Mitral regurgitation resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]; Mugilan Poongkunran M.B.B.S [3]
| Mitral Regurgitation Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Complete Diagnostic Approach |
| Treatment |
| Do's |
| Don'ts |
Overview
Mitral regurgitation (MR), mitral insufficiency or mitral incompetence refers to a disorder of the heart in which the mitral valve fails to close properly during systole. This leads to leakage of blood flow from left ventricle to left atrium during systole and reduction in cardiac output. The symptoms associated with mitral regurgitation are dependent on which phase of the disease process the individual is in. Individuals with acute mitral regurgitation are often gravely ill with significant hemodynamic abnormalities due to decompensated congestive heart failure and low cardiac output that require urgent treatment, whereas individuals with chronic compensated mitral regurgitation may be asymptomatic, with a normal exercise tolerance and no evidence of heart failure.[1] The management of chronic MR depends on whether the condition is chronic primary MR (the mitral valve is usually abnormal) or chronic secondary MR (the mitral valve is usually normal) and the severity of the valve anatomy.[2]
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Acute Mitral Regurgitation
- Papillary muscle rupture: Acute myocardial infarction, chest trauma, ischemia
- Ruptured mitral chordae tendinae: Acute rheumatic fever, chest trauma, mitral valve prolapse, infective endocarditis, spontaneous rupture[3][4][5]
Chronic Primary Mitral Regurgitation
Chronic Secondary Mitral Regurgitation
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in salmon colour signify that an urgent management is needed
Identify cardinal findings that increase the pretest probability of mitral regurgitation: ❑ Murmur:
❑ Heart sounds: | |||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings of acute mitral regurgitation? ❑ Sudden onset and rapid progression of pulmonary edema:
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
| Continue with complete diagnostic approach below | |||||||||||||||||||||||||||||||||||||||
Initial resusticative measures: ❑ Secure airway Order transthoracic echocardiography (TTE) (urgent): ❑ Confirmatory Initiate medical therapy: ❑ Vasodilator therapy AND Consider the following: ❑ Pulmonary artery catheterization | |||||||||||||||||||||||||||||||||||||||
Ischemic mitral regurgitation: Initiate medical therapy: ❑ In cases of reduced LVEF Reperfusion or revascularization Mitral valve surgery: ❑ Papillary muscle rupture
Cardiac transplantation: ❑ On some occasions with no contraindication for surgery | MR due to cardiomyopathy: Heart failure management: ❑ Click here for acute heart failure resident survival guide
Mitral valve surgery: ❑ When there is no response to medical management ❑ Mitral valve replacement or mitral valve repair | MR due to infective endocarditis: Mitral valve surgery:
Initiate medical therapy: | |||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach to Mitral Regurgitation
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention. Shown below is an algorithm summarizing the complete diagnostic approach to mitral regurgitation according to 2014 AHA/ACC guidelines for management of valvular heart disease.[2].
AF: Atrial fibrillation; MR: Mitral regurgitation; EKG: Electrocardiogram; EF: Ejection fraction; S1: First heart sound; S2: Second heart sound; S3: Third heart sound; LV: Left ventricle; MVP: Mitral valve prolapse
Characterize the symptoms: Acute mitral regurgitation: ❑ Symptoms of shock and pulmonary edema:
❑ Symptoms suggestive of precipitating events:
Chronic mitral regurgitation:
❑ Symptoms associated with decreased forward flow and increased backflow across mitral valve:
❑ Symptoms associated with complications:
❑Other etiology associated symptoms:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: ❑ Past medical history:
❑ Family history: ❑ Medications: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vital signs:
Skin: Cardiovascular system:
❑ Thrill (in acute MR and severe chronic MR)
Auscultation:
❑ Murmur
Respiratory system: Abdominal system: Neurological system: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order electrocardiogram (Urgent):
❑ In acute MR
❑ In chronic MR
Order chest X-ray (urgent): ❑ Acute MR
Order transthoracic echocardiography (TTE) (urgent): ❑ Confirmatory Order lab tests: ❑ CBC Other tests ❑ Transesophageal echocardiography (TEE if TTE is equivocal)
❑ Exercise testing
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Cardinal findings that are suggestive of acute mitral regurgitation ❑ Sudden onset and rapid progression of pulmonary edema
| Cardinal findings that are suggestive of chronic mitral regurgitation ❑ Asymptomatic to chronic symptoms
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mitral valve anatomy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Normal | Abnormal | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chronic primary mitral regurgitation | Chronic secondary mitral regurgitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Treatment of Acute Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.[1][2].
