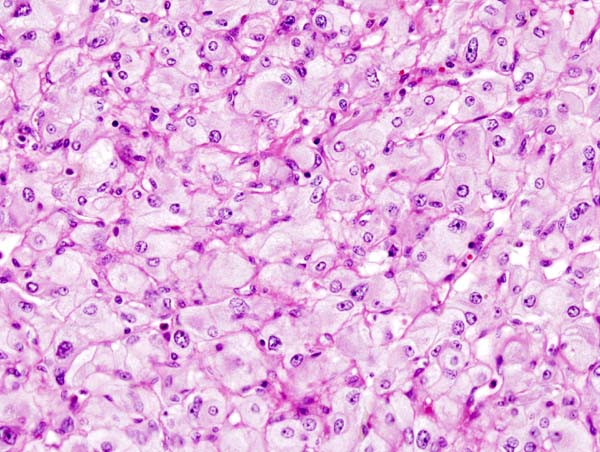
Gross pathology
Adrenocortical carcinoma
- Gross pathology of adrenocortical carcinomas shows often a large mass (>5 cm in largest diameter), with a tan-yellow cut surface and areas of hemorrhage and necrosis (always present)
- Cut surface ranges from brown to orange to yellow depending on the lipid content of the cells
- Typical adrenocortical carcinoma consists of a hypercellular population of cells with the earliest form of tumor necrosis
- Atypical adrenocortical carcinoma consists of a solid growth pattern and an abundant eosinophilic cytoplasm with focal clear areas, consistent with lipid
 |
Pheochromocytoma
- Gross pathology of pheochromocytoma varies from small to large and usually associated with hemorrhage and necrosis
- Pheochromocytoma is usually lobulated and small tumors have compressed adrenal gland
- Familial tumors are bilateral
- It may be associated with hyperplasia in the adjacent medulla
- Shows Chromaffin reaction: fresh tumor's cut section turns dark brown on adding potassium dichromate at pH 5-6
 |
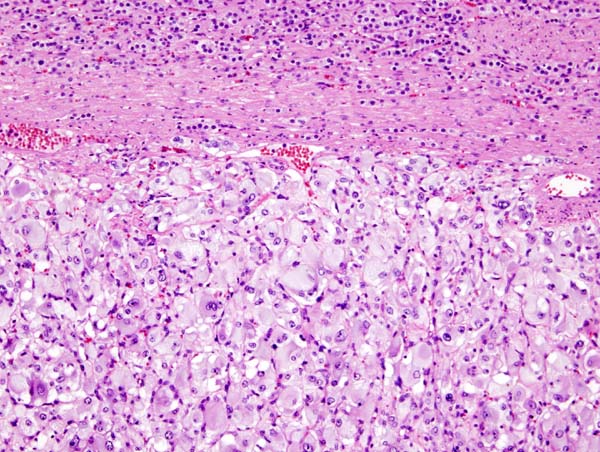
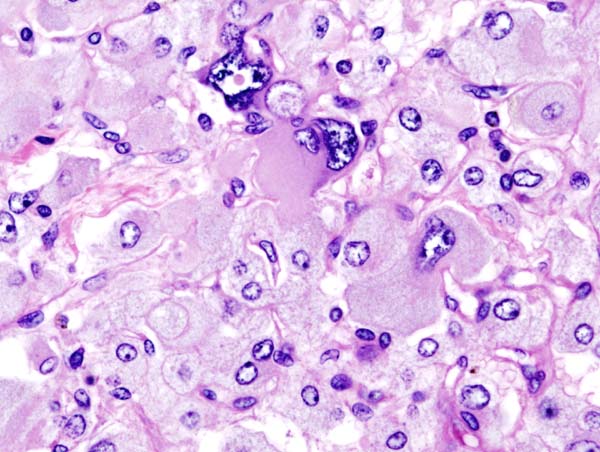
Microscopic pathology
- Pheochromocytoma demonstrates a typical nesting (Zellballen) pattern on histopathological analysis which is composed of well-defined clusters of tumor cells containing eosinophilic cytoplasm separated by fibrovascular stroma
- Histopathological criterias for the diagnosis of adrenocortical carcinoma are given below
Pathologic criterias for adrenocortical carcinoma
- Different pathological criterias for adrenocortical carcinoma are given in the table below:[16][17][18][19][20][21][22][23]
| Pathologic criteria | Details | Age applicability |
|---|---|---|
| Weiss criteria |
Adrenocortical carcinoma can be diagnosed by the presence of at least 3 of the 9 Weiss criteria:
Modified Weiss criteria (score of 3 or more suggests malignancy): |
Adults |
| Volante criteria |
Simplified criteria by Volante et al (not widely used) is as follows:
| |
| Wieneke et al and Dehner & Hill |
Wieneke et al and Dehner and Hill proposed the following very simple system:
|
Pediatrics |
 |
 |
 |
 |
|
{{#ev:youtube|7jMFENhPaOM}} |
{{#ev:youtube|7yjxG3KmX98}} |
Epidemiology and demographics
- Adrenal carcinoma is a relatively rare tumor
- It accounts for only 0.02-0.2% of all the cancer-related deaths[24]
- It has bimodal age distribution i.e. occurs in children or in adults round the age of 40-50 years[25]
- Prevalence of adrenocortical carcinoma is estimated to be between 4 and 12 per million in adults[26]
- There is an increased prevalence of adrenocortical carcinoma in female patients with Cushing syndrome diagnosed during pregnancy as compared to the non-pregnant patients
- Incidence of adrenocortical carcinoma is estimated to be between 0.72/1 to 2 per million cases per year in adults in North America and Europe[27]
- Incidence is ten times lower except in South Brazil having a higher incidence of pediatric adrenocortical carcinoma (due to a specific germline p53 mutation)
- Increased risk of adrenal carcinoma in females than males has been reported
- Pheochromocytoma is mostly found in middle-aged adults
Risk factors
- Risk factors for adrenal carcinoma include:[28][29]
- Genetic mutations
- Family history of adrenal carcinoma
- Having some genetic diseases increases the chance of getting adrenal carcinoma upto 15% and include:[30][31][32][33][34]
