Restless legs syndrome: Difference between revisions
No edit summary |
|||
| Line 26: | Line 26: | ||
==[[Restless legs syndrome epidemiology and demographics|Epidemiology and Demographics]]== | ==[[Restless legs syndrome epidemiology and demographics|Epidemiology and Demographics]]== | ||
==[[Restless legs syndrome risk factors|Risk | ==[[Restless legs syndrome risk factors|Risk Factors]]== | ||
==[[Restless legs syndrome screening|Screening]]== | ==[[Restless legs syndrome screening|Screening]]== | ||
Revision as of 14:23, 10 June 2013
| Restless legs syndrome | |
 | |
|---|---|
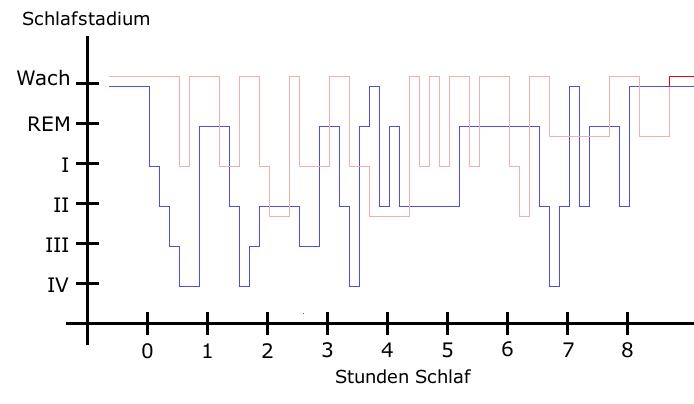
| Sleep pattern of a Restless Legs Syndrome patient (red) vs. a healthy sleep pattern (blue). |
|
Restless legs syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Restless legs syndrome On the Web |
|
American Roentgen Ray Society Images of Restless legs syndrome |
|
Risk calculators and risk factors for Restless legs syndrome |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: Wittmaack-Ekbom's syndrome; RLS
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Restless legs syndrome from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Diagnosis
Symptoms
- "An urge to move, usually due to uncomfortable sensations that occur primarily in the legs."
The sensations are unusual and unlike other common sensations, and those with RLS have a hard time describing them. People use words such as: uncomfortable, antsy, electrical, creeping, painful, itching, pins and needles, pulling, creepy-crawly, ants inside the legs, and many others. The sensation and the urge can occur in any body part; the most cited location is legs, followed by arms. Some people have little or no sensation, yet still have a strong urge to move.
- "Motor restlessness, expressed as activity, that relieves the urge to move."
Movement will usually bring immediate relief, however, often only temporary and partial. Walking is most common; however, doing stretches, yoga, biking, or other physical activity may relieve the symptoms. Constant and fast up-and-down movement of the leg, coined "sewing machine legs" by at least one RLS sufferer, is often done to keep the sensations at bay without having to walk. Sometimes a specific type of movement will help a person more than another.
- "Worsening of symptoms by relaxation."
Any type of inactivity involving sitting or lying – reading a book, a plane ride, watching TV or a movie, taking a nap - can trigger the sensations and urge to move. This depends on several factors: the severity of the person’s RLS, the degree of restfulness, the duration of the inactivity, etc.
- "Variability over the course of the day-night cycle, with symptoms worse in the evening and early in the night."
While some only experience RLS at bedtime and others experience it throughout the day and night, most sufferers experience the worst symptoms in the evening and the least in the morning.
NIH criteria
In 2003, a National Institutes of Health (NIH) consensus panel modified their criteria to include the following:
- (1) An urge to move the limbs with or without sensations
- (2) Worsening at rest
- (3) Improvement with activity
- (4) Worsening in the evening or night.[1]
Treatment
Medical Therapy
See potential causal relationship between acidosis and RLS above in "Explanation." An algorithm for treating Primary RLS ( RLS without any secondary medical condition including iron deficiency, varicose vein, thyroid, etc.) was created by leading RLS researchers at the Mayo Clinic and is endorsed by the Restless Legs Syndrome Foundation. This document provides guidance to both the treating physician and the patient, and includes both nonpharmacological and pharmacological treatments.[2] Treatment of primary RLS should not be considered unless all the secondary medical conditions are ruled out. Drug therapy in RLS is not curative and is known to have significant side effects and needs to be considered with caution. The secondary form of RLS has the potential for cure if the precipitating medical condition (iron deficiency, venous reflux/varicose vein, thyroid, etc.) is managed effectively.
Iron supplements
All people with RLS should have their ferritin levels tested; ferritin levels should be at least 50 mcg for those with RLS. Oral iron supplements, taken under a doctor's care, can increase ferritin levels. For some people, increasing ferritin will eliminate or reduce RLS symptoms. A ferritin level of 50 mcg is not sufficient for some sufferers and increasing the level to 80 mcg may greatly reduce symptoms. However, at least 40% of people will not notice any improvement. Treatment with IV iron is being tested at the US Mayo Clinic and Johns Hopkins Hospital. It is dangerous to take iron supplements without first having ferritin levels tested, as many people with RLS do not have low ferritin and taking iron when it is not called for can cause iron overload disorder, potentially a very dangerous condition.
New results from the first ever double-blind clinical study,[3] performed at Örebro University Hospital show that all 29 out of 60 patients that were treated with IV-infusion of up to a total of 1000 mg of iron (in the form of iron saccharose, Venofer), were markedly improved after 3 weeks. The effect lasted for 5-6 months. Those 31 receiving placebo had just a slight effect after 3 weeks that additionally disappeared rapidly.
