Lung abscess pathophysiology: Difference between revisions
Aditya Ganti (talk | contribs) |
|||
| Line 3: | Line 3: | ||
{{CMG}};{{AE}}{{ADG}} | {{CMG}};{{AE}}{{ADG}} | ||
==Overview== | ==Overview== | ||
[[Aspiration (medicine)|Aspiration]] of [[anaerobic bacteria]] is the inciting event for the development of lung abscess. Once the aspirate is localized it results in [[pneumonitis]]. [[Inflammation|Inflammatory]] mediators are released, resulting in the formation of colliquative [[necrosis]]. The right side lung is more commonly affected than the left. On gross morphology, the lesions are well circumscribed filled with necrotic debris and do not demonstrate well-defined borders with the surrounding [[lung]] parenchyma. Microscopic examination demonstrates neutrophilic [[granulocytes]] with dilated [[blood vessels]] and inflammatory [[edema]]. | [[Aspiration (medicine)|Aspiration]] of [[anaerobic bacteria]] is the inciting event for the development of lung abscess. Once the aspirate is localized it results in [[pneumonitis]]. [[Inflammation|Inflammatory]] [[Mediator|mediators]] are released, resulting in the formation of colliquative [[necrosis]]. The right side lung is more commonly affected than the left. On gross morphology, the lesions are well circumscribed filled with [[necrotic]] debris and do not demonstrate well-defined borders with the surrounding [[lung]] [[parenchyma]]. [[Microscopic]] examination demonstrates neutrophilic [[granulocytes]] with dilated [[blood vessels]] and [[inflammatory]] [[edema]]. | ||
. | . | ||
==Pathophysiology== | ==Pathophysiology== | ||
*[[Aspiration (medicine)|Aspiration]] of [[anaerobic bacteria]] from the | *[[Aspiration (medicine)|Aspiration]] of [[anaerobic bacteria]] from the [[oropharynx]], due to altered level of [[consciousness]], absent [[gag reflex]] or inability to [[swallow]] is the inciting event for the development of primary lung abscess.<ref name="pmid936601">{{cite journal |vauthors= |title=Lung abscess |journal=West. J. Med. |volume=124 |issue=6 |pages=476–82 |year=1976 |pmid=936601 |pmc=1130102 |doi= |url=}}</ref> | ||
*In healthy individuals, [[defense mechanisms]] cope up with the small amounts of aspirates with no effects, however, in conditions like [[alcoholism]], [[diabetes mellitus]], and [[immunocompromised]] state these defense mechanisms can be compromised leading to decreased activity of alveolar [[macrophages]] and mobility of [[leukocytes]]. <ref name="pmid5683476">{{cite journal |vauthors=Green LH, Green GM |title=Differential suppression of pulmonary antibacterial activity as the mechanism of selection of a pathogen in mixed bacterial infection of the lung |journal=Am. Rev. Respir. Dis. |volume=98 |issue=5 |pages=819–24 |year=1968 |pmid=5683476 |doi=10.1164/arrd.1968.98.5.819 |url=}}</ref>. | *In healthy individuals, [[defense mechanisms]] cope up with the small amounts of aspirates with no effects, however, in conditions like [[alcoholism]], [[diabetes mellitus]], and [[immunocompromised]] state these defense mechanisms can be compromised leading to decreased activity of [[alveolar]] [[macrophages]] and mobility of [[leukocytes]]. <ref name="pmid5683476">{{cite journal |vauthors=Green LH, Green GM |title=Differential suppression of pulmonary antibacterial activity as the mechanism of selection of a pathogen in mixed bacterial infection of the lung |journal=Am. Rev. Respir. Dis. |volume=98 |issue=5 |pages=819–24 |year=1968 |pmid=5683476 |doi=10.1164/arrd.1968.98.5.819 |url=}}</ref>. | ||