- Multiple endocrine neoplasia (MEN1 and MEN2)
- Familial adenomatous polyposis (FAP)
- Beckwith-Wiedemann syndrome
- Li-Fraumeni syndrome
- Lynch syndrome or Hereditary nonpolyposis colorectal cancer (HNPCC)
- Von Hippel-Lindau disease
- Carney Complex/Syndrome
- Neurofibromatosis type 1
- Congenital adrenal hyperplasia
- Cigarette smoking
- Oral contraceptives use (especially before 25 years of age)
- Exposure to carcinogens
Natural History, Complications and Prognosis
- ACC, generally, carries a poor prognosis and is unlike most tumours of the adrenal cortex, which are benign (adenomas) and only occasionally cause Cushing's syndrome
- Five-year disease-free survival for a complete resection of a stage I-III ACC is approximately <30%[35][36][37][38]
- Metastatic adrenocortical carcinoma has an overall survival of less than one year[27]
- Local adrenal tumors of McFarlane stages 1 and 2 have a better outcome and prognosis[26]
- Invasive and metastatic adrenal tumors of McFarlane stages 3 and 4 have a poor outcome and prognosis
- Weiss criteria has a really good prognostic value for adrenocortical tumors[39][9][35]
- Limitations to Weiss criteria include:
- Difficult to apply to individual cases
- Requires trained pathologists
- Score is not totally reliable (may differ from one area to another in the same tumor)
- tumor size and histological grade are strong predictors of recurrence (tumors >5 cm in diameter and a Weiss score of ≥4)
- Other diagnostic markers for malignancy are required due to limitations of Weiss crieteria, three of the tested molecular markers which are strong predictors of disease-free survival include:
- 17p13 LOH
- 11p15 LOH caused by parental isodisomy (overexpression of IGF-II gene which leads to proliferation of malignant adrenal H295R cells)
- Overexpression of IGF-II gene
Diagnosis
History and Symptoms
Symptoms in children
- Most tumors in children are functional, and present with:
- Virilization (most common presenting symptom)
- Cushing's syndrome (glucocorticoid excess):
- Weight gain
- Muscle wasting
- Purple striae/lines on the abdomen
- Fatty "buffalo hump" on the neck
- "Moonlike" face
- Thinning of skin
- Fragile skin
- Precocious puberty[44]
{{#ev:youtube|https://www.youtube.com/watch?v=ea1sXgd5ui8&t=697s}}
Symptoms in adults
- Adults present with hormonal syndromes such as:
- Cushing's syndrome (most common)
- Mixed Cushing's syndrome and virilization (glucocorticoid and androgen overproduction), with virilization presenting most obviously in women as:
- Excess facial and body hair (hirsutism)
- Acne
- Enlargement of clitoris
- Deepening of voice
- Coarsening of facial features
- Cessation of menstruation (amenorrhea)
- Feminization (i.e. estrogen excess, most readily seen in men) presents as:
- Breast enlargement (gynecomastia)
- Decreased libido
- Impotence
- Conn syndrome (mineralcorticoid excess, <10% cases) with low plasma renin activity, and high serum aldosterone presents with:[45]
- Pheochromocytoma-like hypersecretion of catecholamines (rarely)
Presentation of non-functional adrenal carcinoma
- Non-functional tumors (40%) usually present with:
- Abdominal or flank or back pain
- Lump in abdomen
- Feeling of fullness (might keeps patient from eating much)
- Asymptomatic
- Detected incidentally
Physical Examination
- All patients with suspected adrenocortical carcinoma should be carefully examined for the signs and symptoms of following hormonal syndromes as mentioned above:
