Differentiating Diabetes insipidus from other diseases: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
|||
| (23 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | [[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Diabetes_insipidus]] | ||
{{ | {{CMG}}; {{AE}} {{DAMI}} | ||
==Overview== | ==Overview== | ||
The most important differential diagnosis for diabetes insipidus include: Central diabetes insipidus, acquired, [[Trauma]] ([[surgery]], deceleration injury), [[Vascular]] ([[cerebral hemorrhage]], [[infarction]], [[anterior communicating artery aneurysm]] or [[ligation]], intra-hypothalamic [[hemorrhage]]), [[Neoplastic]] ([[craniopharyngioma]], [[meningioma]], [[germinoma]], [[pituitary tumor]] or [[Metastasis|metastases]]), [[Granulomatous]] ([[histiocytosis]], [[sarcoidosis]]), [[Infectious]] ([[meningitis]], [[encephalitis]]), [[Inflammatory]]/[[autoimmune]] ([[lymphocytic]] infundibuloneurohypophysitis), [[Drug]]/[[toxin]]-induced ([[ethanol]], [[diphenylhydantoin]], snake venom), [[hydrocephalus]], [[Idiopathic]], [[Congenital disorder|congenital]], [[Congenital malformations]], nephrogenic diabetes insipidus: [[Acquired disorder|Acquired]], drug-induced ([[demeclocycline]], [[lithium]], [[cisplatin]], [[methoxyflurane]], etc.), [[Hypercalcemia]], [[hypokalemia]], infiltrating lesions ([[sarcoidosis]], [[amyloidosis]], [[multiple myeloma]], [[Sjögren's syndrome|Sjogren's disease]]), [[Vascular]] ([[Sickle-cell disease|sickle cell disease]]), congenital, [[X-linked recessive]], primary polydipsia,[[Psychogenic]], dipsogenic (downward resetting of thirst threshold), gestational diabetes insipidus, [[Diabetes mellitus]]. | |||
== Differentiating diabetes insipidus based on the type of diabetes insipidus caused == | |||
