Pulmonary embolism pathophysiology: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 18: | Line 18: | ||
=== Hemodynamic Consequences === | === Hemodynamic Consequences === | ||
*Hemodynamic complications | *Hemodynamic complications and the nature of the clinical manifestations of a pulmonary embolism depend on a number of factors:<ref name="Hellas">Kostadima, E., & Zakynthinos, E. (2007). Pulmonary Embolism: Pathophysiology, Diagnosis, Treatment. Hellenic Journal of Cardiology, 94-107.</ref> | ||
** The size of the embolus and the degree to which it occludes the vascular tree and its subsequent branches. | |||
** The presence of any preexisting cardiopulmonary conditions | ** The presence of any preexisting cardiopulmonary conditions | ||
** The role of chemical [[vasoconstriction]] as it is insinuated by platelets releasing [[serotonin]] and [[thromboxane]] which adhere to the embolus | ** The role of chemical [[vasoconstriction]] as it is insinuated by platelets releasing [[serotonin]] and [[thromboxane]] which adhere to the embolus | ||
** The presence of pulmonary artery dilatation and subsequent [[vasoconstriction|reflex vasoconstriction]]. | ** The presence of pulmonary artery dilatation and subsequent [[vasoconstriction|reflex vasoconstriction]]. | ||
* | * Pulmonary embolism results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the capillary by the embolism, but also due to pulmonary vasoconstriction. Pulmonary vasoconstriction can be either biochemically mediated, hypoxia induced, or reflex-induced. (1555481)(11033105) | ||
** | |||
** | * Several mediators are involved the pulmonary vasoconstriction that occurs in the setting of acute PE, such as: | ||
* | ** Thromboxane A2 (end product of arachidonic acid metabolism) (11033105) | ||
** Serotonin (vasoconstrictor in the pulmonary circulation and vasodilator in the systemic circulation) (11033105) | |||
* | ** Endothelin 1 (11033105) | ||
** Prostaglandin F2alpha (11033105) | |||
** Thrombin (14656907) | |||
** Histamine (14656907) | |||
* While serotonin and thromboxane A2 are mainly produced by activated platelets, the vascular wall and pulmonary endocrine cells might also be the source of vasoconstrictors. (11033105) | |||
* When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular afterload leads to the dilatation of the RV wall and subsequent right heart failure. In addition, the elevated pulmonary vascular resistance causes a decrease in the left ventricular preload and consequently leads to systemic hypotension. (3916797)(7484782) In patients with underlying cardiopulmonary disease, the [[cardiac output]] suffers substantial deterioration in overall output as compared to otherwise healthy individuals. | |||
* Right heart failure, as well as systemic hypotension, can contribute to decrease coronary perfusion and subsequent coronary ischemia. (3916797)(7484782) | |||
* In summary, the hemodynamic consequences of PE include: | |||
**[[Pulmonary hypertension]] | **[[Pulmonary hypertension]] | ||
**[[Right ventricular strain]] | **[[Right ventricular strain]] | ||
**[[Congestive heart failure]] | **[[Congestive heart failure]] | ||
**[[ | **[[Systemic hypotension]] | ||
* | |||
* | ====Adaptive Mechanisms==== | ||
*Prostacyclin is a vasodilator produced by the endothelial cells in response to the hemodynamic changes induced by the acute PE. (11033105) | |||
**[[ | * Changes in the the right ventricle occur as an adaptative mechanism of the right ventricle to preserve pulmonary perfusion. Without these adapations, a pulmonary embolism will lead to [[right heart failure]].<ref name="pmid6488744">{{cite journal| author=Benotti JR, Dalen JE| title=The natural history of pulmonary embolism. | journal=Clin Chest Med | year= 1984 | volume= 5 | issue= 3 | pages= 403-10 | pmid=6488744 | doi= | pmc= | url= }}</ref> These adaptations aim to: | ||
** | **Generate a [[systolic blood pressure]] in excess of 50 mmHg | ||
**Maintain an average pulmonary artery pressure of approximately 40 mmHg | |||
=== Mechanism === | === Mechanism === | ||
Revision as of 19:29, 7 July 2014
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism pathophysiology On the Web |
|
Directions to Hospitals Treating Pulmonary embolism pathophysiology |
|
Risk calculators and risk factors for Pulmonary embolism pathophysiology |
Editor(s)-In-Chief: C. Michael Gibson, M.S., M.D. [1], The APEX Trial Investigators; Associate Editor(s)-in-Chief:
Overview
Pulmonary embolism occurs when there is an acute obstruction of the pulmonary artery or one of its branches. It is commonly caused by a venous thrombus that has dislodged from its site of formation and embolized to the arterial blood supply of one of the lungs. The process of clot formation and embolization is termed thromboembolism.
Pathophysiology
Clot Formation
- Most pulmonary emboli commonly originate in the iliofemoral vein, deep within the vasculature of the lower extremity.
- Less commonly, a pulmonary embolism may also arise in the upper extremity veins, renal veins, or pelvic veins.
