Tricuspid regurgitation surgery
|
Tricuspid Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid regurgitation surgery On the Web |
|
American Roentgen Ray Society Images of Tricuspid regurgitation surgery |
|
Risk calculators and risk factors for Tricuspid regurgitation surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Zand, M.D.[2] Rim Halaby, M.D. [3] Fatimo Biobaku M.B.B.S [4] Synonyms and keywords: TR; Tricuspid regurgitation; Primary TR; Secondary TR; AF; Atrial fibrillation; RV; Right ventricle, TTE; Transthoracic echocardiography
Overview
Pulmonary hypertension or myocardial disease are two factors that affect the treatment of secondary TR. The surgical approach is considered for selected patients with severe TR (stage C,D) at the time of left-sided valve lesions surgery and to prevent later development of severe TR in patients with progressive TR (Stage B). For selected patients with isolated TR (either primary TR or secondary TR attributable to annular dilation in the absence of pulmonary hypertension or dilated cardiomyopathy), surgical intervention is recommended. Mortality rate is high in patients undergone interventions for severe isolated TR due to end-organ damage. However, outcomes of patients with severe primary TR are poor with medical management. Earlier surgery for patients with severe isolated TR before the onset of severe RV dysfunction or end-organ damage is recommended.
Surgery
Indications for Surgery
- Primary or secondary severe TR may not improve after treatment of the left-sided valve lesion and reduction of RV afterload. [1]
- Re-operation for severe, isolated TR after left-sided valve surgery is associated with a perioperative mortality rate of 10% to 25%.
- Tricuspid valve repair will not increase the risks of surgery.[2]
- Tricuspid valve repair is preferable to replacement due to lower operative risk, but replacement may be indicated if there is marked dilation of the annulus or intrinsic disease of the tricuspid leaflets.[3]
- The risks and benefits of tricuspid valve operation should be carefully considered in the presence of severe RV systolic dysfunction or irreversible pulmonary hypertension because of the possibility of RV failure after the operation.
- If mild or moderate degrees of secondary TR are left uncorrected at the time of left-sided valve surgery, they may progress over time in approximately 25% of patients and result in reduced long-term functional outcome and survival.
- Risk factors for persistence or progression of TR include tricuspid annulus dilation (>40 mm diameter or 21 mm/m2 diameter indexed to body surface area on preoperative TTE measured at end-diastole; >70 mm diameter on direct intraoperative measurement of the intercomissural distance), degree of RV dysfunction or remodeling, leaflet tethering height, pulmonary artery hypertension, AF, and intra-annular RV pacemaker or implantable cardioverter-defibrillator leads.
- Studies showed the benefits of tricuspid repair at the time of mitral valve surgery for progressive TR (Stage B) with tricuspid annulus dilation.
- In patients with symptomatic severe primary TR, reduction of the regurgitant volume load by tricuspid valve surgery can decrease systemic venous and hepatic congestion and the need for diuretics.
- Patients with severe congestive hepatopathy may also benefit from surgery to prevent irreversible cirrhosis of the liver.
- Quality and duration of long-term survival are related to residual RV function.[4]
- In patients with severe symptomatic primary TR from either device leads or endomyocardial biopsy, TR develops rapidly, and surgery can be performed before the onset of RV dysfunction.
- Correction of symptomatic severe primary TR (Stage D) in patients without left-sided valve disease would preferentially be performed before the onset of significant RV dysfunction or end-organ damage
- TR can develop in attribution with AF and annular dilation (a form of secondary TR).[5]
- AF-related TR may represent greater basal dilation and annular enlargement. However, RV elongation with leaflet tethering is seen in patients who have secondary TR caused by pulmonary hypertension or myocardial disease.
- These patients with AF-related TR have rapid progression of TR severity and right-sided chamber dilation.
- In AF-related severe TR, quality of life and symptoms can be improved by surgical intervention for TR.
- Outcomes are better in patients undergoing intervention and no evidence of severe RV dysfunction or end-organ damage.