The most important differential diagnosis for diabetes insipidus include:<ref name="pmid10369876">{{cite journal| author=Willcutts MD, Felner E, White PC| title=Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin. | journal=Hum Mol Genet | year= 1999 | volume= 8 | issue= 7 | pages= 1303-7 | pmid=10369876 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10369876 }} </ref><ref name="pmid19897608">{{cite journal| author=Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC et al.| title=Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy. | journal=Eur J Endocrinol | year= 2010 | volume= 162 | issue= 2 | pages= 221-6 | pmid=19897608 | doi=10.1530/EJE-09-0772 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19897608 }} </ref><ref name="pmid9350817">{{cite journal| author=Barrett TG, Bundey SE| title=Wolfram (DIDMOAD) syndrome. | journal=J Med Genet | year= 1997 | volume= 34 | issue= 10 | pages= 838-41 | pmid=9350817 | doi= | pmc=1051091 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9350817 }} </ref> | |||
* | {| class="wikitable" | ||
** | !Type of DI | ||
*** | !Subclass | ||
*** | !Disease | ||
** | !Defining signs and symptoms | ||
*** | !Lab/Imaging findings | ||
*** | |- | ||
** | ! rowspan="5" |Central | ||
*** | ! rowspan="3" |Acquired | ||
**** | ![[Histiocytosis]] | ||
**** | | | ||
**** | * Bone lysis and [[Bone fracture|fracture]] | ||
*** | * Purulent [[otitis media]] | ||
**** | * [[Diabetes insipidus]] and delayed puberty | ||
**** | * [[Maxillary]], [[mandibular]], and [[gingival]] disease | ||
**** | * [[Rash]] and [[Erythematous|maculoerythematous]] skin lesions | ||
* Scaly, [[erythematous]] scalp patches | |||
* [[Lung]] involvement | |||
* [[GI bleeding]] | |||
* [[Lymphadenopathy|Lymph node enlargement]]<ref name="pmid1340034">{{cite journal| author=Ghosh KN, Bhattacharya A| title=Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory. | journal=Rev Inst Med Trop Sao Paulo | year= 1992 | volume= 34 | issue= 2 | pages= 181-2 | pmid=1340034 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1340034 }} </ref> | |||
| | |||
* CD1a and CD45 + | |||
* Interleukin-17 (ILITA) | |||
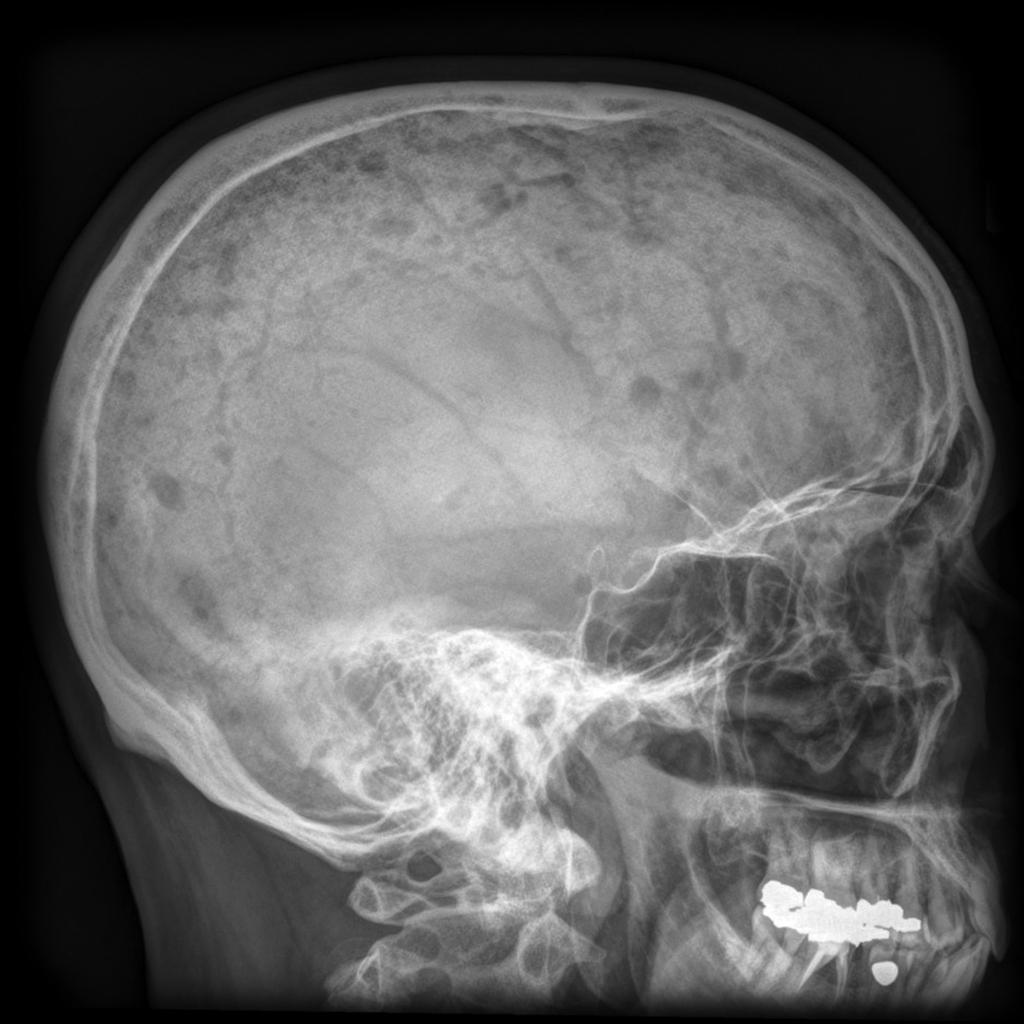
