Iron deficiency anemia
For patient information on iron deficiency anemia in adults, click here
For patient information on iron deficiency anemia in children, click here
| Iron deficiency anemia | |
 | |
|---|---|
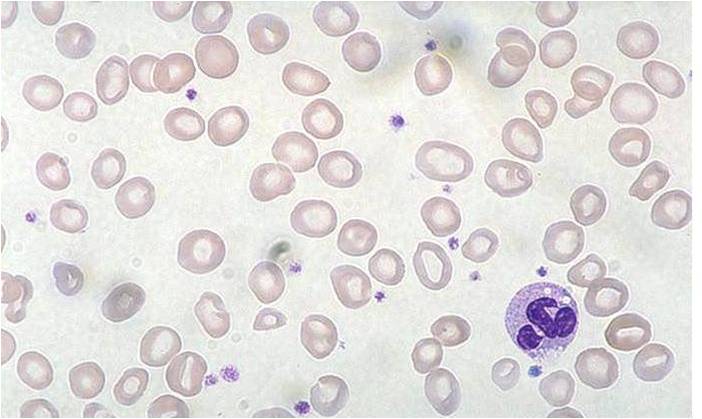
| Peripheral blood: Iron deficiency anemia | |
| ICD-10 | D50 |
| ICD-9 | 280 |
| DiseasesDB | 6947 |
| MedlinePlus | 000584 |
| MeSH | D018798 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Iron deficiency anemia is the most common type of anemia, and the most common cause of microcytic anemia.
Iron deficiency anemia occurs when the dietary intake or absorption of iron is insufficient, and hemoglobin, which contains iron, cannot be formed. In the United States, 20% of all women of childbearing age have iron deficiency anemia, compared with only 2% of adult men. The principal cause of iron deficiency anemia in premenopausal women is blood lost during menses.
Iron deficiency anemia is the final stage of iron deficiency. When the body has sufficient iron to meet its needs (functional iron), the remainder is stored for later use in the bone marrow, liver, and spleen. Iron deficiency ranges from iron depletion, which yields little physiological damage, to iron deficiency anemia, which can affect the function of numerous organ systems. Iron depletion causes the amount of stored iron to be reduced, but has no effect on the functional iron. However, a person with no stored iron has no reserves to use if the body requires more iron. In essence, the amount of iron absorbed by the body is not adequate for growth and development or to replace the amount lost.
History
A disease believed to be iron deficiency anemia is described in about 1500 B.C. in the Egyptian Ebers papyrus. It was termed chlorosis or green sickness in Medieval Europe, and iron salts were used for treatment in France by the mid-17th century. Thomas Sydenham recommended iron salts as treatment for chlorosis, but treatment with iron was controversial until the 20th century, when its mechanism of action was more fully elucidated.
Pathophysiology of Iron Deficiency
Iron deficiency (or "sideropenia") is the most common known form of nutritional deficiency. In the human body, iron is present in all cells and has several vital functions—as a carrier of oxygen to the tissues from the lungs in the form of hemoglobin, as a transport medium for electrons within the cells in the form of cytochromes, and as an integral part of enzyme reactions in various tissues. Too little iron can interfere with these vital functions and lead to morbidity and mortality.
The direct consequence of iron deficiency is iron deficiency anemia. Groups that are most prone to developing this disease are children and pre-menopausal women.
Total body iron averages approximately 3.8 g in men and 2.3 g in women. There are several mechanisms that control human iron metabolism and safeguard against iron deficiency. The main regulatory mechanism is situated in the gastrointestinal tract. When loss of iron is not sufficiently compensated by adequate intake after some time that is determined by the state of body iron storage, iron deficiency develops.
Causes
- chronic bleeding (hemoglobin contains iron)
- excessive menstrual bleeding
- non-menstrual bleeding
- bleeding from the gastrointestinal tract (ulcers, hemorrhoids, etc.)
- rarely laryngological bleeding or from the respiratory tract
- inadequate intake (special diets low in dietary iron)
- substances (in diet or drugs) interfering with iron absorption
- malabsorption syndromes
Though genetic defects causing iron deficiency have been studied in rodents, there are no known genetic disorders of human iron metabolism that directly cause iron deficiency.
Symptoms
Symptoms of iron deficiency can occur even before the condition has progressed to iron deficiency anemia.
Symptoms of iron deficiency are not unique to iron deficiency (i.e. not pathognomonic). Iron is needed for many enzymes to function normally, so a wide range of symptoms may eventually emerge, either as the secondary result of the anemia, or as other primary results of iron deficiency. Main symptoms of iron deficiency include:
In severe cases, dyspnea can occur. Unusual obsessive food cravings, known as pica, may develop. Hair loss and lightheadedness can also be associated with iron deficiency anemia.
