Verapamil
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Verapamil is a Calcium Channel Blocker that is FDA approved for the {{{indicationType}}} of essential hypertension (tablet and capsule), rapid conversion to sinus rhythm of paroxysmal supraventricular tachycardias, Temporary control of rapid ventricular rate in atrial flutter or atrial fibrillation (injection). Common adverse reactions include edema, hypotension,constipation,dizziness, headache,pharyngitis,sinusitis,influenza-like symptoms.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Essential Hypertension
- Dosing information (tablet)
- The dose of verapamil HCl extended-release should be individualized by titration and the drug should be administered with food.
- Initiate dosage: 180 mg in the morning.
- Lower initial dosage: 120 mg PO qd may be warranted in patients who may have an increased response to verapamil (e.g., the elderly or small people etc.).
- Upward titration should be based on therapeutic efficacy and safety evaluated weekly and approximately 24 hours after the previous dose. ::* The antihypertensive effects of verapamil HCl extended-release are evident within the first week of therapy.
- If adequate response is not obtained with 180 mg of verapamil HCl extended-release, the dose may be titrated upward in the following manner:
- 240 mg each morning,
- 180 mg each morning plus 180 mg each evening; or 240 mg each morning plus 120 mg each evening,
- 240 mg every twelve hours.
- When switching from immediate release verapamil to extended-release verapamil, the total daily dose in milligrams may remain the same.
- Dosing information (capsule)
- Administer Verapamil Hydrochloride Extended-release Capsules (PM) once daily at bedtime.
- Usual dosage: 200 mg PO qd at bedtime
- In rare instances, initial doses of 100 mg PO qd may be warranted in patients who have an increased response to verapamil [e.g. patients with impaired renal function, impaired hepatic function, elderly, low-weight patients, etc. (see Use in Specific Populations (8.5, 8.6, 8.7))].
- Base upward titration on therapeutic efficacy and safety evaluated approximately 24 hours after dosing. The antihypertensive effects of Verapamil Hydrochloride Extended-release Capsules (PM) are evident within the first week of therapy.
- If an adequate response is not obtained with 200 mg of Verapamil Hydrochloride Extended-release Capsules (PM), the dose may be titrated upward in the following manner:
- a) 300 mg each evening
- b) 400 mg each evening (2 × 200 mg)
- When Verapamil Hydrochloride Extended-release Capsules (PM) is administered at bedtime, office evaluation of blood pressure during morning and early afternoon hours is essentially a measure of peak effect. The usual evaluation of trough effect, which sometimes might be needed to evaluate the appropriateness of any given dose of Verapamil Hydrochloride Extended-release Capsules (PM), would be just prior to bedtime.
- THE CONTENTS OF THE Verapamil Hydrochloride Extended-release Capsules (PM) CAPSULE SHOULD NOT BE CRUSHED OR CHEWED. Verapamil Hydrochloride Extended-release Capsules (PM) ARE TO BE SWALLOWED WHOLE OR THE ENTIRE CONTENTS OF THE CAPSULE SPRINKLED ONTO APPLESAUCE.
- Sprinkling the Capsule Contents on Food
- Verapamil Hydrochloride Extended-release Capsules (PM) capsules may also be administered by carefully opening the capsule and sprinkling the pellets onto one tablespoonful of applesauce. Swallow the applesauce immediately without chewing and follow with a glass of cool water to ensure complete swallowing of the pellets. The applesauce used should not be hot and it should be soft enough to be swallowed without chewing. Use any pellet/applesauce mixture immediately and do not store for future use. Absorption of the pellets sprinkled onto other foods has not been tested. This method of administration may be beneficial for patients who have difficulty swallowing whole capsules. Subdividing the contents of a Verapamil Hydrochloride Extended-release Capsules (PM) capsule is not recommended.
paroxysmal supraventricular tachycardias
- Indication (injection only)
- Rapid conversion to sinus rhythm of paroxysmal supraventricular tachycardias, including those associated with accessory bypass tracts (Wolff-Parkinson-White [W-P-W] and Lown-Ganong- Levine [L-G-L] syndromes). When clinically advisable, appropriate vagal maneuvers (e.g., Valsalva maneuver) should be attempted prior to verapamil hydrochloride administration.
atrial flutter or atrial fibrillation
- Indication (injection only)
- Temporary control of rapid ventricular rate in atrial flutter or atrial fibrillation except when the atrial flutter and/or atrial fibrillation are associated with accessory bypass tracts (Wolff-Parkinson-White (W-P-W) and Lown-Ganong-Levine (L-G-L) syndromes).
- In controlled studies in the United States, about 60% of patients with supraventricular tachycardia converted to normal sinus rhythm within 10 minutes after intravenous verapamil hydrochloride. Uncontrolled studies reported in the world literature describe a conversion rate of about 80%. About 70% of patients with atrial flutter and/or fibrillation with a faster ventricular rate respond with a decrease in ventricular rate of at least 20%. Conversion of atrial flutter or fibrillation to sinus rhythm is uncommon (about 10%) after verapamil hydrochloride and may reflect the spontaneous conversion rate, since the conversion rate after placebo was similar. Slowing of the ventricular rate in patients with atrial fibrillation/flutter lasts 30 to 60 minutes after a single injection.
- Because a small fraction (<1%) of patients treated with verapamil hydrochloride respond with life-threatening adverse responses (rapid ventricular rate in atrial flutter/fibrillation, and an accessory bypass tract, marked hypotension, or extreme bradycardia/asystole − see CONTRAINDICATIONS and WARNINGS), the initial use of verapamil hydrochloride injection should, if possible, be in a treatment setting with monitoring and resuscitation facilities, including D.C.-cardioversion capability (see ADVERSE REACTIONS, Suggested Treatment of Acute Cardiovascular Adverse Reactions). As familiarity with the patient’s response is gained, use in an office setting may be acceptable.
- Cardioversion has been used safely and effectively after verapamil hydrochloride injection.
