Glomerular disease: Difference between revisions
| Line 16: | Line 16: | ||
==Classification== | ==Classification== | ||
=== Glomerular dieseases can be classified into several clinical and pathological syndromes as below: === | |||
{| class="wikitable" | {| class="wikitable" | ||
!Syndrome | !Syndrome | ||
| Line 91: | Line 91: | ||
|} | |} | ||
Glomerular diseases also may classified by their presentation as below: | === Also, glomerular diseases can be classified based on their clinical and urinary pattern in to below types: === | ||
==== Mild nephritc: ==== | |||
This category include mild nephritic sediment that is associated with less than half involvement of glomeruli. | |||
==== Severe nephritic: ==== | |||
More severe clinical features such as edema, heavy proteinuria, hypertension, and/or renal failure may occur. | |||
==== Nephrotic: ==== | |||
This syndrome is associated with heavy proteinuria and lipiduria. | |||
=== Glomerular diseases also may classified by their presentation as below: === | |||
====== Glomerular [[hematuria]]: ====== | ====== Glomerular [[hematuria]]: ====== | ||
| Line 200: | Line 211: | ||
Glomerulonephritis may be proliferative or non-proliferative and may be associated with [[Nephrotic syndrome|nephrotic]] or [[Nephritic syndrome|nephritic]] features. The various types of glomerulonephritides should be differentiated from each other based on associations, presence of [[pitting edema]], hemeturia, [[hypertension]], [[hemoptysis]], [[oliguria]], peri-orbital edema, [[hyperlipidemia]], type of [[antibodies]], [[Light microscope|light]] and [[Electron microscopy|electron microscopic]] features. | Glomerulonephritis may be proliferative or non-proliferative and may be associated with [[Nephrotic syndrome|nephrotic]] or [[Nephritic syndrome|nephritic]] features. The various types of glomerulonephritides should be differentiated from each other based on associations, presence of [[pitting edema]], hemeturia, [[hypertension]], [[hemoptysis]], [[oliguria]], peri-orbital edema, [[hyperlipidemia]], type of [[antibodies]], [[Light microscope|light]] and [[Electron microscopy|electron microscopic]] features. | ||
The following table differentiates between various types of glomerulonephritides:<ref name="pmid17195422">{{cite journal |vauthors=Saha TC, Singh H |title=Minimal change disease: a review |journal=South. Med. J. |volume=99 |issue=11 |pages=1264–70 |date=November 2006 |pmid=17195422 |doi=10.1097/01.smj.0000243183.87381.c2 |url=}}</ref><ref name="pmid27092244">{{cite journal |vauthors=Saleem MA, Kobayashi Y |title=Cell biology and genetics of minimal change disease |journal=F1000Res |volume=5 |issue= |pages= |date=2016 |pmid=27092244 |pmc=4821284 |doi=10.12688/f1000research.7300.1 |url=}}</ref><ref name="pmid26064510">{{cite journal |vauthors=Keskar V, Jamale TE, Kulkarni MJ, Kiggal Jagadish P, Fernandes G, Hase N |title=Minimal-change disease in adolescents and adults: epidemiology and therapeutic response |journal=Clin Kidney J |volume=6 |issue=5 |pages=469–72 |date=October 2013 |pmid=26064510 |pmc=4438390 |doi=10.1093/ckj/sft063 |url=}}</ref><ref name="pmid21974967">{{cite journal |vauthors=Chugh SS, Clement LC, Macé C |title=New insights into human minimal change disease: lessons from animal models |journal=Am. J. Kidney Dis. |volume=59 |issue=2 |pages=284–92 |date=February 2012 |pmid=21974967 |pmc=3253318 |doi=10.1053/j.ajkd.2011.07.024 |url=}}</ref><ref name="pmid28242845">{{cite journal |vauthors=Rosenberg AZ, Kopp JB |title=Focal Segmental Glomerulosclerosis |journal=Clin J Am Soc Nephrol |volume=12 |issue=3 |pages=502–517 |date=March 2017 |pmid=28242845 |pmc=5338705 |doi=10.2215/CJN.05960616 |url=}}</ref><ref name="pmid25168829">{{cite journal |vauthors=Jefferson JA, Shankland SJ |title=The pathogenesis of focal segmental glomerulosclerosis |journal=Adv Chronic Kidney Dis |volume=21 |issue=5 |pages=408–16 |date=September 2014 |pmid=25168829 |pmc=4149756 |doi=10.1053/j.ackd.2014.05.009 |url=}}</ref><ref name="pmid2429634">{{cite journal |vauthors=Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT |title=Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens |journal=Arch. Pathol. Lab. Med. |volume=110 |issue=10 |pages=902–5 |date=October 1986 |pmid=2429634 |doi= |url=}}</ref><ref name="pmid25558821">{{cite journal |vauthors=Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ |title=Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment |journal=J. Formos. Med. Assoc. |volume=114 |issue=2 |pages=102–11 |date=February 2015 |pmid=25558821 |doi=10.1016/j.jfma.2014.11.002 |url=}}</ref><ref name="pmid10495797">{{cite journal |vauthors=Wasserstein AG |title=Membranous glomerulonephritis |journal=J. Am. Soc. Nephrol. |volume=8 |issue=4 |pages=664–74 |date=April 1997 |pmid=10495797 |doi= |url=}}</ref><ref name="pmid21949093">{{cite journal |vauthors=Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA |title=The pathophysiology of IgA nephropathy |journal=J. Am. Soc. Nephrol. |volume=22 |issue=10 |pages=1795–803 |date=October 2011 |pmid=21949093 |pmc=3892742 |doi=10.1681/ASN.2011050464 |url=}}</ref><ref name="pmid23782179">{{cite journal |vauthors=Wyatt RJ, Julian BA |title=IgA nephropathy |journal=N. Engl. J. Med. |volume=368 |issue=25 |pages=2402–14 |date=June 2013 |pmid=23782179 |doi=10.1056/NEJMra1206793 |url=}}</ref><ref