*In secondary lung abscess, abscess formation depends on the underlying [[lung disease]] and predisposing factors, for example, bronchial [[obstruction]] from benign or malignant intrabronchial lesions or extrinsic compression of [[bronchus]] as in middle lobe syndrome results in [[distal]] abscess formation due to decreased oropharyngeal clearance and favoring abscess formation. | *In secondary lung abscess, [[abscess]] formation depends on the underlying [[lung disease]] and predisposing factors, for example, [[bronchial]] [[obstruction]] from benign or malignant intrabronchial [[lesions]] or extrinsic compression of [[bronchus]] as in middle lobe syndrome results in [[distal]] abscess formation due to decreased [[oropharyngeal]] clearance and favoring abscess formation. | ||
*Once the aspirate is localized it results in [[pneumonitis]]. <ref name="pmid15599270">{{cite journal |vauthors=Brook I |title=Anaerobic pulmonary infections in children |journal=Pediatr Emerg Care |volume=20 |issue=9 |pages=636–40 |year=2004 |pmid=15599270 |doi= |url=}}</ref> | *Once the aspirate is localized it results in [[pneumonitis]]. <ref name="pmid15599270">{{cite journal |vauthors=Brook I |title=Anaerobic pulmonary infections in children |journal=Pediatr Emerg Care |volume=20 |issue=9 |pages=636–40 |year=2004 |pmid=15599270 |doi= |url=}}</ref> | ||
*[[Inflammation|Inflammatory]] mediators along with various bacterial [[toxins]] and [[Proteolytic enzyme|proteolytic]] enzymes from the [[neutrophils]] are released, leading to the rupture of small [[blood vessels]] resulting in the formation of colliquative [[necrosis]]. <ref name="pmid22388585">{{cite journal |vauthors=Tsai YF, Ku YH |title=Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration |journal=Curr Opin Pulm Med |volume=18 |issue=3 |pages=246–52 |year=2012 |pmid=22388585 |doi=10.1097/MCP.0b013e3283521022 |url=}}</ref><br> | *[[Inflammation|Inflammatory]] mediators along with various [[bacterial]] [[toxins]] and [[Proteolytic enzyme|proteolytic]] [[enzymes]] from the [[neutrophils]] are released, leading to the rupture of small [[blood vessels]] resulting in the formation of colliquative [[necrosis]]. <ref name="pmid22388585">{{cite journal |vauthors=Tsai YF, Ku YH |title=Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration |journal=Curr Opin Pulm Med |volume=18 |issue=3 |pages=246–52 |year=2012 |pmid=22388585 |doi=10.1097/MCP.0b013e3283521022 |url=}}</ref><br> | ||
====Location of abscess==== | ====Location of abscess==== | ||
*The right side lung is more commonly affected than the left because the right [[bronchus]] is more acutely angulated when compared to left [[Bronchus|bronch]]<nowiki/>i. | *The right side lung is more commonly affected than the left because the right [[bronchus]] is more acutely angulated when compared to left [[Bronchus|bronch]]<nowiki/>i. | ||
| Line 18: | Line 18: | ||
===Genetics=== | ===Genetics=== | ||
*Congenital diseases such as [[cystic fibrosis]], [[vasculitis]], [[pulmonary sequestration]] and bronchial cysts are associated with increased the risk of lung abscess in children.<ref name="pmid3715782">{{cite journal |vauthors=Canny GJ, Marcotte JE, Levison H |title=Lung abscess in cystic fibrosis |journal=Thorax |volume=41 |issue=3 |pages=221–2 |year=1986 |pmid=3715782 |pmc=460300 |doi= |url=}}</ref> | *Congenital diseases such as [[cystic fibrosis]], [[vasculitis]], [[pulmonary sequestration]] and [[bronchial]] [[Cyst|cysts]] are associated with increased the risk of lung abscess in children.<ref name="pmid3715782">{{cite journal |vauthors=Canny GJ, Marcotte JE, Levison H |title=Lung abscess in cystic fibrosis |journal=Thorax |volume=41 |issue=3 |pages=221–2 |year=1986 |pmid=3715782 |pmc=460300 |doi= |url=}}</ref> | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
