Respiratory patterns: Difference between revisions
(Created page with "__NOTOC__ {{Respiratory patterns}} {{CMG}}; {{AE}} {{EG}} {{SK}} ==Overview==") |
m (Bot: Removing from Primary care) |
||
| (23 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}} {{EG}} | {{CMG}}; {{AE}} {{EG}} | ||
==Overview== | |||
Normal [[breathing]] is consisted of [[inhalation]] (sucking the air into the [[lungs]]) followed by [[exhalation]] (blowing the air out of the [[lungs]]). Every [[exhalation]] is followed by an automatic pause of about 2 second, before the next [[inhalation]]. Normal respiratory rate in a healthy adult is 12-20 per minutes. There are some conditions that may cause variation in rate and depth of respiration. Tachypnea is defined as increase in rate and decrease in depth of [[breathing]]. [[Bradypnea]] is a decrease in number of [[breath]] to less than 8-10 per minute in adults and 16 per minute in [[infants]]. [[Apnea]] is the [[respiratory arrest]] for couple of seconds. Cheyne-Stokes [[respiration]] is recurrent central [[Apneustic respirations|apneustic episodes]] during [[sleep]]. Biot's [[respiration]] is a kind of slow [[respiration]] pattern with periodic increasing 10-20 [[respiration]] per minute, without crescendo–decrescendo pattern. Apneustic respiration is prolonged [[inspiration]] arrest followed by inadequate [[expiration]]. Agonal [[breathing]] is slow, very shallow irregular [[Respiration|respirations]]. Kussmaul's respiration is a deep, sighing [[respiration]] with normal or slow rate. Sighing [[respiration]] is a normal [[physiologic]] reaction of human body to [[fatigue]] and [[emotional]] changes. | |||
== Eupnea == | |||
* Normal [[breathing]] is consisted of [[inhalation]] (sucking the air into the [[lungs]]) followed by [[exhalation]] (blowing the air out of the [[lungs]]). | |||
* Every [[exhalation]] is followed by an automatic pause of about 2 second, before the next [[inhalation]]. | |||
* [[Inhalation]] is an active process using [[diaphragm]] muscles, despite [[exhalation]] which is a passive process. | |||
* [[Eupnea]] is the normal pattern of [[breathing]] with a rate of 10-12 per minute, each cycle is composed of:<ref name="pmid14637316">{{cite journal |vauthors=St -John WM, Paton JF |title=Defining eupnea |journal=Respir Physiol Neurobiol |volume=139 |issue=1 |pages=97–103 |date=December 2003 |pmid=14637316 |doi= |url=}}</ref> | |||
** [[Inhalation]] for 1.5-2 seconds | |||
** [[Exhalation]] for 1.5-2 seconds | |||
** Spontaneous stop of 2 seconds | |||
* The main characteristics of eupnea are as following:<ref name="pmid18322090">{{cite journal |vauthors=Ruangkittisakul A, Schwarzacher SW, Secchia L, Ma Y, Bobocea N, Poon BY, Funk GD, Ballanyi K |title=Generation of eupnea and sighs by a spatiochemically organized inspiratory network |journal=J. Neurosci. |volume=28 |issue=10 |pages=2447–58 |date=March 2008 |pmid=18322090 |doi=10.1523/JNEUROSCI.1926-07.2008 |url=}}</ref> | |||
** Slow | |||
** Regular | |||
** Nasal [[inhalation]], oral [[exhalation]] | |||
** [[Diaphragmatic breathing|Diaphragmatic]] | |||
** Effortless | |||
** Clear auscultation: | |||
*** No panting | |||
*** No [[wheezing]] | |||
*** No sighing | |||
*** No deep [[breathing]] | |||
=== Normal respiratory rate in every age group is as following: === | |||
{| class="wikitable" | |||
!Age group | |||
!Normal respiratory rate (Breath number per minute) | |||
|- | |||
|Infants | |||
|30 to 60 | |||
|- | |||
|1 to 3 years | |||
|24 to 40 | |||
|- | |||
|3 to 6 years | |||
|22 to 34 | |||
|- | |||
|6 to 12 years | |||
|18 to 30 | |||
|- | |||
|12 to 18 years | |||
|12 to 16 | |||
|} | |||
== Tachypnea == | |||
* Tachypnea is increased rate and decrease depth of [[breathing]]. | |||
<div style="text-align: center;">'''The main pathophysiology of tachypnea is as following:'''<ref name="pmid171314692">{{cite journal| author=Browne GW, Pitchumoni CS| title=Pathophysiology of pulmonary complications of acute pancreatitis. | journal=World J Gastroenterol | year= 2006 | volume= 12 | issue= 44 | pages= 7087-96 | pmid=17131469 | doi= | pmc=4087768 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17131469 }}</ref></div> | |||
{{family tree/start}} | |||
{{family tree| | | | | | | | A01 | | A02 | | A03 | | A04 | |A01=Decreased plasma [[oxygen]] ([[hypoxemia]])|A02=Increased plasma [[CO2]] <br>([[respiratory acidosis]])|A03=Decreased [[pulmonary compliance]]|A04=Increased [[airway]] resistance}} | |||
{{family tree| | | | | | | | |!| | | |!| | | |!| | | |!| | |}} | |||
{{family tree| | | | | | | | B01 | | B02 | | B03 | | B04 | |B01=[[Carotid body]]|B02=[[Medullary]] [[chemoreceptors]]|B03=[[Pulmonary]] or [[muscle]] [[mechanoreceptors]]|B04=[[Airway]] [[receptors]]}} | |||
{{family tree| | | | | | | | |`|-|-|-|^|-|v|-|^|-|-|-|'| | |}} | |||
{{family tree| | | | | | | | | | | | | | C01 | | | | | | | |C01='''Tachypnea'''}} | |||
{{family tree/end}} | |||
=== The main causes of tachypnea are classified into [[pulmonary]], [[cardiovascular]], [[hematologic]], and [[metabolic]] pathophysiologies.<ref name="pmid20807157">{{cite journal |vauthors=Yurdakök M |title=Transient tachypnea of the newborn: what is new? |journal=J. Matern. Fetal. Neonatal. Med. |volume=23 Suppl 3 |issue= |pages=24–6 |date=October 2010 |pmid=20807157 |doi=10.3109/14767058.2010.507971 |url=}}</ref> === | |||
{| class="wikitable" | |||
! colspan="2" |Causes | |||
!Other findings | |||
|- | |||
| rowspan="5" |[[Pulmonary]] | |||
|[[Asthma]] | |||
| | |||
