Tuberculosis pathophysiology: Difference between revisions
Mohamed riad (talk | contribs) |
Mohamed riad (talk | contribs) |
||
| Line 13: | Line 13: | ||
==Pathogenesis== | ==Pathogenesis== | ||
[[Transmission (medicine)|Transmission]] of ''M. [[tuberculosis]]'' bacterium occurs when individuals with active [[Lung|pulmonary]] disease [[cough]], [[speak]], [[sneeze]] or sing [[expelling]] the [[Infection|infectious]] [[droplets]] that can pass to the terminal [[Bronchiole|bronchioles]] and [[Pulmonary alveolus|alveoli]] then [[Phagocytosis|phagocytosed]] by [[Alveolus|alveolar]] [[Macrophage|macrophages]] where they can [[replicate]] in the [[Endosome|endosomes]] of [[Alveolus|alveolar]] [[Macrophage|macrophages]]. As a part of the [[Immunity (medical)|immune]] response by these [[Macrophage|macrophages]], the [[Alveolus|alveolar]] [[Macrophage|macrophages]] [[Release (information centre)|release]] [[Cytokine|cytokines]] that [[recruits]] further [[Macrophage|macrophages]], [[Neutrophil|neutrophils]], and [[Monocyte|monocytes]], surrounding the [[bacilli]]. Despite having a very low [[Infection|infectious]] dose (ID<200 bacteria), 90% of the infected [[Immunocompetence|immunocompetent]] individuals are [[Asymptomatic condition|asymptomatic]]. In most cases, the bacteria may either be eliminated or enclosed within a [[granuloma]]. The [[granuloma]] is a structured, radial [[aggregation]] of [[Macrophage|macrophages]], [[epithelioid]] cells, T [[Lymphocyte|lymphocytes]], B [[Lymphocyte|lymphocytes]], and [[Fibroblast|fibroblasts]] that prevents the spreading of [[M. tuberculosis|mycobacteria]] and enhances interaction of the [[Immunity (medical)|immune]] cells.<ref name="Mandell">{{cite book | last = Mandell | first = Gerald | title = Mandell, Douglas, and Bennett's principles and practice of infectious diseases | publisher = Churchill Livingstone/Elsevier | location = Philadelphia, PA | year = 2010 | isbn = 0443068399 }}</ref> The primary site of [[infection]] in the [[lung]] is called the [[Ghon focus]] that is mainly located in either the upper part of the lower [[Lobe (anatomy)|lobe]], or the lower part of the upper [[Lobe (anatomy)|lobe]].<ref name="Mandell"></ref><ref name="Herrmann_2005">{{cite journal |author=Herrmann J, Lagrange P |title=Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse? |journal=Pathol Biol (Paris) |volume=53 |issue=1 |pages=35–40 |year=2005 | pmid = 15620608}}</ref> | |||
===Primary Infection=== | ===Primary Infection=== | ||
The infected [[macrophages]] are transported through the [[lymph|lymphatics]] to the regional [[lymph nodes]] in the [[Immunocompetence|immunocompetent]] individuals. However, with impaired immune response, these [[macrophages]] can pass through the bloodstream to enter any part of the body. Those foci of primary infection usually resolve without any consequences, but they can act as a foci of M. tuberculosis dissemination. There are particular organs that are more susceptible to bacterial replication as well as being potential metastatic foci which include:<ref name="Mandell"></ref><ref name="Herrmann_2005">{{cite journal |author=Herrmann J, Lagrange P |title=Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse? |journal=Pathol Biol (Paris) |volume=53 |issue=1 |pages=35–40 |year=2005 | pmid = 15620608}}</ref> | |||
*Apical-posterior regions of the lungs | *Apical-posterior regions of the lungs | ||
| Line 25: | Line 25: | ||
*Juxta ependymal [[meningeal]] regions | *Juxta ependymal [[meningeal]] regions | ||
Although TB can | Although [[Tuberculosis|TB]] is a [[systemic]] disease and all [[Organ (anatomy)|organs]] can be affected, the [[heart]], [[pancreas]], [[skeletal muscle]]s and [[thyroid]] are rarely involved.<ref>{{cite journal |author=Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15857515 |title=Tuberculous dilated cardiomyopathy: an under-recognized entity? |journal=BMC Infect Dis |volume=5 |issue=1 |pages=29 |year=2005 |pmid=15857515}}</ref> In a few cases, when the [[Infection|infectious]] [[dose]] is high and [[antigens]] concentration in the primary focus is high, the [[immune response]] and [[hypersensitivity]] can lead to [[necrosis]] and [[calcification]] of this lesion, and these primary [[Calcification|calcified]] foci are then called '''Ranke complex'''.<ref name="Mandell"></ref><ref name="Grosset">{{cite journal |author=Grosset J |title=Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary |journal=Antimicrob Agents Chemother |volume=47 |issue=3 |pages=833-6 |year=2003 | pmid = 12604509}}</ref> | ||
===Progression of the Primary Infection=== | ===Progression of the Primary Infection=== | ||
Primary foci of [[infection]] can enter the large [[pulmonary]] [[lymph nodes]]. These may lead to:<ref name="Mandell"></ref> | |||
*[[Bronchial]] collapse | *[[Bronchial]] [[Collapse (medical)|collapse]] | ||
* | *[[atelectasis]] | ||
*[[bronchus|Bronchial]] erosion, with more | *[[bronchus|Bronchial]] [[Erosion (dental)|erosion]], with more [[dissemination]] of infection | ||
<nowiki>*</nowiki>In non-caucasian children, [[Old age|elderly]] patients and [[Human Immunodeficiency Virus (HIV)|HIV]]/[[HIV AIDS|AIDS]], the immune response is impaired, consequently the primary focus of infection can deteriorate into constitute progressive primary disease, with advancing [[pneumonia]]. | |||
<nowiki>*</nowiki>In additin,the infection may result in cavity formation with transmission of the infection through the [[bronchi]].<ref name="Mandell"></ref><ref name="pmid3990748">{{cite journal| author=Stead WW, Lofgren JP, Warren E, Thomas C| title=Tuberculosis as an endemic and nosocomial infection among the elderly in nursing homes. | journal=N Engl J Med | year= 1985 | volume= 312 | issue= 23 | pages= 1483-7 | pmid=3990748 | doi=10.1056/NEJM198506063122304 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3990748 }} </ref><ref name="pmid2274719">{{cite journal| author=Murray JF| title=Cursed duet: HIV infection and tuberculosis. | journal=Respiration | year= 1990 | volume= 57 | issue= 3 | pages= 210-20 | pmid=2274719 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2274719 }} </ref> | |||
