Granulomatosis with polyangiitis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
===Click [[The Heart in Wegener's Granulomatosis|here]] for The heart in Wegener's granulomatosis=== | ===Click [[The Heart in Wegener's Granulomatosis|here]] for The heart in Wegener's granulomatosis=== | ||
==Overview== | ==[[Wegener's granulomatosis overview|Overview]]== | ||
== | ==[[Wegener's granulomatosis historical perspective|Historical Perspective]]== | ||
==Epidemiology== | ==Epidemiology== | ||
Revision as of 18:48, 21 September 2011
For patient information click here Template:DiseaseDisorder infobox
|
Granulomatosis with polyangiitis Microchapters |
|
Differentiating Granulomatosis with polyangiitis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Granulomatosis with polyangiitis On the Web |
|
American Roentgen Ray Society Images of Granulomatosis with polyangiitis |
|
Directions to Hospitals Treating Granulomatosis with polyangiitis |
|
Risk calculators and risk factors for Granulomatosis with polyangiitis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Click here for The heart in Wegener's granulomatosis
Overview
Historical Perspective
Epidemiology
The incidence is 10 cases per million per year.[1] 90% of the patients are whites. While it mainly occurs in the middle-aged, it has been reported in much younger and older patients.
Pathophysiology
Inflammation with granuloma formation against a nonspecific inflammatory background is the classical tissue abnormality in all organs affected by Wegener's granulomatosis.[2]
It is now widely presumed that the anti-neutrophil cytoplasmic antibodies (ANCAs) are responsible for the inflammation in Wegener's.[2] The typical ANCAs in Wegener's are those that react with proteinase 3, an enzyme prevalent in neutrophil granulocytes.[3] This type of ANCA is also known as cANCA, with the c indicating cytoplasmic (in contrast to pANCA, which is perinuclear).
ANCAs activate neutrophils, increase their adherence to endothelium, and lead to their degranulation. This causes extensive damage to the vessel wall, particularly of arterioles.[2]
The exact cause for the production of ANCAs is unknown, although some drugs have been implicated in secondary forms of Wegener's. As with many autoimmune disorders, the cause is probably genetic predisposition combined with molecular mimicry caused by a virus or bacterium.
Signs and symptoms
Initial signs are protean, and diagnosis can be severely delayed due to the non-specific nature of the symptoms. The rhinitis is generally the first sign in most patients.[2]
- Upper airway, eye and ear disease:
- Nose: pain, stuffiness, nosebleeds, rhinitis, crusting, saddle-nose deformity due to a perforated septum
- Ears: conductive hearing loss due to Eustachian tube dysfunction, sensorineural hearing loss (unclear mechanism)
- Eyes: pseudotumours, scleritis, conjunctivitis, uveitis, episcleritis
- Airways:
- Trachea: subglottal stenosis
- Lungs: pulmonary nodules (referred to as "coin lesions"), infiltrates (often interpreted as pneumonia), cavitary lesions, pulmonary hemorrhage causing hemoptysis), and rarely bronchial stenosis.
- Kidney: rapidly progressive segmental necrotising glomerulonephritis (75%), leading to chronic renal failure
- Arthritis: Pain or swelling (60%), often initially diagnosed as rheumatoid arthritis
- Skin: nodules on the elbow, purpura, various others (see cutaneous vasculitis)
- Nervous system: occasionally sensory neuropathy (10%) and rarely mononeuritis multiplex
- Heart, gastrointestinal tract, brain other organs: rarely affected.
Symptoms in Detail
The first symptoms of Wegener's granulomatosis are often vague and frequently include upper respiratory tract symptoms, joint pains, weakness, and tiredness.
Upper respiratory tract
The most common sign of Wegener's granulomatosis is involvement of the upper respiratory tract, which occurs in nearly all patients. Symptoms include sinus pain, discolored or bloody fluid from the nose, and, occasionally, nasal ulcers. A common sign of the disease is almost constant rhinorrhea ("runny nose") or other cold symptoms that do not respond to usual treatment or that become increasingly worse.