* [[Wheezing]] | |||
* Prolonged [[Expiration]] | |||
* Hyperinflated lungs | |||
|- | |||
|[[Chronic obstructive pulmonary disease|Chronic obstructive pulmonary disease (COPD)]] | |||
| | |||
* Clear lung field in [[chest X-ray]] | |||
* Flattened [[diaphragm]] | |||
* Hyperinflated [[lungs]] | |||
|- | |||
|[[Pneumonia]] | |||
| | |||
* [[Rhonchi]] and scattered [[wheezing]] | |||
* Air-bronchograms | |||
* [[Lobar pneumonia|Lobar]] or [[interstitial]] infiltrates | |||
|- | |||
|[[Congestive heart failure|Congestive heart failure (CHF)]] | |||
| | |||
* Basilar [[crackles]] | |||
* [[Jugular vein distention|Jugular vein distention (JVD)]] | |||
* [[Pulmonary edema]] and [[Pulmonary congestion|congestion]] | |||
|- | |||
|[[Pneumothorax]] | |||
| | |||
* Absent [[breath sounds]] | |||
* Loss of [[pulmonary]] and [[vascular]] marking | |||
|- | |||
| rowspan="4" |[[Cardiovascular]] | |||
|[[Pericardial effusion]] | |||
| | |||
* Low voltage [[ECG]] | |||
* [[Pericardial]] fluid accumulation | |||
|- | |||
|[[Cardiac tamponade|Cardiac Tamponade]] | |||
| | |||
* [[Electrical alternans]] | |||
* [[Right ventricular]] collapse during [[diastole]] | |||
|- | |||
|[[Pulmonary embolism]] | |||
| | |||
* [[Sinus tachycardia]] | |||
* [[Right ventricular]] enlargement | |||
* [[McConnell sign]] in [[echocardiography]] | |||
|- | |||
|[[Myocardial infarction|Myocardial infarct]] | |||
| | |||
* Inverted [[T-wave]] or depressed/elevated [[ST-segment]] | |||
* Local or generalized wall motion abnormality | |||
|- | |||
| rowspan="2" |[[Hematologic]] | |||
|[[Anemia]] | |||
| | |||
* [[Hypoxemia]]-induced [[Carotid body|carotid chemoreceptors]] stimulation | |||
* Chronic [[fatigue]] and [[numbness]] | |||
|- | |||
|[[Sickle cell disease]] | |||
| | |||
* Severe [[bone pain]] | |||
* [[Autosplenectomy]] | |||
* [[Hematuria]] | |||
|- | |||
| rowspan="2" |[[Metabolic]] | |||
|[[Metabolic acidosis]] | |||
| | |||
* [[Dyspnea]] and [[tachypnea]] | |||
* May lead to [[cardiac arrest]] and death in severe uncompensated cases | |||
|- | |||
|[[Diabetic ketoacidosis|Diabetic ketoacidosis (DKA)]] | |||
| | |||
* [[Abdominal pain]] and [[ketonemia]] | |||
* High [[blood glucose]] | |||
|} | |||
== Bradypnea == | |||
* [[Bradypnea]] is defined as decrease in respiratory rate to less than 8-10 per minute in adults and 16 per minute in [[infants]]. | |||
* Mostly in [[bradypnea]] the [[exhalation]] phase is increased. | |||
* The depth of [[Breathe|breathes]] and [[tidal volume]] may be increased during [[bradypnea]] episodes. | |||
* The main [[pathophysiology]] of bradypnea includes:<ref name="LeungSchmitt2009">{{cite journal|last1=Leung|first1=Alexander K. C.|last2=Schmitt|first2=Marcus|last3=Thomas|first3=Christie P.|last4=Sunderkötter|first4=Cord|last5=Schiller|first5=Meinhard|last6=Schwarz|first6=Thomas|last7=Berneburg|first7=Mark|last8=Kohlschütter|first8=Alfried|last9=Cerroni|first9=Lorenzo|last10=Direskeneli|first10=Haner|last11=Calamia|first11=Kenneth|last12=David|first12=Gloria L.|last13=Zeldin|first13=Darryl C.|last14=Schütte|first14=Bärbel|last15=Denson|first15=Lee A.|last16=Erhardt|first16=Andreas|last17=Kubitz|first17=Ralf|last18=Häussinger|first18=Dieter|last19=Sealey|first19=Wendy M.|last20=Mock|first20=Donald M.|last21=Wolf|first21=Barry|last22=Schumacher|first22=Johannes|last23=Propping|first23=Peter|last24=Metze|first24=Dieter|last25=Leung|first25=Alexander K. C.|last26=Wong|first26=Andrew L.|last27=Berneburg|first27=Mark|last28=Schwarz|first28=Thomas|last29=Hengstschläger|first29=Markus|last30=High|first30=Whitney A.|last31=Shroyer|first31=Kenneth R.|last32=McCready|first32=M. Elizabeth|last33=Bulman|first33=Dennis E.|last34=Afzal|first34=Ali R.|last35=Everman|first35=David B.|last36=Stoll|first36=Claude|last37=Darcan|first37=Sukran|last38=Kou|first38=Yu Ru|last39=Lin|first39=You Shuei|last40=Suzuki|first40=Yoichi|last41=Tada|first41=Keiya|last42=Leung|first42=Alexander K. C.|last43=Kupka|first43=Susan|last44=Dietmaier|first44=Wolfgang|last45=Hartmann|first45=Arndt|last46=Hennekam|first46=Raoul C. M.|last47=Belperio|first47=John A.|last48=Keane|first48=Michael P.|last49=Smith|first49=M. Iain|last50=Strieter|first50=Robert M.|last51=Molfino|first51=Nestor A.|last52=Sciandra|first52=Francesca|last53=Rossenbacker|first53=Tom|last54=Priori|first54=Silvia G.|last55=Senzolo|first55=Marco|last56=Triantos|first56=Christos|last57=Samonakis|first57=Dimitrios|last58=Cholongitas|first58=Evangelos|last59=Burroughs|first59=Andrew K.|last60=Mura|first60=Marco|last61=Braun-Falco|first61=Markus|last62=Hofmann|first62=Silke|last63=Bruckner-Tuderman|first63=Leena|title=Bradypnea|year=2009|pages=241–243|doi=10.1007/978-3-540-29676-8_246}}</ref> | |||
** [[Desensitization]] of the [[medullary]] responses to [[PCO2|PCO<sub>2</sub>]] | |||
** Reduction in [[respiratory]] [[neuronal]] activity | |||
** Inhibition of [[neural]] transmission within the [[respiratory center]] | |||
** [[Neuronal]] damage to the [[brain stem]] | |||
* The main causes of bradypnea are as following:<ref name="pmid11943527">{{cite journal |vauthors=Flisberg P, Jakobsson J, Lundberg J |title=Apnea and bradypnea in patients receiving epidural bupivacaine-morphine for postoperative pain relief as assessed by a new monitoring method |journal=J Clin Anesth |volume=14 |issue=2 |pages=129–34 |date=March 2002 |pmid=11943527 |doi= |url=}}</ref> | |||
{| class="wikitable" | |||
! colspan="3" |Causes | |||
!Other | |||
|- | |||
| rowspan="9" |[[Drugs|'''Drugs''']] | |||