<nowiki>*</nowiki>In young children, the onset of immune response may be delayed after the [[Bacteria|bacterial]] dissemination resulting in '''military tuberculosis'''. Bacteria can spread directly from the primary focus, or from the ''Weigart focus'' ([[Metastasis|metastatic]] focus adjacent to a [[pulmonary vein]]) through the blood.<ref name="Mandell"></ref><ref name="Kim_2003">{{cite journal |author=Kim J, Park Y, Kim Y, Kang S, Shin J, Park I, Choi B |title=Miliary tuberculosis and acute respiratory distress syndrome |journal=Int J Tuberc Lung Dis |volume=7 |issue=4 |pages=359-64 |year=2003 | pmid = 12733492}}</ref> | |||
<nowiki>*</nowiki>In younger patients, [[rupture]] of subpleural foci into the [[pleural space]] may occur leading to [[serofibrinous]] [[pleurisy]].<ref name="Mandell"></ref> The most serious site of the M. [[tuberculosis]] dissemination is the postero-apical regions of the lung where it can [[replicate]] hidden from the [[immune system]].<ref name="Mandell"></ref> | |||
==Immunopathogenesis== | ==Immunopathogenesis== | ||
There are two types of [[Immunity (medical)|immune]] response against [[tuberculosis]] that include the [[Innate immune system|innate]] and [[acquired]] [[Immunity (medical)|immune]] responses. However, the [[Cell-mediated immunity|cell-mediated]] [[Immunity (medical)|immune]] response predominates over the [[Humoral immunity|humoral]] type. | |||
===Innate Immune Response=== | ===Innate Immune Response=== | ||
Initially, The [[Immunity (medical)|immune]] response generated against ''[[M. tuberculosis]]'' is minimal, enabling it to replicate inside the alveolar [[macrophages]] forming the [[Ghon focus]], or metastatic foci. Recognition and phagocytosis of the ''M. tuberculosis'' bacilli by the [[Alveolus|alveolar]] [[Macrophage|macrophages]] occurs through interaction with certain [[Receptor (biochemistry)|receptors]] that are located on the surface of macrophages:<ref name="pmid10358769">{{cite journal| author=Aderem A, Underhill DM| title=Mechanisms of phagocytosis in macrophages. | journal=Annu Rev Immunol | year= 1999 | volume= 17 | issue= | pages= 593-623 | pmid=10358769 | doi=10.1146/annurev.immunol.17.1.593 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10358769 }} </ref> | |||
*Toll-like Receptor 2 (TLR2) | *[[Toll-like Receptor]] 2 (TLR2) | ||
*TLR4 | *TLR4 | ||
*TLR9 | *TLR9 | ||
*Dectin-1 | *Dectin-1 | ||
*DC-SIGN | *DC-SIGN | ||
*Mannose receptor | *[[Mannose-binding protein|Mannose]] receptor | ||
*Complement receptors | *[[Complement]] receptors | ||
*NOD2 | *NOD2 | ||
===Acquired Immunity and Granuloma Formation=== | ===Acquired Immunity and Granuloma Formation=== | ||
<nowiki>*</nowiki>The [[granuloma]] control the [[infection]]; however, it enables the [[mycobacterium]] to survive inside for a long time. | |||
<nowiki>*</nowiki>It is important to maintain a balance between the [[pro-inflammatory]] and anti-inflammatory [[Cytokine|cytokines]] released to decrease or control the [[Mycobacterium|mycobacterial]] proliferation. | |||
<nowiki>*</nowiki>[[Tumor necrosis factor-alpha|TNF-α]] and [[IFN-γ]] stimulate [[granuloma]] formation. On the other hand, [[Interleukin 10|IL-10]] is one of the major negative [[regulators]] and inhibitors of [[granuloma]] formation. | |||
<nowiki>*</nowiki>The [[granuloma]] is structured by blood-derived [[Macrophage|macrophages]] (derived from [[Monocyte|monocytes]]), [[epithelioid]] cells (differentiated [[Macrophage|macrophages]]), and [[multinucleated giant cells]] (also known as [[Langhans giant cell|Langhans giant cells]]), surrounded by [[T lymphocytes]]. | |||
[[Caseous granulomas|*Caseous granulomas]] are the main characteristic of [[tuberculosis]]. The caseous granulomas include [[epithelioid]] [[Macrophage|macrophages]] and some [[Lymphocyte|lymphocytes]] with a necrotic center. Other types of [[granuloma]] include non-necrotizing granulomas, that are mainly formed of [[Macrophage|macrophages]] and a few [[Lymphocyte|lymphocytes]], necrotic neutrophilic granulomas, and completely fibrotic granulomas.<ref name="pmid22811737">{{cite journal| author=Silva Miranda M, Breiman A, Allain S, Deknuydt F, Altare F| title=The tuberculous granuloma: an unsuccessful host defense mechanism providing a safe shelter for the bacteria? | journal=Clin Dev Immunol | year= 2012 | volume= 2012 | issue= | pages= 139127 | pmid=22811737 | doi=10.1155/2012/139127 | pmc=PMC3395138 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22811737 }} </ref> | |||
<nowiki>*</nowiki>Several [[Chemokine|chemokines]] are involved in granuloma formation released either from the [[Respiratory system|respiratory]] tract [[epithelium]] or the [[Immunity (medical)|immune]] cells themselves. | |||
<nowiki>*</nowiki>Interaction with CCR2 receptor with (CCL2/MCP-1, CCL12, and CCL13) is necessary for the initial recruitment of macrophages. | |||
<nowiki>*</nowiki>Macrophages and lymphocytes release a chemokine called [[osteopontin]] that enhances the [[adhesion]] and [[Recruitment status|recruitment]] of the [[Immunity (medical)|immune]] cells. | |||
<nowiki>*</nowiki>CCL19 and CCL21 are important for recruitment of [[Interferon|IFN]]--producing T cells. | |||
<nowiki>*</nowiki>In [[Tumor necrosis factors|TNF]]-deficient mice, absence of these chemokines as a result of inhibition of the expression of the CC and CXC [[Chemokine|chemokines]] prevents the [[Recruitment status|recruitment]] of other [[Macrophage|macrophages]] and [[T lymphocytes]]. This finding sheds the light on the role of [[Tumor necrosis factors|TNF]] in [[granuloma]] formation.<ref name="pmid22811737">{{cite journal| author=Silva Miranda M, Breiman A, Allain S, Deknuydt F, Altare F| title=The tuberculous granuloma: an unsuccessful host defense mechanism providing a safe shelter for the bacteria? | journal=Clin Dev Immunol | year= 2012 | volume= 2012 | issue= | pages= 139127 | pmid=22811737 | doi=10.1155/2012/139127 | pmc=PMC3395138 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22811737 }} </ref> | |||
