|
|
| Line 1: |
Line 1: |
| [[Image:TSC1.jpg|thumb|300px|Tuberous sclerosis skin lesion - Angiofibromas - image taken from: www.atlasdermatologico.com.br]]
| |
| [[Image:Ts22.jpg|thumb|300px|Tuberous sclerosis skin lesion - Ash-leaf spot - image taken from: www.atlasdermatologico.com.br]]
| |
| [[Image:TSC3.jpg|thumb|300px|Tuberous sclerosis skin lesion - Ungual fibroma - image taken from: www.atlasdermatologico.com.br]]
| |
|
| |
| ==Overview== | | ==Overview== |
| '''Tuberous sclerosis complex''' ('''TSC'''), is a rare autosomal dominant congenital disorder that affects multiple organ systems and is characterized by an abnormal growth of ectodermal and mesodermal cells that causes [[benign tumor|non-cancerous tumours]] to grow in the [[human brain|brain]] and on other vital organs such as the [[kidney]]s, [[human heart|heart]], [[human liver|liver]], [[human eye|eye]]s, [[human lung|lung]]s, and [[human skin|skin]]. <ref name=":2">Henske, Elizabeth P., et al. "Tuberous sclerosis complex." ''Nature reviews Disease primers'' 2.1 (2016): 1-18.</ref>
| | Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes [[inflammation]] of some parts of the body like [[heart]], [[blood vessels]], [[Kidney|kidneys]], digestive system, [[brain]], [[skin]], or [[Eye|eyes]]. According to recent evidence, it is suggested that children with MIS-C had antibodies against [[COVID-19]] suggesting children had [[COVID-19]] infection in the past. This syndrome appears to be similar in presentation to [[Kawasaki disease]], hence also called Kawasaki -like a disease. It also shares features with s[[Streptococcal toxic shock syndrome|taphylococcal and streptococcal toxic shock syndromes]], [[Sepsis|bacterial sepsis]], and macrophage activation syndromes. |
| | | ==Historical Perspective== |
| A combination of symptoms may include [[seizure]]s, [[intellectual disability]], [[Specific developmental disorder|developmental delay]], behavioral problems, skin abnormalities, and lung and kidney disease. TSC is caused by a [[mutation]] of either of two [[gene]]s, ''[[TSC1]]'' and ''[[TSC2]]'', which code for the [[protein]]s [[hamartin]] and [[tuberin]], respectively. These proteins act as [[Tumor suppressor gene|tumor growth suppressors]], agents that regulate cell proliferation and differentiation.<ref name="TSFactSheet">{{cite web|url=https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Tuberous-Sclerosis-Fact-Sheet|title=Tuberous Sclerosis Fact Sheet|publisher=National Institute of Neurological Disorders and Stroke|accessdate=16 December 2018|date=2018-07-06}}</ref>
| |
|
| |
|
| The disease presents with a myriad of symptoms, having been described by multiple doctors throughtout the 19th century and called by many different names, but it is now called '''tuberous sclerosis complex''', and the relationship between benign brain tumors and the symptoms of the disease was [[timeline of tuberous sclerosis|first described]] by [[Désiré-Magloire Bourneville]] in 1880. <ref name=":0">Morgan, J. Elizabeth, and Francis Wolfort. "The early history of tuberous sclerosis." Archives of dermatology 115.11 (1979): 1317-1319.</ref>
| | * Reports of a new febrile pediatric entity began to appear in late April 2020 during the COVID-19 pandemic in the Western Europe, characterized by systemic hyperinflammation, abdominal pain with gastrointestinal symptoms and multiorgan involvement affecting specially the myocardium causing cardiogenic shock which reminded the physicians of Kawasaki disease;<ref name=":0">Shulman, Stanford T. "Pediatric coronavirus disease-2019–associated multisystem inflammatory syndrome." ''Journal of the Pediatric Infectious Diseases Society'' (2020).</ref> |
| | * Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the COVID-19 pandemic;<ref name=":0" /> |
| | * A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of inflammation such as ferritin, D-dimers, triglycerides, elevated cardiac enzymes, high NT-pro-BNP levels and troponin, being empirically treated with IVIG;<ref name=":0" /> |
| | * In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with Kawasaki's Syndrome, noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the macrophage activation syndrome and not Kawasaki's disease.<ref name=":0" /> |
|
| |
|
| ==Historical Perspective== | | ==Classification of Disease Severity of MIS-C == |
| Tuberous Sclerosis was described as a specific disease in the 19th century, being initially referred to adenoma sebaceum, epiloia, Pringle's disease or Bourneville's disease. Rayer, a French dermatologist, was the one to first describe the disease and the fibrovascular papules that characterize it, making illustrations of it. He described two cases of tuberous sclerosis in patients who had the nasolabial papular eruption with telangiectasias at the base. In 1850 the first written report of tuberous sclerosis appeared in "Vitiligoidea", published by Addison and Gull. It was not recognized as a distinct disease but was classified as "vitiligoidea tuberosa". In 1862, von Recklinghausen reported a tumor of the heart found in a newborn during autopsy, and by that he is credited to be the first that described the microscopic appearance of tuberous sclerosis. Bourneville in 1880, a French neurologist, described the case of a girl who presented at the age of 3 with facial eruption and died at 15 years of age due to epilepsy, which complicated with pneumonia and inanition. He found brain and kidney tumors on the autopsy which were correctly believed to be the cause of her seizures and mental retardation. In 1911, E. B. Sherlock, superintendent of Belmont Asylum of Idiots, London, coined the word "epiloia" that indicated a clinical triad of epilepsy, low intelligence and adenoma sebaceum.<ref name=":0" />
| |
|
| |
|
| In 2002, treatment with [[rapamycin]] was found to be effective at shrinking tumours in animals. This has led to human trials of rapamycin as a drug to treat several of the tumors associated with TSC.<ref name="Rott2005">{{cite web |url = http://www.tsdev.de/92001/Uploaded/hhehn%7Cgeschichte_der_tsc2005.pdf |format = PDF |title = Zur Geschichte der Tuberösen Sklerose (The History of Tuberous Sclerosis) |accessdate = 8 January 2007 |vauthors = Rott HD, Mayer K, Walther B, Wienecke R |date = March 2005 |publisher = Tuberöse Sklerose Deutschland e.V |language = German |deadurl = yes |archiveurl = https://web.archive.org/web/20070315134445/http://www.tsdev.de/92001/Uploaded/hhehn%7Cgeschichte_der_tsc2005.pdf |archivedate = 15 March 2007 |df = dmy-all}}</ref>
| | *'''Mild Disease''' |
| | | *Children with MIS-C fall under this category who- |
| ==Classification==
| | **require minimal to no respiratory support. |
| There is no established system for the classification of tuberous sclerosis.