name="pmid22373436">{{cite journal |vauthors=He S, Wu Z |title=Gene-based Higher Criticism methods for large-scale exonic single-nucleotide polymorphism data |journal=BMC Proc |volume=5 Suppl 9 |issue= |pages=S65 |date=November 2011 |pmid=22373436 |pmc=3287904 |doi=10.1186/1753-6561-5-S9-S65 |url=}}</ref><ref name="pmid8746284">{{cite journal |vauthors=Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC |title=Vasculitis and rapidly progressive glomerulonephritis in the elderly |journal=Postgrad Med J |volume=72 |issue=843 |pages=41–4 |date=January 1996 |pmid=8746284 |pmc=2398323 |doi= |url=}}</ref><ref name="pmid12631105">{{cite journal |vauthors=Jennette JC |title=Rapidly progressive crescentic glomerulonephritis |journal=Kidney Int. |volume=63 |issue=3 |pages=1164–77 |date=March 2003 |pmid=12631105 |doi=10.1046/j.1523-1755.2003.00843.x |url=}}</ref><ref name="pmid8914046">{{cite journal |vauthors=Bolton WK |title=Goodpasture's syndrome |journal=Kidney Int. |volume=50 |issue=5 |pages=1753–66 |date=November 1996 |pmid=8914046 |doi= |url=}}</ref><ref name="pmid1090223">{{cite journal |vauthors=Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P |title=Goodpasture's syndrome: normal renal diagnostic findings |journal=Ann. Intern. Med. |volume=82 |issue=2 |pages=215–8 |date=February 1975 |pmid=1090223 |doi= |url=}}</ref><ref name="pmid18172777">{{cite journal |vauthors=Renaudineau Y, Le Meur Y |title=Renal involvement in Wegener's granulomatosis |journal=Clin Rev Allergy Immunol |volume=35 |issue=1-2 |pages=22–9 |date=October 2008 |pmid=18172777 |doi=10.1007/s12016-007-8066-6 |url=}}</ref><ref name="pmid6384024">{{cite journal |vauthors=Weiss MA, Crissman JD |title=Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis |journal=Hum. Pathol. |volume=15 |issue=10 |pages=943–56 |date=October 1984 |pmid=6384024 |doi= |url=}}</ref><ref name="pmid16632015">{{cite journal |vauthors=Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C |title=Renal involvement in Churg-Strauss syndrome |journal=Am. J. Kidney Dis. |volume=47 |issue=5 |pages=770–9 |date=May 2006 |pmid=16632015 |doi=10.1053/j.ajkd.2006.01.026 |url=}}</ref><ref name="pmid21325353">{{cite journal |vauthors=Cartin-Ceba R, Keogh KA, Specks U, Sethi S, Fervenza FC |title=Rituximab for the treatment of Churg-Strauss syndrome with renal involvement |journal=Nephrol. Dial. Transplant. |volume=26 |issue=9 |pages=2865–71 |date=September 2011 |pmid=21325353 |pmc=3218640 |doi=10.1093/ndt/gfq852 |url=}}</ref><ref name="pmid20688249">{{cite journal |vauthors=Chung SA, Seo P |title=Microscopic polyangiitis |journal=Rheum. Dis. Clin. North Am. |volume=36 |issue=3 |pages=545–58 |date=August 2010 |pmid=20688249 |pmc=2917831 |doi=10.1016/j.rdc.2010.04.003 |url=}}</ref><ref name="pmid18524109">{{cite journal |vauthors=Pagnoux C |title=[Wegener's granulomatosis and microscopic polyangiitis] |language=French |journal=Rev Prat |volume=58 |issue=5 |pages=522–32 |date=March 2008 |pmid=18524109 |doi= |url=}}</ref><ref name="pmid19908070">{{cite journal |vauthors=Alchi B, Jayne D |title=Membranoproliferative glomerulonephritis |journal=Pediatr. Nephrol. |volume=25 |issue=8 |pages=1409–18 |date=August 2010 |pmid=19908070 |pmc=2887509 |doi=10.1007/s00467-009-1322-7 |url=}}</ref><ref name="pmid657595">{{cite journal |vauthors=Davis AE, Schneeberger EE, Grupe WE, McCluskey RT |title=Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children |journal=Clin. Nephrol. |volume=9 |issue=5 |pages=184–93 |date=May 1978 |pmid=657595 |doi= |url=}}</ref> | The following table differentiates between various types of glomerulonephritides:<ref name="pmid17195422">{{cite journal |vauthors=Saha TC, Singh H |title=Minimal change disease: a review |journal=South. Med. J. |volume=99 |issue=11 |pages=1264–70 |date=November 2006 |pmid=17195422 |doi=10.1097/01.smj.0000243183.87381.c2 |url=}}</ref><ref name="pmid27092244">{{cite journal |vauthors=Saleem MA, Kobayashi Y |title=Cell biology and genetics of minimal change disease |journal=F1000Res |volume=5 |issue= |pages= |date=2016 |pmid=27092244 |pmc=4821284 |doi=10.12688/f1000research.7300.1 |url=}}</ref><ref name="pmid26064510">{{cite journal |vauthors=Keskar V, Jamale TE, Kulkarni MJ, Kiggal Jagadish P, Fernandes G, Hase N |title=Minimal-change disease in adolescents and adults: epidemiology and therapeutic response |journal=Clin Kidney J |volume=6 |issue=5 |pages=469–72 |date=October 2013 |pmid=26064510 |pmc=4438390 |doi=10.1093/ckj/sft063 |url=}}</ref><ref name="pmid21974967">{{cite journal |vauthors=Chugh SS, Clement LC, Macé C |title=New insights into human minimal change disease: lessons from animal models |journal=Am. J. Kidney Dis. |volume=59 |issue=2 |pages=284–92 |date=February 2012 |pmid=21974967 |pmc=3253318 |doi=10.1053/j.ajkd.2011.07.024 |url=}}</ref><ref name="pmid28242845">{{cite journal |vauthors=Rosenberg AZ, Kopp JB |title=Focal Segmental Glomerulosclerosis |journal=Clin J Am Soc Nephrol |volume=12 |issue=3 |pages=502–517 |date=March 2017 |pmid=28242845 |pmc=5338705 |doi=10.2215/CJN.05960616 |url=}}</ref><ref name="pmid25168829">{{cite journal |vauthors=Jefferson JA, Shankland SJ |title=The pathogenesis of focal segmental glomerulosclerosis |journal=Adv Chronic Kidney Dis |volume=21 |issue=5 |pages=408–16 |date=September 2014 |pmid=25168829 |pmc=4149756 |doi=10.1053/j.ackd.2014.05.009 |url=}}</ref><ref name="pmid2429634">{{cite journal |vauthors=Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT |title=Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens |journal=Arch. Pathol. Lab. Med. |volume=110 |issue=10 |pages=902–5 |date=October 1986 |pmid=2429634 |doi= |url=}}</ref><ref name="pmid25558821">{{cite journal |vauthors=Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ |title=Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment |journal=J. Formos. Med. Assoc. |volume=114 |issue=2 |pages=102–11 |date=February 2015 |pmid=25558821 |doi=10.1016/j.jfma.2014.11.002 |url=}}</ref><ref name="pmid10495797">{{cite journal |vauthors=Wasserstein AG |title=Membranous glomerulonephritis |journal=J. Am. Soc. Nephrol. |volume=8 |issue=4 |pages=664–74 |date=April 1997 |pmid=10495797 |doi= |url=}}</ref><ref name="pmid21949093">{{cite journal |vauthors=Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA |title=The pathophysiology of IgA nephropathy |journal=J. Am. Soc. Nephrol. |volume=22 |issue=10 |pages=1795–803 |date=October 2011 |pmid=21949093 |pmc=3892742 |doi=10.1681/ASN.2011050464 |url=}}</ref><ref name="pmid23782179">{{cite journal |vauthors=Wyatt RJ, Julian BA |title=IgA nephropathy |journal=N. Engl. J. Med. |volume=368 |issue=25 |pages=2402–14 |date=June 2013 |pmid=23782179 |doi=10.1056/NEJMra1206793 |url=}}</ref><ref name="pmid22373436">{{cite journal |vauthors=He S, Wu Z |title=Gene-based Higher Criticism methods for large-scale exonic single-nucleotide polymorphism data |journal=BMC Proc |volume=5 Suppl 9 |issue= |pages=S65 |date=November 2011 |pmid=22373436 |pmc=3287904 |doi=10.1186/1753-6561-5-S9-S65 |url=}}</ref><ref name="pmid8746284">{{cite journal |vauthors=Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC |title=Vasculitis and rapidly progressive glomerulonephritis in the elderly |journal=Postgrad Med J |volume=72 |issue=843 |pages=41–4 |date=January 1996 |pmid=8746284 |pmc=2398323 |doi= |url=}}</ref><ref name="pmid12631105">{{cite journal |vauthors=Jennette JC |title=Rapidly progressive crescentic glomerulonephritis |journal=Kidney Int. |volume=63 |issue=3 |pages=1164–77 |date=March 2003 |pmid=12631105 |doi=10.1046/j.1523-1755.2003.00843.x |url=}}</ref><ref name="pmid8914046">{{cite journal |vauthors=Bolton WK |title=Goodpasture's syndrome |journal=Kidney Int. |volume=50 |issue=5 |pages=1753–66 |date=November 1996 |pmid=8914046 |doi= |url=}}</ref><ref name="pmid1090223">{{cite journal |vauthors=Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P |title=Goodpasture's syndrome: normal renal diagnostic findings |journal=Ann. Intern. Med. |volume=82 |issue=2 |pages=215–8 |date=February 1975 |pmid=1090223 |doi= |url=}}</ref><ref name="pmid18172777">{{cite journal |vauthors=Renaudineau Y, Le Meur Y |title=Renal involvement in Wegener's granulomatosis |journal=Clin Rev Allergy Immunol |volume=35 |issue=1-2 |pages=22–9 |date=October 2008 |pmid=18172777 |doi=10.1007/s12016-007-8066-6 |url=}}</ref><ref name="pmid6384024">{{cite journal |vauthors=Weiss MA, Crissman JD |title=Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis |journal=Hum. Pathol. |volume=15 |issue=10 |pages=943–56 |date=October 1984 |pmid=6384024 |doi= |url=}}</ref><ref name="pmid16632015">{{cite journal |vauthors=Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C |title=Renal involvement in Churg-Strauss syndrome |journal=Am. J. Kidney Dis. |volume=47 |issue=5 |pages=770–9 |date=May 2006 |pmid=16632015 |doi=10.1053/j.ajkd.2006.01.026 |url=}}</ref><ref name="pmid21325353">{{cite journal |vauthors=Cartin-Ceba R, Keogh KA, Specks U, Sethi S, Fervenza FC |title=Rituximab for the treatment of Churg-Strauss syndrome with renal involvement |journal=Nephrol. Dial. Transplant. |volume=26 |issue=9 |pages=2865–71 |date=September 2011 |pmid=21325353 |pmc=3218640 |doi=10.1093/ndt/gfq852 |url=}}</ref><ref name="pmid20688249">{{cite journal |vauthors=Chung SA, Seo P |title=Microscopic polyangiitis |journal=Rheum. Dis. Clin. North Am. |volume=36 |issue=3 |pages=545–58 |date=August 2010 |pmid=20688249 |pmc=2917831 |doi=10.1016/j.rdc.2010.04.003 |url=}}</ref><ref name="pmid18524109">{{cite journal |vauthors=Pagnoux C |title=[Wegener's granulomatosis and microscopic polyangiitis] |language=French |journal=Rev Prat |volume=58 |issue=5 |pages=522–32 |date=March 2008 |pmid=18524109 |doi= |url=}}</ref><ref name="pmid19908070">{{cite journal |vauthors=Alchi B, Jayne D |title=Membranoproliferative glomerulonephritis |journal=Pediatr. Nephrol. |volume=25 |issue=8 |pages=1409–18 |date=August 2010 |pmid=19908070 |pmc=2887509 |doi=10.1007/s00467-009-1322-7 |url=}}</ref><ref name="pmid657595">{{cite journal |vauthors=Davis AE, Schneeberger EE, Grupe WE, McCluskey RT |title=Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children |journal=Clin. Nephrol. |volume=9 |issue=5 |pages=184–93 |date=May 1978 |pmid=657595 |doi= |url=}}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
Revision as of 20:06, 15 May 2018
This page contains general information about Glomerular disease. For more information on specific types, please visit the pages on nephritic syndrome, nephrotic syndrome, Fabry's disease, amyloidosis, pulmonary-renal syndromes (vasculitis), thin basement membrane disease, Alport's Syndrome, anti-GBM Disease, hypertensive nephrosclerosis, and subacute bacterial endocarditis.