| Recommendations for intervention in tricuspid valve disease | |
| Primary Tricuspid Regurgitation (Class I, Level of Evidence C): | |
|
❑Surgery is recommended in patients with severe primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Primary Tricuspid Regurgitation (Class IIa, Level of Evidence C): | |
|
❑Surgery should be considered in patients with moderate primary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class I, Level of Evidence B): | |
|
❑Surgery is recommended in patients with severe secondary tricuspid regurgitation undergoing left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIa, Level of Evidence B): | |
|
❑Surgery should be considered in patients with mild or moderate secondary tricuspid regurgitation with a dilated annulus (≥40 mm or >21 mm/m2 by 2D echocardiography) undergoing
left-sided valve surgery | |
| Secondary Tricuspid Regurgitation (Class IIb, Level of Evidence C): | |
|
❑Transcatheter treatment of symptomatic secondary severe tricuspid regurgitation may be considered in inoperable patients |
| The above table adopted from 2021 ESC Guideline[6] |
|---|
| Tricuspid regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Progressive TR (Stage B) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| At time of left sided valve surgery | Severe TR (Stage C,D) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Annular dilation> 4 cm, or perior righ heart failure | Asymptomatic (Stage C) | At time of left sided valve surgery | Right heart failure (Stage D) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TV surgery (2a) | Primary TR with progressive RV dilation or systolic dysfunction | TV surgery (1) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TV surgery (2b) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Primary TR | Prior left sided valve surgery | Secondary TR | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TV surgery (2a) | Absent of severe pulmonary hypertension or RV systolic dysfunction | Poor response to medical therapy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TV surgery (2b) | Annular dilation without pulmonary hypertension or left sided disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TV surgery (2a) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Abbreviations:
TR: Tricuspid Regurgitation;
TV: Tricuspid valve;
RV: Right ventricle
| The above algorithm adapted from 2020 AHA Guideline[7] |
|---|
Surgical Methods
Annuloplasty
The principal surgical repair for secondary TR is tricuspid annuloplasty. The aim of tricuspid annuloplasty is to improve leaflet coaptation by correcting annular dilatation and restoring annular geometry. The two principle surgical methods are:[8][9]
- Ring annuloplasty: It is regarded as the standard for surgical repair. The size of the tricuspid annulus is permanently fixed by implantation of a rigid or semi rigid prosthesis, undersized ring, and it is associated with a reduced incidence of late, recurrent tricuspid regurgitation.
- Suture annuloplasty: It is technically easy and can be done quickly. Also, compared with the ring annuloplasty, a prosthetic implant is not used with suture annuloplasty and the risk of postoperative conduction disturbances is lower.
Other methods:[8]
- Adjunctive repair techniques: This may be necessary for augmentation of the effects of the ring annuloplasty in patients with marked leaflet tethering and right ventricular remodeling. The long-term outcomes and durability of these adjunctive techniques are not well established. Types of adjunctive repair techniques are listed in the table below.
| Anterior leaflet augmentation using an autologous pericardial patch | ''Clover'' technique | Double orifice valve technique |
|---|---|---|
| Helps improve leaflet coaptation while maintaining leaflet mobility |
|
|
- Tricuspid valve replacement
- The initial approach in tricuspid surgery is repair; however, replacement is done whenever the valve is badly diseased.
- Bioprosthetic valves are currently favored, however, no significant hemodynamic difference between mechanical and biological valves was observed.[11]
- Transcatheter therapies
- The safety and feasibility of transcatheter therapies for treating severe tricuspid regurgitation are shown in the study:
- Three types of transcatheter therapies have recently emerged for treating severe tricuspid regurgitation:
- Heterotopic caval transcatheter valve implantation
- Transcatheter tricuspid valve annuloplasty
- Coaptation device
- Transcatheter tricuspid valve replacement[12]
2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[13]
Recommendations for Timing of Intervention Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1. In patients with severe TR (Stages C and D) undergoing left-sided valve surgery, tricuspid valve surgery is recommended. (Level of Evidence: B-NR) |
| Class IIa |
| 2. In patients with progressive TR (Stage B) undergoing left-sided valve surgery, tricuspid valve surgery can be beneficial in the context of either 1) tricuspid annular dilation (tricuspid annulus end diastolic diameter >4.0 cm) or 2) prior signs and symptoms of right-sided HF.(Level of Evidence: B-NR)
3. In patients with signs and symptoms of right-sided HF and severe primary TR (Stage D), isolated tricuspid valve surgery can be beneficial to reduce symptoms and recurrent hospitalizations(Level of Evidence: B-NR) 4. In patients with signs and symptoms of right-sided HF and severe isolated secondary TR attributable to annular dilation (in the absence of pulmonary hypertension or left-sided disease) who are poorly responsive to medical therapy (Stage D), isolated tricuspid valve surgery can be beneficial to reduce symptoms and recurrent hospitalizations.(Level of Evidence: B-NR) |
| Class IIb |
| 5. In asymptomatic patients with severe primary TR (Stage C) and progressive RV dilation or systolic dysfunction, isolated tricuspid valve surgery may be considered(Level of Evidence: C-LD)
6. In patients with signs and symptoms of right-sided HF and severe TR (Stage D) who have undergone previous left-sided valve surgery, reoperation with isolated tricuspid valve surgery may be considered in the absence of severe pulmonary hypertension or severe RV systolic dysfunction(Level of Evidence: B-NR) |
References
- ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O'Gara PT, Rigolin VH, Sundt TM, Thompson A, Toly C (February 2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e72–e227. doi:10.1161/CIR.0000000000000923. PMID 33332150 Check
|pmid=value (help). - ↑ Rogers JH, Bolling SF (May 2009). "The tricuspid valve: current perspective and evolving management of tricuspid regurgitation". Circulation. 119 (20): 2718–25. doi:10.1161/CIRCULATIONAHA.108.842773. PMID 19470900.