| | **minimal to no organ injury |
| | **normotensive |
| | ** Do not meet the criteria for ICU admission. |
| | *'''Severe Disease''' |
| | *Children with MIS-C fall under this category who- |
| | **have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation). |
| | **have a mild-severe organ injury and ventricular dysfunction. |
| | **have a vasoactive requirement. |
| | **meet the criteria for ICU admissions |
|
| |
|
| ==Pathophysiology== | | ==Pathophysiology== |
|
| |
|
| Patients with tuberous sclerosis have loss-of-function germline mutations in both alleles of the following tumor suppressor genes: TSC1 or TSC2. One third of the mutations is inherited, two thirds are de novo mutations. The mutations causes the loss of one allele, but as long as the second one remains intact, the cell won't present any metabolic change. When there is a second TSC1 or TSC2 mutation, which typically occurs in multiple cells over a person's lifetime, then the disease starts to manifest (fitting the "two-hit" tumor-suppressor gene model, with the germline mutation inactivating one gene and then a somatic event inactivating the remaining other one). TSC1 codes for a protein called hamartin, and TSC2 codes for a protein called tuberin. They belong to a protein complex that inhibits the mammalian target of rapamycin (mTOR) complex 1 via RAS homologue enriched in brain (RHEB) which regulates cell growth. In a normal patient, RHEB activates mTORC1 when bound to GTP, but in TSC there is a hyperactivarion of RHEB and consequently of mTORC1. mTOR regulates cellular proliferation, autophagy, growth and protein and lipid synthesis and it enhances protein translation when activated, reprograming the cell metabolism, which increases cell proliferation but also may make it vulnerable to death in nutrient-restricted media.
| | * The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement. |
| Besides the TSC-RHEB-mTORC1 pathway, there is evidence of alternate pathways also having a role in the disease that are mTORC1 independent, but they are currently under investigation.<ref>NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020</ref><ref name=":2" />
| | *Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C). |
| ==Causes==
| | * It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract. |
| Loss of function mutation of the genes TSC1 and TSC2 which are responsible for the production of hamartin and tuberin. These proteins regulate the cell cycle. Damage to this pathway leads to a very variable presentation of benign tumors in multiple systems.
| |
| ''TSC1'' and ''TSC2'' are both [[tumor suppressor gene]]s that function according to [[Knudson hypothesis|Knudson's "two hit" hypothesis]]. That is, a second random mutation must occur before a tumor can develop. This explains why, despite its high [[penetrance]], TSC has wide [[expressivity (genetics)|expressivity]].<ref name=":2" />
| |
| ==Differentiating Tuberous Sclerosis from other Diseases==
| |
| Tuberous sclerosis must be differentiated from other diseases that cause myxoma or other benign tumors and/or seizures, such as Sturge Weber, hypomelanosis of Ito, Birt-Hogg-Dube syndrome, multiple endocrine neoplasia and various seizures disorders.<ref>NORD: National Organization for Rare Diseases - Tuberous Sclerosis - available at: https://rarediseases.org/rare-diseases/tuberous-sclerosis/#:~:text=Examples%20of%20such%20disorders%20include,be%20differentiated%20from%20tuberous%20sclerosis. accessed at 06/12/2020</ref>
| |
|
| |
|
| ==Epidemiology and Demographics== | | ==Differentiating Any Disease from other disease== |
| Tuberous sclerosis complex affects about 1 in 6,000 people, occurring in all races and ethnic groups, and in both genders. Prior to the invention of CT scanning to identify the nodules and tubers in the brain, the prevalence was thought to be much lower and the disease associated with those people diagnosed clinically with learning disability, seizures, and facial angiofibroma. Whilst still regarded as a rare disease, TSC is common when compared to many other genetic diseases, with at least 1 million individuals worldwide.<ref>Curatolo, Paolo, ed. ''Tuberous sclerosis complex: from basic science to clinical phenotypes''. Cambridge University Press, 2003.</ref><ref>NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020</ref>
| |
|
| |
|
| ==Risk Factors== | | * Children who met criteria for PIMS-TS presented features that overlapped with the ones seen on Kawasaki Disease and Toxic Shock Syndrome.<ref name=":1">Whittaker E, Bamford A, Kenny J, et al; PMIS-TS Study Group; EUCLIDS and PERFORM Consortia. Clinical and laboratory characteristics of 58 children with a pediatric multisystem inflammatory syndrome temporally associated with SARSCoV-2. JAMA. doi:10.1001/jama.2020.10369</ref> |
| There are no established environmental risk factors for tuberous sclerosis. One third of the cases are familial, so family history can be a risk factor for the disease.<ref name=":2" />
| | * PCR tests for SARS-CoV-2 were positive in the minority of cases (26%), while the IgG antibody was positive in most patients (87%)<ref name=":1" /> and it remains as the preferred laboratory for differentiating such diseases; |
|
| |
|
| ==Screening==
| | {| class="wikitable" |
| As it is a rare disease, screening is not recommended.