| Glomerular disease | |
 | |
|---|---|
| Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2], Syed Hassan A. Kazmi BSc, MD [3]
Overview
Glomerular disease is a condition that affects the glomerulus. It consists of different diseases with different clinical courses and treatment options. Glomerular disease can be isolated hematuria, isolated proteinuria; acute or chronic glomerulonephritis, and nephrotic or nephritic features of glomerulonephritis. The end stage of all of these diseases will be glomerulosclerosi swhich is characterized by fibrosis of the glomerulus, and end-stage renal disease.
Classification
Glomerular dieseases can be classified into several clinical and pathological syndromes as below:
| Syndrome | Disease |
|---|---|
| Acute nephritic syndromes |
|
| Nephrotic syndrome | |
| Glomerular Deposition Diseases |
|
| Pulmonary-Renal Syndromes: | |
| Basement Membrane Syndromes | |
| Glomerular-Vascular Syndromes |
|
| Infectious Disease–Associated Syndromes |
Also, glomerular diseases can be classified based on their clinical and urinary pattern in to below types:
Mild nephritc:
This category include mild nephritic sediment that is associated with less than half involvement of glomeruli.
Severe nephritic:
More severe clinical features such as edema, heavy proteinuria, hypertension, and/or renal failure may occur.
Nephrotic:
This syndrome is associated with heavy proteinuria and lipiduria.
Glomerular diseases also may classified by their presentation as below:
Glomerular hematuria:
1- Isolated hematuria
2- Glomerulonephritis (nephritic syndrome)
Proteinuria:
1-Isolated non-nephrotic proteinuria
Rapidly progressive glomerulonephritis
Glomerulonephritis
Glomerulonephritis which is inflammation of the glomeruli can be classified based on pathogenic type into three subtypes:
- Immune complex glomerulonephritis: Granular deposit of immune complex.
- Infection mediated types
- Autoimmune types, eg SLE
- MPGN
- IgA nephropathy (Berger nephropathy)
- Membranous nephropathy
- Anti-GBM disease: Linear deposit
- Goodpasture syndrome (renal and lung involvement)