| rowspan="5" |'''[[Opioids]]''' | |||
|[[Heroin]] | |||
| rowspan="5" |Can become worse when used along with: | |||
* [[Smoking]] | |||
* [[Benzodiazepines]] | |||
* [[Barbiturates]] | |||
* [[Phenobarbital]] | |||
* [[Gabapentin|Gabapentinoids]] | |||
* [[Alcohol]] consuming | |||
* [[Obstructive sleep apnea]] | |||
* [[Chronic obstructive pulmonary disease|Chronic obstructive pulmonary disease (COPD)]] | |||
* [[Lung cancer]] | |||
|- | |||
|[[Codeine]] | |||
|- | |||
|[[Hydrocodone]] | |||
|- | |||
|[[Morphine]] | |||
|- | |||
|[[Oxycodone]] | |||
|- | |||
| rowspan="2" |'''[[Toxins]]''' | |||
|[[Sodium azide]] | |||
| | |||
* Found in automobile airbags | |||
|- | |||
|[[Carbon monoxide]] | |||
| | |||
* Produced from [[oil]] or [[gas]] furnaces | |||
* Absorbed by lungs and decrease the blood oxygen level | |||
|- | |||
| rowspan="2" |'''Other [[drugs]]''' | |||
|[[Sedatives]] | |||
| rowspan="2" | | |||
* Decrease [[respiratory]] drive | |||
* Desensitizing to lowered [[PaO2|plasma oxygen level]] | |||
|- | |||
|[[Anesthetics]] | |||
|- | |||
| rowspan="8" |[[Systemic disease|'''Systemic disease''']] | |||
| rowspan="5" |[[Lung diseases|'''Lung diseases''']] | |||
|[[Emphysema]] | |||
| rowspan="5" | - | |||
|- | |||
|[[Chronic bronchitis]] | |||
|- | |||
|[[Asthma|Severe asthma]] | |||
|- | |||
|[[Pneumonia]] | |||
|- | |||
|[[Pulmonary edema]] | |||
|- | |||
|[[Thyroid|'''Thyroid''']] | |||
|[[Hypothyroidism]] | |||
| - | |||
|- | |||
| rowspan="2" |[[Neuromuscular|'''Neuromuscular''']] | |||
|[[Guillain-Barré syndrome]] | |||
| rowspan="2" | | |||
* Affect [[Respiratory system|respiratory]] [[nerve]] and [[muscles]] | |||
** [[Diaphragm]] | |||
** [[Intercostal muscles]] | |||
|- | |||
|[[Amyotrophic lateral sclerosis|Amyotrophic lateral sclerosis (ALS)]] | |||
|} | |||
== Apnea == | |||
* [[Apnea]] is the [[respiratory arrest]] for couple of seconds. | |||
* The most common form of [[apnea]] in generally healthy people is [[obstructive sleep apnea]]. | |||
* The [[pathophysiology]] of [[sleep apnea]] are as following:<ref name="urlObstructive Sleep Apnea - National Library of Medicine - PubMed Health">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024431/ |title=Obstructive Sleep Apnea - National Library of Medicine - PubMed Health |format= |work= |accessdate=}}</ref> | |||
<small> | |||
{{family tree/start}} | |||
{{family tree| | | | | | | | | | | | | | A01 | | | | | | | | | | | | | | | | | |A01='''Apnea'''}} | |||
{{family tree| | | | | | |,|-|-|-|-|-|-|-|^|-|-|-|-|-|-|-|.| | | | | | | | | | |}} | |||
{{family tree| | | | | | B01 | | | | | | | | | | | | | | B02 | | | | | | | | | |B01='''''[[Sleep disturbances]]'''''|B02='''''↓[[oxygen|O2]], ↑[[CO2]], ↓[[pH]]'''''}} | |||
{{family tree| | | | | | |!| | | | | | | | | | | | | | | |!| | | | | | | | | | |}} | |||
{{family tree| | |,|-|-|-|+|-|-|-|.| | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | |}} | |||
{{family tree| | D01 | | D02 | | D03 | | D04 | | D05 | | D06 | | D07 | | D08 | |D01=Excessive motor activity|D02=Loss of deep sleep<br>Sleep fragmentation|D03=[[Brain]] malfunction|D04=Severe [[CO2 retention]]|D05=Systemic [[vasoconstriction]]|D06=[[Pulmonary]] [[vasoconstriction]]|D07=[[Vagal]] [[bradycardia]]<br>Ectopic [[cardiac]] [[pulses]]|D08=Decreased [[pulmonary]] pressure<br> Increased [[afterload|cardiac afterload]]}} | |||
{{family tree| | |!| | | |`|-|v|-|'| | | |!| | | |!| | | |!| | | |!| | | |!| | |}} | |||
{{family tree| | E01 | | | | E02 | | | | E03 | | E04 | | E05 | | E06 | | E07 | |E01=Restless sleep|E02=Excessive daytime [[fatigue]]|E03=Chronic [[hypoventilation]]|E04=[[Systemic hypertension]]|E05=[[Pulmonary hypertension]]|E06=Unexplained '''''nocturnal death'''''|E07=[[Left heart failure]]}} | |||
{{family tree| | | | | | | | F01 | | | | | | | | | | | | F02 | | | | | | | | | |F01=Intellectual deterioration|F02=[[Right heart failure]]}} | |||
{{family tree| | | | | | | | F01 | | | | | | | | | | | | | | | | | | | | | | | |F01=[[Personality]] change}} | |||
{{family tree| | | | | | | | F01 | | | | | | | | | | | | | | | | | | | | | | | |F01=[[Behavioral disorder]]}} | |||
{{family tree/end}} | |||
</small> | |||
To read more about sleep apnea, click [[Sleep apnea|here]]. | |||
* The main causes of [[apnea]] include:<ref name="pmid26336596">{{cite journal| author=Spicuzza L, Caruso D, Di Maria G| title=Obstructive sleep apnoea syndrome and its management. | journal=Ther Adv Chronic Dis | year= 2015 | volume= 6 | issue= 5 | pages= 273-85 | pmid=26336596 | doi=10.1177/2040622315590318 | pmc=4549693 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26336596 }}</ref> | |||
** [[Obstructive sleep apnea]] | |||
** [[Opioid toxicity]] | |||
** [[Seizure]] | |||
** [[Asthma]] | |||
** [[Neurologic]] causes | |||
*** [[Stroke]] | |||
*** [[Myotonic dystrophy]] | |||
*** [[Neuromuscular]] [[respiratory failure]] | |||
*** [[Spinal cord injury]] | |||
*** [[Bacterial meningitis]] | |||
** [[Pulmonary]] causes | |||
*** [[Chronic obstructive pulmonary disease|Chronic obstructive pulmonary disease (COPD)]] | |||
*** [[Influenza]] | |||
*** [[Pulmonary emboli]] | |||
*** [[Aspiration pneumonia]] | |||
*** [[Atelectasis]] | |||
*** [[Chronic bronchitis]] | |||
*** [[Foreign body aspiration]] | |||
*** [[Pulmonary edema]] | |||
*** [[Viral pneumonia]] | |||
** [[Down syndrome]] | |||
** [[Metabolic acidosis]] | |||
** [[Cannabis]] use | |||
== Cheyne-Stokes Respiration == | |||
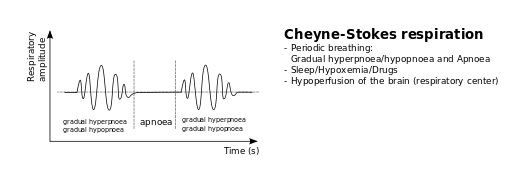