| | |+Summary of laboratory parameters of a PIMS-TS cohort compared with the historic cohorts of Kawasaki Disease, Kawasaki Disease Shock Syndrome and Toxic Shock Syndrome<ref name=":1" /> |
| ==Natural History, Complications, and Prognosis==
| | !Parameters |
| ===Skin===
| | !Pediatric Inflammatoy Multisystem Syndrome Temporally associated with SARS-CoV-2 Infection (PIMS-TS) |
| Symptoms develop in almost all patients with TSC and include ungual fibromas, facial angiofibromas (may demand treatment and may worsen with UV exposure), shagreen patches (oval-shaped lesions, generally skin-colored but can be sometimes pigmented, may be crinkled or smooth), focal hypopigmented macules (ash-leaf spots), dental enamel pits (present in 100% of the patients), oral fibromas, retinal astrocytic hamartomas (tumors of the retinal nerve), retinal achromic patches (light or dark spots on the eye).<ref name=":2" />
| | !Kawasaki Disease (KD) |
| | | !Kawasaki Disease Shock (KDS) |
| ===Renal===
| | !Toxic Shock Syndrome (TSS) |
| TSC leads to the formation of renal angiomyolipomas (present in 60-80% of the TSC patients), benign tumors composed of abnormal vessels, smooth-muscle cells and fat cells which may cause hematuria. These tumors can be detectable in early childhood by MRI, CT or ultrasound. Although benign, in TSC they are commonly multiple and bilateral. Angiomyolipomas larger than 4 cm are at risk for potentially catastrophic hemorrhage either spontaneously or with minimal trauma. Patients may also develop epithelial cysts, polycystic kidney disease (as 2-3% of the patients carries a deletion that affects both TSC2 gene and one of the genes that lead to autosomal dominant polycystic kidney disease) and renal-cell carcinomas that may be diagnosed at a younger age (mean 28 years).<ref name="PMID17005952" /><ref name=":2" /> Patients ≥18 years may have higher rates of chronic kidney disease, hematuria, kidney failure, embolization (EMB), and partial and complete nephrectomy compared to patients <18 years.<ref>Song, Xue, et al. "Natural history of patients with tuberous sclerosis complex related renal angiomyolipoma." ''Current medical research and opinion'' 33.7 (2017): 1277-1282.</ref>
| |
| | |
| ===Pulmonary===
| |
| Lymphangiomyomatosis affects mostly women and is a proliferation of smooth-muscle cells that may result in cystic changes in the lungs. Recent genetic analysis has shown that the proliferative bronchiolar smooth muscle in TSC-related lymphangioleiomyomatosis is monoclonal metastasis from a coexisting renal angiomyolipoma. Cases of TSC-related lymphangioleiomyomatosis recurring following lung transplant have been reported.<ref>Henske EP (December 2003). "Metastasis of benign tumor cells in tuberous sclerosis complex". ''Genes, Chromosomes & Cancer''. '''38''' (4): 376–81. [[Digital object identifier|doi]]:10.1002/gcc.10252. <nowiki>PMID 14566858</nowiki>.</ref> Diagnosed mostly during early adulthood, may cause pneumothorax. Multifocal micronodular pneumocyte hyperplasia can occur in both men and women and are mostly asymptomatic.<ref name="PMID17005952" /><ref name=":2" />
| |
| | |
| In 2020 a paper showed that epilepsy remission by appropriate treatment in early life can possibly prevent autism and intellectual disability.<ref>Gupta, Ajay, et al. "Epilepsy and neurodevelopmental comorbidities in tuberous sclerosis complex: a natural history study." ''Pediatric Neurology'' (2020).</ref>
| |
| | |
| ===Neurologic===
| |
| These manifestations are one of the major causes of morbidity in patients with TSC. TSC may cause epilepsy, which is the most common neurological presentation occurring in 70-80% of patients and may complicate with infantile spasms, a severe form of epileptic syndrome. If epilepsy presents with an early onset t is associated with cognitive disabilities, which are also very prevalent in such patients. Neuropsychiatric disorders are present in two-thirds of the patients and anxiety is one of the most common presentations. Autism is one possible manifestation and is especially associated with cerebral cortical tubers. It consists of neurologic tissue that grows in a different pattern, losing the normal six-layered cortical structure, with dysmorphic neurons, large astrocytes and giant cells. Some patients may also present with subependymal giant cell astrocytomas, which may cause obstructive hydrocephalus. Risk of such benign tumors decreases after age of 20.<ref name="PMID17005952" /><ref name=":2" />