[[Image:Langerhans Skull X ray.jpg|center|300px|thumb|Skull x-ray of a patient with Langerhan's histiocytosis showing lytic lesions - Case courtesy of Dr Hani Salam, Radiopaedia.org, rID: 9459]] | |||
|- | |||
![[Craniopharyngioma]] | |||
| | |||
* [[Headache]] | |||
* [[Endocrine disorders|Endocrine dysfunction]] | |||
** [[Diabetes insipidus]] | |||
** [[Hypothyroidism]] | |||
** [[Adrenal failure]] | |||
** [[Diabetes insipidus]] (e.g., excessive fluid intake and urination) | |||
** Growth failure and [[delayed puberty]] | |||
| | |||
* [[Suprasellar]] calcified cyst on [[MRI]] | |||
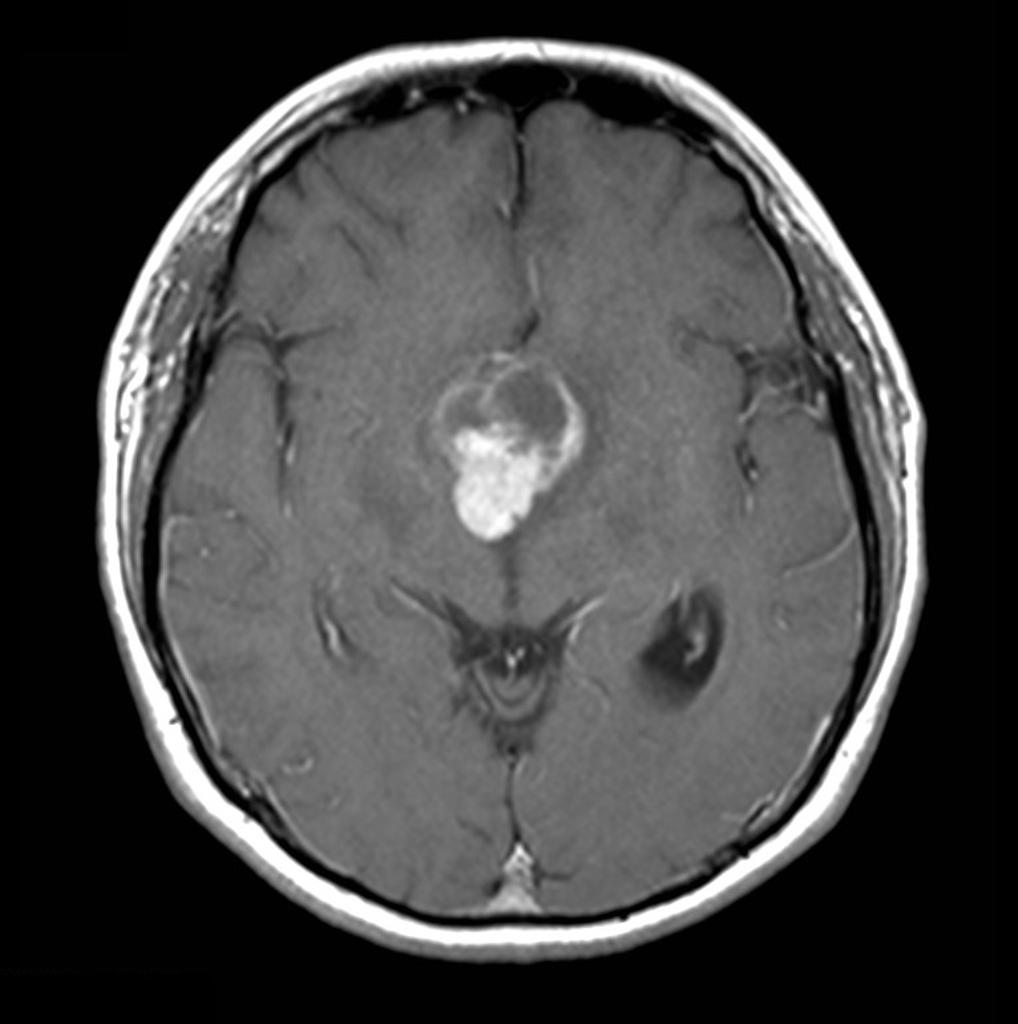
[[Image:Craniopharyngioma-papillary-1.jpg|center|300px|thumb|Brain MRI showing suprasellar mass consistent with the diagnosis of craniopharyngioma - Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 16812]] | |||
|- | |||
![[Sarcoidosis]] | |||
| | |||
* Systemic complaints | |||
** [[Fever]] | |||
** [[Anorexia]] | |||
** [[Arthralgias]] | |||
* Pulmonary complaints | |||
** [[Dyspnea on exertion]] | |||
** [[Cough]] | |||
** Chest pain, | |||
** [[Hemoptysis]] (rare) | |||
* [[Diabetes mellitus]] | |||
| | |||
* [[Hypercalcemia]] | |||
* [[Hypercalciuria]] ([[Granulomas|noncaseating granulomas]]) | |||
* Elevated [[alkaline phosphatase]] | |||
* [[Serum amyloid A]] (SAA) | |||
* [[Angiotensin-converting enzyme|ACE]] levels may be elevated | |||
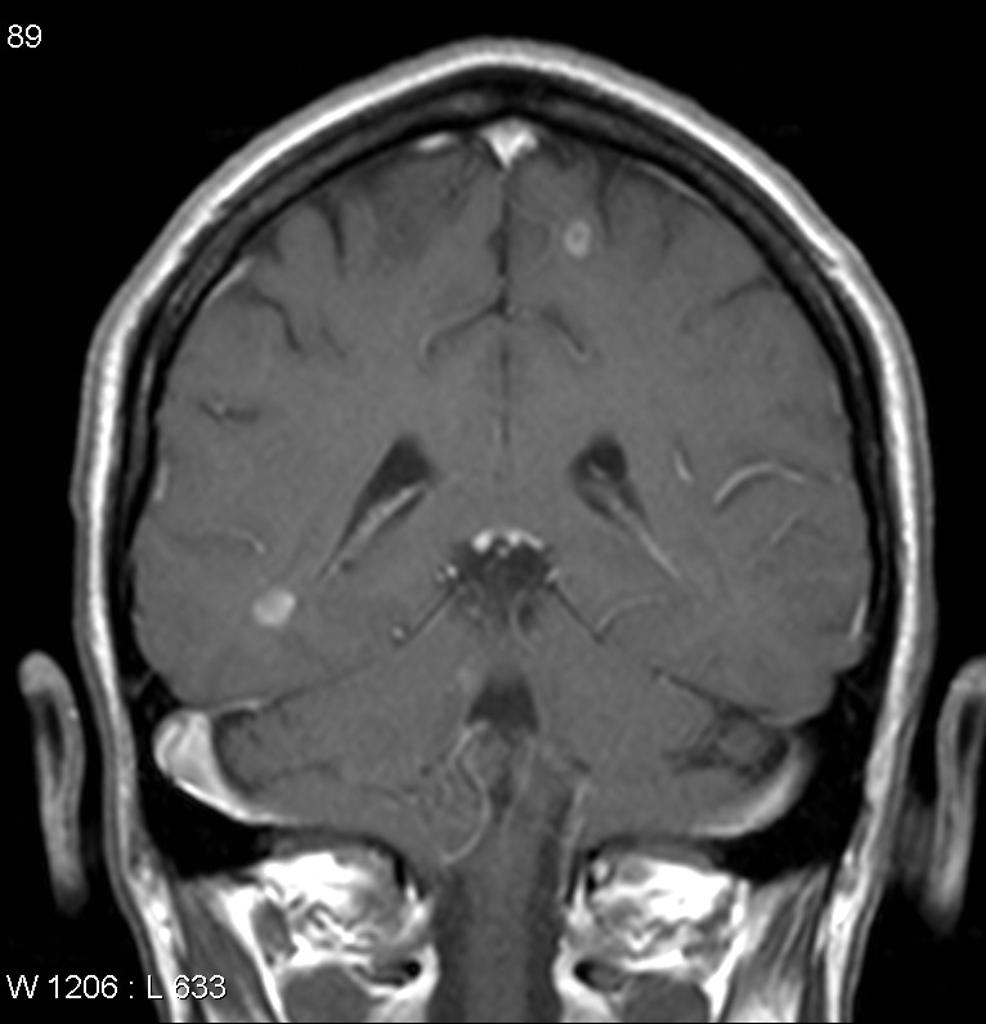
[[Image:Neurosarcoidosis.jpg|center|300px|thumb|Contrast-enhanced patches in a patient previously diagnosed with lung sarcoidosis - Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 10930]] | |||
|- | |||
! rowspan="2" |Congenital | |||
![[Hydrocephalus]] | |||
| | |||
* Cognitive deterioration | |||
* [[Headaches]] | |||
* [[Neck pain]] | |||
* [[Blurred vision]] | |||
* [[Unsteady gait]] | |||
* [[Incontinence]] such as [[polyuria]] | |||
|Dilated [[ventricles]] on [[Computed tomography|CT]] and [[Magnetic resonance imaging|MRI]] | |||
