Tricuspid regurgitation cardiac MRI: Difference between revisions
Jump to navigation
Jump to search
| (6 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Tricuspid regurgitation}} | {{Tricuspid regurgitation}} | ||
{{CMG}}; {{AE}} {{Rim}} | {{CMG}}; {{AE}} {{VKG}} {{Rim}} | ||
==Overview== | ==Overview== | ||
| Line 9: | Line 9: | ||
* [[Cardiac magnetic resonance|Cardiac MRI]] is useful in evaluating the structure and function of the [[right atrium]] and [[right ventricle]] as well as the severity of the [[tricuspid regurgitation]], especially when [[echocardiography]] is inconclusive. | * [[Cardiac magnetic resonance|Cardiac MRI]] is useful in evaluating the structure and function of the [[right atrium]] and [[right ventricle]] as well as the severity of the [[tricuspid regurgitation]], especially when [[echocardiography]] is inconclusive. | ||
* Findings on MRI suggestive | * Findings on [[Magnetic resonance imaging|MRI]] suggestive of [[tricuspid regurgitation]] include:<ref name="ZoghbiAdams2017">{{cite journal|last1=Zoghbi|first1=William A.|last2=Adams|first2=David|last3=Bonow|first3=Robert O.|last4=Enriquez-Sarano|first4=Maurice|last5=Foster|first5=Elyse|last6=Grayburn|first6=Paul A.|last7=Hahn|first7=Rebecca T.|last8=Han|first8=Yuchi|last9=Hung|first9=Judy|last10=Lang|first10=Roberto M.|last11=Little|first11=Stephen H.|last12=Shah|first12=Dipan J.|last13=Shernan|first13=Stanton|last14=Thavendiranathan|first14=Paaladinesh|last15=Thomas|first15=James D.|last16=Weissman|first16=Neil J.|title=Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation|journal=Journal of the American Society of Echocardiography|volume=30|issue=4|year=2017|pages=303–371|issn=08947317|doi=10.1016/j.echo.2017.01.007}}</ref><ref name="pmid29332606">{{cite journal| author=Driessen MMP, Schings MA, Sieswerda GT, Doevendans PA, Hulzebos EH, Post MC | display-authors=etal| title=Tricuspid flow and regurgitation in congenital heart disease and pulmonary hypertension: comparison of 4D flow cardiovascular magnetic resonance and echocardiography. | journal=J Cardiovasc Magn Reson | year= 2018 | volume= 20 | issue= 1 | pages= 5 | pmid=29332606 | doi=10.1186/s12968-017-0426-7 | pmc=5767973 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29332606 }}</ref><ref name="pmid24224411">{{cite journal| author=Reddy ST, Shah M, Doyle M, Thompson DV, Williams RB, Yamrozik J | display-authors=etal| title=Evaluation of cardiac valvular regurgitant lesions by cardiac MRI sequences: comparison of a four-valve semi-quantitative versus quantitative approach. | journal=J Heart Valve Dis | year= 2013 | volume= 22 | issue= 4 | pages= 491-9 | pmid=24224411 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24224411 }}</ref><ref name="pmid30259253">{{cite journal| author=Mathew RC, Löffler AI, Salerno M| title=Role of Cardiac Magnetic Resonance Imaging in Valvular Heart Disease: Diagnosis, Assessment, and Management. | journal=Curr Cardiol Rep | year= 2018 | volume= 20 | issue= 11 | pages= 119 | pmid=30259253 | doi=10.1007/s11886-018-1057-9 | pmc=6415765 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30259253 }}</ref><ref name="ZhanDebs2019">{{cite journal|last1=Zhan|first1=Yang|last2=Debs|first2=Dany|last3=Khan|first3=Mohammad|last4=Nguyen|first4=Duc|last5=Graviss|first5=Edward|last6=Shah|first6=Dipan J.|title=CLINICAL OUTCOMES OF SECONDARY TRICUSPID REGURGITATION QUANTIFIED USING CARDIOVASCULAR MAGNETIC RESONANCE|journal=Journal of the American College of Cardiology|volume=73|issue=9|year=2019|pages=3074|issn=07351097|doi=10.1016/S0735-1097(19)33680-0}}</ref><ref name="ZhanSenapati2020">{{cite journal|last1=Zhan|first1=Yang|last2=Senapati|first2=Alpana|last3=Vejpongsa|first3=Pimprapa|last4=Xu|first4=Jiaqiong|last5=Shah|first5=Dipan J.|last6=Nagueh|first6=Sherif F.|title=Comparison of Echocardiographic Assessment of Tricuspid Regurgitation Against Cardiovascular Magnetic Resonance|journal=JACC: Cardiovascular Imaging|year=2020|issn=1936878X|doi=10.1016/j.jcmg.2020.01.008}}</ref> | ||
**[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in giving the quantitative assessment of tricuspid regurgitant volume (TRV)<ref name="pmid28027750">{{cite journal| author=Medvedofsky D, León Jiménez J, Addetia K, Singh A, Lang RM, Mor-Avi V | display-authors=etal| title=Multi-parametric quantification of tricuspid regurgitation using cardiovascular magnetic resonance: A comparison to echocardiography. | journal=Eur J Radiol | year= 2017 | volume= 86 | issue= | pages= 213-220 | pmid=28027750 | doi=10.1016/j.ejrad.2016.11.025 | pmc=5372350 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28027750 }}</ref> | **[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in giving the quantitative assessment of [[Tricuspid regurgitation|tricuspid regurgitant]] volume (TRV)<ref name="pmid28027750">{{cite