- Dosing information (injection)
- Initial dosage: 5 to 10 mg (0.075 to 0.15 mg/kg body weight) given as an intravenous bolus over at least 2 minutes.
- Repeat dosage: 10 mg (0.15 mg/kg body weight) 30 minutes after the first dose if the initial response is not adequate. An optimal interval for subsequent I.V. doses has not been determined, and should be individualized for each patient.
- Older patients − The dose should be administered over at least 3 minutes to minimize the risk of untoward drug effects.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Myocardial Infarction
- Class of Recommendation: Class I
- Level of Evidence: Not applicable
- Dosing Information
- Not applicable
Non–Guideline-Supported Use
Arteriosclerotic vascular disease
- Dosing Information
Amaurosis fugax
- Dosing information
Cluster headache
- Dosing information
Muscle Cramp
- Dosing information
Electroconvulsive therapy
- Dosing information
- 0.1 mg/kg[12]
Hypertrophic cardiomyopathy
- Dosing information
Keloid scar
- Dosing information
- Intralesional injection 0.5 to 2 mL [15]
Kidney disease
- Dosing information
- 180 mg/day [16]
Prophylaxis of Migraine
- Dosing information
- 80 mg qid [17]
Peyronie's disease
- Dosing information
- 5 mg [18]
Pulmonary hypertension
- Dosing information
Spasm of cerebral arteries
- Dosing information
- 20 mg [21]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- Dosing information
- Initial dose:
- 0 to 1 year: 0.1 to 0.2 mg/kg body weight (usual single dose range: 0.75 to 2 mg) should be administered as an intravenous bolus over at least 2 minutes under continuous ECG monitoring.
- 1 to 15 years: 0.1 to 0.3 mg/kg body weight (usual single dose range: 2 to 5 mg) should be administered as an intravenous bolus over at least 2 minutes. Do not exceed 5 mg.
- Repeat dose:
- 0 to 1 year: 0.1 to 0.2 mg/kg body weight (usual single dose range: 0.75 to 2 mg) 30 minutes after the first dose if the initial response is not adequate (under continuous ECG monitoring). An optimal interval for subsequent I.V. doses has not been determined, and should be individualized for each patient.
- 1 to 15 years: 0.1 to 0.3 mg/kg body weight (usual single dose range: 2 to 5 mg) 30 minutes after the first dose if the initial response is not adequate. Do not exceed 10 mg as a single dose. An optimal interval for subsequent I.V. doses has not been determined, and should be individualized for each patient.
- Note: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Use only if solution is clear and vial seal is intact. Unused amount of solution should be discarded immediately following withdrawal of any portion of contents.
- For stability reasons this product is not recommended for dilution with Sodium Lactate Injection, USP in polyvinyl chloride bags. Verapamil is physically compatible and chemically stable for at least 24 hours at 25°C protected from light in most common large volume parenteral solutions. Admixing verapamil hydrochloride injection with albumin, amphotericin B, hydralazine hydrochloride and trimethoprim with sulfamethoxazole should be avoided. Verapamil hydrochloride injection will precipitate in any solution with a pH above 6.0.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Verapamil in pediatric patients.
Non–Guideline-Supported Use
Cluster Headache
- Dosing information
- 4.3 to 5.5 mg/kg/day [22]
Hypertrophic cardiomyopathy
- Dosing information
Contraindications
Contradiction to Verapamil tablet and capsule, injection
1-Severe left ventricular dysfunction (see WARNINGS)
2-Hypotension (systolic pressure less than 90 mm Hg) or cardiogenic shock
3-Sick sinus syndrome (except in patients with a functioning artificial ventricular pacemaker)
4-degree AV block or third-degree AV block (except in patients with a functioning artificial ventricular pacemaker)
5-Patients with atrial flutter or atrial fibrillation and an accessory bypass tract (eg, Wolff-Parkinson-White, Lown-Ganong-Levine syndromes) (see WARNINGS)
6-Patients with known hypersensitivity to verapamil hydrochloride
Contradiction to Verapamil injection only
7.Severe congestive heart failure (unless secondary to a supraventricular tachycardia amenable to verapamil therapy). 8.Ventricular tachycardia: Administration of intravenous verapamil to patients with wide-complex ventricular tachycardia (QRS ≥ 0.12 sec) can result in marked hemodynamic deterioration and ventricular fibrillation. Proper pretherapy diagnosis and differentiation from wide-complex supraventricular tachycardia is imperative in the emergency room setting.
Warnings
Heart failure
Verapamil has a negative inotropic effect, which in most patients is compensated by its afterload reduction (decreased systemic vascular resistance) properties without a net impairment of ventricular performance. In clinical experience with 4,954 patients, 87 (1.8%) developed congestive heart failure orpulmonary edema. Verapamil should be avoided in patients with severe left ventricular dysfunction (eg, ejection fraction less than 30%) or moderate to severe symptoms of cardiac failure and in patients with any degree of ventricular dysfunction if they are receiving a beta-adrenergic blocker (see PRECAUTIONS, Drug interactions). Patients with milder ventricular dysfunction should, if possible, be controlled with optimum doses of digitalis and/or diuretics before verapamil treatment. (Note interactions with digoxin underPRECAUTIONS)
Hypotension
Occasionally, the pharmacologic action of verapamil may produce a decrease in blood pressure below normal levels, which may result in dizziness or symptomatic hypotension. The incidence of hypotension observed in 4,954 patients enrolled in clinical trials was 2.5%. In hypertensive patients, decreases in blood pressure below normal are unusual. Tilt-table testing (60 degrees) was not able to induceorthostatic hypotension.
Elevated liver enzymes
Elevations of transaminases with and without concomitant elevations in alkaline phosphatase and bilirubin have been reported. Such elevations have sometimes been transient and may disappear even with continued verapamil treatment. Several cases of hepatocellular injury related to verapamil have been proven by rechallenge; half of these had clinical symptoms (malaise, fever, and/or right upper quadrant pain), in addition to elevation of SGOT, SGPT, and alkaline phosphatase. Periodic monitoring of liver function in patients receiving verapamil is therefore prudent.