Laboratory findings
- Hormonal syndromes should be confirmed with laboratory testing
| Hormonal syndrome | Laboratory findings |
|---|---|
| Cushing syndrome |
|
| Virilization |
|
| Conn syndrome |
|
| Feminization |
Imaging studies
CT
- Radiological studies of the abdomen, such as CT scans and magnetic resonance imaging are useful for identifying the site of the tumor, differentiating it from other diseases, such as adrenocortical adenoma, and determining the extent of invasion of the tumor into surrounding organs and tissues.[46]
- CT scans of the chest and bone scans are routinely performed to look for metastases to the lungs and bones respectively. These studies are critical in determining whether or not the tumor can be surgically removed, the only potential cure at this time.
- CT scan of adrenocortical carcinoma shows:
- Central tumor necrosis
- Calcifications
- Larger and more heterogeneous tumor
MRI
- Adrenocortical carcinoma appears as a large heterogeneous mass with low fat content
PET scan
Molecular imaging
- Iodometomidate (IMTO) as tracer for molecular imaging of cytochrome P450 family 11B (Cyp11B) enzymes[49]
Treatment
Medical Therapy
- Radiation therapy
- Radiofrequency ablation may be used for palliation in patients who are not surgical candidates
- Chemotherapy (chemoembolization) regimens typically include the drug mitotane, an inhibitor of steroid synthesis which is toxic to cells of the adrenal cortex, as well as standard cytotoxic drugs. One widely used regimen consists of cisplatin, doxorubicin, etoposide) and mitotane. The endocrine cell toxin streptozotocin has also been included in some treatment protocols. Chemotherapy may be given to patients with unresectable disease, to shrink the tumor prior to surgery (neoadjuvant chemotherapy), or in an attempt to eliminate microscopic residual disease after surgery (adjuvant chemotherapy).[50][51][52][53]
- Hormonal therapy with steroid synthesis inhibitors such as aminoglutethimide may be used in a palliative manner to reduce the symptoms of hormonal syndromes
Surgery
- The only curative treatment is complete surgical excision of the tumor, which can be performed even in the case of invasion into large blood vessells, such as the renal vein or inferior vena cava
- The 5-year survival rate after successful surgery is 50-60%, but unfortunately, a large percentage of patients are not surgical candidates
- surgical (McFarlane) criteria
Differentiating Adrenal carcinoma from other Diseases
Bilateral
- ACTH-dependent Cushing's Syndrome
- Adrenal Hemorrhage
- Adrenal metastases
- Amyloidosis
- Congenital adrenal hyperplasia
- Conn syndrome
- Fungi
- Idiopathic bilateral adrenal hypertrophy
- Leukemia
- Lymphoma
- Micronodular Adrenal Disease
- Pheochromocytoma
- Tuberculosis
Unilateral
- Adrenal adenoma
- Adrenal metastases
- Adrenolipoma
- Ganglioneuroma
- Hematoma
- Myelolipoma
- Pheochromocytoma
- Primary aldosteronism
References
- ↑ 1.0 1.1 Lam AK (2017). "Update on Adrenal Tumours in 2017 World Health Organization (WHO) of Endocrine Tumours". Endocr Pathol. 28 (3): 213–227. doi:10.1007/s12022-017-9484-5. PMID 28477311.
- ↑ "Adrenocortical Carcinoma Treatment - National Cancer Institute".
- ↑ "WHO Classification of Tumours of Endocrine Organs. Fourth Edition - WHO - OMS -".
- ↑ "Update on Adrenal Tumours in 2017 World Health Organization (WHO) of Endocrine Tumours - Semantic Scholar".