*In acute lung abscess, the lesions are well circumscribed filled with necrotic debris and do not demonstrate well-defined borders with the surrounding lung parenchyma.<ref name="pmid26366400">{{cite journal |vauthors=Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D |title=Lung abscess-etiology, diagnostic and treatment options |journal=Ann Transl Med |volume=3 |issue=13 |pages=183 |year=2015 |pmid=26366400 |pmc=4543327 |doi=10.3978/j.issn.2305-5839.2015.07.08 |url=}}</ref> | *In acute lung abscess, the lesions are well circumscribed filled with [[necrotic]] debris and do not demonstrate well-defined borders with the surrounding lung parenchyma.<ref name="pmid26366400">{{cite journal |vauthors=Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D |title=Lung abscess-etiology, diagnostic and treatment options |journal=Ann Transl Med |volume=3 |issue=13 |pages=183 |year=2015 |pmid=26366400 |pmc=4543327 |doi=10.3978/j.issn.2305-5839.2015.07.08 |url=}}</ref> | ||
*In chronic long standing abscess, the lesions are irregular and filled with grayish thick debris. | *In chronic long standing abscess, the lesions are irregular and filled with grayish thick debris. | ||
| Line 30: | Line 30: | ||
===Microscopic Findings=== | ===Microscopic Findings=== | ||
*In acute lung abscess, neutrophilic [[granulocytes]] are demonstrated with dilated blood vessels and [[Inflammation|inflammatory]] [[edema]].<ref name="pmid26366400">{{cite journal |vauthors=Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D |title=Lung abscess-etiology, diagnostic and treatment options |journal=Ann Transl Med |volume=3 |issue=13 |pages=183 |year=2015 |pmid=26366400 |pmc=4543327 |doi=10.3978/j.issn.2305-5839.2015.07.08 |url=}}</ref> | *In acute lung abscess, neutrophilic [[granulocytes]] are demonstrated with dilated [[blood vessels]] and [[Inflammation|inflammatory]] [[edema]].<ref name="pmid26366400">{{cite journal |vauthors=Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D |title=Lung abscess-etiology, diagnostic and treatment options |journal=Ann Transl Med |volume=3 |issue=13 |pages=183 |year=2015 |pmid=26366400 |pmc=4543327 |doi=10.3978/j.issn.2305-5839.2015.07.08 |url=}}</ref> | ||
*In chronic lung abscess, biopsy specimen demonstrates [[lymphocytes]], [[plasma cells]], and [[histiocytes]] around a layer of [[pyogenic]] membrane surrounding the abscess [[cavity]] which is filled with [[pus]]. | *In chronic lung abscess, [[biopsy]] specimen demonstrates [[lymphocytes]], [[plasma cells]], and [[histiocytes]] around a layer of [[pyogenic]] membrane surrounding the abscess [[cavity]] which is filled with [[pus]]. | ||
<gallery> | <gallery> | ||
Image:Acute lung abscess microscopic.png|Acute lung abscess abscess full of inflammatory cells (primarily neutrophils) (arrows). There is a bacterial colony in the center of this abscess (1).. | Image:Acute lung abscess microscopic.png|Acute lung abscess abscess full of inflammatory cells (primarily neutrophils) (arrows). There is a bacterial colony in the center of this abscess (1).. | ||
Revision as of 18:25, 5 April 2017
|
Lung abscess Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Lung abscess pathophysiology On the Web |
|
American Roentgen Ray Society Images of Lung abscess pathophysiology |
|
Risk calculators and risk factors for Lung abscess pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Aspiration of anaerobic bacteria is the inciting event for the development of lung abscess. Once the aspirate is localized it results in pneumonitis. Inflammatory mediators are released, resulting in the formation of colliquative necrosis. The right side lung is more commonly affected than the left. On gross morphology, the lesions are well circumscribed filled with necrotic debris and do not demonstrate well-defined borders with the surrounding lung parenchyma. Microscopic examination demonstrates neutrophilic granulocytes with dilated blood vessels and inflammatory edema. .