Accessory bypass tract (Wolff-Parkinson-White or Lown-Ganong-Levine)
Some patients with paroxysmal and/or chronic atrial fibrillation or atrial flutter and a coexisting accessory AV pathway have developed increased antegrade conduction across the accessory pathway bypassing the AV node, producing a very rapid ventricular response or ventricular fibrillation after receiving intravenous verapamil (or digitalis).
Although a risk of this occurring with oral verapamil has not been established, such patients receiving oral verapamil may be at risk and its use in these patients is contraindicated (see CONTRAINDICATIONS). Treatment is usually DC-cardioversion. Cardioversion has been used safely and effectively after oral Verapamil.
Atrioventricular block
The effect of verapamil on AV conduction and the SA node may cause asymptomatic first-degree AV block and transient bradycardia, sometimes accompanied by nodal escape rhythms. PR-interval prolongation is correlated with verapamil plasma concentrations especially during the early titration phase of therapy. Higher degrees of AV block, however, were infrequently (0.8%) observed. Marked first-degree block or progressive development to second-degree AV blockor third-degree AV block requires a reduction in dosage or, in rare instances, discontinuation of verapamil HCl and institution of appropriate therapy, depending on the clinical situation.
Patients with hypertrophic cardiomyopathy (IHSS)
In 120 patients with hypertrophic cardiomyopathy (most of them refractory or intolerant to propranolol) who received therapy with verapamil at doses up to 720 mg/day, a variety of serious adverse effects were seen. Three patients died in pulmonary edema; all had severe left ventricular outflow obstruction and a past history of left ventricular dysfunction. Eight other patients hadpulmonary edema and/or severe hypotension; abnormally high (greater than 20 mm Hg) pulmonary wedge pressure and a marked left ventricular outflow obstruction were present in most of these patients. Concomitant administration of quinidine (see PRECAUTIONS, Drug interactions) preceded the severe hypotension in 3 of the 8 patients (2 of whom developed pulmonary edema). Sinus bradycardia occurred in 11% of the patients, second-degree AV block in 4%, and sinus arrest in 2%. It must be appreciated that this group of patients had a serious disease with a high mortality rate. Most adverse effects responded well to dose reduction, and only rarely did verapamil use have to be discontinued.
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Verapamil Clinical Trials Experience in the drug label.
Postmarketing Experience
There is limited information regarding Verapamil Postmarketing Experience in the drug label.
Drug Interactions
Cytochrome inducers/inhibitors
In vitro metabolic studies indicate that verapamil is metabolized by cytochrome P450 CYP3A4, CYP1A2, CYP2C8, CYP2C9, and CYP2C18. Clinically significant interactions have been reported with inhibitors of CYP3A4 (e.g., erythromycin, ritonavir) causing elevation of plasma levels of verapamil while inducers of CYP3A4 (e.g., rifampin) have caused a lowering of plasma levels of verapamil.
HMG-CoA reductase inhibitors
The use of statins that are CYP3A4 substrates in combination with verapamil has been associated with reports of myopathy/rhabdomyolysis.
Co-administration of multiple doses of 10 mg of verapamil with 80 mg simvastatin resulted in exposure to simvastatin 2.5-fold that following simvastatin alone. Limit the dose of simvastatin in patients on verapamil to 10 mg daily. Limit the daily dose of lovastatin to 40 mg. Lower starting and maintenance doses of other CYP3A4 substrates (e.g., atorvastatin) may be required as verapamil may increase the plasma concentration of these drugs.
Aspirin
In a few reported cases, co-administration of verapamil with aspirin has led to increased bleeding times greater than observed with aspirin alone.
Grapefruit juice
Grapefruit juice may increase plasma levels of verapamil.
Alcohol
Verapamil may increase blood alcohol concentrations and prolong its effects.
Beta-blockers
Controlled studies in small numbers of patients suggest that the concomitant use of Verapamil and oral beta-adrenergic blocking agents may be beneficial in certain patients with chronic stable angina or hypertension, but available information is not sufficient to predict with confidence the effects of concurrent treatment in patients with left ventricular dysfunction or cardiac conduction abnormalities. Concomitant therapy with beta-adrenergic blockers and verapamil may result in additive negative effects on heart rate, atrioventricular conduction and/or cardiac contractility.
In one study involving 15 patients treated with high doses of propranolol (median dose: 480 mg/day; range: 160 to 1,280 mg/day) for severe angina, with preserved left ventricular function (ejection fraction greater than 35%), the hemodynamic effects of additional therapy with verapamil HCl were assessed using invasive methods. The addition of verapamil to high-dosebeta-blockers induced modest negative inotropic and chronotropic effects that were not severe enough to limit short-term (48 hours) combination therapy in this study. These modest cardiodepressant effects persisted for greater than 6 but less than 30 hours after abrupt withdrawal of beta-blockers and were closely related to plasma levels of propranolol. The primary verapamil/beta-blocker interaction in this study appeared to be hemodynamic rather than electrophysiologic.
In other studies, verapamil did not generally induce significant negative inotropic, chronotropic, or dromotropic effects in patients with preserved left ventricular function receiving low or moderate doses of propranolol (less than or equal to 320 mg/day); in some patients, however, combined therapy did produce such effects. Therefore, if combined therapy is used, close surveillance of clinical status should be carried out. Combined therapy should usually be avoided in patients with atrioventricular conduction abnormalities and those with depressed left ventricular function.
Asymptomatic bradycardia (36 beats/min) with a wandering atrial pacemaker has been observed in a patient receiving concomitant timolol (a beta-adrenergic blocker) eyedrops and oral verapamil.
A decrease in metoprolol and propranolol clearance has been observed when either drug is administered concomitantly with verapamil. A variable effect has been seen when verapamil and atenolol were given together.