LVEF: Left ventricular ejection fraction; MR: Mitral regurgitation; IE: Infective endocarditis
| Acute mitral regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Assess if the patient is hemodynamically stable? ❑ Hemodynamic instability | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Unstable | Stable | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initial resusticative measures: ❑ Secure airway Initiate medical therapy: ❑ Vasodilator therapy AND Consider the following: ❑ Pulmonary artery catheterization | Initial resusticative measures: ❑ O2 Initiate medical therapy: ❑ Vasodilator therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ischemic mitral regurgitation | Non-ischemic mitral regurgitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| MR due to cardiomyopathy (functional MR) | MR due to IE (organic MR) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Intra-aortic balloon pump Initiate medical therapy: ❑ In cases of reduced LVEF Reperfusion or revascularization Mitral valve surgery: ❑ Papillary muscle rupture
Cardiac transplantation: ❑ On some occasions with no contraindication for surgery | Heart failure management: ❑ Click here for acute heart failure resident survival guide
Mitral valve surgery: ❑ When there is no response to medical management ❑ Mitral valve replacement or mitral valve repair | Mitral valve surgery:
Initiate medical therapy: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment of Chronic Mitral Regurgitation
Chronic Primary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic primary mitral regurgitation.[2].
AF: Atrial fibrillation; IE: Infective endocarditis; LVEF: Left ventricular ejection fraction; LVESD: Left ventricular end systolic dimension; MR: Mitral regurgitation; MVP: Mitral valve proplapse; PASP: Pulmonary artery systolic pressure; RHD: Rheumatic heart disease;
| Chronic primary mitral regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Etiologies:
❑ Left ventricular dilation | Progressive MR (Stage B): ❑ Etiologies: ❑ No Left ventricular dilation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Symptomatic (Stage D) | Asymptomatic (Stage C) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate medical therapy:
❑ Beta blocker Mitral valve surgery:
Revascularisation: ❑ Concurrent coronary artery disease Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Mitral valve surgery: ❑ Performed in the following patients:
Revascularization: ❑ Concurrent coronary artery disease Periodic monitoring: ❑ In stage C1 patients with the following:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Periodic monitoring: ❑ Clinical evaluation:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: ❑ Initiate infective endocarditis antimicrobial treatment in case of valve involvement | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Chronic Secondary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic secondary mitral regurgitation.[2].
AF: Atrial fibrillation; CAD: Coronary artery disease; HF: Heart failure; IE: Infective endocarditis; LV: Left ventricle; MR: Mitral regurgitation
| Chronic secondary mitral regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Heart failure treatment: ❑ Click here for heart failure resident survival guide
| CAD treatment: ❑ Click here for coronary artery disease medical therapy ❑ Coronary angiography | Cardiac resynchronization therapy: ❑ Cardiac resynchronization therapy with biventricular pacing:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Echo findings:
❑ LV dilation and systolic dysfunction due to primary myocardial disease | Progressive MR (Stage B): ❑ Echo findings:
❑ LV dilation and systolic dysfunction due to primary myocardial disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Stage D: Symptomatic (HF symptoms due to MR persist even after revascularization and medical therapy) | Stage C: Asymptomatic (HF and coronary ischemia symptoms respond to revascularization and medical herapy) | HF and coronary ischemia symptoms respond to revascularization and medical herapy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Mitral valve surgery:
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: | Periodic monitoring: ❑ Clinical evaluation:
Mitral valve surgery: ❑ Only in patients undergoing other cardiac surgery
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: ❑ Initiate infective endocarditis antimicrobial treatment for patients undergoing mitral valve surgery | Periodic monitoring: ❑ Clinical evaluation:
Mitral valve surgery: ❑ Only in patients undergoing other cardiac surgery
Anticoagulation therapy: ❑ Warfarin:
❑ Aspirin:
Endocarditis prophylaxis: ❑ Initiate infective endocarditis antimicrobial treatment for patients undergoing mitral valve surgery | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Diagnosis
Symptoms
- Acute mitral regurgitation causes the following symptoms:
- Chronic mitral regurgitation may have a prolonged asymptomatic interval phase until the heart decompensates and the symptoms of low cardiac output and pulmonary congestion start. By the time the symptoms develop, left ventricular dysfunction may have already occurred.
Physical Examination
- S3 and S4 may be heard on auscultation.
- A holosystolic murmur is heard in the apical region of the heart. MR murmur radiates to the axillary region. It may be soft, short and even absent. 70% of the cases of papillary muscle rupture have no murmur.