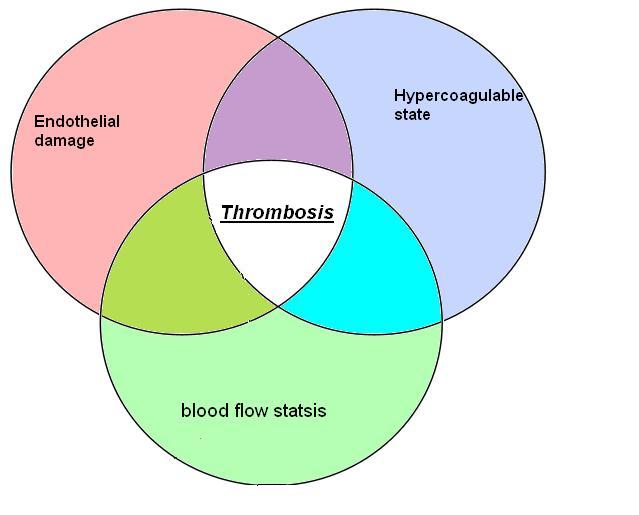
- The development of thrombosis is classically due to a group of conditions referred to as Virchow's triad. Virchow's triad includes alterations in blood flow, factors in the vessel wall, and factors affecting the properties of the blood. It is common for more than one risk factor to be present. Shown below is an image depicting Virchow's triad.
Embolization
- After formation, a thrombus might dislodge from the site of origin and circulate through the inferior vena cava, into the right ventricle, and into the pulmonary vasculature.[1]
Hemodynamic Consequences
- Hemodynamic complications and the nature of the clinical manifestations of a pulmonary embolism depend on a number of factors:[2]
- The size of the embolus and the degree to which it occludes the vascular tree and its subsequent branches.
- The presence of any preexisting cardiopulmonary conditions
- The role of chemical vasoconstriction as it is insinuated by platelets releasing serotonin and thromboxane which adhere to the embolus
- The presence of pulmonary artery dilatation and subsequent reflex vasoconstriction.
- Pulmonary embolism results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the capillary by the embolism, but also due to pulmonary vasoconstriction. Pulmonary vasoconstriction can be either biochemically mediated, hypoxia induced, or reflex-induced. (1555481)(11033105)
- Several mediators are involved the pulmonary vasoconstriction that occurs in the setting of acute PE, such as:
- Thromboxane A2 (end product of arachidonic acid metabolism) (11033105)
- Serotonin (vasoconstrictor in the pulmonary circulation and vasodilator in the systemic circulation) (11033105)
- Endothelin 1 (11033105)
- Prostaglandin F2alpha (11033105)
- Thrombin (14656907)
- Histamine (14656907)
- While serotonin and thromboxane A2 are mainly produced by activated platelets, the vascular wall and pulmonary endocrine cells might also be the source of vasoconstrictors. (11033105)
- When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular afterload leads to the dilatation of the RV wall and subsequent right heart failure. In addition, the elevated pulmonary vascular resistance causes a decrease in the left ventricular preload and consequently leads to systemic hypotension. (3916797)(7484782) In patients with underlying cardiopulmonary disease, the cardiac output suffers substantial deterioration in overall output as compared to otherwise healthy individuals.
- Right heart failure, as well as systemic hypotension, can contribute to decrease coronary perfusion and subsequent coronary ischemia. (3916797)(7484782)
- In summary, the hemodynamic consequences of PE include:
Adaptive Mechanisms
- Prostacyclin is a vasodilator produced by the endothelial cells in response to the hemodynamic changes induced by the acute PE. (11033105)
- Changes in the the right ventricle occur as an adaptative mechanism of the right ventricle to preserve pulmonary perfusion. Without these adapations, a pulmonary embolism will lead to right heart failure.[3] These adaptations aim to:
- Generate a systolic blood pressure in excess of 50 mmHg
- Maintain an average pulmonary artery pressure of approximately 40 mmHg
Mechanism
The diagram below summarizes the sequence of pathophysiologic events in pulmonary embolism:[4]

References
- ↑ McGill University. (2004, June 24). Pulmonary Embolism. Retrieved May 7, 2012, from McGill Virtual Stethoscope Pathophysiology.
- ↑ Kostadima, E., & Zakynthinos, E. (2007). Pulmonary Embolism: Pathophysiology, Diagnosis, Treatment. Hellenic Journal of Cardiology, 94-107.
- ↑ Benotti JR, Dalen JE (1984). "The natural history of pulmonary embolism". Clin Chest Med. 5 (3): 403–10. PMID 6488744.
- ↑ Fengler BT, Brady WJ (2009). "Fibrinolytic therapy in pulmonary embolism: an evidence-based treatment algorithm". Am J Emerg Med. 27 (1): 84–95. doi:10.1016/j.ajem.2007.10.021. PMID 19041539. Retrieved 2011-12-21. Unknown parameter
|month=ignored (help)