Pulmonary embolism surgery
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism surgery On the Web |
|
Risk calculators and risk factors for Pulmonary embolism surgery |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients.[1]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
Embolectomy
Embolectomy is the process of removing an embolus surgically or with a catheter. The procedure should be used when a high risk patient presents with persistent hypotension and thrombolysis has either failed or is contraindicated.
To read more about embolectomy (types, procedure), click here.
ACC/AHA 2011 Guidelines- Recommendations for Catheter Embolectomy and Fragmentation (DO NOT EDIT)
| Class III (No Benefit) |
| "1.Catheter embolectomy and surgical thrombectomy are not recommended for patients with low-risk PE or submassive acute PE with minor RV dysfunction, minor myocardial necrosis, and no clinical worsening (Level of Evidence: C)" |
| Class IIa |
| "1. Depending on local expertise, either catheter embolectomy and fragmentation or surgical embolectomy is reasonable for patients with massive PE and contraindications to fibrinolysis(Level of Evidence: C). " |
|
"2. Catheter embolectomy and fragmentation or surgical embolectomy is reasonable for patients with massive PE who remain unstable after receiving fibrinolysis (Level of Evidence: C)." |
|
"3. For patients with massive PE who cannot receive fibrinolysis or who remain unstable after fibrinolysis, it is reasonable to consider transfer to an institution experienced in either catheter embolectomy or surgical embolectomy if these procedures are not available locally and safe transfer can be achieved (Level of Evidence: C)." |
| Class IIb |
| "1. Either catheter embolectomy or surgical embolectomy may be considered for patients with submassive acute PE judged to have clinical evidence of adverse prognosis (new hemodynamic instability, worsening respiratory failure, severe RV dysfunction, or major myocardial necrosis) (Level of Evidence: C)." |
ACC/AHA 2011 Guidelines-Recommendations for Endovascular Thrombolysis and Surgical Venous Thrombectomy (DO NOT EDIT)
| Class I |
| "1. CDT or PCDT should be given to patients with IFDVT associated with limb-threatening circulatory compromise (ie, phlegmasia cerulea dolens) (Level of Evidence: C)." |
| "2. Patients with IFDVT at centers that lack endovascular thrombolysis should be considered for transfer to a center with this expertise if indications for endovascular thrombolysis are present (Level of Evidence: C)." |
| Class III (No Benefit) |
| "1. Systemic fibrinolysis should not be given routinely to patients with IFDVT (Level of Evidence: A)." |
| "2. CDT or PCDT should not be given to most patients with chronic DVT symptoms (>21 days) or patients who are at high risk for bleeding complications (Level of Evidence: B)." |
| Class IIa |
| "1. CDT or PCDT is reasonable for patients with IFDVT associated with rapid thrombus extension despite anticoagulation (Level of Evidence: C) and/or symptomatic deterioration from the IFDVT despite anticoagulation (Level of Evidence: B)." |
| "2. CDT or PCDT is reasonable as first-line treatment of patients with acute IFDVT to prevent PTS in selected patients at low risk of bleeding complications (Level of Evidence: B)." |
| Class IIb |
| "1. Surgical venous thrombectomy by experienced surgeons may be considered in patients with IFDVT (Level of Evidence: B)." |
Inferior vena cava filter
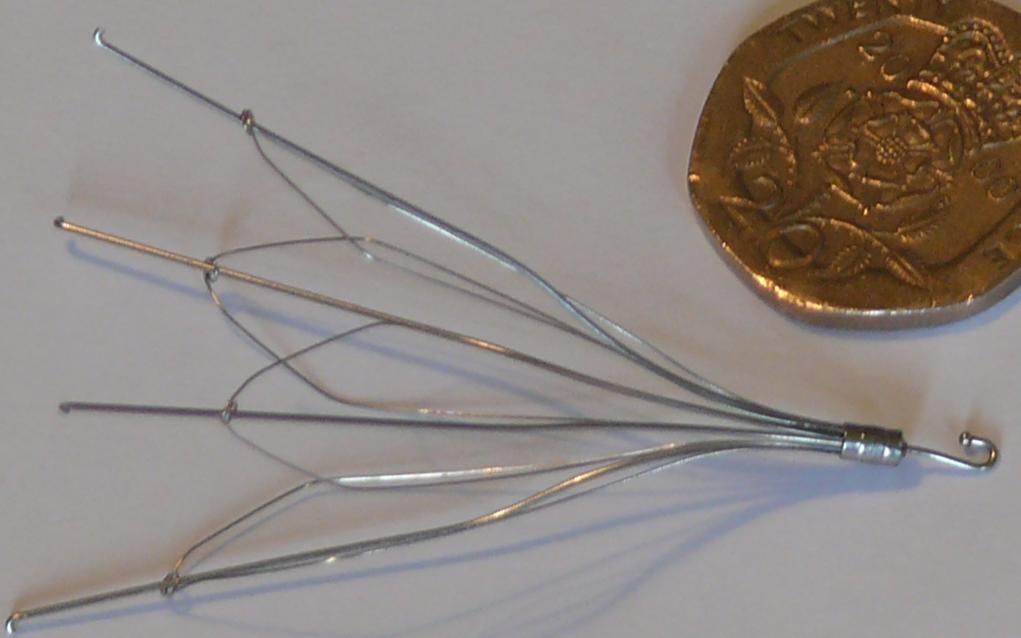
An inferior vena cava filter] is a medical device that is implanted into the inferior vena cava to prevent pulmonary emboli (PEs).
IVC filters are used in the following cases:
- Anticoagulation is contraindicated
- Failure of anticoagulation