journal| author=Medvedofsky D, León Jiménez J, Addetia K, Singh A, Lang RM, Mor-Avi V | display-authors=etal| title=Multi-parametric quantification of tricuspid regurgitation using cardiovascular magnetic resonance: A comparison to echocardiography. | journal=Eur J Radiol | year= 2017 | volume= 86 | issue= | pages= 213-220 | pmid=28027750 | doi=10.1016/j.ejrad.2016.11.025 | pmc=5372350 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28027750 }}</ref> | ||
***Severe [[tricuspid regurgitation]] if TMR is ≥30 ml, or in a separate analysis, ≥40 ml | ***Severe [[tricuspid regurgitation]] if TMR is ≥30 ml, or in a separate analysis, ≥40 ml | ||
***Moderate or mild [[tricuspid regurgitation]] if TMR is < the above threshold. | ***Moderate or mild [[tricuspid regurgitation]] if TMR is < the above threshold. | ||
**[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in estimation of regurgitant fraction | **[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in estimation of [[Regurgitation|regurgitant]] fraction | ||
**[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in estimation of RV volumes and ejection fraction | **[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in estimation of [[Right ventricle|RV]] volumes and [[ejection fraction]] | ||
**[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in evaluation of associated left ventricle and mitral disease | **[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in evaluation of associated left ventricle and [[Mitral valve|mitral]] disease | ||
**[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in identification of TR jet area | **[[Cardiac magnetic resonance|Cardiac magnetic resonance imaging]] ([[CMR]]) helps in identification of TR jet area | ||
** | ** | ||
| Line 28: | Line 28: | ||
|- | |- | ||
|} | |} | ||
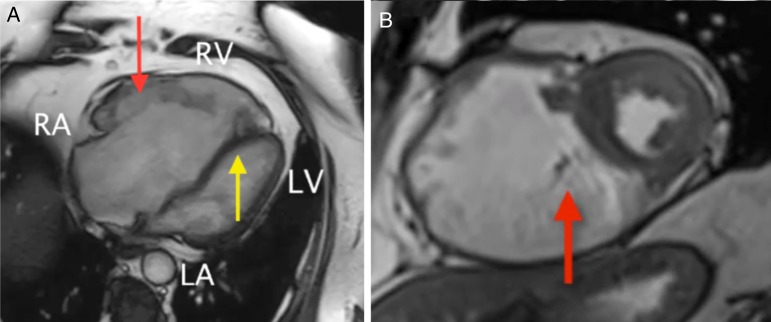
[[File:CMR four-chamber cine view. Seen here is the grossly dilated right heart, with an atrialized RV and dilated tricuspid annulus.jpg|alt=CMR four-chamber cine view|center|thumb|771x771px|('''A''') CMR four-chamber cine view. Seen here is the grossly dilated right heart, with an atrialized RV and dilated [[Tricuspid valve|tricuspid]] annulus. The enlarged anterior TV leaflet is well visualized (red arrow), as is the mislaid and hypoplastic septal leaflet (yellow arrow). The LA and LV are small, owing to compression from the volume-overload right heart. LA, [[left atrium]]; LV, [[left ventricle]]; RA, [[right atrium]]. RV, right ventricle. ('''B''') CMR short-axis cine view. The massively dilated atrial and ventricular portions of the right heart are visualized. Again the tricuspid valve septal leaflet is seen (red arrow) and the pale jet of tricuspid regurgitation is notable here in systole. Case courtesy by Gaurav Singh Gulsin et al<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4731738/|title=Gross right heart dilatation secondary to Ebstein's anomaly|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
[[File:MRI velocity-encoding magnitude.jpg|center|thumb|685x685px|(a) [[Magnetic resonance imaging|MRI]] velocity-encoding magnitude (top) and phase (bottom) flow images through the main pulmonary artery at different time points during early [[Systole (medicine)|systole]]. The images show a dilated [[pulmonary artery]] (PA), which appears larger than the aorta (Ao). The PA shows a negligible change in the cross-sectional area despite the flow increase with time (shown in the phase images). (b) [[Magnetic resonance imaging|MRI]] velocity-encoding magnitude (top) and phase (bottom) flow images through the tricuspid valve at end-systole showing severe tricuspid regurgitation (arrows). LV = left ventricle; RV = right ventricle. Case courtesy by El-Sayed H. Ibrahim et al<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4578844/|title=Severe Pulmonary Arterial Hypertension: Comprehensive Evaluation by Magnetic Resonance Imaging|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
<br /> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 04:15, 28 April 2020
|
Tricuspid Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid regurgitation cardiac MRI On the Web |
|
American Roentgen Ray Society Images of Tricuspid regurgitation cardiac MRI |
|
Risk calculators and risk factors for Tricuspid regurgitation cardiac MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vamsikrishna Gunnam M.B.B.S [2] Rim Halaby, M.D. [3]
Overview
Cardiac magnetic resonance imaging (CMR) may be beneficial when echocardiography findings are inconclusive, particularly before tricuspid valve surgery.[1]
Cardiac MRI
- Cardiac MRI is useful in evaluating the structure and function of the right atrium and right ventricle as well as the severity of the tricuspid regurgitation, especially when echocardiography is inconclusive.
