Mitral regurgitation physical examination: Difference between revisions
No edit summary |
Aditya Ganti (talk | contribs) |
||
| (14 intermediate revisions by 5 users not shown) | |||
| Line 2: | Line 2: | ||
{| class="infobox" style="float:right;" | {| class="infobox" style="float:right;" | ||
|- | |- | ||
| [[File:Siren.gif|30px|link=Mitral | | [[File:Siren.gif|30px|link=Mitral regurgitation resident survival guide]]|| <br> || <br> | ||
| [[Mitral | | [[Mitral regurgitation resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | ||
|} | |} | ||
{{Mitral regurgitation}} | {{Mitral regurgitation}} | ||
{{CMG}}; | {{CMG}}; {{AE}} {{CZ}}; [[Varun Kumar]], M.B.B.S.; [[Lakshmi Gopalakrishnan]], M.B.B.S.; {{YK}} | ||
==Overview== | ==Overview== | ||
Chronic compensated mitral regurgitation causes a blowing [[ | Chronic compensated mitral regurgitation (MR) causes a blowing holosystolic murmur which radiates to the left [[axilla]]. In acute severe MR, the murmur can be early systolic rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the [[left atrium]] and the equalization of pressures between the [[left atrium]] and [[left ventricle]]. The intensity of the murmur decreases with [[valsalva maneuver]] and standing and becomes louder with hand grip, squatting, and leg raising. The murmur might be short or absent in severe acute MR. In addition, [[S1]] is usually diminished and [[S2]] is commonly widely split. The pulmonic component of the second heart sound ([[P2]]) is louder than the aortic component ([[A2]]) in the presence of severe [[pulmonary hypertension]] thus widening the [[splitting of S2]]. | ||
==Physical Examination== | ==Physical Examination== | ||
Chronic compensated mitral regurgitation (MR) causes a blowing holosystolic murmur which radiates to the left [[axilla]]. In acute severe MR, the murmur can be early systolic rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the [[left atrium]] and the equalization of pressures between the [[left atrium]] and [[left ventricle]]. The intensity of the murmur decreases with [[valsalva maneuver]] and standing and becomes louder with hand grip, squatting, and leg raising. The murmur might be short or absent in severe acute MR. In addition, [[S1]] is usually diminished and [[S2]] is commonly widely split. The pulmonic component of the second heart sound ([[P2]]) is louder than the aortic component ([[A2]]) in the presence of severe [[pulmonary hypertension]] thus widening the [[splitting of S2]].<ref name="pmid245898522">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= 129 | issue= 23 | pages= 2440-92 | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }}</ref><ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= 129 | issue= 23 | pages= 2440-92 | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | |||
===Vitals=== | ===Vitals=== | ||
*In acute mitral regurgitation, [[cardiogenic shock]] may be present. | *In acute mitral regurgitation, [[cardiogenic shock]] may be present. | ||
*A compensatory [[tachycardia]] may be present. | *A compensatory [[tachycardia]] may be present. Tachycardia can also be present in case of [[atrial fibrillation]]. | ||
===Heart=== | ===Heart=== | ||
| Line 24: | Line 25: | ||
====Auscultation==== | ====Auscultation==== | ||
=====Heart Sound===== | =====Heart Sound===== | ||
* First heart sound, [[S1]] is usually diminished due to failure of mitral valves to close properly. In case of mitral valve prolapse, S1 is normal as initial closure of mitral valve cusps is unimpeded. | * First heart sound, [[S1]] is usually diminished due to failure of mitral valves to close properly. In case of [[mitral valve prolapse]], S1 is normal as initial closure of mitral valve cusps is unimpeded. | ||
* Second heart sound, [[S2]] is commonly widely split due to shorter time duration of left ventricular ejection so an early [[A2]]. | * Second heart sound, [[S2]] is commonly widely split due to shorter time duration of left ventricular ejection so an early [[A2]]. | ||
* Pulmonic component of second heart sound ([[P2]]) is louder than aortic component ([[A2]]) in presence of severe [[pulmonary hypertension]] thus further widening the splitting of S2. | * Pulmonic component of second heart sound ([[P2]]) is louder than aortic component ([[A2]]) in presence of severe [[pulmonary hypertension]] thus further widening the splitting of S2. | ||
* Third heart sound, [[S3]] may also be heard due to rapid filling of left ventricle. S3 in this case should not be interpreted as a feature of [[heart failure]]. | * Third heart sound, [[S3]] may also be heard due to rapid filling of [[left ventricle]]. S3 in this case should not be interpreted as a feature of [[heart failure]]. | ||
* In patients with mitral regurgitation due to [[mitral valve prolapse]], a mid systolic click is usually present. | * In patients with mitral regurgitation due to [[mitral valve prolapse]], a mid systolic click is usually present. | ||