* Cheyne-Stokes [[respiration]] is recurrent central [[Apneustic respirations|apneustic episodes]] during [[sleep]]. | |||
* [[Tidal volume]] has crescendo-decrescendo pattern during Cheyne-Stokes [[respiration]]. | |||
* Cheyne-Stokes [[respiration]] is almost always due to congestive heart failure, contributed with:<ref name="pmid7723977">{{cite journal |vauthors=Nachtmann A, Siebler M, Rose G, Sitzer M, Steinmetz H |title=Cheyne-Stokes respiration in ischemic stroke |journal=Neurology |volume=45 |issue=4 |pages=820–1 |date=April 1995 |pmid=7723977 |doi= |url=}}</ref> | |||
** [[Orthopnoea|Orthopnea]] | |||
** [[Paroxysmal nocturnal dyspnea]] | |||
** [[Excessive daytime sleepiness]] | |||
** Witnessed [[Apnea|apneas]] | |||
* Patients with [[congestive heart failure]] who have already Cheyne-Stokes [[respiration]] pattern, would have more [[mortality rate]].<ref name="pmid8542128">{{cite journal |vauthors=Hanly PJ, Zuberi-Khokhar NS |title=Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure |journal=Am. J. Respir. Crit. Care Med. |volume=153 |issue=1 |pages=272–6 |date=January 1996 |pmid=8542128 |doi=10.1164/ajrccm.153.1.8542128 |url=}}</ref> | |||
<div style="text-align: center;">'''The main pathophysiology of Cheyne-Stokes respiration pattern is as following:<ref name="Naughton1998">{{cite journal|last1=Naughton|first1=M T|title=Pathophysiology and treatment of Cheyne-Stokes respiration|journal=Thorax|volume=53|issue=6|year=1998|pages=514–518|issn=0040-6376|doi=10.1136/thx.53.6.514}}</ref>''' | |||
</div> | |||
<br> | |||
<small><small> | |||
{{family tree/start}} | |||
{{family tree| | A01 | | A02 | | A03 | | A04 | | A05 | | A06 | | A07 | | A08 | | A09 | | A10 | | A11 | | |A01=[[Hypoxemia]]|A02=[[Pulmonary vein]] [[congestion]]|A03=[[Pulmonary]] [[C fibers]] stimulation|A04=Spontaneous arousal|A05=Increased circulating [[noradrenaline]]|A06=Decreased [[cardiac output]]|A07=Increased [[cardiac]] chamber size|A08=Increased [[blood volume]]|A09=[[Hyperventilation]] during day and night|A10=Restrictive [[ventilator|ventilatory]] defect|A11=Decreased [[CO2]] transfer capacity}} | |||
{{family tree| | |!| | | |`|-|v|-|'| | | |`|-|v|-|'| | | |`|-|-|-|+|-|-|-|'| | | |!| | | |!| | | |!| | | |}} | |||
{{family tree| | B01 | | | | B02 | | | | | | B03 | | | | | | | | B04 | | | | | | B05 | | B06 | | B07 | | |B01=Peripheral [[chemoreceptor]] stimulation|B02=Increased [[pulmonary]] [[vagal]] efferent activity|B03=Increased [[sympathetic]] activity|B04=[[Circulation|Circulatory]] delay|B05=Decreased total body [[CO2]]|B06=Decreased total body [[oxygen|O2]]|B07=Increased [[pulmonary capillary wedge pressure]]}} | |||
{{family tree| | |`|-|-|-|-|-|+|-|-|-|-|-|-|-|'| | | | | | |,|-|-|^|-|-|.| | | | |`|-|-|-|+|-|-|-|'| | | |}} | |||
{{family tree| | | | | | | | C01 | | | | | | | | | | | | | C02 | | | | C03 | | | | | | | C04 | | | | | | |C01='''''[[Hyperventilation]]'''''|C02='''''Length of the apnea-hyperpnea cycle'''''|C03='''''Crescendo-decrescendo respiratory pattern'''''|C04='''''Decreased [[blood gas]] [[buffering agent|buffering]] capacity'''''}} | |||
{{family tree| | | | | | | | |!| | | | | | | | | | | | | | |`|-|-|v|-|-|'| | | | | | | | |!| | | | | | | |}} | |||
{{family tree| | | | | | | | |`|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-| D01 |-|-|-|-|-|-|-|-|-|-|'| | | | | | | |D01='''Cheyne-Stokes respiration'''}} | |||
{{family tree/end}} | |||
</small> | |||
</small> | |||
* Cheyne-Stokes respiration is mostly secondary to [[heart failure]], but can be associated with following conditions:<ref name="pmid1509783">{{cite journal| author=Lieber C, Mohsenin V| title=Cheyne-Stokes respiration in congestive heart failure. | journal=Yale J Biol Med | year= 1992 | volume= 65 | issue= 1 | pages= 39-50 | pmid=1509783 | doi= | pmc=2589377 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1509783 }}</ref> | |||
[[image:Cheyne Stokes.jpg|thumb|500px|Cheyne-Stokes respiration pattern - By Sav vas (Own work), via Wikimedia Commons<ref name="https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0, <"https://commons.wikimedia.org/wiki/File%3ABreathing_abnormalities.svg"></ref>]] | |||
** [[Altitude sickness]] | |||
** [[Brain injury]] | |||
** [[Brain tumors]] | |||
** [[Carbon monoxide poisoning]] | |||
** [[Pulmonary edema]] | |||
** [[Hyponatremia]] | |||
** High [[intracranial pressure]] | |||
** [[Renal failure]] | |||
** [[Toxic encephalopathy]] | |||
<br> | |||
== Biot's Respiration == | |||
{| align="right" | |||
|{{#ev:youtube|P7zvzDUcCCQ|500}} | |||
{{#ev:youtube|REeIL9a0_PM|500}} | |||
|} | |||
* Camille Biot, in 1878 distinguished Biot's respiration from Cheyne-Stokes, named it “rhythme meningitique”. | |||
* Biot's [[respiration]] is a kind of slow [[respiration]] pattern with periodic increasing 10-20 [[respiration]] per minute, without crescendo–decrescendo pattern. | |||
* Accelerations are different in a patient with Biot's respiration:<ref name="Wijdicks2006">{{cite journal|last1=Wijdicks|first1=E. F M|title=Biot's breathing|journal=Journal of Neurology, Neurosurgery & Psychiatry|volume=78|issue=5|year=2006|pages=512–513|issn=0022-3050|doi=10.1136/jnnp.2006.104919}}</ref> | |||
** Short and incomplete | |||
** Long and deep | |||
** Often interrupted by gasps | |||
* The periods are different in length, ended to a sigh just before the pause. | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