| |
| | |
| ===Cardiovascular===
| |
| Rhabdomyomas may be present, being intramural or intracavitary in its distribution along the myocardium. May be detected in utero on fetuses and is associated with cardiac failure. Often disappear spontaneously in later life.<ref name=":2" /> 80% of children under two-years-old with TSC have at least one rhabdomyoma, and about 90% of those will have several.<ref>Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK (November 2014). "Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group". ''Journal of the American Heart Association''. '''3''' (6): e001493. [[Digital object identifier|doi]]:10.1161/JAHA.114.001493. [[PubMed Central|PMC]] 4338742. <nowiki>PMID 25424575</nowiki>.</ref>
| |
| ==Diagnosis==
| |
| Tuberous sclerosis complex is diagnosed if a set of diagnostic criteria are met. These criteria include major and minor features. If a case meets the clinical diagnostic criteria, then it is performed a genetic molecular testing which is seem mostly as corroborative. Most of the patients seek medical assistance due to their dermatologic lesions or seizures but for making this diagnosis an evaluation that assesses all the clinical features of the tuberous sclerosis complex is necessary, as these manifestations have variable penetrance.<ref name="PMID17005952" /> The latest diagnostic criteria was developed by the 2012 International Tuberous Sclerosis Complex Consensus Conference, and it is showed at the table below:
| |
| | |
| {| class=wikitable width="75%" style="margin: 1em auto 1em auto"
| |
| |+Diagnostic Criteria for Tuberous Sclerosis Complex<ref name="TSCDiagnosis">{{cite journal | vauthors = Northrup H, Krueger DA | title = Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference | journal = Pediatric Neurology | volume = 49 | issue = 4 | pages = 243–54 | date = October 2013 | pmid = 24053982 | pmc = 4080684 | doi = 10.1016/j.pediatrneurol.2013.08.001 }}</ref>
| |
| ! colspan="5" width="100%" | Major Features | |
| |- | | |- |
| ! width="2%" |
| | |'''Age (median, IQR)''' |
| ! width="12%" | Location
| | |9 (5.7-14) |
| ! width="42%" | Sign
| | |2.7 (1.4-4.7) |
| ! width="22%" | Onset<ref name="PMID17005952">{{cite journal | vauthors = Crino PB, Nathanson KL, Henske EP | title = The tuberous sclerosis complex | journal = The New England Journal of Medicine | volume = 355 | issue = 13 | pages = 1345–56 | date = September 2006 | pmid = 17005952 | doi = 10.1056/NEJMra055323 }}</ref>
| | |3.8 (0.2-18) |
| ! width="22%" | Note
| | |7.38 (2.4-15.4) |
| |- | | |- |
| ! 1
| | |'''Total white cell count (*10^9/L)''' |
| | Skin | | |17 (12-22) |
| | Hypomelanotic [[macules]] | | |13.4 (10.5-17.3) |
| | Infant – child | | |12.1 (7.9-15.5) |
| | At least three, at least 5 mm in diameter. | | |15.6 (7.5-20) |
| |- | | |- |
| ! 2
| | |'''Neutrophil count (*10^9/L)''' |
| | Head | | |13 (10-19) |
| | Facial angiofibromas or fibrous cephalic plaque | | |7.2 (5.1-9.9) |
| | Infant – adult | | |5.5 (3.2-10.3) |
| | At least three angiofibromas | | |16.4 (12-22) |
| |- | | |- |
| ! 3
| | |'''Lymphocyte count (*10^9/L)''' |
| | Fingers and toes | | |0.8 (0.5-1.5) |
| | Ungual [[fibroma]] | | |2.8 (1.5-4.4) |
| | Adolescent – adult | | |1.6 (1-2.5) |
| | At least two | | |0.63 (0.41, 1.13) |
| |- | | |- |
| ! 4
| | |'''Hemoglobin (g/L)''' |
| | Skin | | |92 (83-103) |
| | Shagreen patch ([[connective tissue]] [[nevus]]) | | |111.0 (105-119) |
| | Child | | |107 (98-115) |
| | | | |114 (98-130) |
| |- | | |- |
| ! 5
| | |'''Platelet number (10^9/L)''' |
| | Eyes | | |151 (104-210) |
| | Multiple [[retinal]] [[nodule (medicine)|nodular]] [[hamartomas]] | | |365.0 (288-462) |
| | Infant | | |235 (138-352) |
| | | | |155 (92- 255) |
| |- | | |- |
| ! 6
| | |'''C-reactive protein (mg/L)''' |
| | Brain | | |229 (156-338) |
| | [[cortex (anatomy)|Cortical]] dysplasias (includes tubers and cerebral white matter radial migration lines) | | |67.0(40-150) |
| | Fetus | | |193 (83-237) |
| | | | |201 (122, 317) |
| |- | | |- |
| ! 7
| | |'''ALT (IU/L)''' |
| | Brain | | |42 (26-95) |
| | [[Subependymal zone|Subependymal]] [[nodule (medicine)|nodule]] | | |42.0 (24-112) |
| | Child – adolescent | | |73 (34-107) |
| | | | |30.00 (22.10, 49.25) |
| |- | | |- |
| ! 8
| | |'''Albumin (g/L)''' |
| | Brain | | |24 (21-27) |
| | [[Subependymal zone|Subependymal]] giant cell [[astrocytoma]] | | |38.0 (35-41) |