Digitalis
Clinical use of verapamil in digitalized patients has shown the combination to be well tolerated if digoxin doses are properly adjusted. However, chronic verapamil treatment can increase serum digoxin levels by 50% to 75% during the first week of therapy, and this can result in digitalis toxicity. In patients with hepatic cirrhosis, the influence of verapamil on digoxin kinetics is magnified. Verapamil may reduce total body clearance and extrarenal clearance of digitoxin by 27% and 29%, respectively. Maintenance and digitalization doses should be reduced when verapamil is administered, and the patient should be reassessed to avoid over- or under-digitalization. Whenever over-digitalization is suspected, the daily dose of digitalis should be reduced or temporarily discontinued. On discontinuation of Verapamil use, the patient should be reassessed to avoid under-digitalization.
Antihypertensive agents
Verapamil administered concomitantly with oral antihypertensive agents (e.g., vasodilators, angiotensin-converting enzyme inhibitors, diuretics, beta-blockers) will usually have an additive effect on lowering blood pressure. Patients receiving these combinations should be appropriately monitored. Concomitant use of agents that attenuate alpha-adrenergic function with verapamil may result in a reduction in blood pressure that is excessive in some patients. Such an effect was observed in one study following the concomitant administration of verapamil and prazosin.
Antiarrhythmic agents
Disopyramide
Until data on possible interactions between verapamil and disopyramide are obtained, disopyramide should not be administered within 48 hours before or 24 hours after verapamil administration.
Flecainide
A study in healthy volunteers showed that the concomitant administration of flecainide and verapamil may have additive effects on myocardial contractility, AV conduction, and repolarization. Concomitant therapy with flecainide and verapamil may result in additive negative inotropic effect and prolongation of atrioventricular conduction.
Quinidine
In a small number of patients with hypertrophic cardiomyopathy (IHSS), concomitant use of verapamil and quinidine resulted in significant hypotension. Until further data are obtained, combined therapy of verapamil and quinidine in patients with hypertrophic cardiomyopathy should probably be avoided.
The electrophysiologic effects of quinidine and verapamil on AV conduction were studied in 8 patients. Verapamil significantly counteracted the effects of quinidine on AV conduction. There has been a report of increased quinidine levels during verapamil therapy.
Other agents
Nitrates
Verapamil has been given concomitantly with short- and long-acting nitrates without any undesirable drug interactions. The pharmacologic profile of both drugs and the clinical experience suggest beneficial interactions.
Cimetidine
The interaction between cimetidine and chronically administered verapamil has not been studied. Variable results on clearance have been obtained in acute studies of healthy volunteers; clearance of verapamil was either reduced or unchanged.
Lithium
Increased sensitivity to the effects of lithium (neurotoxicity) has been reported during concomitant verapamil-lithium therapy; lithium levels have been observed sometimes to increase, sometimes to decrease, and sometimes to be unchanged. Patients receiving both drugs must be monitored carefully.
Carbamazepine
Verapamil therapy may increase carbamazepine concentrations during combined therapy. This may produce carbamazepine side effects such as diplopia, headache, ataxia, or dizziness.
Rifampin
Therapy with rifampin may markedly reduce oral verapamil bioavailability.
Phenobarbital
Phenobarbital therapy may increase verapamil clearance.
Cyclosporine
Verapamil therapy may increase serum levels of cyclosporine.
Theophylline Verapamil may inhibit the clearance and increase the plasma levels of theophylline.
Inhalation anesthetics
Animal experiments have shown that inhalation anesthetics depress cardiovascular activity by decreasing the inward movement of calcium ions. When used concomitantly, inhalation anesthetics and calcium antagonists, such as verapamil, should each be titrated carefully to avoid excessive cardiovascular depression.
Neuromuscular blocking agents
Clinical data and animal studies suggest that verapamil may potentiate the activity of neuromuscular blocking agents (curare-like and depolarizing). It may be necessary to decrease the dose of verapamil and/or the dose of the neuromuscular blocking agent when the drugs are used concomitantly.
Telithromycin
Hypotension and bradyarrhythmias have been observed in patients receiving concurrent telithromycin, an antibiotic in the ketolide class.
Clonidine
Sinus bradycardia resulting in hospitalization and pacemaker insertion has been reported in association with the use of clonidine concurrently with verapamil. Monitor heart rate in patients receiving concomitant verapamil and clonidine.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Reproduction studies have been performed in rabbits and rats at oral doses up to 1.5 (15 mg/kg/day) and 6 (60 mg/kg/day) times the human oral daily dose, respectively, and have revealed no evidence of teratogenicity. In the rat, however, this multiple of the human dose was embryocidal and retarded fetal growth and development, probably because of adverse maternal effects reflected in reduced weight gains of the dams. This oral dose has also been shown to cause hypotension in rats. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. Verapamil crosses the placental barrier and can be detected in umbilical vein blood at delivery.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Verapamil in women who are pregnant.
Labor and Delivery
It is not known whether the use of verapamil during labor or delivery has immediate or delayed adverse effects on the fetus, or whether it prolongs the duration of labor or increases the need for forceps delivery or other obstetric intervention. Such adverse experiences have not been reported in the literature, despite a long history of use of verapamil in Europe in the treatment of cardiac side effects of beta-adrenergic agonist agents used to treat premature labor.
Nursing Mothers
Verapamil is excreted in human milk. Because of the potential for adverse reactions in nursing infants from verapamil, nursing should be discontinued while verapamil is administered.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
There is no FDA guidance on the use of Verapamil in geriatric settings.
Gender
There is no FDA guidance on the use of Verapamil with respect to specific gender populations.
Race
There is no FDA guidance on the use of Verapamil with respect to specific racial populations.
Renal Impairment
About 70% of an administered dose of verapamil is excreted as metabolites in the urine. Verapamil is not removed by hemodialysis. Until further data are available, verapamil should be administered cautiously to patients with impaired renal function. These patients should be carefully monitored for abnormal prolongation of the PR interval or other signs of overdosage (see OVERDOSAGE).