* The main causes of Biot's respiration include:<ref name="pmid21344052">{{cite journal| author=Casas-Méndez LF, Lujan M, Vigil L, Sansa G| title=Biot's breathing in a woman with fatal familial insomnia: is there a role for noninvasive ventilation? | journal=J Clin Sleep Med | year= 2011 | volume= 7 | issue= 1 | pages= 89-91 | pmid=21344052 | doi= | pmc=3041627 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21344052 }}</ref> | |||
** [[Pontine|Pontine lesions]] | |||
** Damage to the [[medulla oblongata]] | |||
*** [[Stroke]] | |||
*** [[Trauma]] | |||
*** Pressure on the [[medulla]] ([[Uncal herniation|uncal]] or [[Transtentorial herniation|tentorial herniation]]) | |||
** Prolonged [[opioid abuse]] | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
== Apneustic Respiration == | |||
* Apneustic respiration is first described in 1888 by Marckwald as prolonged [[inspiration]] arrest followed by inadequate [[expiration]]. | |||
* The rate of [[Apneustic respirations|apneustic breathing]] is about 1.5 breath per minute. | |||
* The main causes of [[Apneustic respirations|apneustic respiration]] include:<ref name="pmid2323256">{{cite journal |vauthors=Mador MJ, Tobin MJ |title=Apneustic breathing. A characteristic feature of brainstem compression in achondroplasia? |journal=Chest |volume=97 |issue=4 |pages=877–83 |date=April 1990 |pmid=2323256 |doi= |url=}}</ref> | |||
** [[Congenital]] [[Brain stem|brain-stem]] abnormalities | |||
** Upper [[pons]] damage secondary to:<ref name="WilkenLalley1997">{{cite journal|last1=Wilken|first1=B.|last2=Lalley|first2=P.|last3=Bischoff|first3=A.M.|last4=Christen|first4=H.J.|last5=Behnke|first5=J.|last6=Hanefeld|first6=F.|last7=Richter|first7=D.W.|title=Treatment of apneustic respiratory disturbance with a serotonin-receptor agonist|journal=The Journal of Pediatrics|volume=130|issue=1|year=1997|pages=89–94|issn=00223476|doi=10.1016/S0022-3476(97)70315-9}}</ref> | |||
*** [[Stroke]] | |||
*** [[Trauma]] | |||
*** [[Hypoxia]] | |||
** Severe [[brain injury]] | |||
** [[Ketamine]] (temporary) | |||
** [[Phenobarbital]] | |||
* [[Apneustic respirations|Apneustic respiration]] almost always carries a poor [[prognosis]] | |||
{{ | == Agonal Respiration == | ||
{| align="right" | |||
|{{#ev:youtube|CBMxH4xtE8w|500}} | |||
|} | |||
* Agonal [[breathing]] is slow, very shallow irregular [[Respiration|respirations]]. | |||
* Agonal [[breathing]] is resulted from [[anoxic brain injury]]. | |||
* The main causes of agonal [[breathing]] include:<ref name="pmid12042401">{{cite journal| author=Perkin RM, Resnik DB| title=The agony of agonal respiration: is the last gasp necessary? | journal=J Med Ethics | year= 2002 | volume= 28 | issue= 3 | pages= 164-9 | pmid=12042401 | doi= | pmc=1733591 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12042401 }}</ref> | |||
** [[Cardiac arrest]] | |||
** [[Stroke]] | |||
*** [[Cerebral ischemia]] | |||
*** [[Hemorrhagic stroke]] | |||
*** [[Cerebral hypoxia]] | |||
* The [[pathophysiology]] of agonal [[respiration]] in decreased [[blood flow]] to the [[brain]], which causes gasps. | |||
<br> | |||
<br> | |||
<br> | |||
== | == Kussmaul's Respiration == | ||
{| align="right" | |||
|{{#ev:youtube|raEKXVfuWTo|500}} | |||
|} | |||
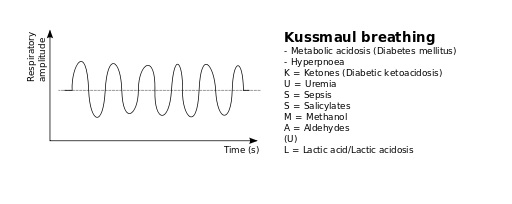
* The most important type of disturbed respiratory pattern; [[Kussmaul's respiration]] was first described by Adolf Kussmaul in 1874, as "[[air hunger]]".<ref name="pmid2757428" /> | |||
* Kussmaul's respiration is a deep, sighing [[respiration]] with normal or slow rate. | |||
* The main [[pathophysiology]] of Kussmaul's [[respiration]] is increased [[tidal volume]] without increasing [[respiratory rate]]. | |||
*# Compensating [[metabolic acidosis]] | |||
*# Stimulation of the [[respiratory center]] which is located in the [[brain stem]] by low [[serum]] [[pH]] | |||
*# Lowering of the [[partial pressure]] of [[CO2]] in the [[alveoli]] | |||
*# [[Hyperventilation]] | |||
* In primary stages of [[acidosis]], breathes are rapid and shallow, while they become deeper and slower in the later stages, which are called Kussmaul's respirations.<ref name="pmid26266145">{{cite journal| author=Seth P, Kaur H, Kaur M| title=Clinical Profile of Diabetic Ketoacidosis: A Prospective Study in a Tertiary Care Hospital. | journal=J Clin Diagn Res | year= 2015 | volume= 9 | issue= 6 | pages= OC01-4 | pmid=26266145 | doi=10.7860/JCDR/2015/8586.5995 | pmc=4525534 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26266145 }}</ref> | |||
* Main causes of Kussmaul's respiration include:<ref name="pmid2757428">{{cite journal |vauthors=Ammons MA, Moore EE, Moore FA |title=Increased incidence of cardiac contusion in patients with traumatic thoracic aortic rupture |journal=Ann. Surg. |volume=210 |issue=2 |pages=252–4 |date=August 1989 |pmid=2757428 |doi= |url=}}</ref> | |||
** [[Diabetic ketoacidosis]] | |||
** [[Renal failure]] | |||
** [[Metabolic acidosis|Metabolic (lactic) acidosis]] | |||
{| align="right" | |||
|[[image:Kussmaul.jpg|thumb|600px|Kussmaul's respiration pattern - By Sav vas (Own work), via Wikimedia Commons<ref name="https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0, <"https://commons.wikimedia.org/wiki/File%3ABreathing_abnormalities.svg"></ref>]] | |||
|} | |||
*** [[Heart failure]] | |||
*** [[Liver failure]] | |||
*** Chronic [[alcohol]] overuse | |||
*** [[Cancers]] | |||
*** [[Seizures]] | |||
*** Intense overuse of [[muscles]] (overexertion) | |||
*** Prolonged low [[blood sugar]] levels | |||
*** Prolonged elevated [[blood sugar]] levels | |||
** [[Toxic ingestion|Toxic ingestions]] | |||
*** [[Alcohols]] | |||
*** [[Salicylate toxicity]] | |||
*** [[Uremia]] | |||
*** [[Acetazolamide]] | |||
*** [[Ethylene glycol]] | |||
== Sighing Respiration == | |||