| | Child – adolescent | | |30 (27-35) |
| | | | |27.00 (21.00, 31.00) |
| |- | | |- |
| ! 9
| | |'''Ferritin (ug/L)''' |
| | Heart | | |610 (359-1280) |
| | Cardiac [[rhabdomyoma]] | | |200 (143-243) |
| | Fetus | | |301 (228-337) |
| | | | | - |
| |- | | |- |
| ! 10
| | |'''NT-Pro-BNP (pg/ml)''' |
| | Lungs | | |788 (174-10548) |
| | [[Lymphangioleiomyomatosis]] | | |41 (12-102) |
| | Adolescent – adult | | |396 (57-1520) |
| | | | | - |
| |- | | |- |
| ! 11
| | |'''Troponin (ng/L)''' |
| | Kidneys | | |45 (8-294) |
| | Renal [[angiomyolipoma]] | | |10.0 (10-20) |
| | Child – adult | | |10 (10-30) |
| | At least two. Together, '''10''' and '''11''' count as one major feature. | | | - |
| |- | | |- |
| ! colspan="5" width="100%" | Minor Features
| | |'''D-dimer (ng/ml)''' |
| |-
| | |3578 (2085- 8235) |
| ! width="2%" |
| | |1650 (970-2660) |
| ! width="12%" | Location
| | |2580 (1460- 2990) |
| ! width="42%" | Sign
| | | - |
| ! width="44%" colspan="2" | Note
| |
| |-
| |
| ! 1
| |
| | Skin
| |
| | "Confetti" skin lesions
| |
| | colspan="2" |
| |
| |- | |
| ! 2
| |
| | Teeth
| |
| | Dental enamel pits
| |
| | colspan="2" | At least three
| |
| |- | |
| ! 3
| |
| | Gums
| |
| | Intraoral fibromas
| |
| | colspan="2" | At least two
| |
| |- | |
| ! 4
| |
| | Eyes
| |
| | Retinal achromic patch
| |
| | colspan="2" |
| |
| |- | |
| ! 5
| |
| | Kidneys
| |
| | Multiple [[renal cyst]]s
| |
| | colspan="2" |
| |
| |- | |
| ! 6
| |
| | Liver, spleen and other organs
| |
| | Nonrenal [[hamartoma]]
| |
| | colspan="2" |
| |
| |} | | |} |
| | <br /> |
| | ==Epidemiology and Demographics== |
|
| |
|
| TSC can be first diagnosed at any stage of life. Prenatal diagnosis is possible by chance if heart tumours are discovered during routine [[ultrasound]]. In infancy, white patches on the skin may be noticed, or the child may present with epilepsy, particularly infantile spasms, or developmental delay may lead to neurological tests. In childhood, behavioural problems and [[autism spectrum disorder]] may also lead to a clinical investigation and a diagnosis. During adolescence it is usually that skin problems appear while in adulthood, kidney and lung problems may become evident. An individual may also be diagnosed at any time as a result of genetic testing of family members of another affected person.<ref name="NHSBirmingham">{{cite web|url=https://www.uhb.nhs.uk/tuberous-sclerosis-complex.htm|title=Tuberous Sclerosis Complex|accessdate=16 December 2018|publisher=University Hospitals Birmingham NHS Foundation Trust}}</ref>
| | *According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20. |
| ===History and Symptoms===
| | *80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation. |
| The most common symptoms of tuberous sclerosis are due to the growth of the already disclosed benign tumors. Tumors in the CSN may cause epilepsy, autism and children may also present with cognitive disabilities. Tumors in the kidneys may compromise renal function and metastasize to the lungs, which in most cases is asymptomatic. Tumors in the heart may compromise heart function, but they tend to spontaneously disappear later in life.
| | *4% of the children required extracorporeal membrane oxygenation. |
| ===Physical Examination===
| | *The mortality rate among 186 children with MIS-C was 2%. |
| Physical examination of patients with tuberous sclerosis is a very rich one due to the different skin lesions that the disease can cause and it is usually remarkable for dental enamel pits (present in 100% of the patients)<ref name=":2" />,hypomelanotic macules, shagreen patches, and forehead plaques.<ref name="TSC-diagnosis">{{cite book | veditors = Curatolo P | title = Tuberous Sclerosis Complex: From Basic Science to Clinical Phenotypes | year = 2003 | isbn = 978-1-898683-39-1 | oclc = 53124670 | chapter = Diagnostic Criteria | series = International review of child neurology | location = London | publisher = Mac Keith Press }}</ref>
| |
| | |
| ===Laboratory Findings===
| |
| There are no typical diagnostic laboratory findings associated with tuberous sclerosis. Patients may present with elevated BUN or creatinine if their renal angiomyolipomas compromise renal function or if they also present with autosomal dominant polycystic kidney disease.
| |
| | |
| ===Electrocardiogram===
| |
| There are no ECG findings associated with tuberous sclerosis.
