Ventricular tachycardia classification
|
Ventricular tachycardia Microchapters |
|
Differentiating Ventricular Tachycardia from other Disorders |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Ventricular tachycardia classification On the Web |
|
to Hospitals Treating Ventricular tachycardia classification |
|
Risk calculators and risk factors for Ventricular tachycardia classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Ventricular tachycardia refers to a rhythm with a heart rate in excess of 100 (and in some definitions 120) beats per minute that arises distal to the bundle of His. Ventricular tachycardia can be classified under three main categories. Firstly, The morphology of the QRS complexes on the EKG (monomorphic ventricular tachycardia vs polymorphic ventricular tachycardia). Secondly, The duration of the episode. Thirdly, The symptoms associated with the episode.
Classification Based Upon Morphology of the QRS Complexes
Based on the morphology of QRS complex ventricular tachycardia can be classified into the following sub types:
Monomorphic ventricular tachycardia
- Monomorphic ventricular tachycardia is defined as a QRS complex morphology that is identical from beat-to-beat in all leads of the surface electrocardiogram (EKG).
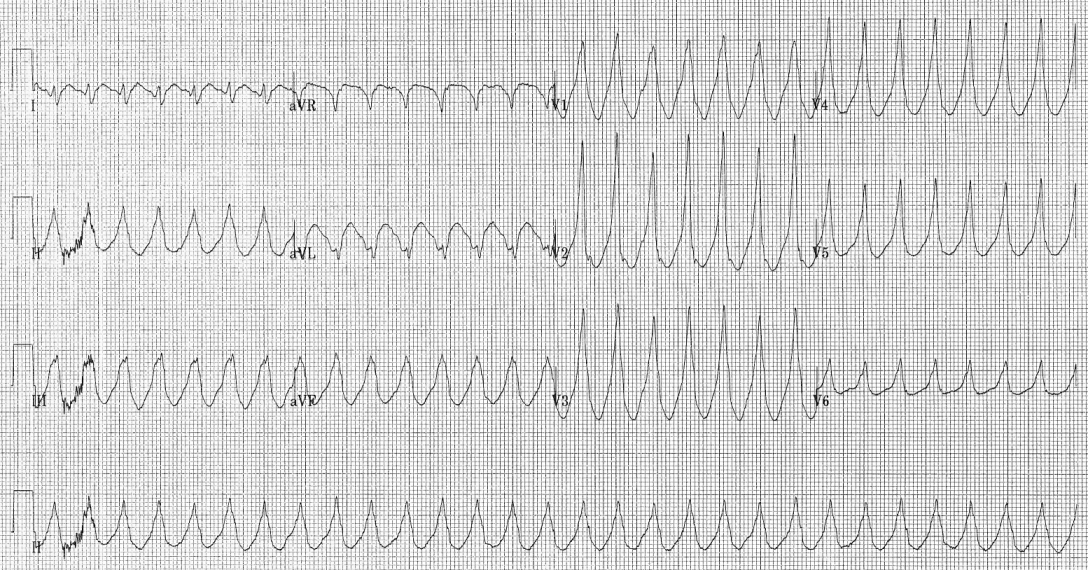
Polymorphic ventricular tachycardia
- Polymorphic ventricular tachycardia, is defined as QRS complexes with beat-to-beat variability in morphology.
- This most commonly appears as a cyclical progressive change in cardiac axis referred to by its french eponym Torsade de pointes (literally translating to "twisting of the points").
Classification Based Upon Duration of Episode
Based upon duration of episode ventricular tachycardia can be classified into:
Non-sustained Ventricular Tachycardia or Paroxysmal Ventricular Tachycardia
- Rapid succession of three or more ectopic beats.
- Self terminates within 30 seconds.
Sustained Ventricular Tachycardia
- Lasts more than 30 seconds.
Incessant Ventricular Tachycardia
- The ventricular tachycardia is recurrent and the episodes are interrupted by only a few sinus beats.
Classification Based Upon Symptoms
Based upon symptoms ventricular tachycardia can be classified into:
Pulseless VT
- Pulseless VT is associated with no effective cardiac output, hence, no effective pulse, and is a cause of cardiac arrest.
- In this circumstance it is best treated the same way as ventricular fibrillation (VF) and is recognized as one of the shockable rhythms on the cardiac arrest protocol.