Hepatic Impairment
Since verapamil is highly metabolized by the liver, it should be administered cautiously to patients with impaired hepatic function. Severe liver dysfunction prolongs the elimination half-life of verapamil to about 14 to 16 hours; hence, approximately 30% of the dose given to patients with normal liver function should be administered to these patients. Careful monitoring for abnormal prolongation of the PR interval or other signs of excessive pharmacologic effects (see OVERDOSAGE) should be carried out.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Verapamil in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Verapamil in patients who are immunocompromised.
Use in patients with attenuated (decreased) neuromuscular transmission
It has been reported that verapamil decreases neuromuscular transmission in patients with Duchenne's muscular dystrophy, prolongs recovery from the neuromuscular blocking agent vecuronium, and causes a worsening of myasthenia gravis. It may be necessary to decrease the dosage of verapamil when it is administered to patients with attenuated neuromuscular transmission.
Administration and Monitoring
Administration
Oral, intravenous
Monitoring
FDA Package Insert for Verapamil contains no information regarding drug monitoring.
IV Compatibility
FDA Package Insert for Verapamil contains no information regarding IV compatibility.
Overdosage
Treat all verapamil overdoses as serious and maintain observation for at least 48 hours (especially Verapamil SR), preferably under continuous hospital care. Delayed pharmacodynamic consequences may occur with the sustained-release formulation. Verapamil is known to decrease gastrointestinal transit time.
Treatment of overdosage should be supportive. Beta-adrenergic stimulation or parenteral administration of calcium solutions may increase calcium ion flux across the slow channel and have been used effectively in treatment of deliberate overdosage with verapamil. In a few reported cases, overdose with calcium channel blockers has been associated with hypotension and bradycardia, initially refractory to atropine but becoming more responsive to this treatment when the patients received large doses (close to 1 gram/hour for more than 24 hours) of calcium chloride. Verapamil cannot be removed by hemodialysis. Clinically significant hypotensive reactions or high degree AV block should be treated with vasopressor agents or cardiac pacing, respectively. Asystole should be handled by the usual measures including cardiopulmonary resuscitation.
Pharmacology
| |
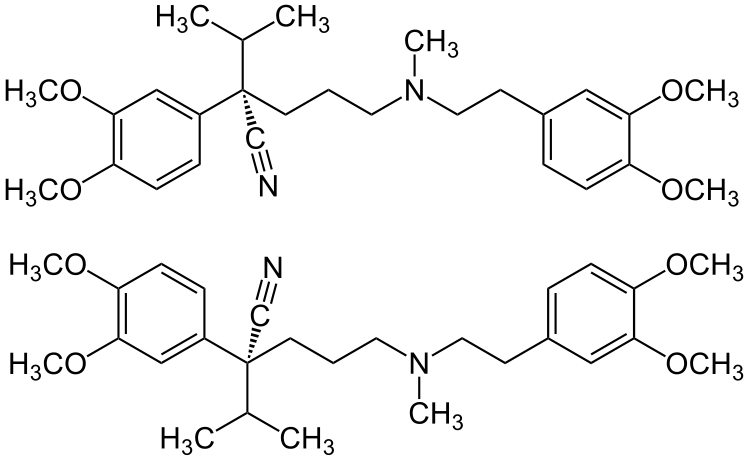
1 : 1 mixture (racemic mixture)Verapamil
| |
| Systematic (IUPAC) name | |
| (RS)-2-(3,4-dimethoxyphenyl)-5-{[2-(3,4-dimethoxyphenyl)ethyl]- (methyl)amino}-2-prop-2-ylpentanenitrile | |
| Identifiers | |
| CAS number | |
| ATC code | C08 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 454.602 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 35.1% |
| Metabolism | Hepatic |
| Half life | 2.8-7.4 hours |
| Excretion | Renal: 11% |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. |
C(US) |
| Legal status |
Template:Unicode Prescription only |
| Routes | Oral, Intravenous |
Mechanism of Action
Angina
The precise mechanism of action of Verapamil as an antianginal agent remains to be fully determined, but includes the following two mechanisms:
Relaxation and prevention of coronary artery spasm: Verapamil dilates the main coronary arteries and coronary arterioles, both in normal and ischemic regions, and is a potent inhibitor of coronary artery spasm, whether spontaneous or ergonovine-induced. This property increases myocardial oxygen delivery in patients with coronary artery spasm and is responsible for the effectiveness of Verapamil in vasospastic (Prinzmetal's or variant) as well as unstable angina at rest. Whether this effect plays any role in classical effort angina is not clear, but studies of exercise tolerance have not shown an increase in the maximum exercise rate–pressure product, a widely accepted measure of oxygen utilization. This suggests that, in general, relief of spasm or dilation of coronary arteries is not an important factor in classical angina.
Reduction of oxygen utilization: Verapamil regularly reduces the total peripheral resistance (afterload) against which the heart works both at rest and at a given level of exercise by dilating peripheral arterioles. This unloading of the heart reduces myocardial energy consumption and oxygen requirements and probably accounts for the effectiveness of Verapamil in chronic stable effort angina.
Arrhythmia
Electrical activity through the AV node depends, to a significant degree, upon calcium influx through the slow channel. By decreasing the influx of calcium, Verapamil prolongs the effective refractory period within the AV node and slows AV conduction in a rate-related manner. This property accounts for the ability of Verapamil to slow the ventricular rate in patients with chronic atrial flutter or atrial fibrillation.
Normal sinus rhythm is usually not affected, but in patients with sick sinus syndrome, Verapamil may interfere with sinus-node impulse generation and may induce sinus arrest or sinoatrial block. Atrioventricular block can occur in patients without preexisting conduction defects (seeWARNINGS). Verapamil decreases the frequency of episodes of paroxysmal supraventricular tachycardia. Verapamil does not alter the normal atrial action potential or intraventricular conduction time, but in depressed atrial fibers it decreases amplitude, velocity of depolarization, and conduction velocity. Verapamil may shorten the antegrade effective refractory period of the accessory bypass tract. Acceleration of ventricular rate and/or ventricular fibrillation has been reported in patients with atrial flutter or atrial fibrillation and a coexisting accessory AV pathway following administration of verapamil (see WARNINGS). Verapamil has a local anesthetic action that is 1.6 times that of procaine on an equimolar basis. It is not known whether this action is important at the doses used in man.