* Sighing [[respiration]] is a normal [[physiologic]] reaction of human body to [[fatigue]] and [[emotional]] changes. | |||
* Sigh is the elongated, often noisy [[expiration]] after [[inspiration]] of considerable amounts of air. | |||
* [[Dyspnea]] and [[shortness of breath]] are commonly contributed to sighing respiration. | |||
* Lack of efficient [[inspiration]] and [[expiration]] for several seconds is the main basic for sighing respiration. | |||
* The most common causes of sighing [[respiration]] are [[anxiety]] and [[depression]] syndromes.<ref name="pmid11964584">{{cite journal |vauthors=Patroniti N, Foti G, Cortinovis B, Maggioni E, Bigatello LM, Cereda M, Pesenti A |title=Sigh improves gas exchange and lung volume in patients with acute respiratory distress syndrome undergoing pressure support ventilation |journal=Anesthesiology |volume=96 |issue=4 |pages=788–94 |date=April 2002 |pmid=11964584 |doi= |url=}}</ref> | |||
{| class="wikitable" | |||
!Sigh syndrome manifestations<ref name="pmid18171560">{{cite journal |vauthors=Sody AN, Kiderman A, Biton A, Furst A |title=Sigh syndrome: is it a sign of trouble? |journal=J Fam Pract |volume=57 |issue=1 |pages=E1–5 |date=January 2008 |pmid=18171560 |doi= |url=}}</ref> | |||
|- | |||
|Recurrent deep [[inspiration]], between other normal [[Breathing|breathings]], by a prolonged and often noisy [[expiration]]. | |||
|- | |||
|Generally shallow [[respiration]]. | |||
|- | |||
|Patients sense the breathing as obstructive, weightened, and tough. | |||
|- | |||
|Some severe episodes may trigger ample [[stress]]. | |||
|- | |||
|Spontaneous episodes, without remarkable trigger or provocation. | |||
|- | |||
|The duration varies from few days to several weeks. | |||
|- | |||
|Without interruption of normal [[speech]]. | |||
|- | |||
|Not presented during [[sleep]]. | |||
|- | |||
|No relation with [[physical activity]] level. | |||
|- | |||
|Self limited, without need to [[urgent care]]. | |||
|} | |||
== References == | |||
{{reflist|2}} | |||
[[Category:Medicine]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Pulmonology]] | |||
[[Category:Cardiology]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 23:58, 29 July 2020
|
Respiratory Patterns |
|
Classification |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
Normal breathing is consisted of inhalation (sucking the air into the lungs) followed by exhalation (blowing the air out of the lungs). Every exhalation is followed by an automatic pause of about 2 second, before the next inhalation. Normal respiratory rate in a healthy adult is 12-20 per minutes. There are some conditions that may cause variation in rate and depth of respiration. Tachypnea is defined as increase in rate and decrease in depth of breathing. Bradypnea is a decrease in number of breath to less than 8-10 per minute in adults and 16 per minute in infants. Apnea is the respiratory arrest for couple of seconds. Cheyne-Stokes respiration is recurrent central apneustic episodes during sleep. Biot's respiration is a kind of slow respiration pattern with periodic increasing 10-20 respiration per minute, without crescendo–decrescendo pattern. Apneustic respiration is prolonged inspiration arrest followed by inadequate expiration. Agonal breathing is slow, very shallow irregular respirations. Kussmaul's respiration is a deep, sighing respiration with normal or slow rate. Sighing respiration is a normal physiologic reaction of human body to fatigue and emotional changes.
Eupnea
- Normal breathing is consisted of inhalation (sucking the air into the lungs) followed by exhalation (blowing the air out of the lungs).
- Every exhalation is followed by an automatic pause of about 2 second, before the next inhalation.
- Inhalation is an active process using diaphragm muscles, despite exhalation which is a passive process.
- Eupnea is the normal pattern of breathing with a rate of 10-12 per minute, each cycle is composed of:[1]
- Inhalation for 1.5-2 seconds
- Exhalation for 1.5-2 seconds
- Spontaneous stop of 2 seconds
- The main characteristics of eupnea are as following:[2]
- Slow
- Regular
- Nasal inhalation, oral exhalation
- Diaphragmatic
- Effortless
- Clear auscultation:
Normal respiratory rate in every age group is as following:
| Age group | Normal respiratory rate (Breath number per minute) |
|---|---|
| Infants | 30 to 60 |
| 1 to 3 years | 24 to 40 |
| 3 to 6 years | 22 to 34 |
| 6 to 12 years | 18 to 30 |
| 12 to 18 years | 12 to 16 |
Tachypnea
- Tachypnea is increased rate and decrease depth of breathing.
| Decreased plasma oxygen (hypoxemia) | Increased plasma CO2 (respiratory acidosis) | Decreased pulmonary compliance | Increased airway resistance | ||||||||||||||||||||||||||||||||||||||||||||
| Carotid body | Medullary chemoreceptors | Pulmonary or muscle mechanoreceptors | Airway receptors | ||||||||||||||||||||||||||||||||||||||||||||
| Tachypnea | |||||||||||||||||||||||||||||||||||||||||||||||
The main causes of tachypnea are classified into pulmonary, cardiovascular, hematologic, and metabolic pathophysiologies.[4]
Bradypnea
- Bradypnea is defined as decrease in respiratory rate to less than 8-10 per minute in adults and 16 per minute in infants.
- Mostly in bradypnea the exhalation phase is increased.
- The depth of breathes and tidal volume may be increased during bradypnea episodes.