Pathophysiology
- Aspiration of anaerobic bacteria from the oropharynx, due to altered level of consciousness, absent gag reflex or inability to swallow is the inciting event for the development of primary lung abscess.[1]
- In healthy individuals, defense mechanisms cope up with the small amounts of aspirates with no effects, however, in conditions like alcoholism, diabetes mellitus, and immunocompromised state these defense mechanisms can be compromised leading to decreased activity of alveolar macrophages and mobility of leukocytes. [2].
- In secondary lung abscess, abscess formation depends on the underlying lung disease and predisposing factors, for example, bronchial obstruction from benign or malignant intrabronchial lesions or extrinsic compression of bronchus as in middle lobe syndrome results in distal abscess formation due to decreased oropharyngeal clearance and favoring abscess formation.
- Once the aspirate is localized it results in pneumonitis. [3]
- Inflammatory mediators along with various bacterial toxins and proteolytic enzymes from the neutrophils are released, leading to the rupture of small blood vessels resulting in the formation of colliquative necrosis. [4]
Location of abscess
- The right side lung is more commonly affected than the left because the right bronchus is more acutely angulated when compared to left bronchi.
- The most common location is the posterior segment of the right apical lobe or apical segments of lower lobes of both the lungs.[5]
- In alcoholics and hospitalized patients are in the supine position, right lateral part of the posterior segment of the upper lobe is more commonly involved.
Genetics
- Congenital diseases such as cystic fibrosis, vasculitis, pulmonary sequestration and bronchial cysts are associated with increased the risk of lung abscess in children.[6]
Gross Pathology
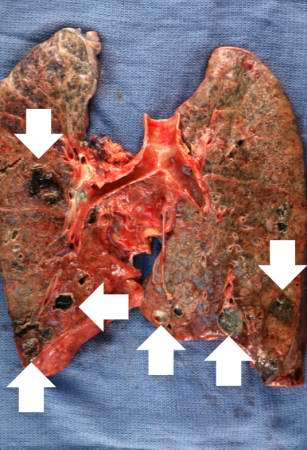
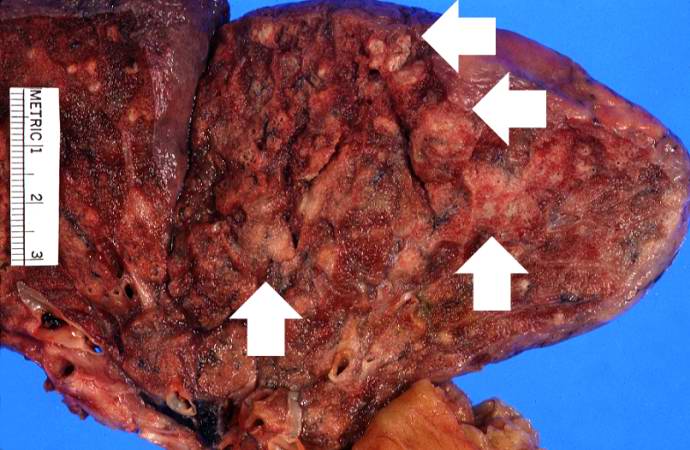
- In acute lung abscess, the lesions are well circumscribed filled with necrotic debris and do not demonstrate well-defined borders with the surrounding lung parenchyma.[7]
- In chronic long standing abscess, the lesions are irregular and filled with grayish thick debris.
-
Gross photograph of the lung abscess. Note the abscesses (arrows) especially in the lower lobes.
-
In this section of upper lobe there are multiple areas of early abscess formation (arrows). Note the circumscribed whitish-tan lesions. These lesions are filled with white blood cells.