- Renal involvement alone
- Lung involvement alone
- ANCA associated, small vessels vasculitis: Few or no deposit
Glomerulonephritis (nephritic syndrome) also may be classified based on disease course into acute or chronic nephritic syndrome; primary vs secondary causes; or systemic vs renal limited disease. For more information about nephritic syndrome classifications click here.
Pathophysiology
Microscopic Pathology
-
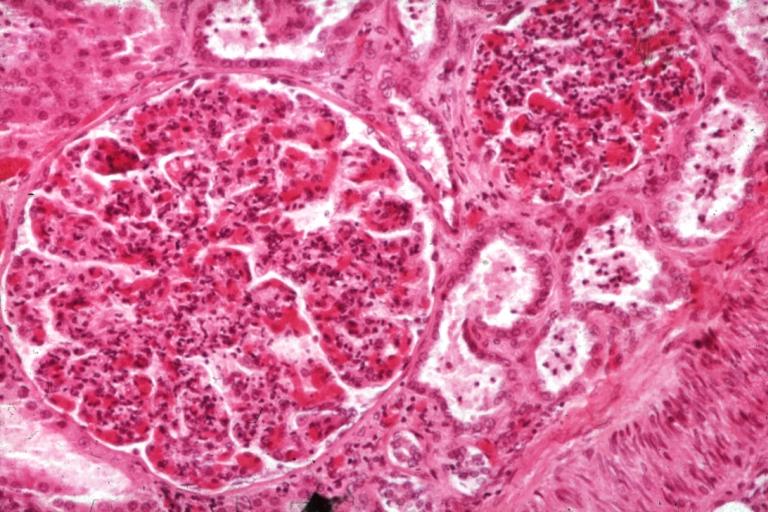
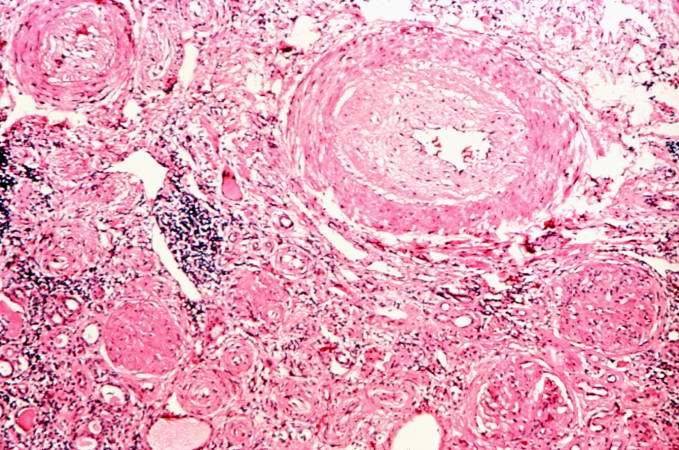
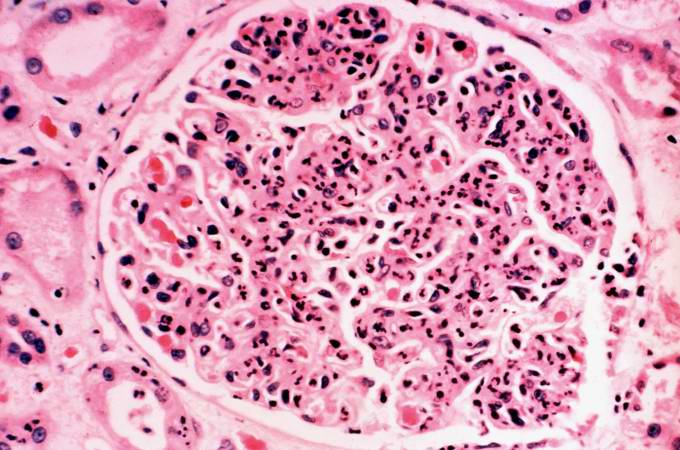
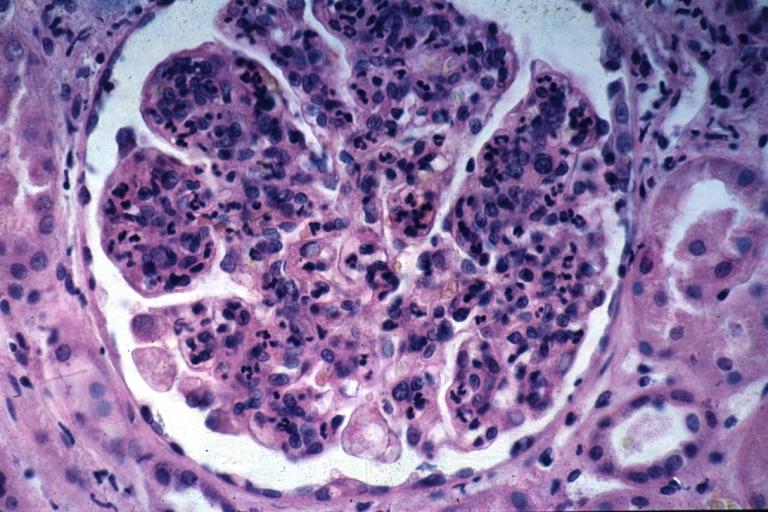
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Images
-
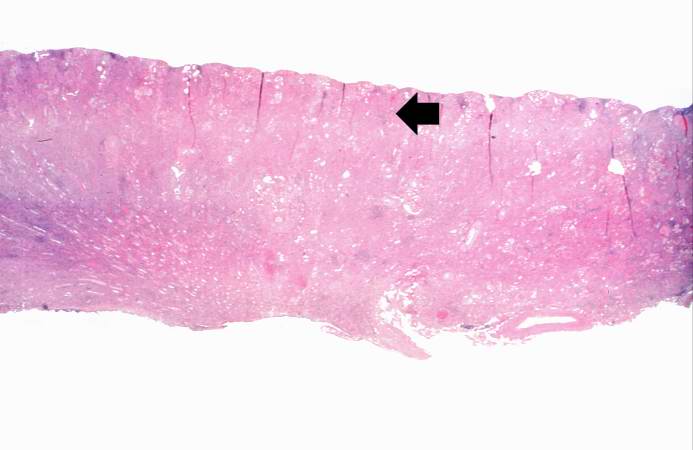
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
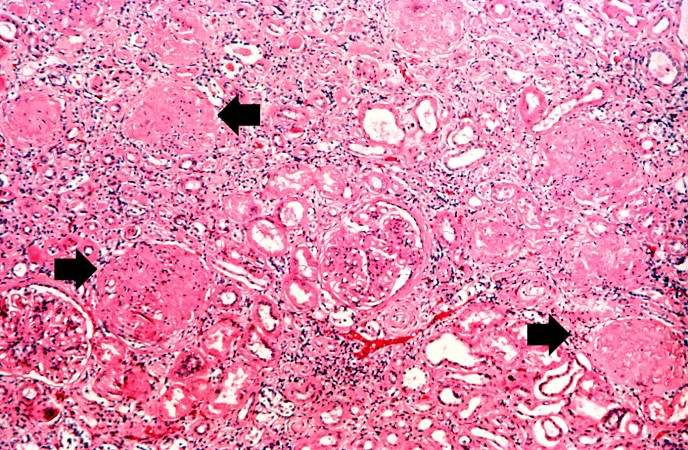
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
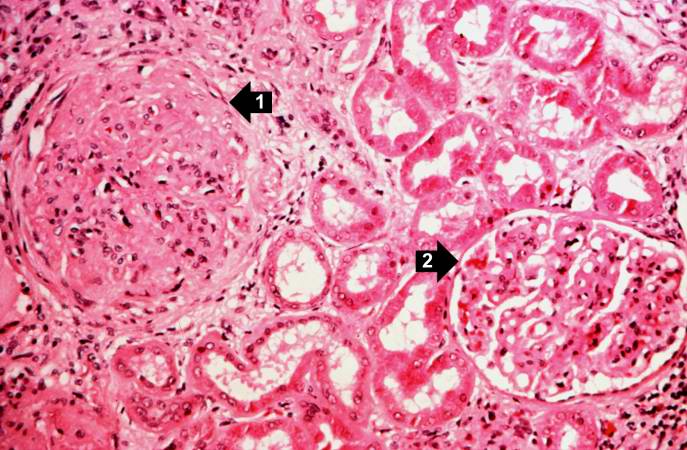
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
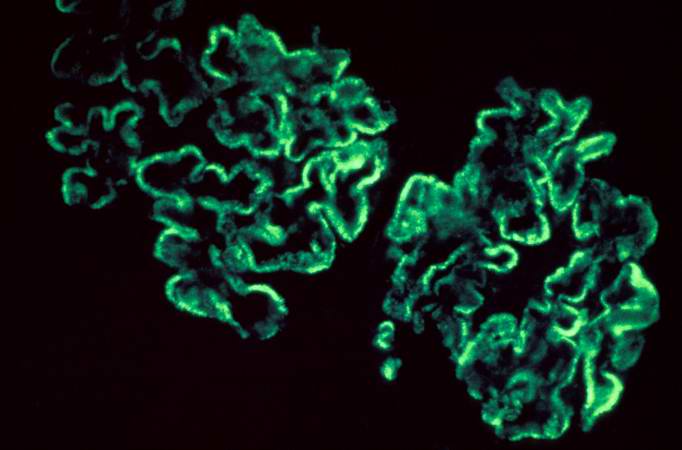
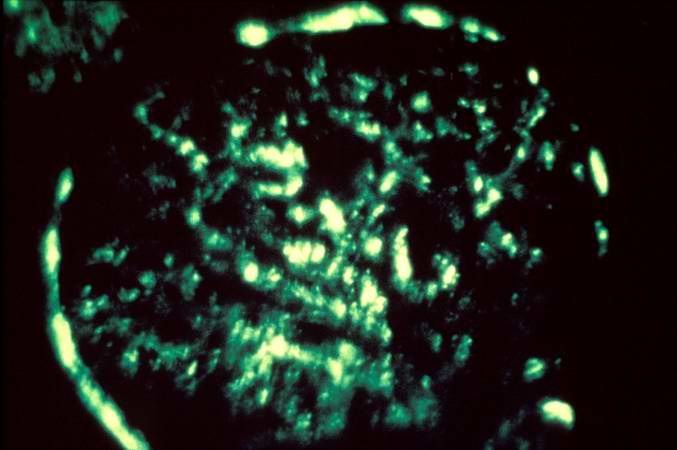
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
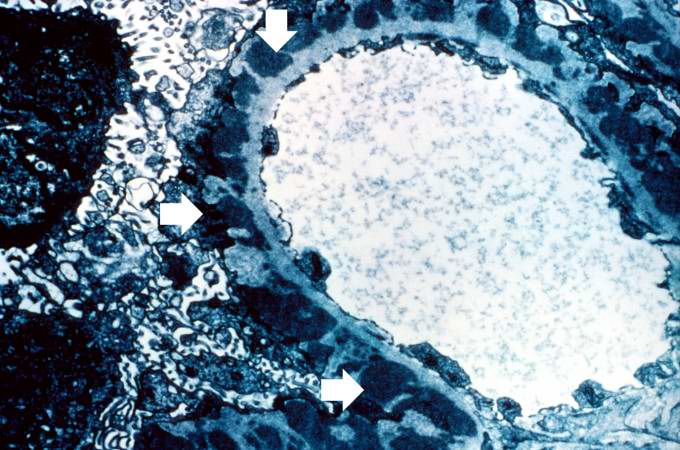
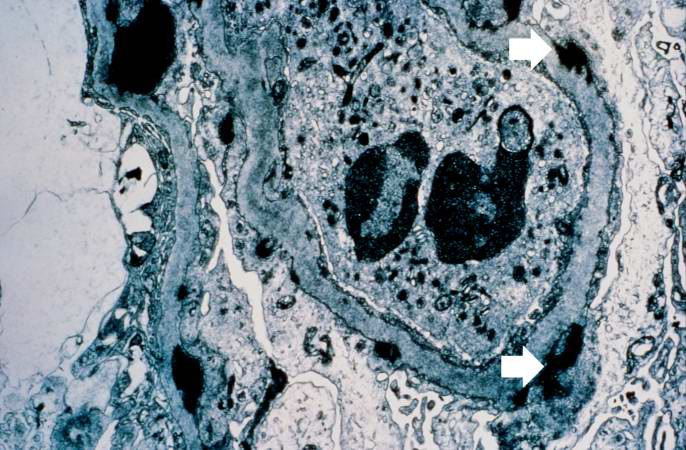
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
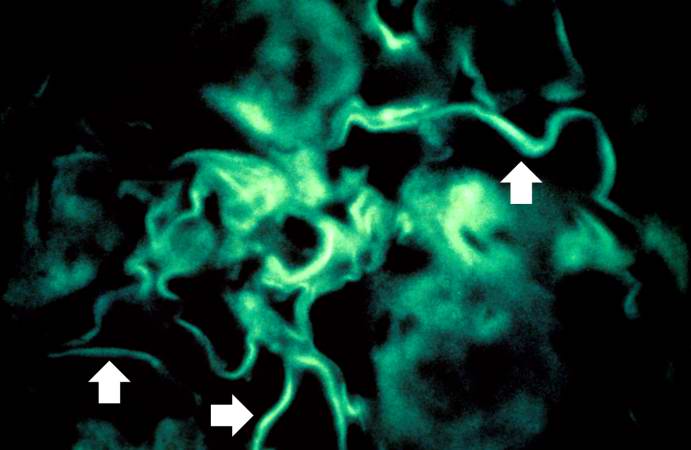
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Images:
Differential Diagnosis
Glomerulonephritis may be proliferative or non-proliferative and may be associated with nephrotic or nephritic features. The various types of glomerulonephritides should be differentiated from each other based on associations, presence of pitting edema, hemeturia, hypertension, hemoptysis, oliguria, peri-orbital edema, hyperlipidemia, type of antibodies, light and electron microscopic features. The following table differentiates between various types of glomerulonephritides:[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24]
| Glomerular diseases | Sub-entity | Causes and associations | History and Symtoms | Laboratory Findings | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyperlipidemia and hypercholesterolemia | Nephrotic features | Nephritic features | ANCA | Anti-glomerular basement membrane antibody (Anti-GBM antibody) | Immune complex formation | Light microscope | Electron microscope | Immunoflourescence pattern | |||||||||||||||||||||||||||||