- The main pathophysiology of bradypnea includes:[5]
- Desensitization of the medullary responses to PCO2
- Reduction in respiratory neuronal activity
- Inhibition of neural transmission within the respiratory center
- Neuronal damage to the brain stem
- The main causes of bradypnea are as following:[6]
| Causes | Other | ||
|---|---|---|---|
| Drugs | Opioids | Heroin | Can become worse when used along with: |
| Codeine | |||
| Hydrocodone | |||
| Morphine | |||
| Oxycodone | |||
| Toxins | Sodium azide |
| |
| Carbon monoxide | |||
| Other drugs | Sedatives |
| |
| Anesthetics | |||
| Systemic disease | Lung diseases | Emphysema | - |
| Chronic bronchitis | |||
| Severe asthma | |||
| Pneumonia | |||
| Pulmonary edema | |||
| Thyroid | Hypothyroidism | - | |
| Neuromuscular | Guillain-Barré syndrome |
| |
| Amyotrophic lateral sclerosis (ALS) | |||
Apnea
- Apnea is the respiratory arrest for couple of seconds.
- The most common form of apnea in generally healthy people is obstructive sleep apnea.
- The pathophysiology of sleep apnea are as following:[7]
| Apnea | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sleep disturbances | ↓O2, ↑CO2, ↓pH | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Excessive motor activity | Loss of deep sleep Sleep fragmentation | Brain malfunction | Severe CO2 retention | Systemic vasoconstriction | Pulmonary vasoconstriction | Vagal bradycardia Ectopic cardiac pulses | Decreased pulmonary pressure Increased cardiac afterload | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Restless sleep | Excessive daytime fatigue | Chronic hypoventilation | Systemic hypertension | Pulmonary hypertension | Unexplained nocturnal death | Left heart failure | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Intellectual deterioration | Right heart failure | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Personality change | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Behavioral disorder | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
To read more about sleep apnea, click here.
- The main causes of apnea include:[8]
Cheyne-Stokes Respiration
- Cheyne-Stokes respiration is recurrent central apneustic episodes during sleep.
- Tidal volume has crescendo-decrescendo pattern during Cheyne-Stokes respiration.
- Cheyne-Stokes respiration is almost always due to congestive heart failure, contributed with:[9]
- Patients with congestive heart failure who have already Cheyne-Stokes respiration pattern, would have more mortality rate.[10]
| Hypoxemia | Pulmonary vein congestion | Pulmonary C fibers stimulation | Spontaneous arousal | Increased circulating noradrenaline | Decreased cardiac output | Increased cardiac chamber size | Increased blood volume | Hyperventilation during day and night | Restrictive ventilatory defect | Decreased CO2 transfer capacity | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Peripheral chemoreceptor stimulation | Increased pulmonary vagal efferent activity | Increased sympathetic activity | Circulatory delay | Decreased total body CO2 | Decreased total body O2 | Increased pulmonary capillary wedge pressure | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hyperventilation | Length of the apnea-hyperpnea cycle | Crescendo-decrescendo respiratory pattern | Decreased blood gas buffering capacity | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cheyne-Stokes respiration | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Cheyne-Stokes respiration is mostly secondary to heart failure, but can be associated with following conditions:[12]
Biot's Respiration
| P7zvzDUcCCQ|500}}
{{#ev:youtube|REeIL9a0_PM|500}} |
- Camille Biot, in 1878 distinguished Biot's respiration from Cheyne-Stokes, named it “rhythme meningitique”.
- Biot's respiration is a kind of slow respiration pattern with periodic increasing 10-20 respiration per minute, without crescendo–decrescendo pattern.
- Accelerations are different in a patient with Biot's respiration:[14]
- Short and incomplete
- Long and deep
- Often interrupted by gasps
- The periods are different in length, ended to a sigh just before the pause.
- The main causes of Biot's respiration include:[15]
- Pontine lesions
- Damage to the medulla oblongata
- Stroke
- Trauma
- Pressure on the medulla (uncal or tentorial herniation)
- Prolonged opioid abuse
Apneustic Respiration
- Apneustic respiration is first described in 1888 by Marckwald as prolonged inspiration arrest followed by inadequate expiration.
- The rate of apneustic breathing is about 1.5 breath per minute.
- The main causes of apneustic respiration include:[16]
- Congenital brain-stem abnormalities
- Upper pons damage secondary to:[17]
- Severe brain injury
- Ketamine (temporary)
- Phenobarbital
- Apneustic respiration almost always carries a poor prognosis
Agonal Respiration
| CBMxH4xtE8w|500}} |
- Agonal breathing is slow, very shallow irregular respirations.
- Agonal breathing is resulted from anoxic brain injury.
- The main causes of agonal breathing include:[18]
- The pathophysiology of agonal respiration in decreased blood flow to the brain, which causes gasps.
Kussmaul's Respiration
| raEKXVfuWTo|500}} |
- The most important type of disturbed respiratory pattern; Kussmaul's respiration was first described by Adolf Kussmaul in 1874, as "air hunger".[19]
- Kussmaul's respiration is a deep, sighing respiration with normal or slow rate.
- The main pathophysiology of Kussmaul's respiration is increased tidal volume without increasing respiratory rate.
- Compensating metabolic acidosis
- Stimulation of the respiratory center which is located in the brain stem by low serum pH
- Lowering of the partial pressure of CO2 in the alveoli
- Hyperventilation
- In primary stages of acidosis, breathes are rapid and shallow, while they become deeper and slower in the later stages, which are called Kussmaul's respirations.[20]
- Main causes of Kussmaul's respiration include:[19]
 |
- Heart failure
- Liver failure
- Chronic alcohol overuse
- Cancers
- Seizures
- Intense overuse of muscles (overexertion)
- Prolonged low blood sugar levels
- Prolonged elevated blood sugar levels
- Toxic ingestions
Sighing Respiration
- Sighing respiration is a normal physiologic reaction of human body to fatigue and emotional changes.
- Sigh is the elongated, often noisy expiration after inspiration of considerable amounts of air.
- Dyspnea and shortness of breath are commonly contributed to sighing respiration.
- Lack of efficient inspiration and expiration for several seconds is the main basic for sighing respiration.
- The most common causes of sighing respiration are anxiety and depression syndromes.[21]
| Sigh syndrome manifestations[22] |
|---|
| Recurrent deep inspiration, between other normal breathings, by a prolonged and often noisy expiration. |
| Generally shallow respiration. |
| Patients sense the breathing as obstructive, weightened, and tough. |
| Some severe episodes may trigger ample stress. |
| Spontaneous episodes, without remarkable trigger or provocation. |
| The duration varies from few days to several weeks. |
| Without interruption of normal speech. |
| Not presented during sleep. |
| No relation with physical activity level. |
| Self limited, without need to urgent care. |
References
- ↑ St -John WM, Paton JF (December 2003). "Defining eupnea". Respir Physiol Neurobiol. 139 (1): 97–103. PMID 14637316.