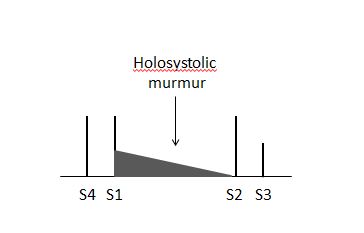 |
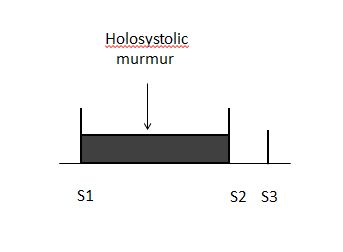 |
Imaging
Transthoracic echocardiography
Echocardiographic findings indicating the presence of severe mitral regurgitation include:
- Regurgitant volume >60 ml
- Regurgitant fraction >55%
- Effective regurgitant orifice (ERO) (ratio of regurgitant flow volume to the velocity of the mitral insufficiency jet: ERO = Flow / Velocity) >0.4 cm2
- If the left ventricular and left atrial sizes are normal on echocardiography, mitral regurgitation is not severe.
- Central jets indicate the presence of a fairly normal mitral valve and therefore the mitral regurgitation is not severe.
- Wide eccentric jets indicate that the regurgitation is severe.
- Echocardiographic findings must match the symptoms, if they do not, perform transesophageal echocardiography (TEE) or cardiac catheterization. TTE can underestimate the magnitude of mitral regurgitation in patients with clinical signs of severe MR.
Treatment
Acute Severe Mitral Regurgitation
- Treatment of acute severe mitral regurgitation depends on the stability of the patient.If the patient is clinically stable, the treatment options are:
- IV vasodilators, diuretics, antibiotics, anti-ischemic agents
- Surgery is preferred in the following cases:
- Endocarditis with progressive congestive heart failure
- No response to antibiotics
- Abscess formation
- Recurrent embolization
- If the patient is clinically unstable , the treatment options are:
- IV nitroprusside is used to maintain blood pressure. Inotropes are added when needed.
- If medical therapy is not effective, an intra aortic balloon pump can be inserted to maintain hemodynamic stability.
- Surgical treatment is usually indicated.
- Knowledge of the etiology of the mitral regurgitation is important to know if the valve can be repaired or replaced.
Chronic Mitral Regurgitation
Why the Mitral valve is replaced Before Symptoms in Patients with Chronic Mitral Regurgitation
- Mitral regurgitation is a syndrome of pure volume overload whereas aortic regurgitation is a combination of both volume and pressure overload.
- Both syndromes are associated with an increase in preload.
- in mitral regurgitation, the afterload is reduced whereas in aortic regurgitation the afterload is increased. This is very important because when the mitral valve is repaired, there is no longer a reduction afterload and the left ventricle may fail due to an abrupt rise in the afterload. In aortic regurgitation, because the afterload is already increased chronically, replacement of the valve is not as likely to precipitate acute left ventricular failure due to an abrupt rise in afterload.
- By the time symptoms develop, there is already left ventricular dysfunction.
- Because of the low pressure system into which the blood is ejected into through the mitral valve, the ejection fraction is always high in mitral regurgitation. If the ejection fraction appears to be "normal", there is already decline in left ventricular function.
- There is no indication for vasodilator therapy in the absence of systemic hypertension in asymptomatic patients with preserved left ventricular function.
Indications for Surgery in Chronic Mitral Regurgitation
The indications for surgery in chronic mitral regurgitation are:
- Any symptoms - this is unlike mitral stenosis where surgeons operate on the heart when patients have class III or IV symptoms.
- Severe organic MR.
- Left ventricular dysfunction - ejection fraction <60% and end systolic diameter >40 mm2.
- Surgery can be considered in asymptomatic patients in the following cases:
- Truly severe MR
- Low operative mortality
- High chance of successful repair (e.g: posterior leaflet - MVP)
- Pre-operative ejection fraction has a prognostic impact in patients who undergo mitral valve repair or replacement. The lower the ejection fraction is, the higher the mortality is.
Do's
Don'ts
- Don't perform coronary angiography before valve surgery in patients who are hemodynamically unstable.
- Avoid coronary angiography in patients of acute coronary syndrome complicated by severe acute mitral regurgitation.
References
- ↑ 1.0 1.1 Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Grenadier E, Alpan G, Keidar S, Palant A (1983). "The prevalence of ruptured chordae tendineae in the mitral valve prolapse syndrome". Am Heart J. 105 (4): 603–10. PMID 6837414.
- ↑ Grinberg AR, Finkielman JD, Piñeiro D, Festa H, Cazenave C (1998). "Rupture of mitral chorda tendinea following blunt chest trauma". Clin Cardiol. 21 (4): 300–1. PMID 9580528.
- ↑ Anderson Y, Wilson N, Nicholson R, Finucane K (2008). "Fulminant mitral regurgitation due to ruptured chordae tendinae in acute rheumatic fever". J Paediatr Child Health. 44 (3): 134–7. doi:10.1111/j.1440-1754.2007.01214.x. PMID 17854408.
- ↑ Otto CM (2001). "Clinical practice. Evaluation and management of chronic mitral regurgitation". N Engl J Med. 345 (10): 740–6. doi:10.1056/NEJMcp003331. PMID 11547744.