- Anticoagulation complication in patients who have a venous thromboembolism disease.
- Prophylactic measures for patients with a high risk of pulmonary embolism.
If anticoagulant therapy is contraindicated and/or ineffective, an inferior vena cava filter should be implanted[3]. It provides a filter in the inferior vena cava, allowing blood to pass through, while preventing large emboli from traveling from the lower extremities to the lung. IVC filters decreases PE recurrence but are not efficacious in preventing mortality[4].
In a study group comprising of 400 patients with proximal deep-vein thrombosis, which were followed for 2 years, it was found that the initial beneficial effect of vena caval filters for the prevention of pulmonary embolism was counterbalanced by an excess of recurrent deep-vein thrombosis, without any difference in mortality[3].
ACC/AHA 2011 Guidelines- Recommendations on IVC Filters in the Setting of Acute PE (DO NOT EDIT)
| Class I |
| "1. Adult patients with any confirmed acute PE (or proximal DVT) with contraindications to anticoagulation or with active bleeding complication should receive an IVC filter. (Level of Evidence: C) " |
| "2. Anticoagulation should be resumed in patients with an IVC filter once contraindications to anticoagulation or active bleeding complications have resolved. (Level of Evidence: B) " |
| "3. Patients who receive retrievable IVC filters should be evaluated periodically for filter retrieval within the specific filter's retrieval window. (Level of Evidence: C)" |
| Class III (No Benefit) |
| "1. An IVC filter should not be used routinely as an adjuvant to anticoagulation and systemic fibrinolysis in the treatment of acute PE. (Level of Evidence: C). " |
| Class IIa |
| "1. For patients with recurrent acute PE despite therapeutic anticoagulation, it is reasonable to place an IVC filter (Level of Evidence: C)" |
| "2. For DVT or PE patients who will require permanent IVC filtration (eg, those with a long-term contraindication to anticoagulation), it is reasonable to select a permanent IVC filter device. (Level of Evidence: C)." |
| "3. For DVT or PE patients with a time-limited indication for an IVC filter (eg, those with a short-term contraindication to anticoagulation therapy), it is reasonable to select a retrievable IVC filter device. (Level of Evidence: C)." |
| Class IIb |
| "1. Placement of an IVC filter may be considered for patients with acute PE and very poor cardiopulmonary reserve, including those with massive PE. (Level of Evidence: C)." |
ACC/AHA 2011 Guidelines- Recommendations for Use of IVC Filters in Patients With Iliofemoral DVT (DO NOT EDIT)
| Class I |
| "1. Adult patients with any acute proximal DVT (or acute PE) with contraindications to anticoagulation or active bleeding complication should receive an IVC filter (Level of Evidence: B). " |
| "2. Anticoagulation should be resumed in patients with an IVC filter once contraindications to anticoagulation or active bleeding complications have resolved (Level of Evidence: B)." |
| "3. Patients who receive retrievable IVC filters should be evaluated periodically for filter retrieval within the specific filter's retrieval window (Level of Evidence: C)." |
| Class III (No Benefit) |
| "1. An IVC filter should not be used routinely in the treatment of iliofemoral DVT (Level of Evidence: B)." |
| Class IIa |
| "1. For patients with recurrent PE despite therapeutic anticoagulation, it is reasonable to place an IVC filter (Level of Evidence: C)." |
| "2. For iliofemoral DVT patients who are likely to require permanent IVC filtration (eg, long-term contraindication to anticoagulation), it is reasonable to select a permanent nonretrievable IVC filter device (Level of Evidence: C)." |