| |
| | |
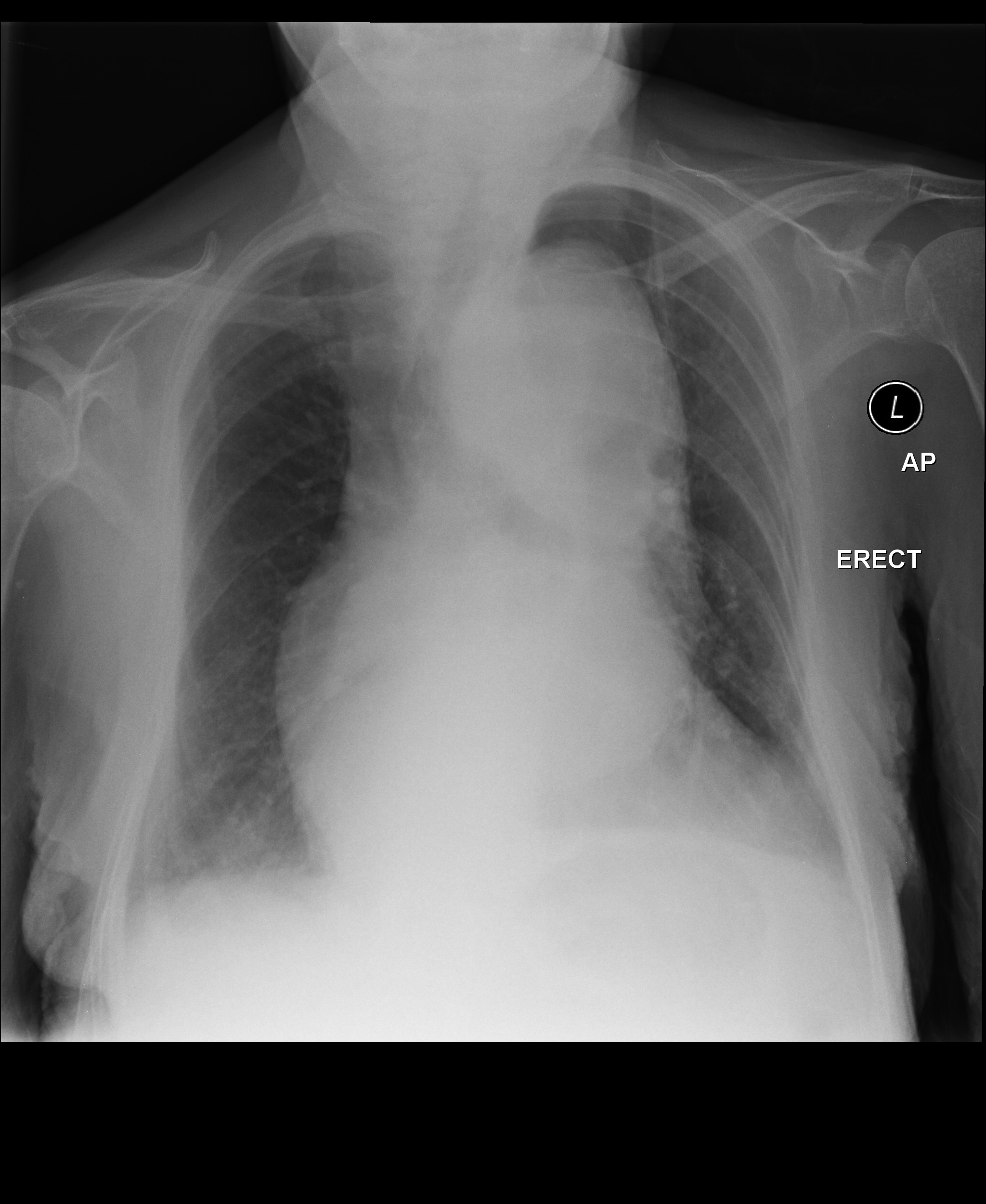
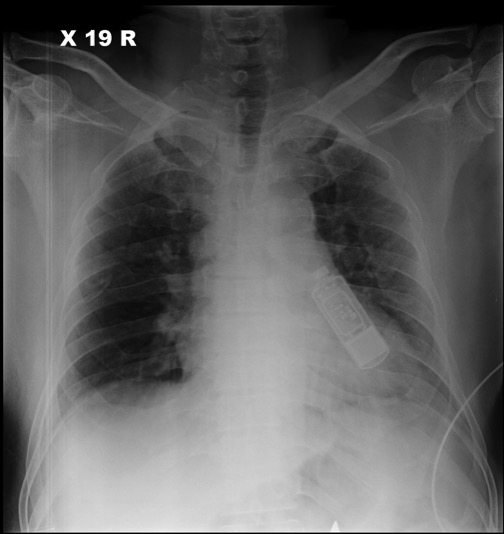
| ===X-ray===
| |
| There are no typical x-ray findings associated with tuberous sclerosis, but patients may present with pneumothorax and/or chylous pleural effusions due if they develop lymphangioleiomyomatosis.
| |
| | |
| ===Echocardiography or Ultrasound===
| |
| Echocardiography/ultrasound may be helpful raising the suspicion of tuberous sclerosis. Echocardiographs can detect cardiac rhabdomyomas, present in more than 80% of the children with TSC. Ultrasound can detect hepatic angiomyolipomas, renal angiomyolipomas (present in 55-75% of patients) and renal cysts (present in 18-55% of the patients).<ref name=":1">Radiopaedia - tuberous sclerosis - available at: <nowiki>https://radiopaedia.org/articles/tuberous-sclerosis</nowiki> accessed at 06/15/2020</ref>
| |
| | |
| ===CT scan===
| |
| CT scan may be helpful in the diagnosis of tuberous sclerosis. It can diagnose cortical or subependymal tubers and white matter abnormalities, subependymal hamartomas, subependymal giant cell astrocytomas, renal angiomyolipomas, renal cysts, renal cell carcinoma (associated with tuberous sclerosis), retroperitoneal lymphangiomyomatosis, gastrointestinal polyps, pancreatic neuroendocrine tumors, lymphangioleiomyomatosis, multifocal micronodular pneumocyte hyperplasia and cardiac rhabdomyomas.<ref name=":1" />
| |
|
| |
|
| ===MRI===
| | '''Age''' |
| MRI may be helpful in the diagnosis of tuberous sclerosis as it can find the same abnormalities found on CT scan which are described above, some of them with much more detail, but it is especially useful for evaluating white matter changes seen in the disease.<ref name=":1" />
| |
|
| |
|
| ===Other Imaging Findings===
| | *Among the 186 children with MIS-C distribution of age group was |
| There are no other imaging findings associated with tuberous sclerosis.