Essential hypertension
Verapamil exerts antihypertensive effects by decreasing systemic vascular resistance, usually without orthostatic decreases in blood pressure or reflex tachycardia; bradycardia (rate less than 50 beats/min) is uncommon (1.4%). During isometric or dynamic exercise, Verapamil does not alter systolic cardiac function in patients with normal ventricular function.
Verapamil does not alter total serum calcium levels. However, one report suggested that calcium levels above the normal range may alter the therapeutic effect of Verapamil.
Structure
Verapamil hydrochloride is a calcium antagonist or slow-channel inhibitor. Verapamil Hydrochloride Injection, USP is a sterile, nonpyrogenic solution containing verapamil hydrochloride 2.5 mg/mL and sodium chloride 8.5 mg/mL in water for injection. The solution contains no bacteriostat or antimicrobial agent and is intended for single-dose intravenous administration. May contain hydrochloric acid for pH adjustment; pH is 4.9 (4.0 to 6.5). The chemical name of Verapamil Hydrochloride, USP is benzeneacetonitrile, α-[3-[{2-(3,4-dimethoxyphenyl)ethyl} methylamino] propyl]-3,4-dimethoxy-α-(1-methylethyl) hydrochloride. Verapamil hydrochloride is a white or practically white crystalline powder. It is practically odorless and has a bitter taste. It is soluble in water; freely soluble in chloroform; sparingly soluble in alcohol; practically insoluble in ether. It has the following structural formula:

Molecular weight: 491.07 Molecular formula: C27H38N2O4 • HCl Verapamil hydrochloride is not chemically related to other antiarrhythmic drugs.
Pharmacodynamics
Verapamil reduces afterload and myocardial contractility. Improved left ventricular diastolic function in patients with Idiopathic Hypertrophic Subaortic Stenosis (IHSS) and those with coronary heart disease has also been observed with Verapamil therapy. In most patients, including those with organic cardiac disease, the negative inotropic action of Verapamil is countered by reduction of afterload, and cardiac index is usually not reduced. However, in patients with severe left ventricular dysfunction (eg,pulmonary wedge pressure above 20 mm Hg or ejection fraction less than 30%), or in patients taking beta-adrenergic blocking agents or other cardiodepressant drugs, deterioration of ventricular function may occur (see PRECAUTIONS, Drug Interactions).
Pharmacokinetics
More than 90% of the orally administered dose of Verapamil is absorbed. Because of rapid biotransformation of verapamil during its first pass through the portal circulation, bioavailability ranges from 20% to 35%. Peak plasma concentrations are reached between 1 and 2 hours after oral administration. Chronic oral administration of 120 mg of verapamil HCl every 6 hours resulted in plasma levels of verapamil ranging from 125 to 400 ng/ml, with higher values reported occasionally. A nonlinear correlation between the verapamil dose administered and verapamil plasma levels does exist. No relationship has been established between the plasma concentration of verapamil and a reduction in blood pressure. In early dose titration with verapamil, a relationship exists between verapamil plasma concentration and prolongation of the PR interval. However, during chronic administration this relationship may disappear. The mean elimination half-life in single-dose studies ranged from 2.8 to 7.4 hours. In these same studies, after repetitive dosing, the half-life increased to a range from 4.5 to 12.0 hours (after less than 10 consecutive doses given 6 hours apart). Half-life of verapamil may increase during titration. Aging may affect the pharmacokinetics of verapamil. Elimination half-life may be prolonged in the elderly. In healthy men, orally administered Verapamil undergoes extensive metabolism in the liver. Twelve metabolites have been identified in plasma; all except norverapamil are present in trace amounts only.
Norverapamil can reach steady-state plasma concentrations approximately equal to those of verapamil itself. The cardiovascular activity of norverapamil appears to be approximately 20% that of verapamil. Approximately 70% of an administered dose is excreted as metabolites in the urine and 16% or more in the feces within 5 days. About 3% to 4% is excreted in the urine as unchanged drug. Approximately 90% is bound to plasma proteins. In patients with hepatic insufficiency, metabolism is delayed and elimination half-life prolonged up to 14 to 16 hours (seePRECAUTIONS); the volume of distribution is increased and plasma clearance reduced to about 30% of normal. Verapamil clearance values suggest that patients with liver dysfunction may attain therapeutic verapamil plasma concentrations with one third of the oral daily dose required for patients with normal liver function. After four weeks of oral dosing (120 mg q.i.d.), verapamil and norverapamil levels were noted in the cerebrospinal fluid with estimated partition coefficient of 0.06 for verapamil and 0.04 for norverapamil.
Nonclinical Toxicology
Carcinogenesis, mutagenesis, impairment of fertility
An 18-month toxicity study in rats, at a low multiple (6-fold) of the maximum recommended human dose, and not the maximum tolerated dose, did not suggest a tumorigenic potential. There was no evidence of a carcinogenic potential of verapamil administered in the diet of rats for two years at doses of 10, 35, and 120 mg/kg/day or approximately 1, 3.5, and 12 times, respectively, the maximum recommended human daily dose (480 mg/day or 9.6 mg/kg/day).
Verapamil was not mutagenic in the Ames test in 5 test strains at 3 mg per plate with or without metabolic activation.
Studies in female rats at daily dietary doses up to 5.5 times (55 mg/kg/day) the maximum recommended human dose did not show impaired fertility. Effects on male fertility have not been determined.
Animal pharmacology and/or animal toxicology
In chronic animal toxicology studies, verapamil caused lenticular and/or suture line changes at 30 mg/kg/day or greater, and frank cataracts at 62.5 mg/kg/day or greater in the beagle dog but not in the rat. Development of cataracts due to verapamil has not been reported in man.
Clinical Studies
FDA Package Insert for Verapamil contains no information regarding clinical studies.