Perfusing Rhythm with VT
- Some VT is associated with reasonable cardiac output and may even be asymptomatic.
- The heart usually tolerates this rhythm poorly in the medium to long term, and patients may certainly deteriorate to pulseless VT or to VF.
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death - Sustained Monomorphic Ventricular Tachycardia (DO NOT EDIT) [1]
| Class I |
| "1. Wide-QRS tachycardia should be presumed to be VT if the diagnosis is unclear. (Level of Evidence: C) " |
| "2. Direct-current cardioversion with appropriate sedation is recommended at any point in the treatment cascade in patients with suspected sustained monomorphic VT with hemodynamic compromise. (Level of Evidence: C) " |
| Class III (Harm) |
| "1. Calcium channel blockers such as verapamil and diltiazem should not be used in patients to terminate wide-QRS-complex tachycardia of unknown origin, especially in patients with a history of myocardial dysfunction. (Level of Evidence: C) " |
| Class IIa |
| "1. Intravenous procainamide (or ajmaline in some European countries) is reasonable for initial treatment of patients with stable sustained monomorphic VT. (Level of Evidence: B)" |
| "2. Intravenous amiodarone is reasonable for patients with sustained monomorphic VT that is hemodynamically unstable, refractory to conversion with countershock, or recurrent despite procainamide or other agents. (Level of Evidence: C)" |
| "3. Transvenous catheter pace termination can be useful to treat patients with sustained monomorphic VT that is refractory to cardioversion or is frequently recurrent despite antiarrhythmic medication. (Level of Evidence: C)" |
| Class IIb |
| "1. Intravenous lidocaine might be reasonable for initial treatment of patients with stable sustained monomorphic VT specifically associated with acute myocardial ischemia or infarction. (Level of Evidence: C)" |
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death - Polymorphic Ventricular Tachycardia (DO NOT EDIT) [1]
| Class I |
| "1. Direct current cardioversion with appropriate sedation as necessary is recommended for patients with sustained polymorphic VT with hemodynamic compromise and is reasonable at any point in the treatment cascade. (Level of Evidence: B) " |
| "2. Intravenous beta blockers are useful for patients with recurrent polymorphic VT especially if ischemia is suspected or cannot be excluded. (Level of Evidence: B) " |
| "3. Intravenous loading with amiodarone is useful for patients with recurrent polymorphic VT in the absence of abnormal repolarization related to congenital or acquired LQTS. (Level of Evidence: C) " |
| "4. Urgent angiography with a view to revascularization should be considered for patients with polymorphic VT when myocardial ischemia cannot be excluded. (Level of Evidence: C)" |
| Class IIb |
| "1. Intravenous lidocaine may be reasonable for treatment of polymorphic VT specifically associated with acute myocardial ischemia or infarction. (Level of Evidence: C)" |
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death - Repetitive Monomorphic Ventricular Tachycardia (DO NOT EDIT) [1]
| Class IIa |
| "1. Intravenous amiodarone, beta blockers, and intravenous procainamide (or sotalol or ajmaline in Europe) can be useful for treating repetitive monomorphic VT in the context of coronary disease and idiopathic VT. (Level of Evidence: C)" |
2006 ACC/AHA/ESC Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death - Incessant Ventricular Tachycardia (DO NOT EDIT) [1]
| Class I |
| "1. Revascularization and beta blockade followed by intravenous antiarrhythmic drugs such as procainamide or amiodarone are recommended for patients with recurrent or incessant polymorphic VT due to acute myocardial ischemia. (Level of Evidence: C) " |
| Class IIa |
| "1. Intravenous amiodarone or procainamide followed by VT ablation can be effective in the management of patients with frequently recurring or incessant monomorphic VT. (Level of Evidence: C)" |
| Class IIb |
| "1. Intravenous amiodarone and intravenous beta blockers separately or together may be reasonable in patients with VT storm. (Level of Evidence: C)" |
| "2. Overdrive pacing or general anesthesia may be considered for patients with frequently recurring or incessant VT. (Level of Evidence: C)" |
| "3. Spinal cord modulation may be considered for some patients with frequently recurring or incessant VT. (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 1.2 1.3 Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M; et al. (2006). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385–484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.