Pulmonary embolism pathophysiology: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 10: | Line 10: | ||
* Most pulmonary emboli commonly originate in the [[iliofemoral vein]], deep within the vasculature of the lower extremity. | * Most pulmonary emboli commonly originate in the [[iliofemoral vein]], deep within the vasculature of the lower extremity. | ||
* Less commonly, a pulmonary embolism may also arise in the upper extremity veins, renal veins, or pelvic veins. | * Less commonly, a pulmonary embolism may also arise in the upper extremity veins, renal veins, or pelvic veins. | ||
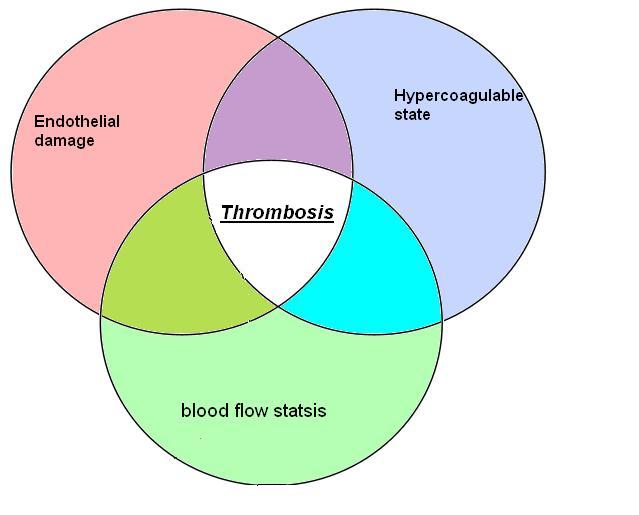
* The development of thrombosis is classically due to a group of causes referred to as [[Virchow's triad]]. Virchow's triad includes alterations in [[blood flow]], factors in the vessel wall, and factors affecting the properties of the [[blood]]. It is common for more than one risk factor to be present. Shown below is an image depicting [[Virchow's triad]]. | * The development of thrombosis is classically due to a group of causes referred to as [[Virchow's triad]]. Virchow's triad includes alterations in [[blood flow]], factors in the vessel wall, and factors affecting the properties of the [[blood]]. It is common for more than one risk factor to be present. Shown below is an image depicting [[Virchow's triad]]. | ||
Revision as of 18:46, 7 July 2014
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism pathophysiology On the Web |
|
Directions to Hospitals Treating Pulmonary embolism pathophysiology |
|
Risk calculators and risk factors for Pulmonary embolism pathophysiology |
Editor(s)-In-Chief: C. Michael Gibson, M.S., M.D. [1], The APEX Trial Investigators; Associate Editor(s)-in-Chief:
Overview
Pulmonary embolism occurs when there is an acute obstruction of the pulmonary artery or one of its branches. It is commonly caused by a venous thrombus that has dislodged from its site of formation and embolized to the arterial blood supply of one of the lungs. The process of clot formation and embolization is termed thromboembolism.
Pathophysiology
Clot Formation
- Most pulmonary emboli commonly originate in the iliofemoral vein, deep within the vasculature of the lower extremity.
- Less commonly, a pulmonary embolism may also arise in the upper extremity veins, renal veins, or pelvic veins.
- The development of thrombosis is classically due to a group of causes referred to as Virchow's triad. Virchow's triad includes alterations in blood flow, factors in the vessel wall, and factors affecting the properties of the blood. It is common for more than one risk factor to be present. Shown below is an image depicting Virchow's triad.
Embolization
- After formation, a thrombus will travel from the site of origin and circulate through the inferior vena cava into the right ventricle and on into the pulmonary vasculature where it will lodge.[1]
- Depending upon the patient, there can be one or many pulmonary emboli present. The size of the clot(s) and their physiologic impact will depend largely on the individual patient and subsequent anatomy of the vasculature. [1]
Hemodynamic Consequences
- Hemodynamic complications arise as a result of the obstruction of flow within the pulmonary arteries.
- In circumstances where more than two-thirds of the pulmonary artery is occluded, the right ventricle needs to find ways to preserve pulmonary perfusion. Some of the adaptative mechanism of the right ventricle are as follows:
- Generate a systolic blood pressure in excess of 50 mmHg.
- Maintain an average pulmonary artery pressure of approximately 40 mmHg.
- Without these adapations, a pulmonary embolism will lead to right heart failure.[2]
- Additional complications include the following:[1]
- Increased resistence in the pulmonary vessels.
- Pulmonary hypertension
- Right ventricular strain
- Congestive heart failure
- Vasoconstriction
- In patients with underlying cardiopulmonary disease, the cardiac output suffers substantial deterioration in overall output as compared to otherwise healthy individuals.
- In patients with coexisting coronary artery disease, right ventricular failure is more common following a pulmonary embolism as compared to those without coexisting CAD.
- In 10% of all pulmonary embolism cases, the pulmonary embolism develops into a pulmonary infarction. This is an exceedingly rare complication.[1]
- Long term complications:[1]
Mechanism
The diagram below summarizes the sequence of pathophysiologic events in pulmonary embolism:[3]

References
- ↑ 1.0 1.1 1.2 1.3 1.4 McGill University. (2004, June 24). Pulmonary Embolism. Retrieved May 7, 2012, from McGill Virtual Stethoscope Pathophysiology.
- ↑ Benotti JR, Dalen JE (1984). "The natural history of pulmonary embolism". Clin Chest Med. 5 (3): 403–10. PMID 6488744.
- ↑ Fengler BT, Brady WJ (2009). "Fibrinolytic therapy in pulmonary embolism: an evidence-based treatment algorithm". Am J Emerg Med. 27 (1): 84–95. doi:10.1016/j.ajem.2007.10.021. PMID 19041539. Retrieved 2011-12-21. Unknown parameter
|month=ignored (help)