Pulmonary embolism surgery
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism surgery On the Web |
|
Risk calculators and risk factors for Pulmonary embolism surgery |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients.[1]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
Inferior vena cava filter
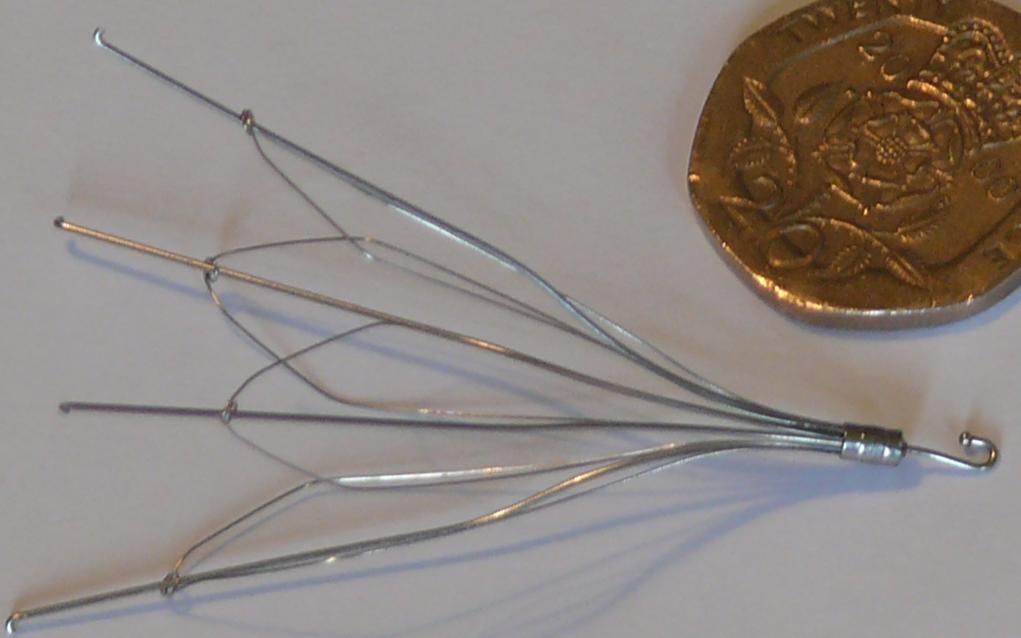
If anticoagulant therapy is contraindicated and/or ineffective, an inferior vena cava filter should be implanted[2]. It provides a filter in the inferior vena cava, allowing blood to pass through, while preventing large emboli from traveling from the lower extremities to the lung. IVC filters decreases PE recurrence but are not efficacious in preventing mortality[3].
In a study group comprising of 400 patients with proximal deep-vein thrombosis, which were followed for 2 years, it was found that the initial beneficial effect of vena caval filters for the prevention of pulmonary embolism was counterbalanced by an excess of recurrent deep-vein thrombosis, without any difference in mortality[2].
Embolectomy
Embolectomy is a process of removal of an embolus via a catheter or surgically. The procedure should be used when a high risk patient present with persistent hypotension and thrombolysis has either failed or is contraindicated.
To read more about embolectomy (types, procedure), click here.
References
- ↑ Augustinos P, Ouriel K (2004). "Invasive approaches to treatment of venous thromboembolism". Circulation. 110 (9 Suppl 1): I27–34. PMID 15339878.
- ↑ 2.0 2.1 Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral F, Huet Y, Simonneau G (1998). "A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group". N Engl J Med. 338 (7): 409–15. PMID 9459643.
- ↑ "Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study". Circulation. 112 (3): 416–22. 2005. doi:10.1161/CIRCULATIONAHA.104.512834. PMID 16009794. Retrieved 2011-12-13. Unknown parameter
|month=ignored (help)