[[Image:Obstructive-hydrocephalus.jpg|center|300px|thumb|Obstructive hydrocephalus showing dilated lateral ventricles - Case courtesy of Dr Paul Simkin, Radiopaedia.org, rID: 30453]] | |||
|- | |||
![[Wolfram syndrome|Wolfram Syndrome]] (DIDMOAD) | |||
| | |||
* [[Diabetes insipidus|Diabetes Insipidus]] | |||
* [[Diabetes mellitus|Diabetes Mellitus]] | |||
* [[Optic atrophy|Optic Atrophy]] | |||
* [[Deafness]] | |||
| | |||
* Negative [[islet cell]] antibodies | |||
* [[Optic atrophy]] on [[electroretinogram]] | |||
* [[Deafness]] on [[audiogram]] | |||
* [[Atrophy]] of brain stem on [[Magnetic resonance imaging|MRI]] | |||
|- | |||
! rowspan="5" |[[Nephrogenic diabetes insipidus|Nephrogenic]] | |||
! rowspan="5" |[[Acquired disorder|Acquired]] | |||
!Drug-induced ([[demeclocycline]], [[lithium]]) | |||
| | |||
* [[Polyuria]] | |||
* [[Polydipsia]] | |||
* [[Nocturia]] | |||
| | |||
* [[Urine osmolality]] <100 mmol/ | |||
* [[Arginine vasopressin]] level >4.6 pmol/ | |||
* Little or no response to administration of exogenous [[arginine vasopressin]] | |||
|- | |||
![[Hypercalcemia]] | |||
| | |||
* [[Polyuria]] | |||
* [[Polydipsia]] | |||
* [[Gastrointestinal]] disturbances | |||
* [[Bone fracture|Pathological fractures]] | |||
* [[Confusion]] | |||
* [[Palpitations]] and [[cardiac arrhythmias]] | |||
| | |||
* Ca levels greater than 11 meq/L | |||
|- | |||
![[Hypokalemia]] | |||
| | |||
* [[Polyuria]] | |||
* [[Hyporeflexia]] | |||
* [[Palpitations]] and [[cardiac arrhythmias]] | |||
| | |||
* K levels less than 3meq/L on CBC | |||
|- | |||
![[Multiple myeloma]] | |||
| | |||
* Pathologic [[bone fractures]] | |||
* [[Bleeding]] | |||
* [[Hypercalcemia]] leading to [[polyuria]] | |||
* [[Infection]] | |||
* [[Hyperviscosity]] | |||
* [[Anemia]] | |||
| | |||
* [[IgG]] or [[IgA]] spike on [[serum protein electrophoresis]] | |||
* [[Monoclonal antibody|Monoclonal M spike]] | |||
* Disordered [[plasma cell]] proliferation on [[bone marrow biopsy]] | |||