Rhinorrhea can result from nasal inflammation or sinus drainage and can cause pain. A hole may develop in the cartilage of the nose, which may lead to collapse (called saddle-nose deformity). The eustachian tubes, which are important for normal ear function, may become blocked, causing chronic ear problems and hearing loss. Bacterial infection can cause Wegener's-related sinusitis (inflammation of the sinuses) with congestion and chronic sinus pain.
Lungs
The lungs are affected in most people with Wegener's granulomatosis, although no symptoms may be present. If symptoms are present, they include cough, hemoptysis (coughing up blood), shortness of breath, and chest discomfort.
Kidneys
Kidney involvement, which occurs in more than three-fourths of people with this disorder, usually does not cause symptoms. If detected by blood and urine tests, a doctor can start proper treatment, preventing long-term damage to the kidneys.
Musculoskeletal system
Pain in the muscles and joints or, occasionally, joint swelling affects two-thirds of people with Wegener's granulomatosis. Although joint pain can be very uncomfortable, it does not lead to permanent joint damage or deformities.
Eyes
Wegener's granulomatosis can affect the eyes in several ways. People may develop;
- Conjunctivitis (inflammation of the conjunctiva, the inner lining of the eyelid)
- Scleritis (inflammation of the scleral layer, the white part of the eyeball)
- Episcleritis (inflammation of the episcleral layer, the outer surface of the sclera)
- Mass lesion behind the eye globe
Symptoms in the eye include redness, burning, or pain. Double vision or a decrease in vision are serious symptoms requiring immediate medical attention.
Skin lesions
Nearly half of people with Wegener's granulomatosis develop skin lesions. These often have the appearance of small red or purple raised areas or blister-like lesions, ulcers, or nodules that may or may not be painful.
Other symptoms
Some people experience narrowing of the trachea. The symptoms can include voice change, hoarseness, shortness of breath, or cough.
The nervous system and heart occasionally may be affected. Fever and night sweats may occur. Fever also may signal an infection, often of the upper respiratory tract.
Diagnosis
Vasculitis such as Wegener's granulomatosis is usually only suspected when a patient has had unexplained symptoms for a longer period of time. Determination of ANCAs can aid in the diagnosis, but positivity is not conclusive and negative ANCAs are not sufficient to reject the diagnosis. Cytoplasmic staining ANCAs that react with the enzyme proteinase 3 (cANCA) in neutrophils (a type of white blood cell) are associated with Wegener's.[2]
If the patient has renal failure or cutaneous vasculitis, these are the most logical organs to obtain a biopsy from. Rarely, thoracoscopic lung biopsy is required. On histopathological examination, a biopsy will show leukocytoclastic vasculitis with necrotic changes and granulomatous inflammation (clumps of typically arranged white blood cells) on microscopy. The latter is the main reason for the appellation of "Wegener's granulomatosis", although it is not an essential feature. Unfortunately, many biopsies can be non-specific and 50% provide too little information for the diagnosis of Wegener's.[2]
Differential diagnosis (alternative possible diagnoses) can be extensive. ANCAs can be positive after the use of certain drugs, and other forms of vasculitis can present with very similar symptoms. The saddle nose deformity may also seen in cocaine abuse and in congenital syphilis.
Diagnostic Criteria
In 1990, the American College of Rheumatology accepted classification criteria for Wegener's. They were not intended for diagnosis, but for inclusion in randomized controlled trials. Two or more positive criteria have a sensitivity of 88.2% and a specificity of 92.0% of describing Wegener's.[4]
- Nasal or oral inflammation:
- painful or painless oral ulcers or
- purulent or bloody nasal discharge
- Lungs: abnormal chest X-ray with:
- nodules,
- infiltrates or
- cavities
- Kidneys: urinary sediment with:
- microhematuriaor
- red cell casts
- Biopsy: granulomatous inflammation
- within the arterial wall or
- in the perivascular area
According to the Chapel Hill Consensus Conference (CHCC) on the nomenclature of systemic vasculitis (1992), establishing the diagnosis of Wegener's granulomatosis demands:[5]
- a granulomatous inflammation involving the respiratory tract, and
- a vasculitis of small- to medium-sized vessels.