The treatment was given even if iron deficiency was not shown according to ferritin levels. Worries of anaphylactic reactions did not come true. This is probably due to the form the IV iron was given. Anaphylaxis has been associated predominantly with dextran based infusions.
Lifestyle changes and other non-medicinal approaches
Treatment for RLS is based on how disruptive the symptoms are. All people should review their lifestyle and see what changes could be made to reduce or eliminate their RLS symptoms. These include: finding the right level of exercise (too much worsens it, too little may trigger it); eliminating caffeine, smoking, and alcohol; changing the diet to eliminate foods that trigger RLS (different for each person, but may include eliminating sugar, triglycerides, gluten, sugar substitutes (aspartame), following a low-fat diet, etc.); keeping good sleep hygiene; treating conditions that may cause secondary RLS; avoiding or stopping OTC or prescription drugs that trigger RLS; adding supplements such as potassium, magnesium, B-12, folate, vitamin E, and calcium. Some of these changes, such as diet (particularly aspartame) and adding supplements are based on anecdotal evidence from RLS sufferers as few studies have been done on these alternatives.
For those who experience RLS infrequently and do not need or want to try medication, in addition to lifestyle changes they can try:
- Some form of exercise for several minutes such as walking, stretching, meditation, yoga, etc. at bedtime
- Heat or cold, such as a hot or cold bath, a heating pad, a cold cloth, or a fan
- Soaking one's feet in hot water just prior to going to sleep
- Engrossing the mind in a game, the computer, or figuring something out
- Wearing compression stockings, tight pantyhose, or wrapping the legs in elastic bandages
- Placing a pillow between the knees or upper-legs while lying in bed
- Eating porridge oats or almonds daily for their magnesium content
- Hot green tea can relieve symptoms
- Deep breathing for one or two minutes
- Massage and chiropractic spinal manipulation provide significant relief for some patients.
Medicinal approaches
For those whose RLS disrupts or prevents sleep or regular daily activities, medication is often required. Many Doctors currently use, and the Mayo Clinic Algorithm includes,[2] medication from four categories:
- 1) Dopamine agonists such as ropinirole, pramipexole, carbidopa/levodopa or pergolide:
| Agent | Timeline | Comments |
| ropinirole | Approved In 2005 by the Food and Drug Administration to treat moderate to severe Restless Legs Syndrome | The drug was first approved for Parkinson's disease in 1997. |
| pramipexole (Mirapex, Sifrol, Mirapexen in the EU) | In February 2006, the EU Scientific Committee issued a positive recommendation for approving for the treatment of RLS in the EU. US FDA approved Mirapex in 2006. | - |
| rotigotine | Currently in process for US FDA and EU approval for RLS | Delivered via a transdermal patch |
| pergolide | In March 2007 was withdrawn from the U.S. market | Withdrawn due to implication in valvular heart disease, that was shown in two independent studies. |
There are some issues with the use of dopamine augmentation. Dopamine agonists may cause augmentation. This is a medical condition where the drug itself causes symptoms to increase in severity and/or occur earlier in the day. Dopamine agonists may also cause rebound, when symptoms increase as the drug wears off. Also, a recent study indicated that dopamine agonists used in restless leg patients can lead to an increase in compulsive gambling.[4]
- 2) Opioids such as propoxyphene, oxycodone, or methadone, etc.
- 3) Benzodiazepines, which often assist in staying asleep and reducing awakenings from the movements
- 4) Anticonvulsants, which often help people who experience the RLS sensations as painful, such as gabapentin
In a study of 10 patients, it was reported that partial relief with taking a supplemental magnesium salt[5] such as magnesium oxide or magnesium gluconate once or twice a day, and reducing the dose if diarrhea develops. Magnesium sulfate is the most active form; however, magnesium supplementation can cause complications for patients with renal problems.[6]
Controversies
Recently, several major pharmaceutical companies are reported to be marketing drugs without an explicit approval for RLS, which are "off-label" applications for drugs approved for other diseases. The Restless Leg Foundation [7] received 44% of its $1.4 million in funding from these pharmaceutical groups[8]. This has called into question the neutrality of this group (significant conflict of interest issue) and the course of action which they recommend to RLS patients.
Related Chapters
References
- ↑ Allen R, Picchietti D, Hening W, Trenkwalder C, Walters A, Montplaisi J (2003). "Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health". Sleep Med. 4 (2): 101–19. PMID 14592341.
- ↑ 2.0 2.1 Mayo Clinic Algorithm also available as .pdf
- ↑ "Järninfusioner minskar symtomen vid restless legs". Retrieved 2007-07-23.
- ↑ "Medical Therapy for Restless Legs Syndrome may Trigger Compulsive Gambling", Mayo Clinic in Rochester, February 08, 2007
- ↑ Hornyak M, Voderholzer U, Hohagen F, Berger M, Riemann D (1998). "Magnesium therapy for periodic leg movements-related insomnia and restless legs syndrome: an open pilot study". Sleep. 21 (5): 501–5. PMID 9703590.
- ↑ "Magnesium Supplements (Systemic) - MayoClinic.com". Retrieved 2007-08-08.
- ↑ * RLS Foundation
- ↑ Marshall, Jessica, and Peter Aldhous. "Patient Groups Special." New Scientist, 10/26/06
Template:Diseases of the nervous system
ca:Síndrome de les cames neguitoses de:Restless-Legs-Syndrom ms:Sindrom kaki resah fi:Levottomat jalat sv:Rastlösa ben