| History | Pitting edema | Hemeturia (pre-dominantly microscopic) | Hypertension | Hemoptysis | Oliguria | Peri-orbital edema | |||||||||||||||||||||||||||||||
| Acute Nephritic Syndromes | Poststreptococcal Glomerulonephritis | ||||||||||||||||||||||||||||||||||||
| Subacute Bacterial Endocarditis | |||||||||||||||||||||||||||||||||||||
| Lupus Nephritis | |||||||||||||||||||||||||||||||||||||
| Antiglomerular Basement Membrane Disease |
|
+/- | + | + | + | + | + | - | - | + | - | + | + |
|
+ (Linear) | ||||||||||||||||||||||
| IgA Nephropathy |
|
+/- | + | + | - | + | +/- | - | - | + | - | - | + |
|
|
- | |||||||||||||||||||||
| ANCA Small-Vessel Vasculitis | Granulomatosis with Polyangiitis (Wegener's) | ||||||||||||||||||||||||||||||||||||
| Microscopic Polyangiitis | |||||||||||||||||||||||||||||||||||||
| Churg-Strauss Syndrome | |||||||||||||||||||||||||||||||||||||
| Membranoproliferative Glomerulonephritis |
|
+/- | + | + | + | + | + | - | + | - | - | - | + |
|
+ (Granular) | ||||||||||||||||||||||
| Mesangioproliferative Glomerulonephritis | |||||||||||||||||||||||||||||||||||||
| Nephrotic Syndrome | Minimal Change Disease |
|
|
+ | - | - | - | +/- | - | + | + | - | - | - | - |
|
|
- | |||||||||||||||||||
| Focal Segmental Glomerulosclerosis |
|
|
+ | - | - | - | +/- | - | + | + | - | - | - | - |
|
|
- | ||||||||||||||||||||
| Membranous Glomerulonephritis |
|
+ | - | - | - | +/- | - | + | + | - | - | - | + |
|
- | ||||||||||||||||||||||
| Diabetic Nephropathy | |||||||||||||||||||||||||||||||||||||
| Glomerular Deposition Diseases | Light Chain Deposition Disease | ||||||||||||||||||||||||||||||||||||
| Renal Amyloidosis | |||||||||||||||||||||||||||||||||||||
| Fibrillary-Immunotactoid Glomerulopathy | |||||||||||||||||||||||||||||||||||||
| Fabry's Disease | |||||||||||||||||||||||||||||||||||||
| Pulmonary-Renal Syndromes: | Goodpasture's syndrome | granulomatosis with polyangiitis (Wegener's) |