=====Murmurs===== | |||
{| align="center" | |||
! | |||
|-valign="top" | |||
| [[Image:MR_murmur_1.JPG|thumb|200px|Holosystolic murmur of acute mitral regurgitation.]] | |||
| [[Image:MR_murmur_2.JPG|thumb|200px|Holosystolic murmur of chronic mitral regurgitation.]] | |||
|} | |||
*Quality: High pitched and blowing. Best heard with diaphragm of stethoscope with patient in left lateral dicubitus position. | *Quality: High pitched and blowing. Best heard with diaphragm of stethoscope with patient in left lateral dicubitus position. | ||
*Location: Usually best heard over the apical region with radiation to left axilla and left subscapular area. | *Location: Usually best heard over the apical region with radiation to left [[axilla]] and left subscapular area. | ||
:*Posterior leaflet dysfunction murmur tends to radiate to the sternum or the aortic area. | :*Posterior leaflet dysfunction murmur tends to radiate to the [[sternum]] or the aortic area. | ||
:*Anterior leaflet dysfunction murmur tends to radiate to the back. | :*Anterior leaflet dysfunction murmur tends to radiate to the back. | ||
*Duration: | *Duration: | ||
:*In the presence of an incompetent mitral valve, the pressure in the left ventricle becomes greater than that in the left atrium at the onset of isovolumic contraction, which corresponds to the closing of the mitral valve (S1). This explains why the murmur in mitral regurgitation starts at the same time as S1. This difference in pressure extends throughout systole and can even continue after the aortic valve has closed, explaining how it can sometimes drown the sound of S2. Hence named '''[[Holosystolic Murmur]]'''. | |||
:*In the presence of an incompetent mitral valve, the pressure in the [[left ventricle]] becomes greater than that in the [[left atrium]] at the onset of isovolumic contraction, which corresponds to the closing of the [[mitral valve]] (S1). This explains why the murmur in mitral regurgitation starts at the same time as S1. This difference in pressure extends throughout [[systole]] and can even continue after the [[aortic valve]] has closed, explaining how it can sometimes drown the sound of S2. Hence named '''[[Holosystolic Murmur]]'''. | |||
:* However, in acute severe MR, the murmur can be '''early systolic''' rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the [[left atrium]] and the equalization of pressures between the [[left atrium]] and [[left ventricle]]. The murmur might be short or absent in severe acute MR.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= 129 | issue= 23 | pages= 2440-92 | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | |||
:*If the murmur is heard in late systolic phase, it may be due to [[mitral valve prolapse]] or [[papillary muscle dysfunction]]. In these cases, S<sub>1</sub> will probably be normal since initial closure of mitral valve cusps is unimpeded. Mid systolic click is also suggestive of [[mitral valve prolapse]]. | :*If the murmur is heard in late systolic phase, it may be due to [[mitral valve prolapse]] or [[papillary muscle dysfunction]]. In these cases, S<sub>1</sub> will probably be normal since initial closure of mitral valve cusps is unimpeded. Mid systolic click is also suggestive of [[mitral valve prolapse]]. | ||
| Line 52: | Line 62: | ||
:*Vasodilators (Amyl nitrate): Mitral regurgitation murmur softens due to decrease in afterload and hence increased stroke volume. Murmur of mitral valve prolapse is biphasic - initially soft, then loud. | :*Vasodilators (Amyl nitrate): Mitral regurgitation murmur softens due to decrease in afterload and hence increased stroke volume. Murmur of mitral valve prolapse is biphasic - initially soft, then loud. | ||
{{#ev:youtube|vL0s_nEkC8Q}} | |||
{{#ev:youtube|akr_MFTKiF4}} | {{#ev:youtube|akr_MFTKiF4}} | ||
Latest revision as of 16:01, 18 December 2019
| Resident Survival Guide |
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation physical examination On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation physical examination |
|
Risk calculators and risk factors for Mitral regurgitation physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.; Yamuna Kondapally, M.B.B.S[3]
Overview
Chronic compensated mitral regurgitation (MR) causes a blowing holosystolic murmur which radiates to the left axilla. In acute severe MR, the murmur can be early systolic rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the left atrium and the equalization of pressures between the left atrium and left ventricle. The intensity of the murmur decreases with valsalva maneuver and standing and becomes louder with hand grip, squatting, and leg raising. The murmur might be short or absent in severe acute MR. In addition, S1 is usually diminished and S2 is commonly widely split. The pulmonic component of the second heart sound (P2) is louder than the aortic component (A2) in the presence of severe pulmonary hypertension thus widening the splitting of S2.
