Sandbox:Sahar
| Differentiating diagnosis of Lymphoma | Symptoms | Signs | Diagnosis | Additional Findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Rash | Diarrhea | Abdominal pain | Weight loss | Painful lymphadenopathy | Hepatosplenomegaly | Arthritis | Lab Findings | ||
| Lymphoma | + | – | – | + | + | – | + | – | Increase ESR, increased LDH | Night sweats, constant fatigue |
| Brucellosis | + | + | – | + | + | + | + | + | Relative lymphocytosis | Night sweats, often with characteristic smell, likened to wet hay |
| Typhoid fever | + | + | – | + | – | – | + | + | Decreased hemoglobin | Incremental increase in temperature initially and than sustained fever as high as 40°C (104°F) |
| Malaria | + | – | + | + | – | – | + | + | Microcytosis,
elevated LDH |
"Tertian" fever: paroxysms occur every second day |
| Tuberculosis | + | + | – | + | + | + | – | + | Mild normocytic anemia, hyponatremia, and | Night sweats, constant fatigue |
| Mumps | + | – | – | – | – | + | – | – | Relative lymphocytosis, serum amylaseelevated | Parotidswelling/tenderness |
| Rheumatoid arthritis | – | + | – | – | – | – | – | + | ESR and CRP elevated, positive rheumatoid factor | Morning stiffness |
| SLE | – | + | – | + | + | – | – | + | ESR and CRP elevated, positive ANA | Fatigue |
| HIV | – | – | – | + | + | + | – | + | Leukopenia | Constant fatigue |
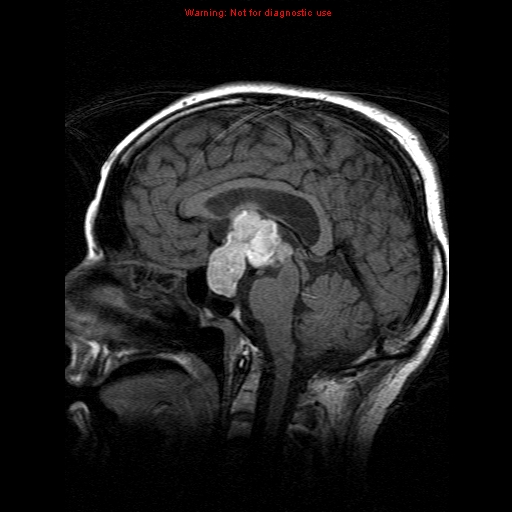
CNS lymphoma must be differentiated from other causes of seizures, headache, and fever in immunocompromised patients such as disseminated tuberculosis and disseminated aspergillosis.
| Disease | Differentiating signs and symptoms | Differentiating tests |
|---|---|---|
| CNS lymphoma[1] |
|
|
| Disseminated tuberculosis[2] |
|
|
| Aspergillosis[3] |
|
|
| Cryptococcosis |
|
|
| Chagas disease[4] |
|
|
| CMV infection[5] |
|
|
| HSV infection[6] |
|
|
| Varicella Zoster infection[7] |
|
|
| Brain abscess[8][9] |
|
|
| Progressive multifocal leukoencephalopathy[10] |
|

Classification
Syncope is classified into three components:
| Classification of Syncope | |||
|---|---|---|---|
| Type | Pathophysiology | Treatment | Additional information |
| syncope | |||||||||||||||||||||||||||||||||
| cardiac | neurogenic | ||||||||||||||||||||||||||||||||
| C01 | |||||||||||||||||||||||||||||||||
| D01 | D02 | D03 | |||||||||||||||||||||||||||||||
| E01 | E02 | E03 | |||||||||||||||||||||||||||||||
| F01 | F02 | ||||||||||||||||||||||||||||||||
| disease | ||||
|---|---|---|---|---|
Syncope is classified into three types.
| Syncope classification | |||
|---|---|---|---|
| Cardia | |||
Syncope
Syncope is classified to three types:
Syncope is classified into three types:
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2]
| Syncope | |||||||||||||||||||||||||||||||||||||||||||||||
| B01 | |||||||||||||||||||||||||||||||||||||||||||||||
| C01 | C03 | C02 | |||||||||||||||||||||||||||||||||||||||||||||
| D01' D01 | D02' D02 | ||||||||||||||||||||||||||||||||||||||||||||||
| E01 | E02 | E03 | E04 | ||||||||||||||||||||||||||||||||||||||||||||
| F01 | F02 | F03 | |||||||||||||||||||||||||||||||||||||||||||||
Syncope classifications:
- Orthostatic:
- Cardiac
- Neurolgoic
| Syncope ddx | ||||
|---|---|---|---|---|
| Clinical manifestations | ||||
- ↑ Gerstner ER, Batchelor TT (2010). "Primary central nervous system lymphoma". Arch. Neurol. 67 (3): 291–7. doi:10.1001/archneurol.2010.3. PMID 20212226.
- ↑ von Reyn CF, Kimambo S, Mtei L, Arbeit RD, Maro I, Bakari M, Matee M, Lahey T, Adams LV, Black W, Mackenzie T, Lyimo J, Tvaroha S, Waddell R, Kreiswirth B, Horsburgh CR, Pallangyo K (2011). "Disseminated tuberculosis in human immunodeficiency virus infection: ineffective immunity, polyclonal disease and high mortality". Int. J. Tuberc. Lung Dis. 15 (8): 1087–92. doi:10.5588/ijtld.10.0517. PMID 21740673.
- ↑ Latgé JP (1999). "Aspergillus fumigatus and aspergillosis". Clin. Microbiol. Rev. 12 (2): 310–50. PMC 88920. PMID 10194462.
- ↑ Rassi A, Rassi A, Marin-Neto JA (2010). "Chagas disease". Lancet. 375 (9723): 1388–402. doi:10.1016/S0140-6736(10)60061-X. PMID 20399979.
- ↑ Emery VC (2001). "Investigation of CMV disease in immunocompromised patients". J. Clin. Pathol. 54 (2): 84–8. PMC 1731357. PMID 11215290.
- ↑ Bustamante CI, Wade JC (1991). "Herpes simplex virus infection in the immunocompromised cancer patient". J. Clin. Oncol. 9 (10): 1903–15. doi:10.1200/JCO.1991.9.10.1903. PMID 1919640.
- ↑ Hambleton S (2005). "Chickenpox". Curr. Opin. Infect. Dis. 18 (3): 235–40. PMID 15864101.
- ↑ Alvis Miranda H, Castellar-Leones SM, Elzain MA, Moscote-Salazar LR (2013). "Brain abscess: Current management". J Neurosci Rural Pract. 4 (Suppl 1): S67–81. doi:10.4103/0976-3147.116472. PMC 3808066. PMID 24174804.
- ↑ Patel K, Clifford DB (2014). "Bacterial brain abscess". Neurohospitalist. 4 (4): 196–204. doi:10.1177/1941874414540684. PMC 4212419. PMID 25360205.
- ↑ Tan CS, Koralnik IJ (2010). "Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis". Lancet Neurol. 9 (4): 425–37. doi:10.1016/S1474-4422(10)70040-5. PMC 2880524. PMID 20298966.