[[Image:Multiple-myeloma-skeletal-survey.jpg|center|300px|thumb|Skeletal survey in a patient with multiple myeloma showing multiple lytic lesions - Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 7682]] | |||
|- | |||
![[Sickle-cell disease|Sickle cell disease]] | |||
| | |||
* [[Chronic pain]] | |||
* [[Anemia]] | |||
* [[Aplastic crisis]] | |||
* Splenic sequestration | |||
* [[Infection]] | |||
* [[Isosthenuria]] presenting with [[polyuria]] | |||
| | |||
* [[Hemoglobin]] level is 5-9 g/dL | |||
* [[Hematocrit]] is decreased to 17-29% | |||
* [[Peripheral blood smear|Peripheral blood smears]] demonstrate [[Target cell|target cells]], elongated cells, and characteristic sickle erythrocytes | |||
* MRI can demonstrate [[avascular necrosis]] of the [[femoral]] and [[humeral]] heads | |||
[[Image:Sickle cells.jpg|center|300px|thumb|Blood film showing the sickle cells - By Dr Graham Beards - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=18421017]] | |||
|- | |||
! colspan="2" |Primary polydipsia | |||
![[Psychogenic]] | |||
| | |||
* [[Polyuria]] | |||
* [[Polydipsia]] | |||
* [[Nocturia]] | |||
| | |||
* Dry mucus membrane | |||
* History of [[psychiatric disorders]] | |||
|- | |||
! colspan="3" |Gestational diabetes insipidus | |||
| | |||
* [[Polyuria]] | |||
* [[Polydipsia]] | |||
* [[Nocturia]] | |||
* [[Pregnancy]] | |||
| | |||
* Dry mucus membranes | |||
* [[Pregnancy]] | |||
|- | |||
! colspan="3" |[[Diabetes mellitus]] | |||
| | |||
* [[Polyuria]] | |||
* [[Polydipsia]] | |||
* [[Nocturia]] | |||
* [[Weight gain (patient information)|Weight gain]] | |||
| | |||
* Elevated blood sugar levels >126 | |||
* Elevated [[HbA1c]] > 6.5 | |||
|} | |||
==References== | ==References== | ||
| Line 81: | Line 186: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Endocrinology]] | [[Category:Endocrinology]] | ||
[[Category:Nephrology]] | [[Category:Nephrology]] | ||
Latest revision as of 18:20, 25 February 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Omodamola Aje B.Sc, M.D. [2]
Overview