Several investigators have compared the ACR and Chapel Hill criteria.[6]
Diagnostic Findings
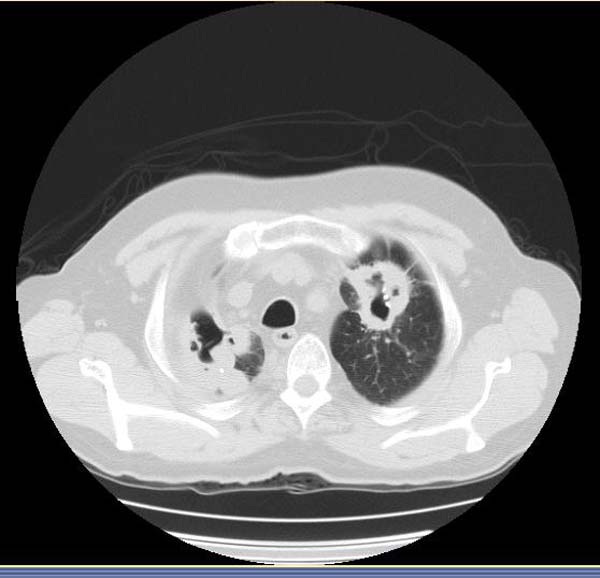
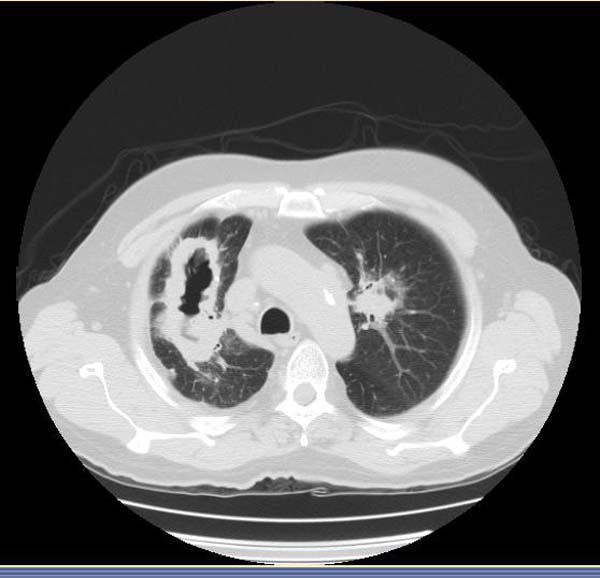
Computed Tomography
-
CT: Wegener's granulomatosis
-
CT: Wegener's granulomatosis
-
CT: Wegener's granulomatosis
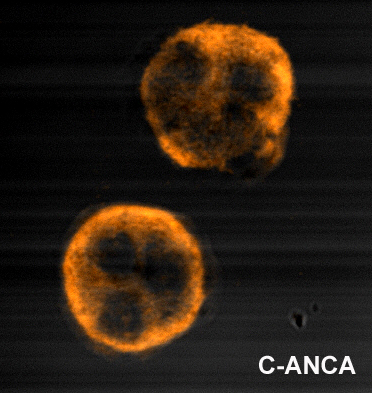
Immunofluorescence
-
Immunofluorescence pattern produced by binding of ANCA from a patient with Wegener's Granulomatosis to ethanol-fixed neutrophils
Treatment
Before steroid treatment became available, mortality within one year was over 90%, with average survival being 5 months. Steroids prolonged average survival to 8 months. The introduction of cyclophosphamide (CYC) in the 1970s was a major breakthrough.[1]
Initial treatment is generally with corticosteroids and oral cyclophosphamide (CYC), 1 mg/kg/day and 2 mg/kg/day, respectively. Occasionally CYC is given in monthly intravenous (IV) doses. Monitoring of the white blood count is essential during CYC therapy. Once remission is attained (normally 3 to 6 months), treatment is frequently changed to azathioprine or methotrexate, which are less toxic drugs. Total duration of therapy should be at least one year, or longer in high risk patients. Corticosteroids are tapered to a low maintenance dose, 5-10 mg/day. Plasmapheresis may be beneficial in severe disease or pulmonary hemorrhage. Experience with other treatment agents is very limited.[2].