| | **<1yr-7% |
| | ** 1-4yr-28% |
| | **5-9yr-25% |
| | **10-14yr-24% |
| | ** 15-20yr-16%. |
|
| |
|
| ===Other Diagnostic Studies===
| | '''Gender''' |
| Genetic testing may be helpful in the diagnosis of tuberous sclerosis but some patients may not have detectable genetic mutations on the test and still have the disease. It is considered to be a corroborative test.
| |
|
| |
|
| ==Treatment==
| | *Among the 186 children with MIS-C |
| Tuberous sclerosis complex affects multiple organ systems so a multidisciplinary team of medical professionals is required.
| |
|
| |
|
| === Screening of complications: ===
| | '''Comorbidities''' |
| In suspected or newly diagnosed TSC, the following tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference.<ref name="TSCManagement">{{cite journal | vauthors = Krueger DA, Northrup H | title = Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference | journal = Pediatric Neurology | volume = 49 | issue = 4 | pages = 255–65 | date = October 2013 | pmid = 24053983 | pmc = 4058297 | doi = 10.1016/j.pediatrneurol.2013.08.002 }}</ref>
| |
|
| |
|
| * Take a [[Medical history|personal]] and [[Family history (medicine)|family history]] covering three generations. [[Genetic counseling|Genetic counselling]] and tests determine if other individuals are at risk. | | *Children with MIS-C had following underlying comorbidities. |
| *A magnetic resonance imaging (MRI) of the brain to identify tubers, subependymal nodules (SEN) and sub-ependymal giant cell astrocytomas (SEGA). | | **Clinically diagnosed Obesity-8% |
| *Children undergo a baseline electroencephalograph (EEG) and family educated to identify seizures if/when they occur. | | **BMI-Based Obesity-29% |
| *Assess children for behavioural issues, autism spectrum disorder, psychiatric disorders, developmental delay, and neuropsychological problems. | | **Cardiovascular diasease-3% |
| *Scan the abdomen for tumours in various organs, but most importantly angiomyolipomata in the kidneys. MRI is superior to CT or ultrasound. Take blood pressure and test renal function. | | **Respiratory disease-18% |
| *In adult women, test pulmonary function and perform a [[high-resolution computed tomography]] (HRCT) of the chest. | | **Autoimmune disease or immunocompromising condition-5% |
| *Examine the skin under a Wood's lamp (hypomelanotic macules), the fingers and toes (ungual fibroma), the face (angiofibromas), and the mouth (dental pits and gingival fibromas). | |
| *In infants under three, perform an [[echocardiogram]] to spot rhabdomyomas, and [[electrocardiogram]] (ECG) for any [[arrhythmia]]. | |
| *Use a [[Fundoscopy|fundoscope]] to spot retinal hamartomas or achromic patches. | |
|
| |
|
| === Treatment: ===
| | '''Organ System Involved''' |
| The various symptoms and complications from TSC may appear throughout life, requiring continued surveillance and adjustment to treatments. The following ongoing tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference:<ref name="TSCManagement" />
| |
|
| |
|
| *In children and adults younger than 25 years, a magnetic resonance imaging (MRI) of the brain is performed every one to three years to monitor for subependymal giant cell astrocytoma (SEGA). If a SEGA is large, growing or interfering with ventricles, the MRI is performed more frequently. After 25 years, if there are no SEGAs then periodic scans may no longer be required. A SEGA causing acute symptoms are removed with surgery, otherwise either surgery or drug treatment with an mTOR inhibitor may be indicated. | | *71% of children had involvement of at least four organ systems. |
| *Repeat screening for TSC-associated neuropsychiatric disorders (TAND) at least annually. Sudden behavioural changes may indicate a new physical problem (for example with the kidneys, epilepsy or a SEGA).
| |
| *Routine EEG determined by clinical need.
| |
| *Infantile spasms are best treated with [[vigabatrin]] and [[adrenocorticotropic hormone]] used as a second-line therapy. Other seizure types have no TSC-specific recommendation, though epilepsy in TSC is typically difficult to treat (medically refractory).
| |
| *Repeat MRI of abdomen every one to three years throughout life. Check renal (kidney) function annually. Should angiomyolipoma bleed, this is best treated with [[embolisation]] and then corticosteroids. Removal of the kidney ([[nephrectomy]]) is strongly to be avoided. An asymptomatic angiomyolipoma that is growing larger than 3cm is best treated with an mTOR inhibitor drug. Other renal complications spotted by imaging include [[polycystic kidney disease]] and [[renal cell carcinoma]].
| |
| *Repeat chest HRCT in adult women every five to 10 years. Evidence of [[lymphangioleiomyomatosis]] (LAM) indicates more frequent testing. An mTOR inhibitor drug can help, though a lung transplant may be required.