|
+/- | + | + | + | + | + | - | - | + | + (C-ANCA) | - | - | - (pauci-immune) | +/- | ||||||||||||||||||||
| Microscopic polyangiitis | +/- | + | + | + | + | + | - | - | + |
+ (P-ANCA) |
- | - | - (pauci-immune) | - | |||||||||||||||||||||||
| Churg-Strauss vasculitis | +/- | + | + | + | + | + | - | - | + |
+ (C-ANCA) |
- | - | - (pauci-immune) | - | |||||||||||||||||||||||
| Henoch-Schönlein purpura | |||||||||||||||||||||||||||||||||||||
| Cryoglobulinemia | |||||||||||||||||||||||||||||||||||||
| Basement Membrane Syndromes | Anti-GBM Disease | ||||||||||||||||||||||||||||||||||||
| Alport's Syndrome | |||||||||||||||||||||||||||||||||||||
| Thin Basement Membrane Disease | |||||||||||||||||||||||||||||||||||||
| Nail-Patella Syndrome | |||||||||||||||||||||||||||||||||||||
| Glomerular-Vascular Syndromes | Atherosclerotic Nephropathy | ||||||||||||||||||||||||||||||||||||
| Hypertensive Nephrosclerosis | |||||||||||||||||||||||||||||||||||||
| Cholesterol Emboli | |||||||||||||||||||||||||||||||||||||
| Sickle Cell Disease | |||||||||||||||||||||||||||||||||||||
| Thrombotic Microangiopathies | |||||||||||||||||||||||||||||||||||||
| Antiphospholipid Antibody Syndrome | |||||||||||||||||||||||||||||||||||||
| Infectious Disease–Associated Syndromes | Post-Streptococcal Glomerulonephritis |
|
+/- | + | + | + | + | + | - | - | + | - | - | + |
|
+ (Granular) | |||||||||||||||||||||
| Subacute Bacterial Endocarditis | |||||||||||||||||||||||||||||||||||||
| Human Immunodeficiency Virus | |||||||||||||||||||||||||||||||||||||
| Hepatitis B and C | |||||||||||||||||||||||||||||||||||||
| Other Viruses | |||||||||||||||||||||||||||||||||||||
| Syphilis | |||||||||||||||||||||||||||||||||||||
| Leprosy | |||||||||||||||||||||||||||||||||||||
| Malaria | |||||||||||||||||||||||||||||||||||||
| Schistosomiasis | |||||||||||||||||||||||||||||||||||||
| Other Parasites | |||||||||||||||||||||||||||||||||||||
References
- ↑ Saha TC, Singh H (November 2006). "Minimal change disease: a review". South. Med. J. 99 (11): 1264–70. doi:10.1097/01.smj.0000243183.87381.c2. PMID 17195422.