A systematic review of 84 trials examined the evidence for various treatments in Wegener's granulomatosis. Many trials include data on pooled groups of patients with Wegener's and microscopic polyangiitis. In this review, cases are divided between localized disease, non-organ threatening, generalized organ-threatening disease and severe renal vasculitis and immediately life-threatening disease.[1]
- In localized disease, treatment with the antibiotic co-trimoxazole is recommended, with steroids in case of treatment failure.[7]
- In generalized non-organ threatening disease, remission can be induced with methotrexate and steroids, where the steroid dose is reduced after a remission has been achieved and methotrexate used as maintenance.
- In case of organ-threatening disease, pulsed intravenous cyclophosphamide with steroids is recommended. Once remission has been achieved, azathioprine and steroids can be used to maintain remission.
- In severe renal vasculitis, the same regimen is used but with the addition of plasma exchange.
- In pulmonary hemorrhage, high doses of cyclophosphamide with pulsed methylprednisolone may be used, or alternatively CYC, steroids, and plasma exchange.
In severe disease not responsive to previously mentioned treatment, the review is positive about mycophenolate mofetil, 15-deoxyspergualin, anti-thymocyte globulin, rituximab and infliximab; data was less favourable for intravenous immunoglobulin (IVIG) and etanercept.[1]
In some patients with severe subglottic stenosis, tracheotomy is required to maintain an airway.
With the appropriate treatment, the outlook is good for people with Wegener's granulomatosis. In a study of 158 patients who were treated with prednisone and cyclophosphamide at the National Institutes of Health (NIH), 91 percent of them markedly improved. After 6 months to 24 years of follow-up, 80 percent of the patients survived.
In most cases, treatment consists of a combination of a glucocorticoid (a steroid) and a cytotoxic medicine. Although these medicines are helpful in treating Wegener's granulomatosis, people and their doctors should be aware that they potentially have serious side effects. In many instances these can be minimized or prevented by careful monitoring by both the doctor and patient.
Approximately half of people with Wegener's granulomatosis may experience a return of their disease. This occurs most frequently within 2 years of stopping medicine but can occur at any point both during treatment or after stopping treatment. Thus, it is extremely important that people continue to see their doctors regularly, both while they are on these medicines, as well as after the medicines have been stopped.
Prednisone
Prednisone is the most common glucocorticoid that doctors use. Prednisone is similar to cortisol, the natural glucocorticoid hormone produced by the body. It is chemically different from the anabolic steroids that have been used by athletes and is given in doses much higher than the body normally produces. Doctors usually give prednisone as a single morning dose to try to imitate how the body normally secretes cortisol.
When the person's illness improves, the prednisone dose is gradually decreased and converted to an every other day dosing schedule, usually over a period of 3 to 4 months. With further improvement in the disease, prednisone is gradually decreased and discontinued completely after approximately 6 to 12 months.
When prednisone is taken by mouth, the body stops making its own natural cortisol. As the prednisone dose is gradually reduced, the body will resume making cortisol again. It is extremely important that prednisone never be stopped suddenly because the body requires prednisone (or cortisol) to function and may not be able to immediately make what it needs.
Prednisone can affect the body's ability to fight off infection. People taking this medicine should report immediately any symptoms of infection and specifically, any fever to their doctors. Prednisone can also cause weight gain, cataracts, brittle bones, diabetes, and changes in mood and personality.
Cyclophosphamide
Cyclophosphamide (Cytoxan) is the most commonly used cytotoxic drug used to treat Wegener's granulomatosis. People take cyclophosphamide once a day by mouth and must take the drug all at once in the morning followed by drinking a large amount of liquid. Although the first dose of cyclophosphamide is based on the person's weight and kidney function, the doctor may adjust the dosage based on blood counts, which are monitored closely to be sure that the white blood cell count is maintained at a safe level.
In the original regimen, cyclophosphamide was continued for a full year beyond that point at which the disease was in remission. The dose of cyclophosphamide was then decreased gradually and eventually stopped. In more recent treatment approaches, however, cyclophosphamide is given until remission and then switched to another medicine such as methotrexate or azathioprine (discussed below).
Cyclophosphamide is a powerful medicine that keeps the immune system from working normally. Doctors must monitor their patients carefully and perform blood tests frequently. Cyclophosphamide can cause an increased risk of infection, bone marrow suppression (lowering of blood counts), sterility, hemorrhagic cystitis (bleeding from the bladder), bladder cancer, as well as other serious side effects.