| "3. For iliofemoral DVT patients with a time-limited indication for an IVC filter (eg, a short-term contraindication to anticoagulant therapy), placement of a retrievable IVC filter is reasonable (Level of Evidence: C)." |
| Class IIb |
| "1. For patients with recurrent DVT (without PE) despite therapeutic anticoagulation, it is reasonable to place an IVC filter(Level of Evidence: C)." |
ESC 2008 Guidelines - Recommendations for Use of IVC Filters (DO NOT EDIT)
| Class III |
| "1.The routine use of IVC filters in patients with PE is not recommended.(Level of Evidence: B)" |
| Class IIb |
| "1.IVC filters may be used when there are absolute contraindications to anticoagulation and a high risk of VTE recurrence.(Level of Evidence: B)" |
Angioplasty
Angioplasty is the mechanical widening of a narrowed or totally obstructed blood vessel. These obstructions are often caused by atherosclerosis. The term angioplasty is a portmanteau of the words angio (from the Latin/Greek word meaning "vessel") and plasticos (Greek: "fit for moulding"). Angioplasty has come to include all manner of vascular interventions typically performed in a minimally invasive or percutaneous method.
ACC/AHA 2011 Guidelines- Recommendations for Percutaneous Transluminal Venous Angioplasty and Stenting (DO NOT EDIT)
| Class IIa |
| "1. Stent placement in the iliac vein to treat obstructive lesions after CDT, PCDT, or surgical venous thrombectomy is reasonable (Level of Evidence: C)." |
| "2. For isolated obstructive lesions in the common femoral vein, a trial of percutaneous transluminal angioplasty without stenting is reasonable (Level of Evidence: C)." |
| "3. The placement of iliac vein stents to reduce PTS symptoms and heal venous ulcers in patients with advanced PTS and iliac vein obstruction is reasonable (Level of Evidence: C)" |
| "4. After venous stent placement, the use of therapeutic anticoagulation with similar dosing, monitoring, and duration as for IFDVT patients without stents is reasonable (Level of Evidence: C)" |
| Class IIb |
| "1. After venous stent placement, the use of antiplatelet therapy with concomitant anticoagulation in patients perceived to be at high risk of rethrombosis may be considered (Level of Evidence: C) " |
Guidelines Resources
- Guidelines on the management of Pulmonary embolism: Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension[2]
- Guidelines on the management of Pulmonary embolism: Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension[2]
- Guidelines on the diagnosis and management of acute pulmonary embolism[5].
- Guidelines on the management of Pulmonary embolism: Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension[2]
- Guidelines on the management of Pulmonary embolism: Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension[2]
References
- ↑ Augustinos P, Ouriel K (2004). "Invasive approaches to treatment of venous thromboembolism". Circulation. 110 (9 Suppl 1): I27–34. PMID 15339878.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ; et al. (2011). "Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association". Circulation. 123 (16): 1788–830. doi:10.1161/CIR.0b013e318214914f. PMID 21422387.
- ↑ 3.0 3.1 Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral F, Huet Y, Simonneau G (1998). "A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group". N Engl J Med. 338 (7): 409–15. PMID 9459643.
- ↑ "Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study". Circulation. 112 (3): 416–22. 2005. doi:10.1161/CIRCULATIONAHA.104.512834. PMID 16009794. Retrieved 2011-12-13. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP (2008). "Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". Eur. Heart J. 29 (18): 2276–315. doi:10.1093/eurheartj/ehn310. PMID 18757870. Retrieved 2011-12-07. Unknown parameter
|month=ignored (help)