- ↑ Ruangkittisakul A, Schwarzacher SW, Secchia L, Ma Y, Bobocea N, Poon BY, Funk GD, Ballanyi K (March 2008). "Generation of eupnea and sighs by a spatiochemically organized inspiratory network". J. Neurosci. 28 (10): 2447–58. doi:10.1523/JNEUROSCI.1926-07.2008. PMID 18322090.
- ↑ Browne GW, Pitchumoni CS (2006). "Pathophysiology of pulmonary complications of acute pancreatitis". World J Gastroenterol. 12 (44): 7087–96. PMC 4087768. PMID 17131469.
- ↑ Yurdakök M (October 2010). "Transient tachypnea of the newborn: what is new?". J. Matern. Fetal. Neonatal. Med. 23 Suppl 3: 24–6. doi:10.3109/14767058.2010.507971. PMID 20807157.
- ↑ Leung, Alexander K. C.; Schmitt, Marcus; Thomas, Christie P.; Sunderkötter, Cord; Schiller, Meinhard; Schwarz, Thomas; Berneburg, Mark; Kohlschütter, Alfried; Cerroni, Lorenzo; Direskeneli, Haner; Calamia, Kenneth; David, Gloria L.; Zeldin, Darryl C.; Schütte, Bärbel; Denson, Lee A.; Erhardt, Andreas; Kubitz, Ralf; Häussinger, Dieter; Sealey, Wendy M.; Mock, Donald M.; Wolf, Barry; Schumacher, Johannes; Propping, Peter; Metze, Dieter; Leung, Alexander K. C.; Wong, Andrew L.; Berneburg, Mark; Schwarz, Thomas; Hengstschläger, Markus; High, Whitney A.; Shroyer, Kenneth R.; McCready, M. Elizabeth; Bulman, Dennis E.; Afzal, Ali R.; Everman, David B.; Stoll, Claude; Darcan, Sukran; Kou, Yu Ru; Lin, You Shuei; Suzuki, Yoichi; Tada, Keiya; Leung, Alexander K. C.; Kupka, Susan; Dietmaier, Wolfgang; Hartmann, Arndt; Hennekam, Raoul C. M.; Belperio, John A.; Keane, Michael P.; Smith, M. Iain; Strieter, Robert M.; Molfino, Nestor A.; Sciandra, Francesca; Rossenbacker, Tom; Priori, Silvia G.; Senzolo, Marco; Triantos, Christos; Samonakis, Dimitrios; Cholongitas, Evangelos; Burroughs, Andrew K.; Mura, Marco; Braun-Falco, Markus; Hofmann, Silke; Bruckner-Tuderman, Leena (2009). "Bradypnea": 241–243. doi:10.1007/978-3-540-29676-8_246.
- ↑ Flisberg P, Jakobsson J, Lundberg J (March 2002). "Apnea and bradypnea in patients receiving epidural bupivacaine-morphine for postoperative pain relief as assessed by a new monitoring method". J Clin Anesth. 14 (2): 129–34. PMID 11943527.
- ↑ "Obstructive Sleep Apnea - National Library of Medicine - PubMed Health".
- ↑ Spicuzza L, Caruso D, Di Maria G (2015). "Obstructive sleep apnoea syndrome and its management". Ther Adv Chronic Dis. 6 (5): 273–85. doi:10.1177/2040622315590318. PMC 4549693. PMID 26336596.
- ↑ Nachtmann A, Siebler M, Rose G, Sitzer M, Steinmetz H (April 1995). "Cheyne-Stokes respiration in ischemic stroke". Neurology. 45 (4): 820–1. PMID 7723977.
- ↑ Hanly PJ, Zuberi-Khokhar NS (January 1996). "Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure". Am. J. Respir. Crit. Care Med. 153 (1): 272–6. doi:10.1164/ajrccm.153.1.8542128. PMID 8542128.
- ↑ Naughton, M T (1998). "Pathophysiology and treatment of Cheyne-Stokes respiration". Thorax. 53 (6): 514–518. doi:10.1136/thx.53.6.514. ISSN 0040-6376.
- ↑ Lieber C, Mohsenin V (1992). "Cheyne-Stokes respiration in congestive heart failure". Yale J Biol Med. 65 (1): 39–50. PMC 2589377. PMID 1509783.
- ↑ 13.0 13.1 CC BY-SA 3.0, <"https://commons.wikimedia.org/wiki/File%3ABreathing_abnormalities.svg">
- ↑ Wijdicks, E. F M (2006). "Biot's breathing". Journal of Neurology, Neurosurgery & Psychiatry. 78 (5): 512–513. doi:10.1136/jnnp.2006.104919. ISSN 0022-3050.
- ↑ Casas-Méndez LF, Lujan M, Vigil L, Sansa G (2011). "Biot's breathing in a woman with fatal familial insomnia: is there a role for noninvasive ventilation?". J Clin Sleep Med. 7 (1): 89–91. PMC 3041627. PMID 21344052.
- ↑ Mador MJ, Tobin MJ (April 1990). "Apneustic breathing. A characteristic feature of brainstem compression in achondroplasia?". Chest. 97 (4): 877–83. PMID 2323256.
- ↑ Wilken, B.; Lalley, P.; Bischoff, A.M.; Christen, H.J.; Behnke, J.; Hanefeld, F.; Richter, D.W. (1997). "Treatment of apneustic respiratory disturbance with a serotonin-receptor agonist". The Journal of Pediatrics. 130 (1): 89–94. doi:10.1016/S0022-3476(97)70315-9. ISSN 0022-3476.
- ↑ Perkin RM, Resnik DB (2002). "The agony of agonal respiration: is the last gasp necessary?". J Med Ethics. 28 (3): 164–9. PMC 1733591. PMID 12042401.
- ↑ 19.0 19.1 Ammons MA, Moore EE, Moore FA (August 1989). "Increased incidence of cardiac contusion in patients with traumatic thoracic aortic rupture". Ann. Surg. 210 (2): 252–4. PMID 2757428.
- ↑ Seth P, Kaur H, Kaur M (2015). "Clinical Profile of Diabetic Ketoacidosis: A Prospective Study in a Tertiary Care Hospital". J Clin Diagn Res. 9 (6): OC01–4. doi:10.7860/JCDR/2015/8586.5995. PMC 4525534. PMID 26266145.
- ↑ Patroniti N, Foti G, Cortinovis B, Maggioni E, Bigatello LM, Cereda M, Pesenti A (April 2002). "Sigh improves gas exchange and lung volume in patients with acute respiratory distress syndrome undergoing pressure support ventilation". Anesthesiology. 96 (4): 788–94. PMID 11964584.
- ↑ Sody AN, Kiderman A, Biton A, Furst A (January 2008). "Sigh syndrome: is it a sign of trouble?". J Fam Pract. 57 (1): E1–5. PMID 18171560.