Other symptoms
Other symptoms patients with iron deficiency anemia have reported are:
- Constipation
- Tinnitus
- Palpitations
- Seeing Bright Colors
- Fainting, Feeling faint
- Depression
- Weakness
- Breathlessness
- Twitching Nerves, Tingling, Numbness
- Burning sensations
- Sleep apnea (rare)
- Missed menstrual cycle
- heavy menstrual cycle
- weak/ brittle nails
- slow social development
- lethargia
- no "get up and go"
- hair loss
- sore/ swollen tongue
- poor skin color
- weak immune system
- exhaustion
- loss of desire for food
Diagnosis
Anemia will be diagnosed on the basis of suggestive symptoms, or found on the basis of routine testing, which includes a complete blood count (CBC). A sufficiently low hemoglobin or hematocrit value is diagnostic of anemia, and further studies will be undertaken to determine its cause. One of the first abnormal values to be noted on a CBC will be a high red blood cell distribution width (RDW), reflecting a varied size distribution of red blood cells. A low MCV, MCH or MCHC, and the appearance of the RBCs on visual examination of a peripheral blood smear will narrow the diagnosis to a microcytic anaemia. Microcytic anemia can also be the result of malabsorption phenomena associated with gluten-sensitive enteropathy/coeliac disease.
The diagnosis of iron deficiency anemia will be suggested by appropriate history (e.g., anemia in a menstruating woman), and by such diagnostic tests as a low serum ferritin, a low serum iron level, an elevated serum transferrin and a high total iron binding capacity (TIBC). Serum ferritin is the most sensitive lab test for iron deficiency anemia.[1]
| Change | Parameter |
|---|---|
| Decrease | ferritin, hemoglobin, MCV |
| Increase | TIBC, transferrin, RDW |
Iron deficient anemia and Thalassemia Minor present with many of the same lab results. It is very important not to treat a patient with Thalassemia with an iron supplement as this can lead to hemochromatosis (accumulation of iron in the liver) A hemoglobin electrophoresis would provide useful evidence in distinguishing these two conditions, along with iron studies.
Gold standard
A definitive diagnosis requires a demonstration of depleted body iron stores by performing a bone marrow aspiration, with the marrow stained for iron. Because this is invasive and painful, while a clinical trial of iron supplementation is inexpensive and non-traumatic, patients are often treated without a definitive diagnosis.
Determination of etiology
The diagnosis of iron deficiency anemia requires further investigation as to its cause. It can be a sign of other disease, such as colon cancer, which will cause the loss of blood in the stool. In adults, 60% of patients with iron deficiency anemia may have underlying gastrointestinal disorders leading to chronic blood loss.[2]. In addition to dietary insufficiency, malabsorption, chronic blood loss, diversion of iron to fetal erythropoiesis during pregnancy, intravascular haemolysis and haemoglobinuria or other forms of chronic blood loss should all be considered.
Likely lab test results in people with iron deficiency
- A full blood count would likely reveal microcytic anemia [3]
- Low serum ferritin
- Low serum iron
- High TIBC (total iron binding capacity)
- It is possible that the fecal occult blood test might be positive, if iron deficiency is the result of gastrointestinal bleeding.
As always, laboratory values have to be interpreted with the lab's reference values in mind and considering all aspects of the individual clinical situation.
Serum ferritin can be elevated in inflammatory conditions and so a normal serum ferritin may not always exclude iron deficiency.
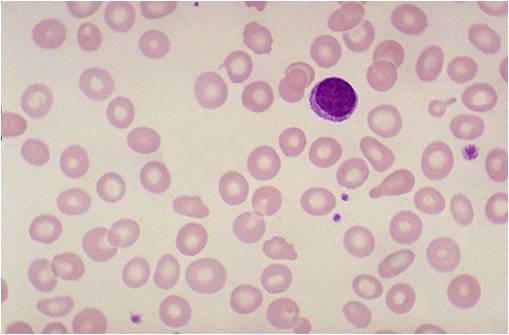
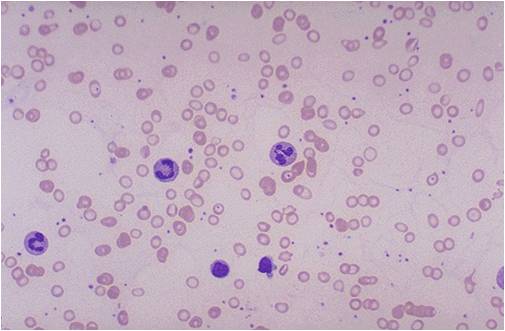
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey)
Treatment
Before any treatment is commenced there should be definitive diagnosis of the underlying cause for iron deficiency, particularly in older patients who are most susceptible to colorectal cancer and the gastrointestinal bleeding it often causes. In adults, 60% of patients with iron deficiency anemia may have underlying gastrointestinal disorders leading to chronic blood loss.[2]
It is likely that the cause of the iron deficiency will need treatment as well.