Microscopic Findings
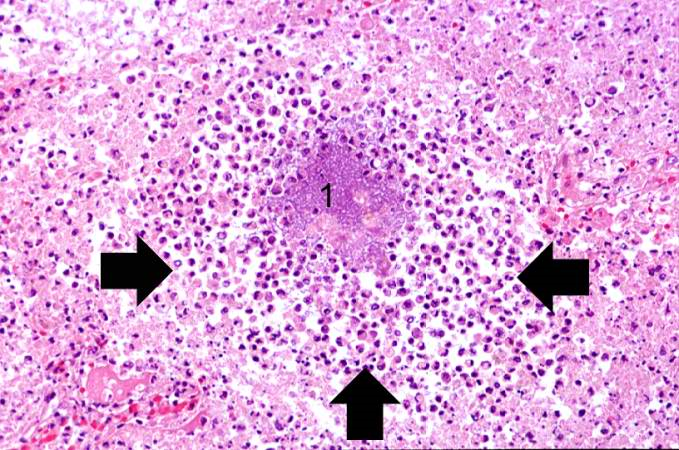
- In acute lung abscess, neutrophilic granulocytes are demonstrated with dilated blood vessels and inflammatory edema.[7]
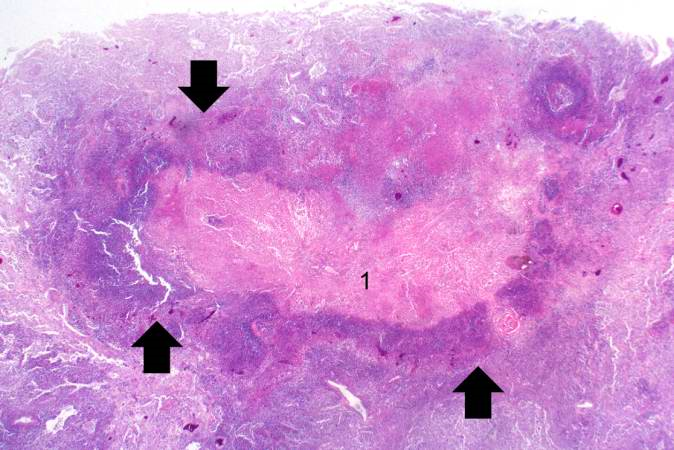
- In chronic lung abscess, biopsy specimen demonstrates lymphocytes, plasma cells, and histiocytes around a layer of pyogenic membrane surrounding the abscess cavity which is filled with pus.
-
Acute lung abscess abscess full of inflammatory cells (primarily neutrophils) (arrows). There is a bacterial colony in the center of this abscess (1)..
-
Chronic lung abscess containing necrotic debris (1) and there is a rim of viable inflammatory cells (arrows) surrounding this abscess..
Reference
- ↑ "Lung abscess". West. J. Med. 124 (6): 476–82. 1976. PMC 1130102. PMID 936601.
- ↑ Green LH, Green GM (1968). "Differential suppression of pulmonary antibacterial activity as the mechanism of selection of a pathogen in mixed bacterial infection of the lung". Am. Rev. Respir. Dis. 98 (5): 819–24. doi:10.1164/arrd.1968.98.5.819. PMID 5683476.
- ↑ Brook I (2004). "Anaerobic pulmonary infections in children". Pediatr Emerg Care. 20 (9): 636–40. PMID 15599270.
- ↑ Tsai YF, Ku YH (2012). "Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration". Curr Opin Pulm Med. 18 (3): 246–52. doi:10.1097/MCP.0b013e3283521022. PMID 22388585.
- ↑ Bartlett JG (1993). "Anaerobic bacterial infections of the lung and pleural space". Clin. Infect. Dis. 16 Suppl 4: S248–55. PMID 8324127.
- ↑ Canny GJ, Marcotte JE, Levison H (1986). "Lung abscess in cystic fibrosis". Thorax. 41 (3): 221–2. PMC 460300. PMID 3715782.
- ↑ 7.0 7.1 Kuhajda I, Zarogoulidis K, Tsirgogianni K, Tsavlis D, Kioumis I, Kosmidis C, Tsakiridis K, Mpakas A, Zarogoulidis P, Zissimopoulos A, Baloukas D, Kuhajda D (2015). "Lung abscess-etiology, diagnostic and treatment options". Ann Transl Med. 3 (13): 183. doi:10.3978/j.issn.2305-5839.2015.07.08. PMC 4543327. PMID 26366400.