- Findings on MRI suggestive of tricuspid regurgitation include:[2][3][4][5][6][7]
- Cardiac magnetic resonance imaging (CMR) helps in giving the quantitative assessment of tricuspid regurgitant volume (TRV)[8]
- Severe tricuspid regurgitation if TMR is ≥30 ml, or in a separate analysis, ≥40 ml
- Moderate or mild tricuspid regurgitation if TMR is < the above threshold.
- Cardiac magnetic resonance imaging (CMR) helps in estimation of regurgitant fraction
- Cardiac magnetic resonance imaging (CMR) helps in estimation of RV volumes and ejection fraction
- Cardiac magnetic resonance imaging (CMR) helps in evaluation of associated left ventricle and mitral disease
- Cardiac magnetic resonance imaging (CMR) helps in identification of TR jet area
- Cardiac magnetic resonance imaging (CMR) helps in giving the quantitative assessment of tricuspid regurgitant volume (TRV)[8]
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary[1]
| Class IIb |
| "1. CMR or real-time 3-dimensional echocardiography may be considered for assessment of RV systolic function and systolic and diastolic volumes in patients with severe TR (stages C and D) and suboptimal 2-dimensional echocardiograms. (Level of Evidence: C)" |

References
- ↑ 1.0 1.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (23): 2440–92. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Zoghbi, William A.; Adams, David; Bonow, Robert O.; Enriquez-Sarano, Maurice; Foster, Elyse; Grayburn, Paul A.; Hahn, Rebecca T.; Han, Yuchi; Hung, Judy; Lang, Roberto M.; Little, Stephen H.; Shah, Dipan J.; Shernan, Stanton; Thavendiranathan, Paaladinesh; Thomas, James D.; Weissman, Neil J. (2017). "Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation". Journal of the American Society of Echocardiography. 30 (4): 303–371. doi:10.1016/j.echo.2017.01.007. ISSN 0894-7317.
- ↑ Driessen MMP, Schings MA, Sieswerda GT, Doevendans PA, Hulzebos EH, Post MC; et al. (2018). "Tricuspid flow and regurgitation in congenital heart disease and pulmonary hypertension: comparison of 4D flow cardiovascular magnetic resonance and echocardiography". J Cardiovasc Magn Reson. 20 (1): 5. doi:10.1186/s12968-017-0426-7. PMC 5767973. PMID 29332606.
- ↑ Reddy ST, Shah M, Doyle M, Thompson DV, Williams RB, Yamrozik J; et al. (2013). "Evaluation of cardiac valvular regurgitant lesions by cardiac MRI sequences: comparison of a four-valve semi-quantitative versus quantitative approach". J Heart Valve Dis. 22 (4): 491–9. PMID 24224411.
- ↑ Mathew RC, Löffler AI, Salerno M (2018). "Role of Cardiac Magnetic Resonance Imaging in Valvular Heart Disease: Diagnosis, Assessment, and Management". Curr Cardiol Rep. 20 (11): 119. doi:10.1007/s11886-018-1057-9. PMC 6415765. PMID 30259253.
- ↑ Zhan, Yang; Debs, Dany; Khan, Mohammad; Nguyen, Duc; Graviss, Edward; Shah, Dipan J. (2019). "CLINICAL OUTCOMES OF SECONDARY TRICUSPID REGURGITATION QUANTIFIED USING CARDIOVASCULAR MAGNETIC RESONANCE". Journal of the American College of Cardiology. 73 (9): 3074. doi:10.1016/S0735-1097(19)33680-0. ISSN 0735-1097.
- ↑ Zhan, Yang; Senapati, Alpana; Vejpongsa, Pimprapa; Xu, Jiaqiong; Shah, Dipan J.; Nagueh, Sherif F. (2020). "Comparison of Echocardiographic Assessment of Tricuspid Regurgitation Against Cardiovascular Magnetic Resonance". JACC: Cardiovascular Imaging. doi:10.1016/j.jcmg.2020.01.008. ISSN 1936-878X.
- ↑ Medvedofsky D, León Jiménez J, Addetia K, Singh A, Lang RM, Mor-Avi V; et al. (2017). "Multi-parametric quantification of tricuspid regurgitation using cardiovascular magnetic resonance: A comparison to echocardiography". Eur J Radiol. 86: 213–220. doi:10.1016/j.ejrad.2016.11.025. PMC 5372350. PMID 28027750.
- ↑ "Gross right heart dilatation secondary to Ebstein's anomaly".
- ↑ "Severe Pulmonary Arterial Hypertension: Comprehensive Evaluation by Magnetic Resonance Imaging".