- ↑ 5.0 5.1 Pinto EM, Chen X, Easton J, Finkelstein D, Liu Z, Pounds S; et al. (2015). "Genomic landscape of paediatric adrenocortical tumours". Nat Commun. 6: 6302. doi:10.1038/ncomms7302. PMC 4352712. PMID 25743702.
- ↑ Zheng S, Cherniack AD, Dewal N, Moffitt RA, Danilova L, Murray BA; et al. (2016). "Comprehensive Pan-Genomic Characterization of Adrenocortical Carcinoma". Cancer Cell. 30 (2): 363. doi:10.1016/j.ccell.2016.07.013. PMID 27505681.
- ↑ Zheng S, Cherniack AD, Dewal N, Moffitt RA, Danilova L, Murray BA; et al. (2016). "Comprehensive Pan-Genomic Characterization of Adrenocortical Carcinoma". Cancer Cell. 29 (5): 723–736. doi:10.1016/j.ccell.2016.04.002. PMC 4864952. PMID 27165744.
- ↑ Assié G, Letouzé E, Fassnacht M, Jouinot A, Luscap W, Barreau O; et al. (2014). "Integrated genomic characterization of adrenocortical carcinoma". Nat Genet. 46 (6): 607–12. doi:10.1038/ng.2953. PMID 24747642.
- ↑ 9.0 9.1 Weiss LM (1984). "Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors". Am J Surg Pathol. 8 (3): 163–9. PMID 6703192.
- ↑ "Mechanism of abnormal production of adrenal androgens in patients with adrenocortical adenomas and carcinomas | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ "Variable Expression of the Transcription Factors cAMP Response Element-Binding Protein and Inducible cAMP Early Repressor in the Normal Adrenal Cortex and in Adrenocortical Adenomas and Carcinomas | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ Fassnacht M, Libé R, Kroiss M, Allolio B (2011). "Adrenocortical carcinoma: a clinician's update". Nat Rev Endocrinol. 7 (6): 323–35. doi:10.1038/nrendo.2010.235. PMID 21386792.
- ↑ Menon V, Krishnamurthy SV (2006). "Adrenocortical carcinomas: a 12-year clinicopathologic study of 15 cases". Indian J Pathol Microbiol. 49 (1): 7–11. PMID 16625963.
- ↑ Libè R, Groussin L, Tissier F, Elie C, René-Corail F, Fratticci A; et al. (2007). "Somatic TP53 mutations are relatively rare among adrenocortical cancers with the frequent 17p13 loss of heterozygosity". Clin Cancer Res. 13 (3): 844–50. doi:10.1158/1078-0432.CCR-06-2085. PMID 17289876.
- ↑ McCabe MJ, Pinese M, Chan CL, Sheriff N, Thompson TJ, Grady J; et al. (2019). "Genomic stratification and liquid biopsy in a rare adrenocortical carcinoma (ACC) case, with dual lung metastases". Cold Spring Harb Mol Case Stud. 5 (2). doi:10.1101/mcs.a003764. PMC 6549567 Check
|pmc=value (help). PMID 30936196. - ↑ Magro G, Esposito G, Cecchetto G, Dall'Igna P, Marcato R, Gambini C; et al. (2012). "Pediatric adrenocortical tumors: morphological diagnostic criteria and immunohistochemical expression of matrix metalloproteinase type 2 and human leucocyte-associated antigen (HLA) class II antigens. Results from the Italian Pediatric Rare Tumor (TREP) Study project". Hum Pathol. 43 (1): 31–9. doi:10.1016/j.humpath.2011.04.016. PMID 21820153.
- ↑ Tischler AS, Kimura N, Mcnicol AM (2006). "Pathology of pheochromocytoma and extra-adrenal paraganglioma". Ann N Y Acad Sci. 1073: 557–70. doi:10.1196/annals.1353.059. PMID 17102124.
- ↑ Ragazzon B, Libé R, Gaujoux S, Assié G, Fratticci A, Launay P; et al. (2010). "Transcriptome analysis reveals that p53 and {beta}-catenin alterations occur in a group of aggressive adrenocortical cancers". Cancer Res. 70 (21): 8276–81. doi:10.1158/0008-5472.CAN-10-2014. PMID 20959480.