Methotrexate
Methotrexate has been studied at NIH for the treatment of Wegener's granulomatosis since 1990. In people with active, but not immediately life threatening, Wegener's granulomatosis, methotrexate has been used in combination with prednisone to bring about remission. It also is used to maintain remission after a person has initially received cyclophosphamide. Methotrexate is usually given for 1 to 2 years, after which time if people stay in remission, it is decreased and stopped.
Methotrexate is given once a week usually by mouth, but occasionally as an injection under the skin or in the muscle. People taking methotrexate need to have regular blood work to monitor their response and to watch for side effects.
The side effects of methotrexate include infection, lowering of the blood counts, nausea, soreness and ulceration of the mouth lining, irritation of the lungs (pneumonitis), and inflammation and scarring of the liver. People taking methotrexate cannot drink alcoholic beverages. Methotrexate cannot be given to people who have poor kidney function or who have underlying liver disease such as hepatitis.
Azathioprine
Azathioprine (also called Imuran) is used primarily to maintain remission in people who have initially been treated and gone into remission with cyclophosphamide. It is taken once a day by mouth. Similar to methotrexate, it is usually given for 1 to 2 years after which time the dosage is lowered until it is stopped.
The side effects of azathioprine include infection, lowering of the blood counts, and rarely an allergic type reaction. In people who receive azathioprine to prevent rejection of a transplanted organ, there has been a suggestion of an increased risk of blood cancers (leukemia and lymphoma) but it is not clear whether this risk exists in other situations. People with poor kidney function or liver disease can take azathioprine.
Other medicines
During the course of treating Wegener's granulomatosis, doctors often give their patients other medicines to prevent medicine-related side effects. These include
- Trimethoprim/sulfamethoxazole (also called bactrim or septra) is given three times a week to prevent Pneumocystis carinii infection (a lung infection)
- A medicine regimen is often given to prevent prednisone-related bone loss (osteoporosis)
- Folic acid or folinic acid (also called leucovorin) are often given to people taking methotrexate
Follow-up
General well-being and laboratory organ markers are checked on a regular basis to ascertain the patient has remained in remission.
Prognosis
25 to 40% of patients suffer from flare-ups, but a majority responds well to treatment. Anatomical problems (sinusitis, tracheal stenosis) may require surgery in a small proportion. Relapses can be long and troublesome.
Long-term complications are very common (86%): mainly chronic renal failure, hearing loss and deafness.[2]
References
- ↑ 1.0 1.1 1.2 1.3 Bosch X, Guilabert A, Espinosa G, Mirapeix E (2007). "Treatment of antineutrophil cytoplasmic antibody associated vasculitis: a systematic review". JAMA. 298 (6): 655–69. doi:10.1001/jama.298.6.655. PMID 17684188.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7
- ↑ van der Woude FJ, Rasmussen N, Lobatto S, Wiik A, Permin H, van Es LA, van der Giessen M, van der Hem GK, The TH. Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener's granulomatosis. Lancet 1985;1(8426):425-9. PMID 2857806.
- ↑ Leavitt RY, Fauci AS, Bloch DA, Michel BA, Hunder GG, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum 1990;33:1101-7. PMID 2202308.
- ↑ Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, Hagen EC, Hoffman GS, Hunder GG, Kallenberg CG, et al. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum 1994;37:187-92. PMID 8129773.
- ↑ Bruce IN, Bell AL. A comparison of two nomenclature systems for primary systemic vasculitis. Br J Rheumatol 1997;36:453-8. PMID 9159539.
- ↑ Stegeman CA, Tervaert JW, de Jong PE, Kallenberg CG (1996). "Trimethoprim-sulfamethoxazole (co-trimoxazole) for the prevention of relapses of Wegener's granulomatosis. Dutch Co-Trimoxazole Wegener Study Group". N. Engl. J. Med. 335 (1): 16–20. PMID 8637536.
External links
- Classification criteria by the American College of Rheumatology
- Vasculitis Foundation Formerly the Wegener's Granulomatosis Association
- Wegener's Granulomatosis Info
- WegenersNet A Wegener's Granulomatosis Community Portal
Template:Diseases of the musculoskeletal system and connective tissue
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs