Reperfusion injury medical therapy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 69: | Line 69: | ||
# [[Beta-blockade]] | # [[Beta-blockade]] | ||
# GIK (glucose-insulin-potassium infusion) (Studied in the [[Glucose]]-[[Insulin]]-[[Potassium]] Infusion in Patients With [[Acute Myocardial Infarction]] Without Signs of [[Heart Failure]]: The Glucose-Insulin-Potassium Study (GIPS)-II and other older studies | # GIK ([[glucose-insulin-potassium infusion]]) (Studied in the [[Glucose]]-[[Insulin]]-[[Potassium]] Infusion in Patients With [[Acute myocardial infarction|Acute Myocardial Infarction]] Without Signs of [[Heart Failure]]: The Glucose-Insulin-Potassium Study (GIPS)-II and other older studies | ||
# [[Sodium]]-[[hydrogen]] exchange inhibitors such as [[cariporide]] (Studied in the GUARDIAN and EXPEDITION trials) | # [[Sodium]]-[[hydrogen]] exchange inhibitors such as [[cariporide]] (Studied in the GUARDIAN and EXPEDITION trials) | ||
# [[Adenosine]] (Studied in the AMISTAD I and AMISTAD II trials as well as the ATTACC trial ). It should be noted that at high doses in anterior [[ST elevation myocardial infarction]]|[[ST elevation MI]] adenosine was effective in the AMISTAD trial. Likewise, [[intracoronary]] administration of [[adenosine]] prior to [[primary PCI]] has been associated with improved [[echocardiographic]] and clinical outcomes in one small study. | # [[Adenosine]] (Studied in the AMISTAD I and AMISTAD II trials as well as the ATTACC trial ). It should be noted that at high doses in anterior [[ST elevation myocardial infarction]]|[[ST elevation MI]] adenosine was effective in the AMISTAD trial. Likewise, [[Intracoronary route|intracoronary]] administration of [[adenosine]] prior to [[primary PCI]] has been associated with improved [[echocardiographic]] and clinical outcomes in one small study. | ||
#[[Calcium-channel blockers]] | #[[Calcium-channel blockers]] | ||
#[[Potassium–adenosine triphosphate channel]] openers | #[[Potassium–adenosine triphosphate channel]] openers | ||
| Line 78: | Line 78: | ||
#[[Pexelizumab]], a humanized [[monoclonal antibody]] that binds the C5 component of complement (Studied in the [[Pexelizumab]] for [[ST elevation myocardial infarction]]|[[Acute ST-Elevation Myocardial Infarction]] in Patients Undergoing Primary [[Percutaneous Coronary Intervention]] (APEX AMI) trial ) | #[[Pexelizumab]], a humanized [[monoclonal antibody]] that binds the C5 component of complement (Studied in the [[Pexelizumab]] for [[ST elevation myocardial infarction]]|[[Acute ST-Elevation Myocardial Infarction]] in Patients Undergoing Primary [[Percutaneous Coronary Intervention]] (APEX AMI) trial ) | ||
# KAI-9803, a [[delta-protein kinase C inhibitor]](Studied in the Intracoronary KAI-9803 as an adjunct to [[primary percutaneous coronary intervention]] for [[ST elevation myocardial infarction|acute ST-segment elevation myocardial infarction]] trial or DELTA AMI trial). | # KAI-9803, a [[delta-protein kinase C inhibitor]](Studied in the Intracoronary KAI-9803 as an adjunct to [[primary percutaneous coronary intervention]] for [[ST elevation myocardial infarction|acute ST-segment elevation myocardial infarction]] trial or DELTA AMI trial). | ||
#[[Atrial natriuretic peptide|Human atrial natriuretic peptide]] (Studied in the Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for [[acute myocardial infarction]] (J-WIND): two randomized trials.) | #[[Atrial natriuretic peptide|Human atrial natriuretic peptide]] (Studied in the [[Atrial natriuretic peptide|Human atrial natriuretic peptide]] and [[nicorandil]] as adjuncts to reperfusion treatment for [[acute myocardial infarction]] (J-WIND): two randomized trials.) | ||
# FX06, an [[anti-inflammatory]] fibrin derivative that competes with | # FX06, an [[anti-inflammatory]] fibrin derivative that competes with f[[Fibrin|ibrin fragment]]<nowiki/>s for binding with the vascular endothelial molecule [[VE-cadherin]] which deters migration of [[leukocytes]] across the endothelial cell monolayer (studied in the F.I.R.E. trial (Efficacy of FX06 in the Prevention of Myocardial Reperfusion Injury) | ||
# [[Magnesium]], which was evaluated by the Fourth International Study of Infarct Survival (ISIS-4) and the MAGIC trial. | # [[Magnesium]], which was evaluated by the Fourth International Study of Infarct Survival (ISIS-4) and the MAGIC trial. | ||
# Hyperoxemia, the delivery of supersaturated [[oxygen]] after [[Percutaneous coronary intervention|PCI]] (Studied in the AMIHOT II trial). | # Hyperoxemia, the delivery of supersaturated [[oxygen]] after [[Percutaneous coronary intervention|PCI]] (Studied in the AMIHOT II trial). | ||
Revision as of 17:55, 22 August 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2] Associate Editor(s)-in-Chief: Anjan K. Chakrabarti, M.D. [3] Shivam Singla, M.D.[4]
Overview
The most common myth about the ischemia-reperfusion injury is itself related to blood flow. One can easily think like if everything is happening due to ischemia and with the restoration of blood flow, the injury should heal. Here is the trick, reperfusion in turn further exacerbates the injury mainly due to the formation of free radicals. There are few approaches that are studied widely and do play a major role in controlling the injury related to ischemia-reperfusion injury
- Prevent generation of free radicals( Oxidative stress) or Increase the tissue's capacity to trap the free radicals
- Controlling the neutrophil activation and infiltration of ischemic tissue
- Hypoxic pre-conditioning
Hyperbaric oxygen therapy is also studied widely and best suited when used within 6 hrs of hypoxia as it helps in the reduction of local and systemic hypoxia and in turn increases the survival of affected tissue.
Medical Therapy
Various proposed medical managements studied are:
- Therapeutic hypothermia
- It has been shown in rats that neurons sometimes die completely 24 hours after the blood flow returns.
- This delayed reaction is the result of the multiple inflammatory immune responses that occur during reperfusion.
- Such inflammatory reactions cause increase inntracranial pressure, a pressure that leads to cell damage and cell death in some cases.
- Hypothermia has been shown to help reduce intracranial pressure and thus decrease the adverse effects of inflammatory immune responses during reperfusion.
- Besides that, reperfusion also increases free radical development. Hypothermia has also been shown to decrease the patient's development of deadly free radicals during reperfusion.
- Hydrogen sulfide treatment
- There are several preliminary studies in mice that seem to show that treatment with hydrogen sulfide ( H2S) could have a protective effect against reperfusion injury
- Cyclosporine
- In addition to its well-known immunosuppressive capabilities, the one-time administration of cyclosporine at the time of percutaneous coronary intervention (PCI) has been found to deliver a 40 percent reduction in infarct size in a small group proof of concept study of human patients with reperfusion injury published in The New England Journal of Medicine in 2008.
- Cyclosporine works by inhibiting the action of Cyclophilin D which usually helps in opening Mitochondrial membrane transport protein ( MPT Pore). So once cyclophilin D action is inhibited, there is no more MPT pore opening and in turn, saves the mitochondria from getting damaged.
- The opening of MTP Pore results in major cell destruction by causing the influx of water into mitochondria, impairing its function and ultimately leading to the collapse. The strategy to protect mitochondria is the most important thing associated with the treatment part.
- TRO40303
- Stem cell therapy
- Recent investigations suggest a possible beneficial effect of mesenchymal stem cells on heart and kidney reperfusion injury
- Superoxide dismutase
- Superoxide dismutase is an important antioxidant enzyme that transforms superoxide anions into water and hydrogen peroxide. Recent work has demonstrated important therapeutic effects on pre-clinical models of reperfusion damage following an ischemic stroke
- Metformin
- Some studies proved the role of metformin in preventing Ischemia-Reperfusion injury by inhibiting the opening of MPT Pore and Mitochondrial complex inhibition. Although the studies are done in rats only still the correlation can be derived clinically for humans as well.
- Cannabinoids
- A synthetic analog of cannabis helps to prevent hepatic ischemia and injury by reducing the inflammation and oxidative stress occurring through CB2 receptors. This in turn lowers the tissue damage and provides protective effects. The various synthetic analogs of phytocannabinoid that play major role are:
- THCV- Tetrahydrocannabivarin
- 8-Tetrahydrocannabivarin
- 11-OH-8-THCV
Therapies Associated with Improved Clinical Outcomes
Therapies that have been associated with improved clinical outcomes include:
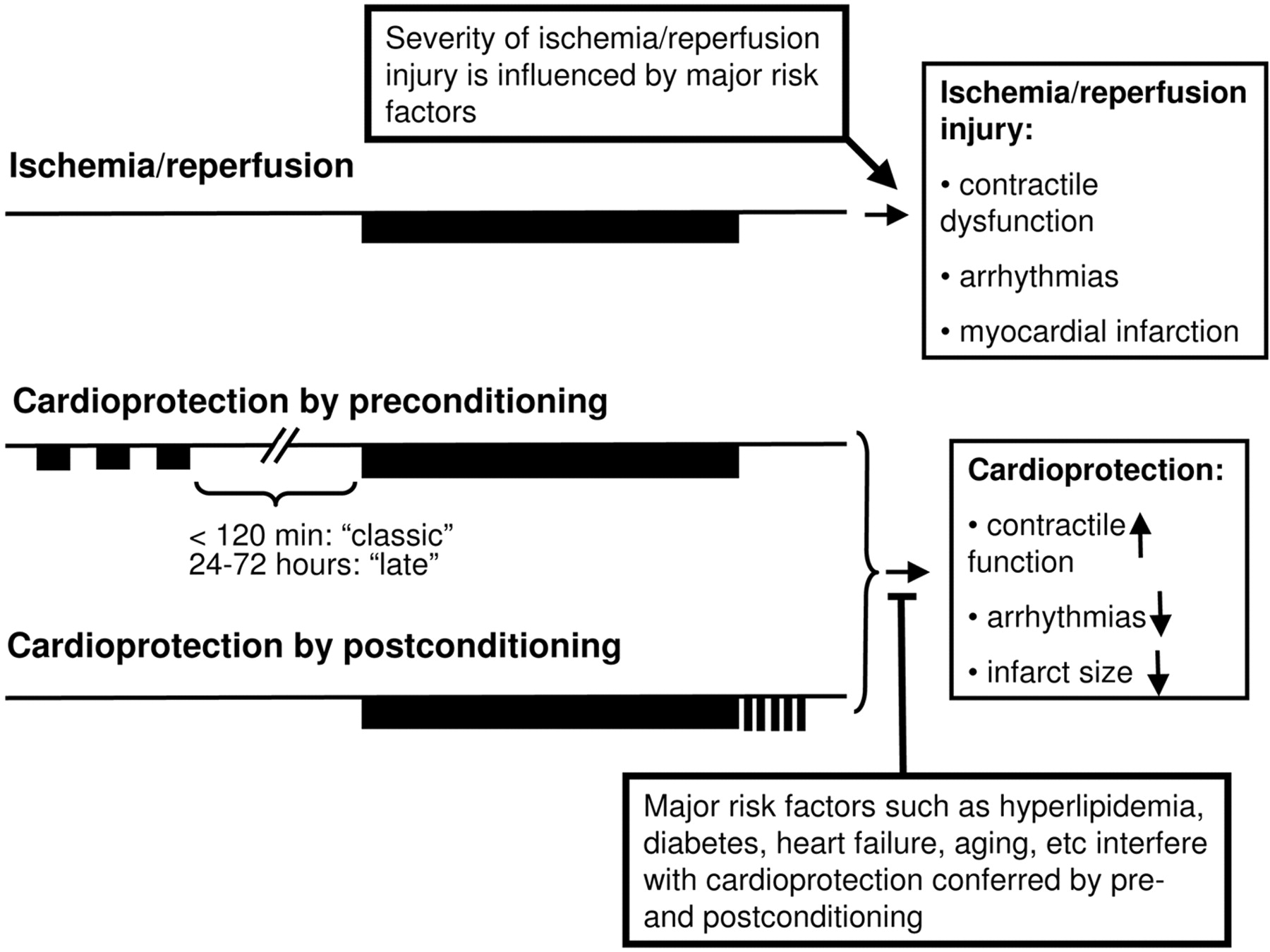
- "Preconditioning" - Preconditioning is basically an adaptive response in which ischemia is exposed for a brief period of time before the actual ischemia phase to the tissue. This phenomenon markedly increases the ability of the heart to withstand subsequent ischemic insults. In addition to that, the application of brief episodes of ischemia at the onset of reperfusion is termed as "postconditioning" which reduces the extent of injury that is supposed to happen.