- ↑ Ragazzon B, Libé R, Assié G, Tissier F, Barreau O, Houdayer C; et al. (2014). "Mass-array screening of frequent mutations in cancers reveals RB1 alterations in aggressive adrenocortical carcinomas". Eur J Endocrinol. 170 (3): 385–91. doi:10.1530/EJE-13-0778. PMID 24347427.
- ↑ Tissier F (2008). "[Sporadic adrenocortical tumors: genetics and perspectives for the pathologist]". Ann Pathol. 28 (5): 409–16. doi:10.1016/j.annpat.2008.07.005. PMID 19068395.
- ↑ Gicquel C, Bertagna X, Gaston V, Coste J, Louvel A, Baudin E; et al. (2001). "Molecular markers and long-term recurrences in a large cohort of patients with sporadic adrenocortical tumors". Cancer Res. 61 (18): 6762–7. PMID 11559548.
- ↑ Das S, Sengupta M, Islam N, Roy P, Datta C, Mishra PK; et al. (2016). "Weineke criteria, Ki-67 index and p53 status to study pediatric adrenocortical tumors: Is there a correlation?". J Pediatr Surg. 51 (11): 1795–1800. doi:10.1016/j.jpedsurg.2016.07.014. PMID 27567308.
- ↑ Chatterjee G, DasGupta S, Mukherjee G, Sengupta M, Roy P, Arun I; et al. (2015). "Usefulness of Wieneke criteria in assessing morphologic characteristics of adrenocortical tumors in children". Pediatr Surg Int. 31 (6): 563–71. doi:10.1007/s00383-015-3708-x. PMID 25895073.
- ↑ "Adrenal Carcinoma: Practice Essentials, Background, Pathophysiology".
- ↑ "Adrenal Cancer Causes and Symptoms".
- ↑ 26.0 26.1 Libè R, Fratticci A, Bertherat J (2007). "Adrenocortical cancer: pathophysiology and clinical management". Endocr Relat Cancer. 14 (1): 13–28. doi:10.1677/erc.1.01130. PMID 17395972.
- ↑ 27.0 27.1 Cabezon-Gutierrez L, Franco-Moreno AI, Khosravi-Shahi P, Custodio-Cabello S, Garcia-Navarro MJ, Martin-Diaz RM (2015). "Clinical Case of Metastatic Adrenocortical Carcinoma With Unusual Evolution: Review the Literature". World J Oncol. 6 (6): 485–490. doi:10.14740/wjon936w. PMC 5624676. PMID 28983351.
- ↑ Hsing AW, Nam JM, Co Chien HT, McLaughlin JK, Fraumeni JF (1996). "Risk factors for adrenal cancer: an exploratory study". Int J Cancer. 65 (4): 432–6. doi:10.1002/(SICI)1097-0215(19960208)65:4<432::AID-IJC6>3.0.CO;2-Y. PMID 8621222.
- ↑ "Adrenal Gland Cancer (Adrenocortical Carcinoma) | Cleveland Clinic: Health Library".
- ↑ "Top Adrenal Cancer Causes & Factors That Put You at Risk | CTCA".
- ↑ "Adrenal Cancer Risk Factors".
- ↑ "Adrenal Cancer Risk Factors | Roswell Park Comprehensive Cancer Center".
- ↑ "Adrenal Cancer: Causes, Symptoms, and Diagnosis".
- ↑ "Adrenal cancer - Symptoms and causes - Mayo Clinic".
- ↑ 35.0 35.1 Weiss LM, Medeiros LJ, Vickery AL (1989). "Pathologic features of prognostic significance in adrenocortical carcinoma". Am J Surg Pathol. 13 (3): 202–6. PMID 2919718.
- ↑ Moreno S, Montoya G, Armstrong J, Leteurtre E, Aubert S, Vantyghem MC; et al. (2004). "Profile and outcome of pure androgen-secreting adrenal tumors in women: experience of 21 cases". Surgery. 136 (6): 1192–8. doi:10.1016/j.surg.2004.06.046. PMID 15657575.
- ↑ Wagner M, Walter PR, Ghnassia JP, Gasser B (1993). "[Adrenocortical tumors. I. Prognostic evaluation of a series of 17 cases using the Weiss criteria]". Ann Pathol. 13 (5): 306–11. PMID 8311856.
- ↑ Gandour MJ, Grizzle WE (1986). "A small adrenocortical carcinoma with aggressive behavior. An evaluation of criteria for malignancy". Arch Pathol Lab Med. 110 (11): 1076–9. PMID 3778125.