If the cause is dietary iron deficiency, iron supplements, usually with iron (II) sulfate, ferrous gluconate, or iron amino acid chelate NaFeEDTA, will usually correct the anemia.
Recent research suggests the replacement dose of iron, at least in the elderly with iron deficiency, may be as little as 15 mg per day of elemental iron [4].
There can be a great difference between iron intake and iron absorption, also known as bioavailability. Scientific studies indicate iron absorption problems when iron is taken in conjunction with milk, tea, coffee and other substances. There are already a number of proven solutions for this problem, including:
- Fortification with ascorbic acid, which increases bioavailability in both presence and absence of inhibiting substances, but which is subject to deterioration from moisture or heat. Ascorbic acid fortification is usually limited to sealed dried foods, but individuals can easily take ascorbic acid with basic iron supplement for the same benefits.
- Microencapsulation with lecithin, which binds and protects the iron particles from the action of inhibiting substances. The primary benefit over ascorbic acid is durability and shelf life, particularly for products like milk which undergo heat treatment.
- Using an iron amino acid chelate, such as NaFeEDTA, which similarly binds and protects the iron particles. A study performed by the Hematology Unit of the University of Chile indicates that chelated iron (ferrous bis-glycine chelate) can work with ascorbic acid to achieve even higher absorption levels [5].
- Separating intake of iron and inhibiting substances by a couple of hours.
- Using goats milk instead of cows milk.
- Gluten-free diet resolves some instances of iron-deficiency anemia.
Iron bioavailability comparisons require stringent controls, because the largest factor affecting bioavailability is the subject's existing iron levels. Informal studies on bioavailability usually do not take this factor into account, so exaggerated claims from health supplement companies based on this sort of evidence should be ignored. Scientific studies are still in progress to determine which approaches yield the best results and the lowest costs.
If anemia does not respond to oral treatments, it may be necessary to administer iron parenterally (e.g., as iron dextran) using a drip or haemodialysis. Parenteral iron involves risks of fever, chills, backache, myalgia, dizziness, syncope, rash, anaphylactic shock[6] and secondary iron overload. Epinephrine is used to counter anaphylactic shock, and Chelation therapy is used to manage secondary iron overload [7].
A follow up blood test is essential to demonstrate whether the treatment has been effective.
Note that iron supplements must be kept out of the reach of children, as iron-containing supplements are a frequent cause of poisoning in the pediatric age group.
Food sources of Iron
Iron deficiency can have serious health consequences that diet may not be able to quickly correct, and iron supplementation is often necessary if the iron deficiency has become symptomatic. However, mild iron deficiency can be corrected, and prevented, by eating iron-rich foods. Because iron is an absolute requirement for most of the earth's plants and animals, a wide range of food can provide iron. However, these foods are absorbed and processed differently by the body; for instance, iron from meat (heme iron source) is more easily broken down and absorbed than iron in grains (nonheme iron source), and minerals and chemicals in one type of food may inhibit absorption of iron from another type of food eaten at the same time.[3] Because iron from plant sources is less easily absorbed than the heme-bound iron of animal sources, vegetarians and vegans should have a somewhat higher total daily iron intake than those who eat meat, fish or poultry.[4] Legumes and dark-green leafy vegetables like broccoli, kale and oriental greens are especially good sources of iron for vegetarians and vegans. However, spinach and swiss chard contain oxalates which bind iron making it largely unavailable for absorption. Iron from nonheme sources is more readily absorbed if consumed with foods that contain either heme-bound iron or vitamin C. [5]