Physical Examination
Chronic compensated mitral regurgitation (MR) causes a blowing holosystolic murmur which radiates to the left axilla. In acute severe MR, the murmur can be early systolic rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the left atrium and the equalization of pressures between the left atrium and left ventricle. The intensity of the murmur decreases with valsalva maneuver and standing and becomes louder with hand grip, squatting, and leg raising. The murmur might be short or absent in severe acute MR. In addition, S1 is usually diminished and S2 is commonly widely split. The pulmonic component of the second heart sound (P2) is louder than the aortic component (A2) in the presence of severe pulmonary hypertension thus widening the splitting of S2.[1][2]
Vitals
- In acute mitral regurgitation, cardiogenic shock may be present.
- A compensatory tachycardia may be present. Tachycardia can also be present in case of atrial fibrillation.
Heart
Palpation
- A palpable thrill may be present in acute mitral regurgitation.
- The apical impulse may be brisk and hyperdynamic and may be displaced leftwards secondary to left ventricular enlargement.
Auscultation
Heart Sound
- First heart sound, S1 is usually diminished due to failure of mitral valves to close properly. In case of mitral valve prolapse, S1 is normal as initial closure of mitral valve cusps is unimpeded.
- Second heart sound, S2 is commonly widely split due to shorter time duration of left ventricular ejection so an early A2.
- Pulmonic component of second heart sound (P2) is louder than aortic component (A2) in presence of severe pulmonary hypertension thus further widening the splitting of S2.
- Third heart sound, S3 may also be heard due to rapid filling of left ventricle. S3 in this case should not be interpreted as a feature of heart failure.
- In patients with mitral regurgitation due to mitral valve prolapse, a mid systolic click is usually present.
Murmurs
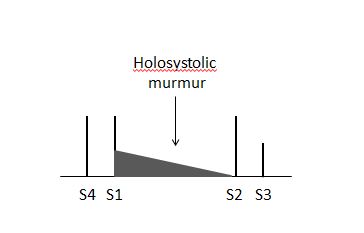 |
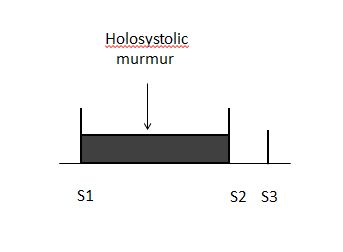 |
- Quality: High pitched and blowing. Best heard with diaphragm of stethoscope with patient in left lateral dicubitus position.
- Location: Usually best heard over the apical region with radiation to left axilla and left subscapular area.
- Posterior leaflet dysfunction murmur tends to radiate to the sternum or the aortic area.
- Anterior leaflet dysfunction murmur tends to radiate to the back.
- Duration:
- In the presence of an incompetent mitral valve, the pressure in the left ventricle becomes greater than that in the left atrium at the onset of isovolumic contraction, which corresponds to the closing of the mitral valve (S1). This explains why the murmur in mitral regurgitation starts at the same time as S1. This difference in pressure extends throughout systole and can even continue after the aortic valve has closed, explaining how it can sometimes drown the sound of S2. Hence named Holosystolic Murmur.
- However, in acute severe MR, the murmur can be early systolic rather than the typical holosystolic murmur in chronic MR due to the abrupt elevation in the pressure in the left atrium and the equalization of pressures between the left atrium and left ventricle. The murmur might be short or absent in severe acute MR.[2]
- If the murmur is heard in late systolic phase, it may be due to mitral valve prolapse or papillary muscle dysfunction. In these cases, S1 will probably be normal since initial closure of mitral valve cusps is unimpeded. Mid systolic click is also suggestive of mitral valve prolapse.
- Effect of Maneuvers: Murmur of mitral regurgitation may be difficult to distinguish from that of other valve diseases. Certain maneuvers may be helpful in this regard.
- Respiration: There is little variation on intensity of mitral regurgitation murmur with respiration. However in some, there is increase in intensity of murmur during expiration.
- Valsalva Maneuver: The intensity of mitral regurgitation murmur decreases with valsalva maneuver as the venous return to heart is reduced. However in mitral regurgitation due to mitral valve prolapse, systolic murmur becomes longer and often louder.
- Hand grip Maneuver: Mitral regurgitation murmur becomes louder with hand grip as afterload increases.
- Positional changes:
- Standing: Intensity of mitral regurgitation murmur decreases while increases in mitral valve prolapse due to decreased in venous return (preload).
- Leg raising: Intensity of mitral regurgitation murmur increases while decreases in mitral valve prolapse due to increase in preload.
- Squatting: Intensity of murmur increases due to increased venous return while murmur of mitral valve prolapse, softens.
- Vasodilators (Amyl nitrate): Mitral regurgitation murmur softens due to decrease in afterload and hence increased stroke volume. Murmur of mitral valve prolapse is biphasic - initially soft, then loud.
{{#ev:youtube|vL0s_nEkC8Q}} {{#ev:youtube|akr_MFTKiF4}}
References
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (23): 2440–92. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ 2.0 2.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (23): 2440–92. doi:10.1161/CIR.0000000000000029. PMID 24589852.