- ↑ Saleem MA, Kobayashi Y (2016). "Cell biology and genetics of minimal change disease". F1000Res. 5. doi:10.12688/f1000research.7300.1. PMC 4821284. PMID 27092244.
- ↑ Keskar V, Jamale TE, Kulkarni MJ, Kiggal Jagadish P, Fernandes G, Hase N (October 2013). "Minimal-change disease in adolescents and adults: epidemiology and therapeutic response". Clin Kidney J. 6 (5): 469–72. doi:10.1093/ckj/sft063. PMC 4438390. PMID 26064510.
- ↑ Chugh SS, Clement LC, Macé C (February 2012). "New insights into human minimal change disease: lessons from animal models". Am. J. Kidney Dis. 59 (2): 284–92. doi:10.1053/j.ajkd.2011.07.024. PMC 3253318. PMID 21974967.
- ↑ Rosenberg AZ, Kopp JB (March 2017). "Focal Segmental Glomerulosclerosis". Clin J Am Soc Nephrol. 12 (3): 502–517. doi:10.2215/CJN.05960616. PMC 5338705. PMID 28242845.
- ↑ Jefferson JA, Shankland SJ (September 2014). "The pathogenesis of focal segmental glomerulosclerosis". Adv Chronic Kidney Dis. 21 (5): 408–16. doi:10.1053/j.ackd.2014.05.009. PMC 4149756. PMID 25168829.
- ↑ Gephardt GN, Tubbs RR, Popowniak KL, McMahon JT (October 1986). "Focal and segmental glomerulosclerosis. Immunohistologic study of 20 renal biopsy specimens". Arch. Pathol. Lab. Med. 110 (10): 902–5. PMID 2429634.
- ↑ Lai WL, Yeh TH, Chen PM, Chan CK, Chiang WC, Chen YM, Wu KD, Tsai TJ (February 2015). "Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment". J. Formos. Med. Assoc. 114 (2): 102–11. doi:10.1016/j.jfma.2014.11.002. PMID 25558821.
- ↑ Wasserstein AG (April 1997). "Membranous glomerulonephritis". J. Am. Soc. Nephrol. 8 (4): 664–74. PMID 10495797.
- ↑ Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA (October 2011). "The pathophysiology of IgA nephropathy". J. Am. Soc. Nephrol. 22 (10): 1795–803. doi:10.1681/ASN.2011050464. PMC 3892742. PMID 21949093.
- ↑ Wyatt RJ, Julian BA (June 2013). "IgA nephropathy". N. Engl. J. Med. 368 (25): 2402–14. doi:10.1056/NEJMra1206793. PMID 23782179.
- ↑ He S, Wu Z (November 2011). "Gene-based Higher Criticism methods for large-scale exonic single-nucleotide polymorphism data". BMC Proc. 5 Suppl 9: S65. doi:10.1186/1753-6561-5-S9-S65. PMC 3287904. PMID 22373436.
- ↑ Higgins RM, Goldsmith DJ, Connolly J, Scoble JE, Hendry BM, Ackrill P, Venning MC (January 1996). "Vasculitis and rapidly progressive glomerulonephritis in the elderly". Postgrad Med J. 72 (843): 41–4. PMC 2398323. PMID 8746284.
- ↑ Jennette JC (March 2003). "Rapidly progressive crescentic glomerulonephritis". Kidney Int. 63 (3): 1164–77. doi:10.1046/j.1523-1755.2003.00843.x. PMID 12631105.
- ↑ Bolton WK (November 1996). "Goodpasture's syndrome". Kidney Int. 50 (5): 1753–66. PMID 8914046.
- ↑ Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid-Smith P (February 1975). "Goodpasture's syndrome: normal renal diagnostic findings". Ann. Intern. Med. 82 (2): 215–8. PMID 1090223.
- ↑ Renaudineau Y, Le Meur Y (October 2008). "Renal involvement in Wegener's granulomatosis". Clin Rev Allergy Immunol. 35 (1–2): 22–9. doi:10.1007/s12016-007-8066-6. PMID 18172777.
- ↑ Weiss MA, Crissman JD (October 1984). "Renal biopsy findings in Wegener's granulomatosis: segmental necrotizing glomerulonephritis with glomerular thrombosis". Hum. Pathol. 15 (10): 943–56. PMID 6384024.
- ↑ Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C (May 2006). "Renal involvement in Churg-Strauss syndrome". Am. J. Kidney Dis. 47 (5): 770–9. doi:10.1053/j.ajkd.2006.01.026. PMID 16632015.
- ↑ Cartin-Ceba R, Keogh KA, Specks U, Sethi S, Fervenza FC (September 2011). "Rituximab for the treatment of Churg-Strauss syndrome with renal involvement". Nephrol. Dial. Transplant. 26 (9): 2865–71. doi:10.1093/ndt/gfq852. PMC 3218640. PMID 21325353.
- ↑ Chung SA, Seo P (August 2010). "Microscopic polyangiitis". Rheum. Dis. Clin. North Am. 36 (3): 545–58. doi:10.1016/j.rdc.2010.04.003. PMC 2917831. PMID 20688249.
- ↑ Pagnoux C (March 2008). "[Wegener's granulomatosis and microscopic polyangiitis]". Rev Prat (in French). 58 (5): 522–32. PMID 18524109.
- ↑ Alchi B, Jayne D (August 2010). "Membranoproliferative glomerulonephritis". Pediatr. Nephrol. 25 (8): 1409–18. doi:10.1007/s00467-009-1322-7. PMC 2887509. PMID 19908070.
- ↑ Davis AE, Schneeberger EE, Grupe WE, McCluskey RT (May 1978). "Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children". Clin. Nephrol. 9 (5): 184–93. PMID 657595.