[[File:Granuloma_Formation_in_Tuberculosis.jpg|thumb|center|800px|Following inhalation of contaminated aerosols, M. Tuberculosis moves to the lower respiratory tract where it is recognized by alveolar macrophages. This recognition is mediated by a set of surface receptors (see text), which drive the uptake of the bacteria and trigger innate immune signaling pathways leading to the production of various chemokines and cytokines (a). Epithelial cells and neutrophils can also produce chemokines in response to bacterial products (not represented). This promotes the recruitment of other immune cells (more macrophages, dendritic cells, and lymphocytes) to the infection site (b). They organize in a spherical structure with infected macrophages in the middle surrounded by various categories of lymphocytes (mainly CD4+, CD8+, and γ/δ T cells). Macrophages (MP) can fuse to form MGCs or differentiate into lipid-rich foamy cells (FM). B lymphocytes tend to aggregate in follicular-type structures adjacent to the granuloma ((c), see text for details). The bacteria can survive for decades inside the granuloma in a latent state. Due to some environmental (e.g., HIV infection, malnutrition, etc.) or genetic factors, the bacteria will reactivate and provoke the death of the infected macrophages. A necrotic zone (called caseum due to its milky appearance) will develop in the center of the granuloma (d). Ultimately the structure will disintegrate allowing the exit of the bacteria, which will spread in other parts of the lungs, and more lesions will be formed. The infection will also be transmitted to other individuals due to the release of the infected droplets by coughing (e).<ref name="pmid22811737">{{cite journal| author=Silva Miranda M, Breiman A, Allain S, Deknuydt F, Altare F| title=The tuberculous granuloma: an unsuccessful host defense mechanism providing a safe shelter for the bacteria? | journal=Clin Dev Immunol | year= 2012 | volume= 2012 | issue= | pages= 139127 | pmid=22811737 | doi=10.1155/2012/139127 | pmc=PMC3395138 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22811737 }} </ref>]] | [[File:Granuloma_Formation_in_Tuberculosis.jpg|thumb|center|800px|Following inhalation of contaminated aerosols, M. Tuberculosis moves to the lower respiratory tract where it is recognized by alveolar macrophages. This recognition is mediated by a set of surface receptors (see text), which drive the uptake of the bacteria and trigger innate immune signaling pathways leading to the production of various chemokines and cytokines (a). Epithelial cells and neutrophils can also produce chemokines in response to bacterial products (not represented). This promotes the recruitment of other immune cells (more macrophages, dendritic cells, and lymphocytes) to the infection site (b). They organize in a spherical structure with infected macrophages in the middle surrounded by various categories of lymphocytes (mainly CD4+, CD8+, and γ/δ T cells). Macrophages (MP) can fuse to form MGCs or differentiate into lipid-rich foamy cells (FM). B lymphocytes tend to aggregate in follicular-type structures adjacent to the granuloma ((c), see text for details). The bacteria can survive for decades inside the granuloma in a latent state. Due to some environmental (e.g., HIV infection, malnutrition, etc.) or genetic factors, the bacteria will reactivate and provoke the death of the infected macrophages. A necrotic zone (called caseum due to its milky appearance) will develop in the center of the granuloma (d). Ultimately the structure will disintegrate allowing the exit of the bacteria, which will spread in other parts of the lungs, and more lesions will be formed. The infection will also be transmitted to other individuals due to the release of the infected droplets by coughing (e).<ref name="pmid22811737">{{cite journal| author=Silva Miranda M, Breiman A, Allain S, Deknuydt F, Altare F| title=The tuberculous granuloma: an unsuccessful host defense mechanism providing a safe shelter for the bacteria? | journal=Clin Dev Immunol | year= 2012 | volume= 2012 | issue= | pages= 139127 | pmid=22811737 | doi=10.1155/2012/139127 | pmc=PMC3395138 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22811737 }} </ref>]] | ||
| Line 59: | Line 81: | ||
===Molecular Pathogenesis=== | ===Molecular Pathogenesis=== | ||
* | *The [[mycobacterial]] [[antigens]] are presented on thee surfaces of alveolar [[macrophages]] and [[dendritic cells]] through class II [[major histocompatibility complex]]. These [[antigens]] are recognized by [[CD4]] lymphocytes through αβ [[T cell|T-cell]] receptors. Following that, [[CD4+ cell|CD4]] [[Lymphocyte|lymphocytes]] release [[Chemokine|chemokines]] that recruit more [[macrophages]] to the foci of infection. | ||
*Interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α) signaling activates | *[[Interferon gamma (IFN-γ)]] and [[tumor necrosis factor alpha]] ([[Tumor necrosis factor-alpha|TNF-α]]) signaling activates additional [[Macrophage|macrophages]]. <ref name="Tuberculosis">{{cite web | title = Tumor Necrosis Factor alpha| url =http://erj.ersjournals.com/content/36/5/1185.long }}</ref> | ||
*Metalloproteinase converts the transmembrane protein to soluble TNF-α | *[[Metalloproteinase]] converts the transmembrane protein to soluble [[Tumor necrosis factor-alpha|TNF-α]] which interacts with the TNFR1 and TNFR2 receptors inducing [[apoptosis]] through [[caspase]]-dependent pathways | ||
*TNF along | *TNF along side the [[Synergy|synergistic]] action of [[Interferon-gamma|interferon]]-gamma enhances the [[Phagocytosis|phagocytic]] activity of the [[Macrophage|macrophages]] and facilitates the intracellular killing of mycobacteria by [[reactive nitrogen and oxygen]] intermediates. | ||
*Neutralization of the TNF-α activity | *[[Neutralization]] of the TNF-α activity leads to the [[Mycobacterium|mycobacteria]] survival within the [[granuloma]] in latent infection. | ||
*TNF | *TNF activates release of CCL2, CCL3, CCL4, CCL5, CCL8 chemokines and increases CD54 leading to accumulation of [[Immunity (medical)|immune]] cells and it is the main element in the process of [[granuloma]] formation and maintenance. <ref name="Tuberculosis">{{cite web | title = Tumor Necrosis Factor and Tuberculosis| url =http://www.nature.com/jidsp/journal/v12/n1/full/5650027a.htm }}</ref> | ||
* | *The [[immune cells]] release large amounts of lytic enzymes leading to tissue [[necrosis]]. | ||
[[File:TNF alpha.png|thumb|center|500px| <SMALL><SMALL> ''[(http://en.wikipedia.org/wiki/Tumor_necrosis_factor_alpha#mediaviewer/File:TNF_signaling.jpg<nowiki>)]</nowiki>''<ref name="TNF Alpha">{{Cite web | title = TNF Alpha |http://en.wikipedia.org/wiki/Tumor_necrosis_factor_alpha#mediaviewer/File:TNF_signaling.jpg url = }}</ref></SMALL></SMALL>]] | [[File:TNF alpha.png|thumb|center|500px| <SMALL><SMALL> ''[(<nowiki>http://en.wikipedia.org/wiki/Tumor_necrosis_factor_alpha#mediaviewer/File:TNF_signaling.jpg</nowiki><nowiki>)]</nowiki>''<ref name="TNF Alpha">{{Cite web | title = TNF Alpha |http://en.wikipedia.org/wiki/Tumor_necrosis_factor_alpha#mediaviewer/File:TNF_signaling.jpg url = }}</ref></SMALL></SMALL>]] | ||
Once within [[alveolar]] [[macrophages]], ''[[M. tuberculosis]]'' uses multiple mechanisms in order to survive:<ref name="Mandell"></ref> | Once within [[alveolar]] [[macrophages]], ''[[M. tuberculosis]]'' uses multiple mechanisms in order to survive:<ref name="Mandell"></ref> | ||
| Line 80: | Line 102: | ||
==Transmission== | ==Transmission== | ||
After contact with a patient having the active [[Tuberculosis|TB]], and [[inhalation]] of the ''[[M. tuberculosis]],'' the risk of developing active [[tuberculosis]] is low with a life-time risk of about 10%.<ref name="pmid23460002">{{cite journal| author=Glaziou P, Falzon D, Floyd K, Raviglione M| title=Global epidemiology of tuberculosis. | journal=Semin Respir Crit Care Med | year= 2013 | volume= 34 | issue= 1 | pages= 3-16 | pmid=23460002 | doi=10.1055/s-0032-1333467 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23460002 }} </ref> The probability of [[transmission]] between individuals depends on the number of expelled [[infectious]] droplets the ventilation, the duration of the [[Exposure effect|exposure]], [[Immunity (medical)|immunity]], and the [[virulence]] of the ''[[Mycobacterium tuberculosis|M. tuberculosis]] strain''.<ref>{{cite web|url=http://www.mayoclinic.com/health/tuberculosis/DS00372/DSECTION=3|title=Causes of Tuberculosis|accessdate=2007-10-19|date=2006-12-21|last=|first=|publisher=[[Mayo Clinic]]}}</ref> The [[probability]] of transmitting the [[infection]] is highest during the first years of getting the infection. After that, it decreases.<ref name="pmid21420161">{{cite journal| author=Lawn SD, Zumla AI| title=Tuberculosis. | journal=Lancet | year= 2011 | volume= 378 | issue= 9785 | pages= 57-72 | pmid=21420161 | doi=10.1016/S0140-6736(10)62173-3 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21420161 }} </ref> | |||
In rare occasions, the [[Mycobacterium|mycobacteria]] can be [[transmitted]] by other ways apart from the [[Respiratory system|respiratory]] route in which, the formation of foci in the regional [[lymph nodes]] frequently occurs. Those routes include:<ref name="Mandell"></ref> | |||
*[[Skin]] abrasions | *[[Skin]] [[Abrasion|abrasions]] | ||
*[[Oropharynx]] | *[[Oropharynx]] | ||
*[[Intestine]] | *[[Intestine]] | ||
| Line 91: | Line 113: | ||
==Associated Conditions== | ==Associated Conditions== | ||
===AIDS=== | ===AIDS=== | ||
Tuberculosis | <nowiki>*</nowiki>[[Tuberculosis]] influence the progression of [[HIV]] [[viral replication|replication]] leading to an increase in in the [[mortality rate]].<ref name="pmid23425167">{{cite journal| author=Zumla A, Raviglione M, Hafner R, von Reyn CF| title=Tuberculosis. | journal=N Engl J Med | year= 2013 | volume= 368 | issue= 8 | pages= 745-55 | pmid=23425167 | doi=10.1056/NEJMra1200894 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23425167 }} </ref> | ||
<nowiki>*</nowiki>[[HIV]] infected patients, particularly those having low [[CD4|CD4 lymphocytes]] counts, are more likely to develop reactivation of latent [[tuberculosis]]. Moreover, when an individual has been recently infected with ''[[M. tuberculosis]]'', they progress rapidly into active disease.<ref name="Mandell"></ref><ref name="pmid1345800">{{cite journal| author=Daley CL, Small PM, Schecter GF, Schoolnik GK, McAdam RA, Jacobs WR et al.| title=An outbreak of tuberculosis with accelerated progression among persons infected with the human immunodeficiency virus. An analysis using restriction-fragment-length polymorphisms. | journal=N Engl J Med | year= 1992 | volume= 326 | issue= 4 | pages= 231-5 | pmid=1345800 | doi=10.1056/NEJM199201233260404 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1345800 }} </ref><ref name="pmid8280411">{{cite journal| author=Bouvet E, Casalino E, Mendoza-Sassi G, Lariven S, Vallée E, Pernet M et al.| title=A nosocomial outbreak of multidrug-resistant Mycobacterium bovis among HIV-infected patients. A case-control study. | journal=AIDS | year= 1993 | volume= 7 | issue= 11 | pages= 1453-60 | pmid=8280411 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8280411 }} </ref> The correlation between [[AIDS]] and the risk of TB [[infection]] is still not fully understood.<ref name="Mandell"></ref> | |||
Patients with [[AIDS]] are more | Patients with [[AIDS]] are more prone to get [[pulmonary]] and [[extrapulmonary tuberculosis]]. [[Extrapulmonary tuberculosis|Extrapulmonary]] disease in [[HIV AIDS|AIDS]] patients has characteristic [[manifestations]], such as:<ref name="Mandell"></ref> | ||
*Higher | *Higher risk of progression into [[Disseminated TB|disseminated]] disease<ref name="pmid1956280">{{cite journal| author=Shafer RW, Kim DS, Weiss JP, Quale JM| title=Extrapulmonary tuberculosis in patients with human immunodeficiency virus infection. | journal=Medicine (Baltimore) | year= 1991 | volume= 70 | issue= 6 | pages= 384-97 | pmid=1956280 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1956280 }} </ref> | ||
*[[DIC]] and acute [[respiratory failure]] | *[[DIC]] and acute [[respiratory failure]] | ||
*Tuberculous [[pleuritis]] occurs bilaterally | *[[Tuberculosis|Tuberculous]] [[pleuritis]] occurs bilaterally | ||
*Abdominal and mediastinal [[lymphadenopathy]] | *[[Abdominal]] and [[Mediastinum|mediastinal]] [[lymphadenopathy]] frequently occurs | ||
* | *Higher risk of [[Immune reconstitution inflammatory syndrome]] ([[IRIS]])<ref name="pmid18652998">{{cite journal| author=Meintjes G, Lawn SD, Scano F, Maartens G, French MA, Worodria W et al.| title=Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. | journal=Lancet Infect Dis | year= 2008 | volume= 8 | issue= 8 | pages= 516-23 | pmid=18652998 | doi=10.1016/S1473-3099(08)70184-1 | pmc=PMC2804035 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18652998 }} </ref> | ||
*Common [[abscesses]] of:<ref name="Mandell"></ref> | *Common [[abscesses]] of:<ref name="Mandell"></ref> | ||
Revision as of 04:49, 28 February 2021
| https://https://www.youtube.com/watch?v=yR51KVF4OX0%7C350}} |
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Tuberculosis pathophysiology |
|
Risk calculators and risk factors for Tuberculosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2], João André Alves Silva, M.D. [3]
Overview
M. tuberculosis infection occurs through inhalation of aerosols produced by patients with active disease The mycobacterium prefers to live in the upper lung lobes due to the high amount of oxygen. Tuberculosis is a prototypical granulomatous infection. The granuloma encloses mycobacteria and prevents their spreading and facilitates immune immune cell communication. Within the granuloma, CD4 T lymphocytes release cytokines such as interferon gamma that activate local macrophages.
Pathogenesis
Transmission of M. tuberculosis bacterium occurs when individuals with active pulmonary disease cough, speak, sneeze or sing expelling the infectious droplets that can pass to the terminal bronchioles and alveoli then phagocytosed by alveolar macrophages where they can replicate in the endosomes of alveolar macrophages. As a part of the immune response by these macrophages, the alveolar macrophages release cytokines that recruits further macrophages, neutrophils, and monocytes, surrounding the bacilli. Despite having a very low infectious dose (ID<200 bacteria), 90% of the infected immunocompetent individuals are asymptomatic. In most cases, the bacteria may either be eliminated or enclosed within a granuloma. The granuloma is a structured, radial aggregation of macrophages, epithelioid cells, T lymphocytes, B lymphocytes, and fibroblasts that prevents the spreading of mycobacteria and enhances interaction of the immune cells.[1] The primary site of infection in the lung is called the Ghon focus that is mainly located in either the upper part of the lower lobe, or the lower part of the upper lobe.[1][2]
Primary Infection
The infected macrophages are transported through the lymphatics to the regional lymph nodes in the immunocompetent individuals. However, with impaired immune response, these macrophages can pass through the bloodstream to enter any part of the body. Those foci of primary infection usually resolve without any consequences, but they can act as a foci of M. tuberculosis dissemination. There are particular organs that are more susceptible to bacterial replication as well as being potential metastatic foci which include:[1][2]
- Apical-posterior regions of the lungs
- Lymph nodes
- Kidneys
- Vertebral bodies
- Extremities of long bones
- Juxta ependymal meningeal regions
Although TB is a systemic disease and all organs can be affected, the heart, pancreas, skeletal muscles and thyroid are rarely involved.[3] In a few cases, when the infectious dose is high and antigens concentration in the primary focus is high, the immune response and hypersensitivity can lead to necrosis and calcification of this lesion, and these primary calcified foci are then called Ranke complex.[1][4]
Progression of the Primary Infection
Primary foci of infection can enter the large pulmonary lymph nodes. These may lead to:[1]
- Bronchial collapse
- atelectasis
- Bronchial erosion, with more dissemination of infection
*In non-caucasian children, elderly patients and HIV/AIDS, the immune response is impaired, consequently the primary focus of infection can deteriorate into constitute progressive primary disease, with advancing pneumonia.
*In additin,the infection may result in cavity formation with transmission of the infection through the bronchi.[1][5][6]
*In young children, the onset of immune response may be delayed after the bacterial dissemination resulting in military tuberculosis. Bacteria can spread directly from the primary focus, or from the Weigart focus (metastatic focus adjacent to a pulmonary vein) through the blood.[1][7]
*In younger patients, rupture of subpleural foci into the pleural space may occur leading to serofibrinous pleurisy.[1] The most serious site of the M. tuberculosis dissemination is the postero-apical regions of the lung where it can replicate hidden from the immune system.[1]
Immunopathogenesis
There are two types of immune response against tuberculosis that include the innate and acquired immune responses. However, the cell-mediated immune response predominates over the humoral type.
Innate Immune Response
Initially, The immune response generated against M. tuberculosis is minimal, enabling it to replicate inside the alveolar macrophages forming the Ghon focus, or metastatic foci. Recognition and phagocytosis of the M. tuberculosis bacilli by the alveolar macrophages occurs through interaction with certain receptors that are located on the surface of macrophages:[8]
- Toll-like Receptor 2 (TLR2)
- TLR4
- TLR9
- Dectin-1
- DC-SIGN
- Mannose receptor
- Complement receptors
- NOD2
Acquired Immunity and Granuloma Formation
*The granuloma control the infection; however, it enables the mycobacterium to survive inside for a long time.
*It is important to maintain a balance between the pro-inflammatory and anti-inflammatory cytokines released to decrease or control the mycobacterial proliferation.
*TNF-α and IFN-γ stimulate granuloma formation. On the other hand, IL-10 is one of the major negative regulators and inhibitors of granuloma formation.
*The granuloma is structured by blood-derived macrophages (derived from monocytes), epithelioid cells (differentiated macrophages), and multinucleated giant cells (also known as Langhans giant cells), surrounded by T lymphocytes.
*Caseous granulomas are the main characteristic of tuberculosis. The caseous granulomas include epithelioid macrophages and some lymphocytes with a necrotic center. Other types of granuloma include non-necrotizing granulomas, that are mainly formed of macrophages and a few lymphocytes, necrotic neutrophilic granulomas, and completely fibrotic granulomas.[9]
*Several chemokines are involved in granuloma formation released either from the respiratory tract epithelium or the immune cells themselves.
*Interaction with CCR2 receptor with (CCL2/MCP-1, CCL12, and CCL13) is necessary for the initial recruitment of macrophages.
*Macrophages and lymphocytes release a chemokine called osteopontin that enhances the adhesion and recruitment of the immune cells.
*CCL19 and CCL21 are important for recruitment of IFN--producing T cells.
*In TNF-deficient mice, absence of these chemokines as a result of inhibition of the expression of the CC and CXC chemokines prevents the recruitment of other macrophages and T lymphocytes. This finding sheds the light on the role of TNF in granuloma formation.[9]

Molecular Pathogenesis
- The mycobacterial antigens are presented on thee surfaces of alveolar macrophages and dendritic cells through class II major histocompatibility complex. These antigens are recognized by CD4 lymphocytes through αβ T-cell receptors. Following that, CD4 lymphocytes release chemokines that recruit more macrophages to the foci of infection.
- Interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α) signaling activates additional macrophages. [10]
- Metalloproteinase converts the transmembrane protein to soluble TNF-α which interacts with the TNFR1 and TNFR2 receptors inducing apoptosis through caspase-dependent pathways
- TNF along side the synergistic action of interferon-gamma enhances the phagocytic activity of the macrophages and facilitates the intracellular killing of mycobacteria by reactive nitrogen and oxygen intermediates.
- Neutralization of the TNF-α activity leads to the mycobacteria survival within the granuloma in latent infection.
- TNF activates release of CCL2, CCL3, CCL4, CCL5, CCL8 chemokines and increases CD54 leading to accumulation of immune cells and it is the main element in the process of granuloma formation and maintenance. [10]
- The immune cells release large amounts of lytic enzymes leading to tissue necrosis.

Once within alveolar macrophages, M. tuberculosis uses multiple mechanisms in order to survive:[1]
- Urease - prevents acidification of macrophageal lysosomes, limiting action of cellular enzymes
- Secretion of antioxidants, for suppression of reactive oxygen species, such as:
Transmission
After contact with a patient having the active TB, and inhalation of the M. tuberculosis, the risk of developing active tuberculosis is low with a life-time risk of about 10%.[12] The probability of transmission between individuals depends on the number of expelled infectious droplets the ventilation, the duration of the exposure, immunity, and the virulence of the M. tuberculosis strain.[13] The probability of transmitting the infection is highest during the first years of getting the infection. After that, it decreases.[14]
In rare occasions, the mycobacteria can be transmitted by other ways apart from the respiratory route in which, the formation of foci in the regional lymph nodes frequently occurs. Those routes include:[1]
Associated Conditions
AIDS
*Tuberculosis influence the progression of HIV replication leading to an increase in in the mortality rate.[15]
*HIV infected patients, particularly those having low CD4 lymphocytes counts, are more likely to develop reactivation of latent tuberculosis. Moreover, when an individual has been recently infected with M. tuberculosis, they progress rapidly into active disease.[1][16][17] The correlation between AIDS and the risk of TB infection is still not fully understood.[1]
Patients with AIDS are more prone to get pulmonary and extrapulmonary tuberculosis. Extrapulmonary disease in AIDS patients has characteristic manifestations, such as:[1]
- Higher risk of progression into disseminated disease[18]
- DIC and acute respiratory failure
- Tuberculous pleuritis occurs bilaterally
- Abdominal and mediastinal lymphadenopathy frequently occurs
- Higher risk of Immune reconstitution inflammatory syndrome (IRIS)[19]
- Common abscesses of:[1]
Gallery
-
Left lateral margin of a tongue of a tuberculosis patient, which had been retracted in order to reveal the lesion that had been caused by the Gram-positive bacterium Mycobacterium tuberculosisAdapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
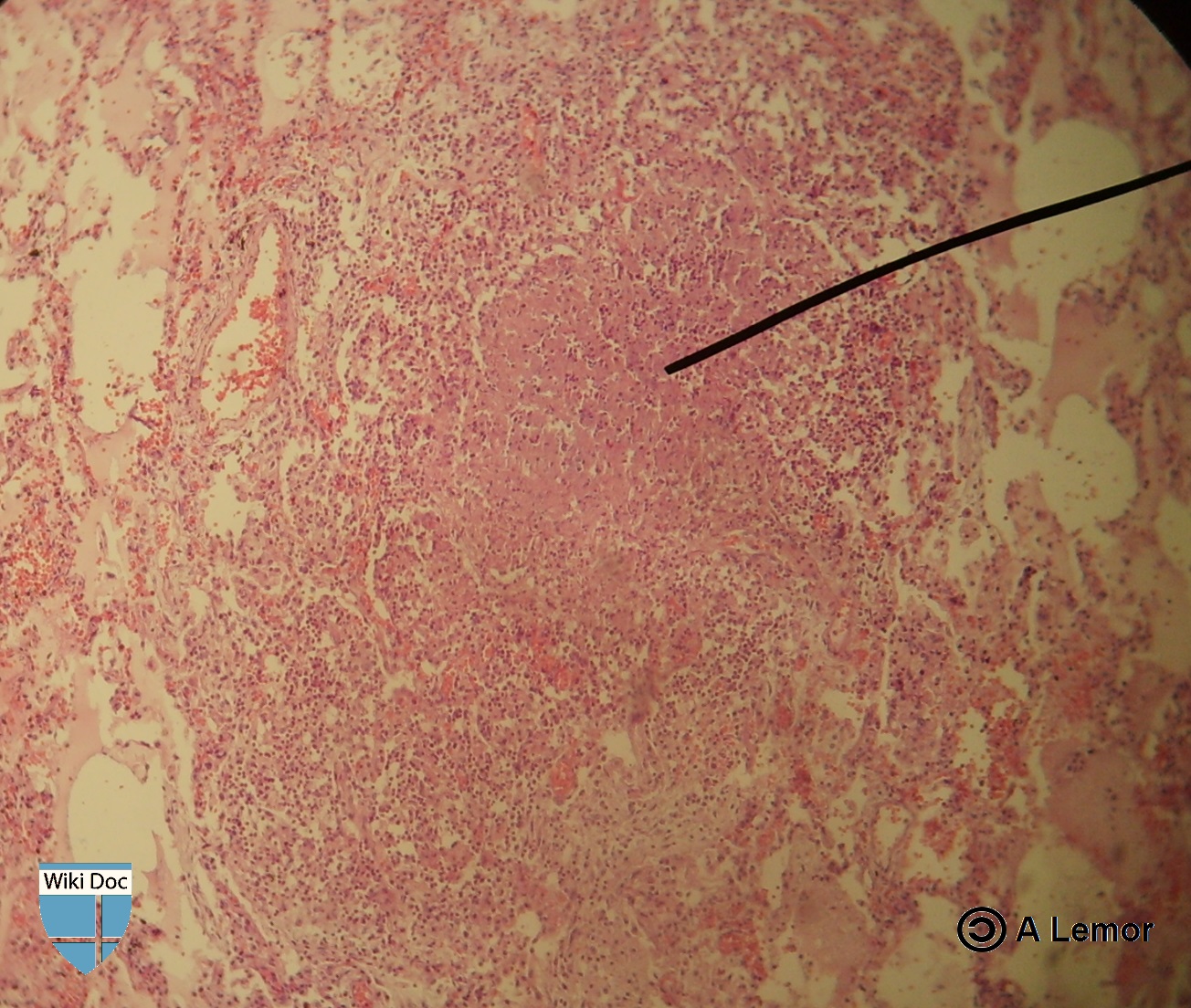
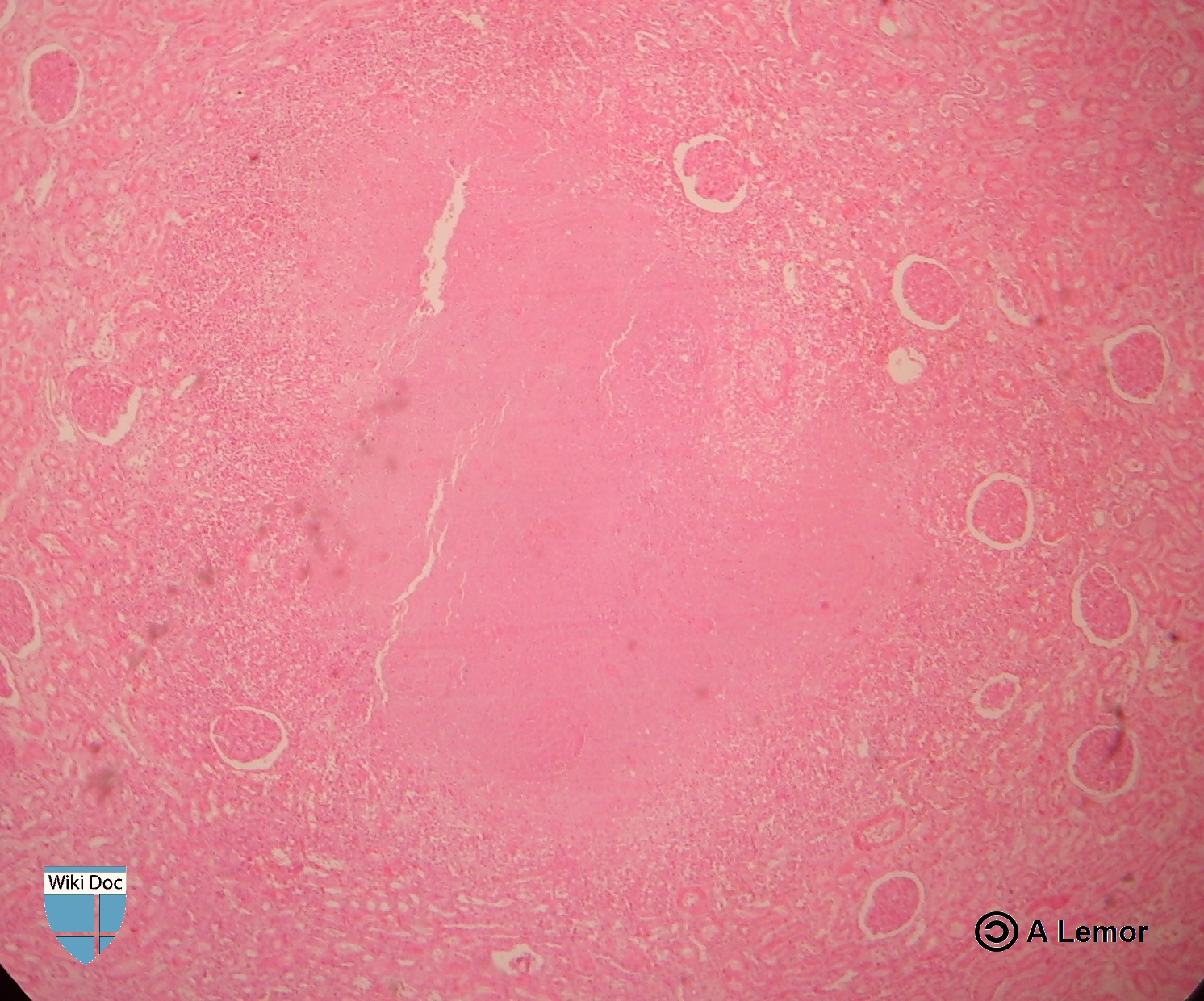
Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection.[ http://phil.cdc.gov/phil/ Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.][20]
-
Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Photomicrograph describing tuberculosis of the placenta.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Histopathology of tuberculosis, endometrium. Ziehl-Neelsen stain.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Histopathology of tuberculosis, placenta.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]
-
Miliar Tuberculosis
-
Renal Tuberculosis lesion
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 0443068399.
- ↑ 2.0 2.1 Herrmann J, Lagrange P (2005). "Dendritic cells and Mycobacterium tuberculosis: which is the Trojan horse?". Pathol Biol (Paris). 53 (1): 35–40. PMID 15620608.
- ↑ Agarwal R, Malhotra P, Awasthi A, Kakkar N, Gupta D (2005). "Tuberculous dilated cardiomyopathy: an under-recognized entity?". BMC Infect Dis. 5 (1): 29. PMID 15857515.
- ↑ Grosset J (2003). "Mycobacterium tuberculosis in the extracellular compartment: an underestimated adversary". Antimicrob Agents Chemother. 47 (3): 833–6. PMID 12604509.
- ↑ Stead WW, Lofgren JP, Warren E, Thomas C (1985). "Tuberculosis as an endemic and nosocomial infection among the elderly in nursing homes". N Engl J Med. 312 (23): 1483–7. doi:10.1056/NEJM198506063122304. PMID 3990748.
- ↑ Murray JF (1990). "Cursed duet: HIV infection and tuberculosis". Respiration. 57 (3): 210–20. PMID 2274719.
- ↑ Kim J, Park Y, Kim Y, Kang S, Shin J, Park I, Choi B (2003). "Miliary tuberculosis and acute respiratory distress syndrome". Int J Tuberc Lung Dis. 7 (4): 359–64. PMID 12733492.
- ↑ Aderem A, Underhill DM (1999). "Mechanisms of phagocytosis in macrophages". Annu Rev Immunol. 17: 593–623. doi:10.1146/annurev.immunol.17.1.593. PMID 10358769.
- ↑ 9.0 9.1 9.2 Silva Miranda M, Breiman A, Allain S, Deknuydt F, Altare F (2012). "The tuberculous granuloma: an unsuccessful host defense mechanism providing a safe shelter for the bacteria?". Clin Dev Immunol. 2012: 139127. doi:10.1155/2012/139127. PMC 3395138. PMID 22811737.
- ↑ 10.0 10.1 "Tumor Necrosis Factor alpha".
- ↑ "TNF Alpha". Missing or empty
|url=(help) - ↑ Glaziou P, Falzon D, Floyd K, Raviglione M (2013). "Global epidemiology of tuberculosis". Semin Respir Crit Care Med. 34 (1): 3–16. doi:10.1055/s-0032-1333467. PMID 23460002.
- ↑ "Causes of Tuberculosis". Mayo Clinic. 2006-12-21. Retrieved 2007-10-19.
- ↑ Lawn SD, Zumla AI (2011). "Tuberculosis". Lancet. 378 (9785): 57–72. doi:10.1016/S0140-6736(10)62173-3. PMID 21420161.
- ↑ Zumla A, Raviglione M, Hafner R, von Reyn CF (2013). "Tuberculosis". N Engl J Med. 368 (8): 745–55. doi:10.1056/NEJMra1200894. PMID 23425167.
- ↑ Daley CL, Small PM, Schecter GF, Schoolnik GK, McAdam RA, Jacobs WR; et al. (1992). "An outbreak of tuberculosis with accelerated progression among persons infected with the human immunodeficiency virus. An analysis using restriction-fragment-length polymorphisms". N Engl J Med. 326 (4): 231–5. doi:10.1056/NEJM199201233260404. PMID 1345800.
- ↑ Bouvet E, Casalino E, Mendoza-Sassi G, Lariven S, Vallée E, Pernet M; et al. (1993). "A nosocomial outbreak of multidrug-resistant Mycobacterium bovis among HIV-infected patients. A case-control study". AIDS. 7 (11): 1453–60. PMID 8280411.
- ↑ Shafer RW, Kim DS, Weiss JP, Quale JM (1991). "Extrapulmonary tuberculosis in patients with human immunodeficiency virus infection". Medicine (Baltimore). 70 (6): 384–97. PMID 1956280.
- ↑ Meintjes G, Lawn SD, Scano F, Maartens G, French MA, Worodria W; et al. (2008). "Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings". Lancet Infect Dis. 8 (8): 516–23. doi:10.1016/S1473-3099(08)70184-1. PMC 2804035. PMID 18652998.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 20.8 "Public Health Image Library (PHIL), Centers for Disease Control and Prevention".
![Left lateral margin of a tongue of a tuberculosis patient, which had been retracted in order to reveal the lesion that had been caused by the Gram-positive bacterium Mycobacterium tuberculosisAdapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/0/09/TB1.jpg)
![Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection.[ http://phil.cdc.gov/phil/ Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.][20]](/images/e/ed/TB2.jpg)
![Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/7/79/Leprosy-35.jpg)
![Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/6/60/Leprosy-36.jpg)
![Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/9/93/Leprosy-37.jpg)
![Light photomicrograph revealing some of the histopathologic cytoarchitectural characteristics seen in a mycobacterial skin infection Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/b/b5/Leprosy-38.jpg)
![Photomicrograph describing tuberculosis of the placenta.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/b/be/TB3.jpg)
![Histopathology of tuberculosis, endometrium. Ziehl-Neelsen stain.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/d/dd/TB4.jpg)
![Histopathology of tuberculosis, placenta.Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.[20]](/images/9/97/TB5.jpg)