The most important differential diagnosis for diabetes insipidus include: Central diabetes insipidus, acquired, Trauma (surgery, deceleration injury), Vascular (cerebral hemorrhage, infarction, anterior communicating artery aneurysm or ligation, intra-hypothalamic hemorrhage), Neoplastic (craniopharyngioma, meningioma, germinoma, pituitary tumor or metastases), Granulomatous (histiocytosis, sarcoidosis), Infectious (meningitis, encephalitis), Inflammatory/autoimmune (lymphocytic infundibuloneurohypophysitis), Drug/toxin-induced (ethanol, diphenylhydantoin, snake venom), hydrocephalus, Idiopathic, congenital, Congenital malformations, nephrogenic diabetes insipidus: Acquired, drug-induced (demeclocycline, lithium, cisplatin, methoxyflurane, etc.), Hypercalcemia, hypokalemia, infiltrating lesions (sarcoidosis, amyloidosis, multiple myeloma, Sjogren's disease), Vascular (sickle cell disease), congenital, X-linked recessive, primary polydipsia,Psychogenic, dipsogenic (downward resetting of thirst threshold), gestational diabetes insipidus, Diabetes mellitus.
Differentiating diabetes insipidus based on the type of diabetes insipidus caused
The most important differential diagnosis for diabetes insipidus include:[1][2][3]
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
| Craniopharyngioma |
|
 | ||
| Sarcoidosis |
|
 | ||
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
| Multiple myeloma |
|
 | ||
| Sickle cell disease |
|
 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
References
- ↑ Willcutts MD, Felner E, White PC (1999). "Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin". Hum Mol Genet. 8 (7): 1303–7. PMID 10369876.
- ↑ Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC; et al. (2010). "Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy". Eur J Endocrinol. 162 (2): 221–6. doi:10.1530/EJE-09-0772. PMID 19897608.
- ↑ Barrett TG, Bundey SE (1997). "Wolfram (DIDMOAD) syndrome". J Med Genet. 34 (10): 838–41. PMC 1051091. PMID 9350817.
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.