| |
| * A 12-lead ECG should be performed every three to five years.
| |
|
| |
|
| The mTOR inhibitor [[everolimus]] was approved in the US for treatment of TSC-related tumors in the brain ([[subependymal giant cell astrocytoma]]) in 2010 and in the kidneys (renal [[angiomyolipoma]]) in 2012.<ref>{{Cite web|url=http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm302048.htm|title=Press Announcements - FDA approves Afinitor for non-cancerous kidney tumors caused by rare genetic disease|website=www.fda.gov|language=en|access-date=2017-02-08}}</ref><ref>{{Cite web|url=https://www.cancer.gov/about-cancer/treatment/drugs/fda-everolimus|title=FDA Approval for Everolimus|website=National Cancer Institute|language=en|access-date=2017-02-08}}</ref> Everolimus also showed evidence of effectiveness at treating epilepsy in some people with TSC.<ref>{{cite journal | vauthors = French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, Curatolo P, de Vries PJ, Dlugos DJ, Berkowitz N, Voi M, Peyrard S, Pelov D, Franz DN | title = Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study | journal = Lancet | volume = 388 | issue = 10056 | pages = 2153–63 | date = October 2016 | pmid = 27613521 | doi = 10.1016/s0140-6736(16)31419-2 }}</ref><ref name="pmid27601910">{{cite journal | vauthors = Capal JK, Franz DN | title = Profile of everolimus in the treatment of tuberous sclerosis complex: an evidence-based review of its place in therapy | journal = Neuropsychiatric Disease and Treatment | volume = 12 | issue = | pages = 2165–72 | date = 2016 | pmid = 27601910 | pmc = 5003595 | doi = 10.2147/NDT.S91248 }}</ref> In 2017, the European Commission approved everolimus for treatment of refractory partial-onset seizures associated with TSC.<ref>{{Cite news|url=https://globenewswire.com/news-release/2017/01/31/912212/0/en/Novartis-drug-Votubia-receives-EU-approval-to-treat-refractory-partial-onset-seizures-in-patients-with-TSC.html|title=Novartis drug Votubia® receives EU approval to treat refractory partial-onset seizures in patients with TSC|last=AG|first=Novartis International|newspaper=GlobeNewswire News Room|access-date=2017-02-08|language=en-US}}</ref> | | The most common organ system involved in MIS-C children among a total of 186 children were. |
|
| |
|
| Neurosurgical intervention may reduce the severity and frequency of seizures in TSC patients.<ref name="Asano_2005">{{cite journal | vauthors = Asano E, Juhász C, Shah A, Muzik O, Chugani DC, Shah J, Sood S, Chugani HT | title = Origin and propagation of epileptic spasms delineated on electrocorticography | journal = Epilepsia | volume = 46 | issue = 7 | pages = 1086–97 | date = July 2005 | pmid = 16026561 | doi = 10.1111/j.1528-1167.2005.05205.x | pmc = 1360692 }}</ref> <ref name="Chugani_2013">{{cite journal | vauthors = Chugani HT, Luat AF, Kumar A, Govindan R, Pawlik K, Asano E | title = α-[11C]-Methyl-L-tryptophan--PET in 191 patients with tuberous sclerosis complex | journal = Neurology | volume = 81 | issue = 7 | pages = 674–80 | date = August 2013 | pmid = 23851963 | doi = 10.1212/WNL.0b013e3182a08f3f | pmc = 3775695 }}</ref> [[Embolization]] and other surgical interventions can be used to treat renal angiomyolipoma with acute hemorrhage. Surgical treatments for symptoms of [[lymphangioleiomyomatosis]] (LAM) in adult TSC patients include pleurodesis to prevent [[pneumothorax]] and [[lung transplantation]] in the case of irreversible lung failure.<ref name="TSCManagement" />
| | *Gastrointestinal(92%) |
| | *Cardiovascular(80%) |
| | *Hematologic(76%) |
| | * Mucocutaneous(74%) |
| | *Pulmonary(70%) |
| | * Historical perspective |
|
| |
|
| Other treatments that have been used to treat TSC manifestations and symptoms include a [[ketogenic diet]] for intractable epilepsy and pulmonary rehabilitation for LAM.<ref>{{cite journal | vauthors = Hong AM, Turner Z, Hamdy RF, Kossoff EH | title = Infantile spasms treated with the ketogenic diet: prospective single-center experience in 104 consecutive infants | journal = Epilepsia | volume = 51 | issue = 8 | pages = 1403–407 | date = August 2010 | pmid = 20477843 | doi = 10.1111/j.1528-1167.2010.02586.x | url = http://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2010.02586.x/abstract }}</ref> Facial angiofibromas can be reduced with [[laser medicine|laser treatment]] and the effectiveness of mTOR inhibitor topical treatment is being investigated. Laser therapy is painful, requires anaesthesia, and has risks of scarring and dyspigmentation.<ref name="DermUpdate">{{cite journal | vauthors = Jacks SK, Witman PM | title = Tuberous Sclerosis Complex: An Update for Dermatologists | journal = Pediatric Dermatology | volume = 32 | issue = 5 | pages = 563–70 | date = September-October 2015 | pmid = 25776100 | doi = 10.1111/pde.12567 }}</ref>
| | <br /> |
| == References == | | == References == |
| {{Reflist|32em}} | | {{Reflist|32em}} |