How Supplied
Verapamil tablet
Verapamil Hydrochloride Extended-Release Tablets, USP 120 mg are supplied as ivory, round, unscored, film-coated tablets debossed with “120” on one side
on the other side, packaged in bottles of 100 tablets and unit-dose boxes of 100 tablets. Verapamil Hydrochloride Extended-Release Tablets USP, 180 mg are supplied as light orange, capsule-shaped, scored, film-coated tablets debossed with “7301” on one side,
on the other side, packaged in bottles of 100 and 500 tablets and unit-dose boxes of 100 tablets. Verapamil Hydrochloride Extended-Release Tablets USP, 240 mg are supplied as ivory, capsule-shaped, scored, film-coated tablets debossed with “7300” on one side,
on the other side, packaged in bottles of 100 and 500 tablets and unit-dose boxes of 100 tablets.
Verapamil capsule
Verapamil Hydrochloride Extended-release Capsules (PM); pellet filled capsules are supplied in three dosage strengths:

Verapamil injection
Verapamil Hydrochloride Injection, USP 2.5 mg/mL is supplied in single-dose containers as follows:

Storage
Verapamil tablet
Store between 20˚ to 25˚ C (68˚ to 77˚ F) [See USP Controlled Room Temperature].
Verapamil capsule
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F). [See USP Controlled Room Temperature]. Protect from moisture. Dispense in tight, light-resistant container as defined in USP.
Verapamil injection
Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.] Protect from light by retaining in package until ready to use.
Images
Drug Images
{{#ask: Page Name::Verapamil |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Verapamil |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Verapamil Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Verapamil interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Verapamil
- Verapamil SR
- Covera-HS
- Isoptin SR
- Verelan
- Verelan PM
Look-Alike Drug Names
FDA Package Insert for Verapamil contains no information regarding look-alike names.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Schneider W, Kober G, Roebruck P, Noack H, Alle M, Cieslinski G; et al. (1990). "Retardation of development and progression of coronary atherosclerosis: a new indication for calcium antagonists?". Eur J Clin Pharmacol. 39 Suppl 1: S17–23. PMID 2261941.
- ↑ Schweizer J, Kirch W, Koch R, Hellner G, Uhlmann K (1998). "Effect of high dose verapamil on restenosis after peripheral angioplasty". J Am Coll Cardiol. 31 (6): 1299–305. PMID 9581724.
- ↑ Winterkorn JM, Kupersmith MJ, Wirtschafter JD, Forman S (1993). "Brief report: treatment of vasospastic amaurosis fugax with calcium-channel blockers". N Engl J Med. 329 (6): 396–8. doi:10.1056/NEJM199308053290604. PMID 8326973.
- ↑ Winterkorn JM, Teman AJ (1991). "Recurrent attacks of amaurosis fugax treated with calcium channel blocker". Ann Neurol. 30 (3): 423–5. doi:10.1002/ana.410300317. PMID 1952830.
- ↑ Gabai IJ, Spierings EL (1989). "Prophylactic treatment of cluster headache with verapamil". Headache. 29 (3): 167–8. PMID 2708046.
- ↑ Gabai IJ, Spierings EL (1990). "Diagnosis and management of cluster headaches". Nurse Pract. 15 (10): 32–6. PMID 2234557.
- ↑ Figuerola ML, Levin G, Leston J, Barontini M (1994). "Opioid and sympathetic nervous system activity in cluster headache under verapamil or prednisone treatment". Headache. 34 (5): 257–60. PMID 8026943.
- ↑ Leone M, D'Amico D, Frediani F, Moschiano F, Grazzi L, Attanasio A; et al. (2000). "Verapamil in the prophylaxis of episodic cluster headache: a double-blind study versus placebo". Neurology. 54 (6): 1382–5. PMID 10746617.
- ↑ Baltodano N, Gallo BV, Weidler DJ (1988). "Verapamil vs quinine in recumbent nocturnal leg cramps in the elderly". Arch Intern Med. 148 (9): 1969–70. PMID 3046538.
- ↑ 10.0 10.1 Walton J (1981). "Diffuse exercise-induced muscle pain of undetermined cause relieved by verapamil". Lancet. 1 (8227): 993. PMID 6112398.
- ↑ Kimose HH, Bagger JP, Aagaard MT, Paulsen PK (1990). "Placebo-controlled, double-blind study of the effect of verapamil in intermittent claudication". Angiology. 41 (8): 595–8. PMID 2202231.
- ↑ Wajima Z, Yoshikawa T, Ogura A, Imanaga K, Shiga T, Inoue T; et al. (2002). "Intravenous verapamil blunts hyperdynamic responses during electroconvulsive therapy without altering seizure activity". Anesth Analg. 95 (2): 400–2, table of contents. PMID 12145060.
- ↑ Bonow RO, Rosing DR, Bacharach SL, Green MV, Kent KM, Lipson LC; et al. (1981). "Effects of verapamil on left ventricular systolic function and diastolic filling in patients with hypertrophic cardiomyopathy". Circulation. 64 (4): 787–96. PMID 7196813.
- ↑ Petkow Dimitrow P, Krzanowski M, Nizankowski R, Szczeklik A, Dubiel JS (2000). "Effect of verapamil on systolic and diastolic coronary blood flow velocity in asymptomatic and mildly symptomatic patients with hypertrophic cardiomyopathy". Heart. 83 (3): 262–6. PMC 1729332. PMID 10677401.
- ↑ Lawrence WT (1996). "Treatment of earlobe keloids with surgery plus adjuvant intralesional verapamil and pressure earrings". Ann Plast Surg. 37 (2): 167–9. PMID 8863976.
- ↑ Muijsers RB, Curran MP, Perry CM (2002). "Fixed combination trandolapril/verapamil sustained-release: a review of its use in essential hypertension". Drugs. 62 (17): 2539–67. PMID 12421112.
- ↑ Solomon GD, Steel JG, Spaccavento LJ (1983). "Verapamil prophylaxis of migraine. A double-blind, placebo-controlled study". JAMA. 250 (18): 2500–2. PMID 6355533.