- ↑ Jain M, Kapoor S, Mishra A, Gupta S, Agarwal A (2010). "Weiss criteria in large adrenocortical tumors: a validation study". Indian J Pathol Microbiol. 53 (2): 222–6. doi:10.4103/0377-4929.64325. PMID 20551521.
- ↑ "Hypoaldosteronism accompanied by normal or elevated mineralocorticosteroid pathway steroid: a marker of adrenal carcinoma. | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ "ADRENAL CORTICAL CARCINOMA IN A MALE WITH EXCESS GONADOTROPIN IN THE URINE | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic".
- ↑ "UpToDate".
- ↑ Allolio B, Fassnacht M (2006). "Clinical review: Adrenocortical carcinoma: clinical update". J Clin Endocrinol Metab. 91 (6): 2027–37. doi:10.1210/jc.2005-2639. PMID 16551738.
- ↑ Sandrini R, Ribeiro RC, DeLacerda L (1997). "Childhood adrenocortical tumors". J Clin Endocrinol Metab. 82 (7): 2027–31. doi:10.1210/jcem.82.7.4057. PMID 9215267.
- ↑ Moreno S, Guillermo M, Decoulx M, Dewailly D, Bresson R, Proye Ch (2006). "Feminizing adreno-cortical carcinomas in male adults. A dire prognosis. Three cases in a series of 801 adrenalectomies and review of the literature". Ann Endocrinol (Paris). 67 (1): 32–8. PMID 16596055.
- ↑ Szolar DH, Korobkin M, Reittner P, Berghold A, Bauernhofer T, Trummer H; et al. (2005). "Adrenocortical carcinomas and adrenal pheochromocytomas: mass and enhancement loss evaluation at delayed contrast-enhanced CT". Radiology. 234 (2): 479–85. doi:10.1148/radiol.2342031876. PMID 15671003.
- ↑ Groussin L, Bonardel G, Silvéra S, Tissier F, Coste J, Abiven G; et al. (2009). "18F-Fluorodeoxyglucose positron emission tomography for the diagnosis of adrenocortical tumors: a prospective study in 77 operated patients". J Clin Endocrinol Metab. 94 (5): 1713–22. doi:10.1210/jc.2008-2302. PMID 19190108.
- ↑ Khan TS, Sundin A, Juhlin C, Långström B, Bergström M, Eriksson B (2003). "11C-metomidate PET imaging of adrenocortical cancer". Eur J Nucl Med Mol Imaging. 30 (3): 403–10. doi:10.1007/s00259-002-1025-9. PMID 12634969.
- ↑ Hahner S, Stuermer A, Kreissl M, Reiners C, Fassnacht M, Haenscheid H; et al. (2008). "[123 I]Iodometomidate for molecular imaging of adrenocortical cytochrome P450 family 11B enzymes". J Clin Endocrinol Metab. 93 (6): 2358–65. doi:10.1210/jc.2008-0050. PMID 18397978.
- ↑ Kwok GTY, Zhao JT, Glover AR, Gill AJ, Clifton-Bligh R, Robinson BG; et al. (2019). "microRNA-431 as a Chemosensitizer and Potentiator of Drug Activity in Adrenocortical Carcinoma". Oncologist. 24 (6): e241–e250. doi:10.1634/theoncologist.2018-0849. PMC 6656493 Check
|pmc=value (help). PMID 30918109. - ↑ Abraham J, Bakke S, Rutt A, Meadows B, Merino M, Alexander R; et al. (2002). "A phase II trial of combination chemotherapy and surgical resection for the treatment of metastatic adrenocortical carcinoma: continuous infusion doxorubicin, vincristine, and etoposide with daily mitotane as a P-glycoprotein antagonist". Cancer. 94 (9): 2333–43. doi:10.1002/cncr.10487. PMID 12015757.
- ↑ Berruti A, Terzolo M, Pia A, Angeli A, Dogliotti L (1998). "Mitotane associated with etoposide, doxorubicin, and cisplatin in the treatment of advanced adrenocortical carcinoma. Italian Group for the Study of Adrenal Cancer". Cancer. 83 (10): 2194–200. PMID 9827725.
- ↑ Williamson SK, Lew D, Miller GJ, Balcerzak SP, Baker LH, Crawford ED (2000). "Phase II evaluation of cisplatin and etoposide followed by mitotane at disease progression in patients with locally advanced or metastatic adrenocortical carcinoma: a Southwest Oncology Group Study". Cancer. 88 (5): 1159–65. PMID 10699907.