| Food | Serving size |
Miligrams per serving |
% DV* |
|---|---|---|---|
| Chicken liver (cooked) | 3˝ ounces | 12.8 | 70 |
| Oysters(breaded and fried) | 6 pieces | 4.5 | 25 |
| Beef, chuck (lean, braised) | 3 ounces | 3.2 | 20 |
| Clams (breaded, fried) | 1 cup | 3.0 | 15 |
| Beef tenderloin (roasted) | 3 ounces | 3.0 | 15 |
| Turkey ( dark meat, roasted) | 3˝ ounces | 2.3 | 10 |
| Beef, eye of round (roasted) | 3 ounces | 2.2 | 10 |
| Turkey, light meat (roasted) | 3˝ ounces | 1.6 | 8 |
| Chicken, leg, meat only (roasted) | 3˝ ounces | 1.3 | 6 |
| Tuna, fresh bluefin (cooked) | 3 ounces | 1.1 | 6 |
| Chicken breast (roasted) | 3 ounces | 1.1 | 6 |
| Halibut (cooked) | 3 ounces | 0.9 | 6 |
| Blue crab (cooked) | 3 ounces | 0.8 | 4 |
| Pork loin (broiled) | 3 ounces | 0.8 | 4 |
| Tuna white (canned in water) | 3 ounces | 0.8 | 4 |
| Shrimp (mixed species, cooked) | 4 large | 0.7 | 4 |
| Food | Serving size |
Miligrams per serving |
% DV* |
|---|---|---|---|
| Ready-to-eat cereal (100% iron fortified | cup | 18.0 | 100 |
| Oatmeal, instant, fortified (prepared with water | 1 cup | 10.0 | 60 |
| Soybeans, mature (boiled) | 1 cup | 8.8 | 50 |
| Lentils (boiled) | 1 cup | 6.6 | 35 |
| Kidney beans mature (boiled) | 1 cup | 5.2 | 25 |
| Lima beans large, mature (boiled) | 1 cup | 4.5 | 25 |
| Navy beans mature (boiled) | 1 cup | 4.5 | 25 |
| Ready-to-eat cereal (25% iron fortified) | 1 cup | 4.5 | 25 |
| Black beans mature (boiled) | 1 cup | 3.6 | 20 |
| Pinto beans mature (boiled) | 1 cup | 3.6 | 20 |
| Molasses (blackstrap) | 1 tablespoon | 3.5 | 20 |
| Tofu (raw, firm) | ˝ cup | 3.4 | 20 |
| Spinach (boiled, drained) | ˝ cup | 3.2 | 20 |
| Spinach (canned, drained solids) | ˝ cup | 2.5 | 10 |
| Black-eyed peas (cowpeas) (boiled) | ˝ cup | 1.8 | 10 |
| Spinach (frozen, chopped, boiled) | ˝ cup | 1.9 | 10 |
| Grits (white, enriched | 1 cup | 1.5 | 8 |
| Raisins (seedless, packed) | ˝ cup | 1.5 | 8 |
| Whole wheat bread | 1 slice | 0.9 | 6 |
| White bread (enriched) | 1 slice | 0.9 | 6 |
Consequences
Continued iron deficiency may progress to anemia and worsening fatigue. Thrombocytosis, or an elevated platelet count, can also result. A lack of iron in the blood is a reason that some people cannot donate blood.
See also
References
- ↑ Guyatt G, Patterson C, Ali M, Singer J, Levine M, Turpie I, Meyer R (1990). "Diagnosis of iron-deficiency anemia in the elderly". Am J Med. 88 (3): 205–9. PMID 2178409.
- ↑ 2.0 2.1 Rockey D, Cello J (1993). "Evaluation of the gastrointestinal tract in patients with iron-deficiency anemia". N Engl J Med. 329 (23): 1691–5. PMID 8179652.
- ↑ Longmore, Murray (2004). Oxford Handbook of Clinical Medicine, 6th Edn. Oxford University Press. pp. pp. 626-628. ISBN 0-19-852558-3. Unknown parameter
|coauthors=ignored (help) - ↑ Rimon E, Kagansky N, Kagansky M, Mechnick L, Mashiah T, Namir M, Levy S (2005). "Are we giving too much iron? Low-dose iron therapy is effective in octogenarians". Am J Med. 118 (10): 1142–7. doi:10.1016/j.amjmed.2005.01.065. PMID 16194646.
- ↑ Olivares M, Pizarro F, Pineda O, Name JJ, Hertrampf E, Walter T. (1997). "Milk inhibits and ascorbic acid favors ferrous bis-glycine chelate bioavailability in humans". J Nutr. 127 (7): 1407–11. PMID 9202099. Unknown parameter
|month=ignored (help) - ↑ http://www.globalrph.com/irondextran.htm
- ↑ James P. Kushner, John P. Porter and Nancy F. Olivieri (2001). "Secondary Iron Overload". Hematology. PMID 11722978. http://asheducationbook.hematologylibrary.org/cgi/content/full/2001/1/47
Sources
- Recommendations to Prevent and Control Iron Deficiency in the United States
- http://www.nlm.nih.gov/medlineplus/ency/article/000584.htm
- http://www.nlm.nih.gov/medlineplus/ency/article/007134.htm
Template:SIB Template:Hematology Template:Nutritional pathology da:Jernmangel de:Eisenmangelanämie el:Σιδηροπενική αναιμία nl:IJzergebreksanemie