- ↑ Chikwe J, Anyanwu AC (2010). "Surgical strategies for functional tricuspid regurgitation". Semin Thorac Cardiovasc Surg. 22 (1): 90–6. doi:10.1053/j.semtcvs.2010.05.002. PMID 20813324.
- ↑ Kadri AN, Menon V, Sammour YM, Gajulapalli RD, Meenakshisundaram C, Nusairat L, Mohananey D, Hernandez AV, Navia J, Krishnaswamy A, Griffin B, Rodriguez L, Harb SC, Kapadia S (December 2019). "Outcomes of patients with severe tricuspid regurgitation and congestive heart failure". Heart. 105 (23): 1813–1817. doi:10.1136/heartjnl-2019-315004. PMID 31422359.
- ↑ Mangoni AA, DiSalvo TG, Vlahakes GJ, Polanczyk CA, Fifer MA (January 2001). "Outcome following isolated tricuspid valve replacement". Eur J Cardiothorac Surg. 19 (1): 68–73. doi:10.1016/s1010-7940(00)00598-4. PMID 11163563.
- ↑ Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Jüni P, Pierard L, Prendergast BD, Sádaba JR, Tribouilloy C, Wojakowski W (February 2022). "2021 ESC/EACTS Guidelines for the management of valvular heart disease". Eur Heart J. 43 (7): 561–632. doi:10.1093/eurheartj/ehab395. PMID 34453165 Check
|pmid=value (help). - ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O'Gara PT, Rigolin VH, Sundt TM, Thompson A, Toly C (February 2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e35–e71. doi:10.1161/CIR.0000000000000932. PMID 33332149 Check
|pmid=value (help). - ↑ 8.0 8.1 Rodés-Cabau J, Taramasso M, O'Gara PT (2016). "Diagnosis and treatment of tricuspid valve disease: current and future perspectives". Lancet. 388 (10058): 2431–2442. doi:10.1016/S0140-6736(16)00740-6. PMID 27048553 PMID: 27048553 Check
|pmid=value (help). - ↑ Taramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O (2012). "The growing clinical importance of secondary tricuspid regurgitation". J Am Coll Cardiol. 59 (8): 703–10. doi:10.1016/j.jacc.2011.09.069. PMID 22340261.
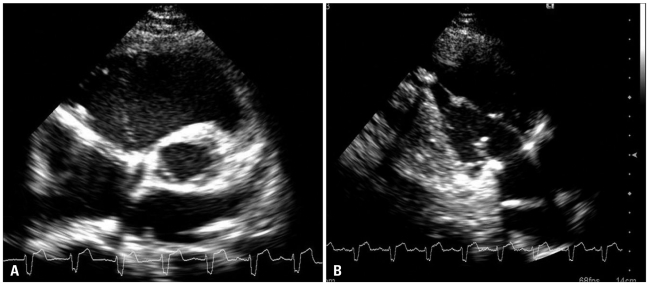
- ↑ "A Case of Traumatic Tricuspid Regurgitation Caused by Multiple Papillary Muscle Rupture".
- ↑ Altaani HA, Jaber S (June 2013). "Tricuspid Valve Replacement, Mechnical vs. Biological Valve, Which Is Better?". Int Cardiovasc Res J. 7 (2): 71–4. PMC 3987430. PMID 24757625.
- ↑ Lu FL, An Z, Ma Y, Song ZG, Cai CL, Li BL, Zhou GW, Han L, Wang J, Bai YF, Liu XH, Wang JF, Meng X, Zhang HB, Yang J, Dong NG, Hu SS, Pan XB, Cheung A, Qiao F, Xu ZY (October 2021). "Transcatheter tricuspid valve replacement in patients with severe tricuspid regurgitation". Heart. 107 (20): 1664–1670. doi:10.1136/heartjnl-2020-318199. PMID 33419880 Check
|pmid=value (help). - ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F; et al. (2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e72–e227. doi:10.1161/CIR.0000000000000923. PMID 33332150 Check
|pmid=value (help).