- "Postconditioning" (short repeated periods of vessel opening by repeatedly blowing the balloon up for short periods of time).
- Mechanisms of protection include formation and release of several autacoids and cytokines, maintained acidosis during early repercussion, activation of protein kinases, and attenuation of the opening of the mitochondrial permeability transition pore (MPTP)
- One study in humans demonstrated an area under the curve (AUC) of creatine kinase (C) release over the first 3 days of reperfusion (as a surrogate for infarct size) was significantly reduced by 36% in the post conditioned versus a control group
- Infarct size reduction by PCI postconditioning persisted 6 months after AMI and resulted in a significant improvement in left ventricular (LV) function at 1 year
- Inhibition of mitochondrial pore opening by cyclosporine.
- Specifically, the study by Piot et al demonstrated that administration of cyclosporine at the time of reperfusion was associated with a reduction in infarct size
- Infarct size was measured by the release of creatine kinase and delayed hyperenhancement on MRI
- Patients with cardiac arrest, ventricular fibrillation, cardiogenic shock, stent thrombosis, previous acute myocardial infarction, or angina within 48 hours before infarction were not included in the study #*Occlusion of the culprit artery (TIMI flow 0) was part of the inclusion criteria.
Limitations to applying strategies that have demonstrated benefit in animal models are the fact that reperfusion therapy was administered prior to or at the time of reperfusion. In the management of STEMI patients, it is impossible to administer the agent before vessel occlusion (except during coronary artery bypass grafting). Given the time constraints and the goal of opening an occluded artery within 90 minutes, it is also difficult to administer experimental agents before reperfusion in STEMI.
Therapies Associated with Limited Success
Pharmacotherapies that have either failed or that have met with limited success in improving clinical outcomes include:
- Beta-blockade
- GIK (glucose-insulin-potassium infusion) (Studied in the Glucose-Insulin-Potassium Infusion in Patients With Acute Myocardial Infarction Without Signs of Heart Failure: The Glucose-Insulin-Potassium Study (GIPS)-II and other older studies
- Sodium-hydrogen exchange inhibitors such as cariporide (Studied in the GUARDIAN and EXPEDITION trials)
- Adenosine (Studied in the AMISTAD I and AMISTAD II trials as well as the ATTACC trial ). It should be noted that at high doses in anterior ST elevation myocardial infarction|ST elevation MI adenosine was effective in the AMISTAD trial. Likewise, intracoronary administration of adenosine prior to primary PCI has been associated with improved echocardiographic and clinical outcomes in one small study.
- Calcium-channel blockers
- Potassium–adenosine triphosphate channel openers
- Antibodies directed against leukocyte adhesion molecules such as CD 18 (Studied in the LIMIT AMI trial )
- Oxygen free radical scavengers/anti-oxidants, including Erythropoietin, estrogen, heme-oxygenase 1, and hypoxia induced factor-1 (HIF-1).
- Pexelizumab, a humanized monoclonal antibody that binds the C5 component of complement (Studied in the Pexelizumab for ST elevation myocardial infarction|Acute ST-Elevation Myocardial Infarction in Patients Undergoing Primary Percutaneous Coronary Intervention (APEX AMI) trial )
- KAI-9803, a delta-protein kinase C inhibitor(Studied in the Intracoronary KAI-9803 as an adjunct to primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction trial or DELTA AMI trial).
- Human atrial natriuretic peptide (Studied in the Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (J-WIND): two randomized trials.)
- FX06, an anti-inflammatory fibrin derivative that competes with fibrin fragments for binding with the vascular endothelial molecule VE-cadherin which deters migration of leukocytes across the endothelial cell monolayer (studied in the F.I.R.E. trial (Efficacy of FX06 in the Prevention of Myocardial Reperfusion Injury)
- Magnesium, which was evaluated by the Fourth International Study of Infarct Survival (ISIS-4) and the MAGIC trial.
- Hyperoxemia, the delivery of supersaturated oxygen after PCI (Studied in the AMIHOT II trial).
- Bendavia studied in the EMBRACE STEMI trial
There are several explanations for why trials of experimental agents have failed in this area:
- The therapy was administered after reperfusion and after reperfusion injury had set in
- The greatest benefit is observed in anterior ST-elevation myocardial infarctions (as demonstrated in the AMISTAD study), and inclusion of non-anterior locations minimizes the potential benefit
- There are uninhibited redundant pathways mediating reperfusion injury
- Inadequate dosing of the agent