Hypopituitarism pathophysiology
|
Hypopituitarism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hypopituitarism pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hypopituitarism pathophysiology |
|
Risk calculators and risk factors for Hypopituitarism pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Elsaiey, MBBCH [2], Iqra Qamar M.D.[3]
Overview
Hypopituitarism is believed to be caused mainly due to ischemia of the pituitary gland. This ischemia can be due to hemorrhage, tumors, or brain injury. Compression of the blood vessels is one of the mechanisms that cause ischemia to the pituitary gland and leads to hypopituitarism. Pituitary adenomas cause compression to the hypophyseal vessels leading to interruption in the pituitary gland function. Traumatic brain injury either primary or secondary also leads to pituitary gland dysfunction.
Pathophysiology
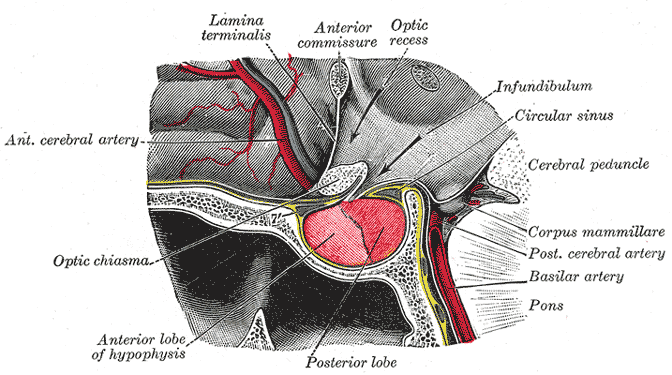
Background on pituitary gland blood supply
- In order to understand the pathophysiology of hypopituitarism, it is necessary to know the blood supply of the pituitary gland as hypopituitarism occurs mainly by ischemia through different mechanisms like hemorrhage, tumors or brain injury.[1][2]
- The pituitary gland is composed of two parts anterior (adenohypophysis) and posterior (neurohypophysis). Both parts are supplied by the carotid arteries.
- Adenohypophysis: It receives blood supply from the long and short hypophyseal arteries which arise from the internal carotid artery and the anterior of the circle of Willis.
- Neurohypophysis: It receives the blood supply from the inferior and middle hypophyseal arteries.
Pathogenesis
- Hypopituitarism pathogenesis is mainly due to the destruction of the pituitary gland cells by different ways like ischemia, inflammation or infiltration. However, ischemia is believed to be the cornerstone of hypopituitarism pathogenesis caused via different ways.[3][4]
- Compression of the blood vessels:[5]
- Pituitary adenoma, secretory or nonsecretory, is one of the common causes that lead to loss of the pituitary dysfunction by compression on the hypophyseal vessels resulting in ischemia.
- Large adenomas (more than 1.5 cm) cause loss of function more than microadenomas. They cause compression on the pituitary stalk and the hypophyseal portal vessels which supply the pituitary gland with blood.
- The tumor growth in the pituitary gland participates in increasing the intrasellar pressure which causes a decrease in the hypophyseal blood flow which ends up by a decrease of hormonal delivery from the hypothalamus to the pituitary gland.
- Other lesions lead to compression includes carotid artery aneurysm, meningioma, and craniopharyngioma.
- Traumatic brain injury (TBI):
- Hypopituitarism occurs either by the following factors:
- Primary brain injury
- Brain injury due to other secondary events like hypotension or hypoxia
- Medication effects
- Critical illness
- The anatomical sitting of the pituitary gland increases its susceptibility to getting injured from trauma.
- It is believed that tissue necrosis results in the release of sequestered antigens, precipitating autoimmunity of the Pituitary gland and hypopituitarism in Sheehan's syndrome.[6][7][8]
- Hypopituitarism occurs either by the following factors:
References
- ↑ Dusick JR, Wang C, Cohan P, Swerdloff R, Kelly DF (2012). "Pathophysiology of hypopituitarism in the setting of brain injury". Pituitary. 15 (1): 2–9. doi:10.1007/s11102-008-0130-6. PMC 4170072. PMID 18481181.
- ↑ Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E (2007). "Hypopituitarism". Lancet. 369 (9571): 1461–70. doi:10.1016/S0140-6736(07)60673-4. PMID 17467517.
- ↑ Arafah BM (2002). "Medical management of hypopituitarism in patients with pituitary adenomas". Pituitary. 5 (2): 109–17. PMID 12675508.
- ↑ Vance, Mary Lee (1994). "Hypopituitarism". New England Journal of Medicine. 330 (23): 1651–1662. doi:10.1056/NEJM199406093302306. ISSN 0028-4793.
- ↑ Arafah BM, Prunty D, Ybarra J, Hlavin ML, Selman WR (2000). "The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas". J Clin Endocrinol Metab. 85 (5): 1789–93. doi:10.1210/jcem.85.5.6611. PMID 10843153.
- ↑ Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N (2002). "Pituitary autoimmunity in patients with Sheehan's syndrome". J. Clin. Endocrinol. Metab. 87 (9): 4137–41. doi:10.1210/jc.2001-020242. PMID 12213861.
- ↑ "AUTOANTIBODIES IN SHEEHAN'S SYNDROME - ScienceDirect".
- ↑ Falorni A, Minarelli V, Bartoloni E, Alunno A, Gerli R (2014). "Diagnosis and classification of autoimmune hypophysitis". Autoimmun Rev. 13 (4–5): 412–6. doi:10.1016/j.autrev.2014.01.021. PMID 24434361.