- ↑ Riedl CR, Plas E, Engelhardt P, Daha K, Pflüger H (2000). "Iontophoresis for treatment of Peyronie's disease". J Urol. 163 (1): 95–9. PMID 10604323.
- ↑ Malcić I, Richter D (1985). "Verapamil in primary pulmonary hypertension". Br Heart J. 53 (3): 345–7. PMC 481767. PMID 3970793.
- ↑ Kopman EA (1983). "Intravenous verapamil to relieve pulmonary congestion in patients with mitral valve disease". Anesthesiology. 58 (4): 374–6. PMID 6837978.
- ↑ Keuskamp J, Murali R, Chao KH (2008). "High-dose intraarterial verapamil in the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage". J Neurosurg. 108 (3): 458–63. doi:10.3171/JNS/2008/108/3/0458. PMID 18312091.
- ↑ Shabbir N, McAbee G (1994). "Adolescent chronic paroxysmal hemicrania responsive to verapamil monotherapy". Headache. 34 (4): 209–10. PMID 8014035.
- ↑ Moran AM, Colan SD (1998). "Verapamil therapy in infants with hypertrophic cardiomyopathy". Cardiol Young. 8 (3): 310–9. PMID 9731645.
- ↑ Pacileo G, De Cristofaro M, Russo MG, Sarubbi B, Pisacane C, Calabrò R (2000). "Hypertrophic cardiomyopathy in pediatric patients: effect of verapamil on regional and global left ventricular diastolic function". Can J Cardiol. 16 (2): 146–52. PMID 10694584.
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_120 mg_NDC 0172-4285.jpg |Drug Name=verapamil hydrochloride tablet, film coated, extended release |Pill Ingred=magnesium stearate, cellulose, microcrystalline, povidones, sodium alginate, hypromelloses, polydextrose, polyethylene glycols, titanium dioxide, triacetin, ferric oxide yellow|+sep=; |Pill Imprint=120 |Pill Dosage=120 mg |Pill Color=White|+sep=; |Pill Shape=Round |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=IVAX Pharmaceuticals, Inc. |NDC=0172-4285
}}
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_180 mg_NDC 0172-4286.jpg |Drug Name=Verapamil hydrochloride 180 MG Extended Release Tablet |Pill Ingred=magnesium stearate, cellulose, microcrystalline, povidones, sodium alginate, hypromelloses, polydextrose, polyethylene glycols, titanium dioxide, triacetin, ferric oxide yellow|+sep=; |Pill Imprint=7301 |Pill Dosage=180 mg |Pill Color=Orange|+sep=; |Pill Shape=Oval |Pill Size (mm)=16.00 |Pill Scoring=2 |Pill Image= |Drug Author=IVAX Pharmaceuticals, Inc. |NDC=0172-4286
}}
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_240 mg_NDC 0172-4280.jpg |Drug Name=Verapamil hydrochloride 240 MG Extended Release Tablet |Pill Ingred=magnesium stearate, cellulose, microcrystalline, povidones, sodium alginate, hypromelloses, polydextrose, polyethylene glycols, titanium dioxide, triacetin, ferric oxide yellow|+sep=; |Pill Imprint=7300 |Pill Dosage=240 mg |Pill Color=White|+sep=; |Pill Shape=Oval |Pill Size (mm)=18.00 |Pill Scoring=2 |Pill Image= |Drug Author=IVAX Pharmaceuticals, Inc. |NDC=0172-4280
}}
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_100 mg_NDC 62175-485.jpg |Drug Name=Verapamil hydrochloride 100 MG 24 HR Extended Release Capsule |Pill Ingred=d&c red no. 28, fd&c blue no. 1, fd&c red no. 40, fumaric acid, gelatin, povidone, shellac, silicon dioxide, sodium lauryl sulfate, talc, titanium dioxide|+sep=; |Pill Imprint=KU;485;100;mg |Pill Dosage=100 mg |Pill Color=Purple|+sep=; |Pill Shape=Capsule |Pill Size (mm)=18.00 |Pill Scoring=1 |Pill Image= |Drug Author=Kremers Urban Pharmaceuticals Inc. |NDC=62175-485
}}
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_200 mg_NDC 62175-486.jpg |Drug Name=Verapamil hydrochloride 200 MG 24 HR Extended Release Capsule |Pill Ingred=d&c red no. 28, fd&c blue no. 1, fd&c red no. 40, fumaric acid, gelatin, povidone, shellac, silicon dioxide, sodium lauryl sulfate, talc, titanium dioxide|+sep=; |Pill Imprint=KU;486;200;mg |Pill Dosage=200 mg |Pill Color=Purple|+sep=; |Pill Shape=Capsule |Pill Size (mm)=22.00 |Pill Scoring=1 |Pill Image= |Drug Author=Kremers Urban Pharmaceuticals Inc. |NDC=62175-486
}}
{{#subobject:
|Page Name=Verapamil |Pill Name=Verapamil_300 mg_NDC 62175-487.jpg |Drug Name=Verapamil hydrochloride 300 MG 24 HR Extended Release Capsule |Pill Ingred=d&c red no. 28, fd&c blue no. 1, fd&c red no. 40, fumaric acid, gelatin, povidone, shellac, silicon dioxide, sodium lauryl sulfate, talc, titanium dioxide|+sep=; |Pill Imprint=KU;487;300;mg |Pill Dosage=300 mg |Pill Color=Purple|+sep=; |Pill Shape=Capsule |Pill Size (mm)=23.00 |Pill Scoring=1 |Pill Image= |Drug Author=Kremers Urban Pharmaceuticals Inc. |NDC=62175-487
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 01.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 02.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 03.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 04.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 05.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 06.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 07.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 08.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil label 09.jpg
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 01.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 02.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 03.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 04.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 05.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 06.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 07.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 08.png
}}
{{#subobject:
|Label Page=Verapamil |Label Name=Verapamil panel 09.png
}}